Abstract
Introducion
The concept of a window of opportunity in hidradenitis suppurativa (HS) management suggests that early initiation of biological therapy leads to better outcomes, though its timing remains uncertain.
Methods
We conducted a retrospective observational multicenter study, including consecutive patients with moderate to severe HS who initiated secukinumab treatment following prior failure with systemic antibiotics or adalimumab. Therapeutic burden was defined as the sum of previous systemic treatment cycles and previous major surgical interventions for HS. Patients were followed up for 24 weeks. Main outcomes were safety and effectiveness, assessed through the proportion of patients achieving HS Clinical Response (HiSCR) and a 55% reduction in International HS Severity Score System (IHS4-55). Additionally, potential predictors of response to secukinumab were studied. Analysis was performed on an intention-to-treat basis.
Results
A total of 67 patients (33 men, 34 women) were included, with a mean age of 41.55 (11.94) years and a mean baseline IHS4 of 17.88 (11.13). The mean therapeutic burden was 6.06 (3.49). At week 24, 10.45% (7/67) of patients experienced adverse events, with three leading to treatment discontinuation. At week 24, 41.79% (28/67) of patients achieved HiSCR, and 44.78% (30/67) of patients achieved IHS4-55. HiSCR could not be calculated in 12 patients with a baseline AN count < 3. A lower therapeutic burden was significantly associated with a higher likelihood of achieving HiSCR and IHS4-55 at week 24.
Conclusions
Secukinumab showed safety and efficacy in real-world patients with HS, and the inverse correlation found between therapeutic burden and treatment response supports the concept of a window of opportunity, offering insights into its timing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
This study aims to evaluate the safety and effectiveness of secukinumab in real-world patients with hidradenitis suppurativa (HS), explore predictors of treatment response, and determine the optimal timing for intervention within the window of opportunity concept, in light of the limited data available. |
Is secukinumab effective and safe for the treatment hidradenitis suppurativa in real-world settings, and when is the window of opportunity? |
What was learned from this study? |
At week 24, 41.79% (28/67) of patients achieved HiSCR, and 44.78% (30/67) of patients achieved IHS4-55. 10.45% (7/67) of patients experienced adverse events. A lower therapeutic burden was significantly associated with a higher likelihood of achieving HiSCR and IHS4-55 at week 24. |
Secukinumab is safe and effective in real-world patients with HS, with a lower therapeutic burden being associated with a higher likelihood of treatment response, supporting the concept of a window of opportunity for intervention. |
Introduction
In June 2023, secukinumab received approval from the European Medicines Agency (EMA) for the treatment of hidradenitis suppurativa (HS) in patients refractory to conventional systemic therapies [1].
Despite the efficacy of biological treatments in managing other inflammatory dermatological conditions like psoriasis, the response rates among patients with HS remain limited, and predictive factors for treatment success are yet to be identified [2, 3].
There is growing recognition of the potential benefits of early intervention in HS, with suggestions of a critical window of opportunity for initiating biological therapy to effectively manage inflammation and halt disease progression. However, determining the precise duration of this window poses a challenge because of insufficient data [4, 5].
In light of these considerations, our study aims to assess the safety and effectiveness of secukinumab in real-world patients with HS, explore potential predictors of treatment response, and elucidate the optimal timing for intervention within the window of opportunity. Additionally, we seek to compare the performance of Hidradenitis Suppurativa Clinical Response (HiSCR) and International Hidradenitis Suppurativa Severity Score System (IHS4) as outcome measures [6,7,8].
Methods
Study Design and Patients
We conducted a multicenter, retrospective, observational study, involving six hospitals in southern Spain (Andalusia). Consecutive patients diagnosed with HS who initiated treatment with secukinumab between January 2018 and February 2023 were enrolled. The use of secukinumab was off-label and administered under compassionate use. Patients were not restricted to receiving secukinumab as monotherapy; they could continue or initiate any other HS medication alongside secukinumab at any time, following clinical practice and current treatment recommendations [9]. Procedures like incision and drainage, intralesional corticosteroid administration, and major surgical interventions for HS were also permitted.
Patients underwent assessment before initiating secukinumab and at weeks 16 and 24 of the treatment. The main endpoints included assessing the safety and effectiveness of secukinumab, as well as identifying potential predictive factors of treatment response. Data were collected from electronic medical records, which had been previously gathered through patient history and physical examination. During the coronavirus pandemic, some patients avoided in-person appointments, leading to the adoption of telemedicine consultations. When this resulted in significant data gaps in medical records, these patients were excluded from the study.
Inclusion and Exclusion Criteria
The inclusion criteria were (a) patients diagnosed with HS; (b) age ≥ 18 years; (c) moderate to severe HS, defined by a baseline IHS4 score of ≥ 4; (d) any baseline count of abscesses, inflammatory nodules, and draining tunnels; (e) previous failure of at least one cycle of oral antibiotic treatment; (f) prior contraindication, failure or adverse event with adalimumab; (g) initiated secukinumab treatment for HS.
The exclusion criteria were (a) age < 18 years; (b) presence of medical conditions contraindicating the use of secukinumab (such as hypersensitivity to secukinumab, inflammatory bowel disease, pregnancy, or lactation).
Variables of Interest
Main Outcomes
-
(A)
Safety: assessed by monitoring adverse events that occurred or worsened after the first dose of secukinumab.
-
(B)
Effectiveness: evaluated at two timepoints (weeks 16 and 24) through two different outcome measures: the proportion of patients achieving HiSCR and the proportion of patients achieving IHS4-55 [6,7,8].
Other Variables of Interest
-
(A)
Pain: assessed according to the Numerical Rating Scale (NRS), ranging from 0 (no pain at all) to 10 (worst possible pain ever) [9].
-
(B)
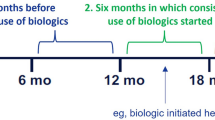
Therapeutic burden: defined as the cumulative sum of previous systemic treatment cycles (whether biological or not) plus the total number of previous surgical interventions (excluding incision and drainage procedures and intralesional steroid administration) that the patient had undergone for HS before initiating the study medication. In instances where the same systemic drug was administered two or more times at different intervals, each cycle was counted separately [10].
-
(C)
Concomitant treatment and cooling: Since this study was conducted in a real-world clinical setting, patients were allowed to use medical and surgical treatments concurrently, overlap them, or apply them on an ad hoc basis to alleviate the signs and symptoms of the disease. This information was collected individually for each patient and subsequently categorized into therapeutic groups for statistical analysis.
Ethics
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the local ethics committee. All participants provided informed consent before their inclusion in the study, and measures were taken to ensure confidentiality and anonymity of their personal information.
Statistics
We conducted an intention-to-treat analysis, which included all patients who initiated secukinumab treatment at week 0, regardless of whether they were lost to follow-up or discontinued secukinumab for any reason. These patients were categorized as non-responders.
Descriptive statistics were used to assess the characteristics of the sample. The Shapiro–Wilk test was utilized to evaluate the normality of the variables. Continuous variables are presented as mean and standard deviation (SD), while qualitative variables are presented as relative and absolute frequency distributions. Nominal variables were compared using the χ2 test or Fisher’s exact test, as appropriate, whereas Student’s t test or the Wilcoxon–Mann–Whitney test was used to compare between nominal and continuous data. Simple linear regression was used to explore potential associated factors for continuous variables, with the β coefficient and SD used to predict the log odds of the dependent variable. Multivariate logistic regression analyses were performed to explore the variables associated with clinical response HiSCR and IHS4-55. Epidemiological and statistical criteria were used to model variable selection. The effect of each exploratory variable on the model and its significance were studied. If the variable improved the model fit and adequacy (based on the likelihood ratio criteria and the significance of the parameter), it was kept; otherwise, the variable was excluded. The model was checked for pairwise interaction between covariates. Potential confounding covariates were studied using a change of significance in the model’s parameters or a change of 30% of its value. Statistical significance was considered at p values less than 0.05. All statistical analyses were performed using JMP version 9.0.1 (SAS Institute, North Carolina, USA).
Results
Baseline Demographic, Disease, and Treatment Characteristics of the Sample
Eighty-one patients with HS who began treatment with secukinumab between January 2018 and February 2023 were identified. Fourteen of these patients were excluded from the study because of significant missing data in their medical records. Consequently, a total of 67 patients with HS starting treatment with secukinumab were included in the study. The sociodemographic information, baseline characteristics, and therapeutic particularities of the sample are displayed in Table 1.
The mean age of the sample was 41.55 (± 11.94) years, and the male/female ratio was 33:34. Mean BMI was 30.21 (± 6.31) kg/m2. Nearly all patients had Hurley stage II (50.75%, 34/67) or III (44.78%, 30/67) HS. Mean baseline IHS4 was 17.88 (± 11.13) points.
All patients had prior exposure to at least one cycle of systemic antibiotics. Almost all patients (94.03%, 63/67) had previously been treated with adalimumab for HS. Prior to commencing secukinumab, 59.7% (40/67) of the patients had undergone at least one major surgical intervention for HS. The mean therapeutic burden before initiating secukinumab was 6.06 (± 3.49).
All 67 patients began secukinumab for HS according to the regimen: 300 mg subcutaneously weekly for 5 weeks, then followed by administration every 2 weeks (14 patients, 20.90%) or every 4 weeks (53 patients, 79.10%). By week 16, the regimen was modified for two patients (2.99%) from secukinumab every 4 weeks to every 2 weeks.
Eleven patients (16.42%) underwent cooling therapy for 4–6 weeks before initiating secukinumab, which was discontinued upon starting secukinumab. At baseline, eight patients (11.94%) were prescribed or continued combination therapy alongside secukinumab. By week 16, this number increased to 22 patients (32.84%), who were prescribed or continued combination therapy alongside secukinumab. The combination therapies included systemic antibiotics, oral corticosteroids, spironolactone, antiandrogenic oral contraceptive pills, or acitretin, either individually or in various combinations, as per standard clinical practice and current recommendations.
During secukinumab treatment, six patients (8.96%) underwent surgical intervention for HS structural lesions, consisting of deroofing or wide excision followed by closure through second intention.
Effectiveness
Hidradenitis Suppurativa Clinical Response (HiSCR)
HiSCR could not be calculated in 12 patients (17.91%) as a result of their baseline AN count being less than three. Firstly, we present the data including all patients, including those 12 in which HiSCR could not be calculated (N = 67): by week 16, 43.28% of patients (29/67) receiving secukinumab achieved HiSCR, while 38.81% (26/67) did not. By week 24, 41.79% (28/67) achieved HiSCR, and 40.30% (27/67) were non-responders. Subsequently, we provide data excluding the 12 patients in which HiSCR could not be calculated (N = 55): by week 16, 52.73% of patients (29/55) achieved HiSCR with secukinumab. By week 24, 50.91% (28/55) achieved HiSCR (Table 2 and Figs. 1 and 2).
Of the six patients who underwent major surgery for HS lesions during treatment with secukinumab, two of them achieved HiSCR at week 16, which was maintained at week 24. Two patients did not achieve HiSCR despite surgery at any point during follow-up. Finally, in two of these patients, HiSCR was not calculable.
Among patients achieving HiSCR at week 16, 79.31% (23/29) maintained the response by week 24, while 20.39% (6/29) experienced loss of response. Among patients not achieving HiSCR at week 16, 19.23% (5/26) achieved HiSCR at week 24 (Table 3).
International Hidradenitis Suppurativa Severity Score System (IHS4)
The mean IHS4 score decreased from 17.88 (± 11.13) points at baseline to 11.21 (± 10.64) points at week 16 and 9.61 (± 10.54) points at week 24 (both p < 0.0001 compared to baseline). This represents a mean reduction in IHS4 of 37.34% (± 2.74%) and 46.25% (± 3.30%) at weeks 16 and 24, respectively, compared to baseline. At week 16, 35.82% of patients (24/67) achieved IHS4-55. By week 24, this percentage increased to 44.78% (30/67).
Of the six patients who underwent major surgery for HS lesions during treatment with secukinumab, three of them achieved IHS4-55 at week 16, which was maintained at week 24. Three patients did not achieve IHS4-55 despite surgery at any point during follow-up.
Among patients achieving IHS4-55 at week 16, 87.50% (21/24) maintained the response at week 24, while 12.50% (3/24) experienced loss of response (Table 2 and Fig. 1) Among patients not achieving IHS4-55 at week 16, 20.93% (9/43) achieved IHS4-55 at week 24 (Table 3).
Pain
The mean pain NRS score decreased from 7.28 (± 2.09) at baseline to 5.04 (± 2.75) at week 16 and further to 4.61 (± 2.84) at week 24 (both p < 0.0001 compared to baseline). This represents a mean reduction in pain of 30.77% (± 9.07%) and 36.69% (± 10.29%) at weeks 16 and 24, respectively, compared to baseline.
Safety and Treatment Discontinuation
While undergoing secukinumab treatment, seven patients (10.45%) experienced adverse events. These included worsening of previous psoriasis, oral candidiasis, headaches, pain at the injection site, two cases of articular pain and inflammation, and one case of Crohn’s disease onset. The last three led to treatment discontinuation. By week 24, 21 patients (31.34%) discontinued secukinumab treatment: three patients (4.48%) due to loss to follow-up, three patients (4.48%) due to adverse events, and 15 patients (22.39%) due to lack of response (Table 4).
Predictors of Response to Secukinumab at Week 24
Hidradenitis Suppurativa Clinical Response (HiSCR)
We observed that patients achieving HiSCR at week 24 presented a shorter disease duration, a higher prevalence of Hurley stage I or II compared to stage III, and a lower therapeutic burden prior to initiating secukinumab, compared to the cohort of patients who did not achieve HiSCR at week 24. Multivariate analysis revealed that a therapeutic burden equal to or less than 5 was significantly and independently associated with a higher probability of achieving HiSCR at week 24 (p = 0.0288) (Table 5).
International Hidradenitis Suppurativa Severity Score System (IHS4)
Regarding IHS4-55, patients achieving it at week 24 showed a shorter disease duration, fewer affected areas, a higher frequency of Hurley stage I or II compared to stage III, a lower baseline IHS4, were more frequently prescribed secukinumab 300 mg every 4 weeks, and had a lower therapeutic burden, compared to those patients who did not achieve IHS4-55 (Table 6). Multivariate analysis also demonstrated that a therapeutic burden equal to or less than 5 was significantly and independently associated with a higher probability of achieving IHS4-55 at week 24 (p = 0.0341) (Table 6).
Cooling and Combination Therapy
The use of cooling therapy was not associated with improved HiSCR or IHS4-55 response rates. Similarly, combination therapy did not increase response probability and actually showed a trend towards worse HiSCR and IHS4-55 response rates.
Discussion
On the basis of the findings of this study, we concluded that secukinumab demonstrates safety and effectiveness in real-world clinical settings for patients with HS refractory to conventional systemic therapy. Key highlights include the comparison between IHS4-55 and HiSCR performance and the notable inverse correlation observed between therapeutic burden and response to secukinumab at week 24 of treatment. This correlation supports the concept of a window of opportunity in HS management.
Two randomized controlled trials (RCTs), known as the Sunny Trials (Sunrise and Sunshine) [11], have evaluated the effectiveness of secukinumab for treating HS over 52 weeks. They compared secukinumab with placebo in patients with moderate to severe HS, with the primary outcome being the proportion of patients achieving HiSCR, ranging from 42% to 46% in the treatment arms. RCTs aim for internal validity by selecting patients on the basis of strict criteria, minimizing confounding variables. Real-world evidence (RWE) studies, like ours, reflect clinical practice, including diverse patients. This approach provides insights into treatment performance in everyday settings and among varied patient populations. Other RWE studies have assessed the effectiveness of secukinumab in HS, predominantly using HiSCR as the primary outcome measure, showing HiSCR rates ranging from 41% to 85% over follow-up durations of 12 to 52 weeks [10, 12,13,14,15,16,17,18,19]. However, these studies often had limited patient populations.
Our study, comprising 67 patients, represents the largest real-world investigation of secukinumab in HS to date. We conducted an intention-to-treat analysis. This approach minimizes bias by preventing higher response rates due to treatment discontinuation and ensuring a precise evaluation of treatment effectiveness. The use of other treatments for HS in combination with secukinumab means that the demonstrated efficacy cannot be entirely attributed to secukinumab in those patients who received additional therapies. Nonetheless, we found that patients receiving other treatments alongside secukinumab had worse HiSCR and IHS4-55 response rates, rather than the improved responses one might expect. This could be explained by the fact that combination therapy was administered to patients with more severe disease, for whom even a combination of systemic drugs and a biologic agent did not result in significant improvement.
Among the most commonly used tools, HiSCR primarily targets the reduction of inflammatory nodules and abscesses, but does not account for the reduction of draining tunnels in its calculation [6]. The most significant limitation of HiSCR is that it is not applicable in patients with a baseline AN count < 3. Recently, a novel tool, IHS4-55, has emerged for assessing HS treatment effectiveness.[7, 8]. It measures the proportion of patients achieving a reduction of at least 55% compared to baseline IHS4. Unlike HiSCR, IHS4-55 is applicable to all patients regardless of the baseline AN count and incorporates draining tunnels into its calculation in a dynamic and validated manner. At week 24, excluding the 12 patients with a baseline AN count < 3, 50.91% of the patients achieved HiSCR. However, considering all patients, 41.79% achieved HiSCR, and 44.78% achieved IHS4-55. These differences, particularly in the HiSCR percentages, underscore significant variations in treatment response depending on patient categorization. This is crucial to note, especially when interpreting scientific study results. In real clinical practice, these tools often hold less significance, as we rely more on the subjective improvement reported by the patient and observed by the attending physician when assessing treatment response.
Among patients achieving HiSCR and IHS4-55 by week 16, approximately 80% and 88%, respectively, sustained this response by week 24, indicating treatment persistence. However, around 20% for HiSCR and 12% for IHS4-55 experienced a loss of response over this period. For those not achieving HiSCR or IHS4-55 by week 16, nearly 20% in each group attained a response by week 24, suggesting delayed treatment efficacy in some individuals. HS involves flares alternating with periods of stability. This may contribute to the observed loss of response by week 24, as the cutoff point might coincide with a peak flare, masking overall treatment efficacy. Relying solely on one-point outcome measures like HiSCR or IHS4-55 may not capture the full disease activity spectrum over time. A new tool, the IHS4 cumulative score (IHS4-C), has been proposed to address this limitation by considering treatment outcomes across the entire observation period [20]. Incorporating factors like outbreak number and intensity could provide further insights into treatment effectiveness. For instance, a patient may not meet responder criteria based on HiSCR during an outbreak but may still benefit if outbreak frequency and intensity decrease over time.
The window of opportunity in HS refers to a critical timeframe during the course of the disease when interventions, particularly aggressive or early treatments, may have the most significant impact on disease progression, symptom management, and overall outcomes [21]. Marzano et al. [4] found an inverse correlation between therapeutic delay and clinical response to adalimumab, supporting early adalimumab use and providing evidence for a window of opportunity in HS treatment. However, despite growing recognition of its importance, the evidence on the precise timing and duration of this window remains limited, presenting a challenge in HS management.
Therapeutic burden (TB) is a concept already established in cancer and other chronic diseases [22, 23]. It refers to the overall impact of treatments on patients’ lives, encompassing factors such as treatment complexity, frequency, duration, and side effects. Managing TB involves optimizing treatment to achieve better outcomes. We adapted this concept for HS defining it as the cumulative impact of previous systemic treatment cycles (whether biological or not) and the number of prior surgical interventions, excluding minor procedures like incision and drainage or intralesional steroid administration [10]. We considered all systemic treatments used for HS management, including systemic antibiotics as well as other medications like acitretin or spironolactone. Regarding surgical interventions, these included only major procedures, specifically deroofing of tunnels or wide excision of areas with permanent structural damage. These interventions have the potential to significantly alter the course and severity of the disease, impacting on patient treatment. Minor procedures, on the other hand, are symptomatic treatments for single lesions, and do not typically affect the course of HS. Therefore, they were not included in the calculation of TB. Unlike broader definitions used in cancer or other chronic diseases, our adaptation of the TB focuses solely on the number of previous medical and surgical treatments in HS. While this adaptation may simplify the original concept, it remains practical and clinically relevant for assessing treatment history and burden on patients with HS. The inverse correlation between TB and clinical response supports the concept of a potential window of opportunity in HS treatment. A high TB may result from either a prolonged disease course with multiple treatments before initiating a biological drug or rapid disease progression with aggressive symptoms and accumulation of numerous treatments in a short timeframe. Our findings suggest that early prescription of secukinumab, based on treatment interventions rather than disease duration, correlates with improved treatment outcomes.
This study has limitations, including its retrospective design, lack of a control group, limited follow-up duration, and small sample size from a single geographic region. A longer follow-up period could provide more comprehensive insights. However, it is crucial to balance the duration of follow-up with maintaining an adequate sample size. Considering that the drug was used on a compassionate basis until it received formal indication and reimbursement, we believe that the 24-week follow-up strikes a reasonable balance. Nonetheless, we are committed to ongoing research and aim to present future data with a larger patient cohort and extended follow-up periods. Cooling therapy and combination treatments were applied heterogeneously according to standard clinical practice, often in patients with initially more severe disease. While this approach allows for the collection of safety data, it prevents us from drawing definitive conclusions about effectiveness, as seen in other studies [24]. These limitations may affect the generalizability of the findings.
Conclusions
Secukinumab demonstrated both safety and efficacy in real-world patients with HS. IHS4-55 offers advantages over HiSCR, being calculable in all patients and considering draining tunnels in its calculation. Therapeutic burden, which focuses on the number of previous medical and surgical treatments for HS, could serve as a valuable tool for assessing treatment history and burden on patients with HS. The observed inverse correlation between therapeutic burden and treatment response further supports the concept of a window of opportunity, offering valuable insights into its timing.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cosentyx | European Medicines Agency. https://www.ema.europa.eu/en/medicines/human/EPAR/cosentyx. Accessed 10 Mar 2024.
Maronese CA, Moltrasio C, Genovese G, Marzano AV. Biologics for hidradenitis suppurativa: evolution of the treatment paradigm. Expert Rev Clin Immunol. 2024;20(5):525–45.
Silverberg JI, Thyssen JP, Fahrbach K, et al. Comparative efficacy and safety of systemic therapies used in moderate-to-severe atopic dermatitis: a systematic literature review and network meta-analysis. J Eur Acad Dermatol Venereol. 2021;35(9):1797–810.
Marzano AV, Genovese G, Casazza G, et al. Evidence for a ‘window of opportunity’ in hidradenitis suppurativa treated with adalimumab: a retrospective, real-life multicentre cohort study. Br J Dermatol. 2021;184(1):133–40.
Melgosa Ramos FJ, García-Ruiz R, Mateu Puchades A, Martorell A. Can we improve prognosis in hidradenitis suppurativa? identifying patients in the window of opportunity. Actas Dermosifiliogr. 2024;115(2):213–4.
Kimball AB, Sobell JM, Zouboulis CC, et al. HiSCR (Hidradenitis Suppurativa Clinical Response): a novel clinical endpoint to evaluate therapeutic outcomes in patients with hidradenitis suppurativa from the placebo-controlled portion of a phase 2 adalimumab study. J Eur Acad Dermatol Venereol. 2016;30(6):989–94.
Zouboulis CC, Tzellos T, Kyrgidis A, et al. Development and validation of the International Hidradenitis Suppurativa Severity Score System (IHS4), a novel dynamic scoring system to assess HS severity. Br J Dermatol. 2017;177(5):1401–9.
Tzellos T, van Straalen KR, Kyrgidis A, et al. Development and validation of IHS4-55, an IHS4 dichotomous outcome to assess treatment effect for hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2023;37(2):395–401.
Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619–44.
Fernandez-Crehuet P, Haselgruber S, Padial-Gomez A, et al. Short-term effectiveness, safety, and potential predictors of response of secukinumab in patients with severe hidradenitis suppurativa refractory to biologic therapy: a multicenter observational retrospective study. Dermatol Ther (Heidelb). 2023;13(4):1029–38.
Kimball AB, Jemec GBE, Alavi A, Reguiai Z, et al. Secukinumab in moderate-to-severe hidradenitis suppurativa (SUNSHINE and SUNRISE): week 16 and week 52 results of two identical, multicentre, randomised, placebo-controlled, double-blind phase 3 trials. Lancet. 2023;401(10378):747–61.
Prussick L, Rothstein B, Joshipura D, et al. Open-label, investigator-initiated, single-site exploratory trial evaluating secukinumab, an anti-interleukin-17A monoclonal antibody, for patients with moderate-to-severe hidradenitis suppurativa. Br J Dermatol. 2019;181(3):609–11.
Casseres RG, Prussick L, Zancanaro P, et al. Secukinumab in the treatment of moderate to severe hidradenitis suppurativa: results of an open-label trial. J Am Acad Dermatol. 2020;82(6):1524–6.
Reguiaï Z, Fougerousse AC, Maccari F, Bécherel PA. Effectiveness of secukinumab in hidradenitis suppurativa: an open study (20 cases). J Eur Acad Dermatol Venereol. 2020;34(11):e750–1.
Ribero S, Ramondetta A, Fabbrocini G, et al. Effectiveness of secukinumab in the treatment of moderate-severe hidradenitis suppurativa: results from an Italian multicentric retrospective study in a real-life setting. J Eur Acad Dermatol Venereol. 2021;35(7):e441–2.
Melgosa Ramos FJ, García-Ruiz R, Gegúndez Hernández H, Mateu-Puchades A. Real-life experience of secukinumab in patients with hidradenitis suppurativa. Actas Dermosifiliogr. 2023;114(4):T360–2.
Melgosa Ramos FJ, García Ruiz R, Estébanez Corrales A, Mateu PA. Long-term secukinumab efficacy in patients with moderate to severe hidradenitis suppurativa: a retrospective single-centre case series (23 patients). J Eur Acad Dermatol Venereol. 2023;37(4):e517–9.
Martora F, Marasca C, Cacciapuoti S, et al. Secukinumab in hidradenitis suppurativa patients who failed adalimumab: a 52-week real-life study. Clin Cosmet Investig Dermatol. 2024;17:159–66.
Ring HC, Thorsen J, Kirby B, et al. Long-term drug survival of adalimumab, infliximab, secukinumab and ustekinumab in hidradenitis suppurativa: a Danish nationwide cohort study. Br J Dermatol. 2024;2:042.
van der Zee HH, van Huijstee JC, van Straalen KR, et al. Viewpoint on the evaluation of severity and treatment effects in mild hidradenitis suppurativa: the cumulative IHS4 (IHS4-C). Dermatology. 2023. https://doi.org/10.1159/000535867.
Zouboulis CC. First real-world data provide evidence for a ‘window of opportunity’ in treatment of hidradenitis suppurativa/acne inversa. Br J Dermatol. 2021;184(1):10–1.
Spratt DE, Shore N, Sartor O, Rathkopf D, Olivier K. Treating the patient and not just the cancer: therapeutic burden in prostate cancer. Prostate Cancer Prostatic Dis. 2021;24(3):647–61.
Roodenrijs NMT, van der Goes MC, Welsing PMJ, et al. Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology (Oxford). 2021;60(8):3778–88.
Aarts P, van Huijstee JC, van der Zee HH, van Straalen KR, Prens EP. Improved clinical effectiveness of adalimumab when initiated with clindamycin and rifampicin in hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2024;38(5):904–9.
Acknowledgements
We would like to extend our heartfelt gratitude to all the patients who generously participated in this study. Their invaluable contribution and dedication made this research possible.
Medical Writing and Editorial Assistance
This article is part of the doctoral thesis conducted by Sofia Haselgruber. We did not receive any medical writing or editorial assistance for this study.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
The authors contributed to the study in the following ways: Data collection: Sofia Haselgruber, Pablo Fernandez-Crehuet-Serrano, Maria Dolores Fernandez-Ballesteros, Alicia Padial-Gomez, Juan Carlos Hernandez-Rodriguez, Juan Ortiz-Alvarez, Pedro Navarro-Guillamon, Cristina Membrive-Jimenez, and Carlos Cuenca-Barrales were responsible for collecting the data. Research supervision: Sofia Haselgruber, Pablo Fernandez-Crehuet-Serrano, Maria Dolores Fernandez-Ballesteros, Alicia Padial-Gomez, Juan Carlos Hernandez-Rodriguez, Juan Ortiz-Alvarez, Pedro Navarro-Guillamon, Cristina Membrive-Jimenez, and Carlos Cuenca-Barrales supervised the research activities. Statistical analysis: Sofia Haselgruber, Pablo Fernandez-Crehuet-Serrano, Maria Dolores Fernandez-Ballesteros, and Alejandro Molina-Leyva conducted the statistical analysis. Manuscript writing and drafting: Sofia Haselgruber, Maria Dolores Fernandez-Ballesteros, Alicia Padial-Gomez, Juan Carlos Hernandez-Rodriguez, Juan Ortiz-Alvarez, Pedro Navarro-Guillamon, Cristina Membrive-Jimenez, Carlos Cuenca-Barrales, and Alejandro Molina-Leyva wrote and drafted the manuscript. Manuscript revision, edition, and final acceptance: Sofia Haselgruber, Pablo Fernandez-Crehuet-Serrano, Maria Dolores Fernandez-Ballesteros, Alicia Padial-Gomez, Juan Carlos Hernandez-Rodriguez, Juan Ortiz-Alvarez, Pedro Navarro-Guillamon, Cristina Membrive-Jimenez, Carlos Cuenca-Barrales, and Alejandro Molina-Leyva revised, edited, and accepted the final version of the manuscript. Concept design: Alejandro Molina-Leyva was responsible for the conceptual design of the study.
Corresponding author
Ethics declarations
Conflict of Interest
Sofia Haselgruber declares no conflict of interest. Pablo Fernandez-Crehuet-Serrano declares no conflict of interest. Maria Dolores Fernandez-Ballesteros declares no conflict of interest. Alicia Padial-Gomez declares no conflict of interest. Juan Carlos Hernandez-Rodriguez declares no conflict of interest. Juan Ortiz-Alvarez declares no conflict of interest. Pedro Navarro-Guillamon declares no conflict of interest. Cristina Membrive-Jimenez declares no conflict of interest. Carlos Cuenca-Barrales declares no conflict of interest. Alejandro Molina-Leyva is an Editorial Board member of Dermatology and Therapy. Alejandro Molina-Leyva was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the local ethics committee. All participants provided informed consent before their inclusion in the study, and measures were taken to ensure confidentiality and anonymity of their personal information.
Additional information
Prior Presentation: The findings from this study were previously shared at the 13th Conference of the European Hidradenitis Suppurativa Foundation e.V., held in Lyon, France, on February 7–9, 2024.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Haselgruber, S., Fernández-Crehuet-Serrano, P., Fernández-Ballesteros, M.D. et al. Insights into the Window of Opportunity and Outcome Measures in Patients with Moderate to Severe Hidradenitis Suppurativa Treated with Secukinumab: A Real-World Study. Dermatol Ther (Heidelb) 14, 1875–1890 (2024). https://doi.org/10.1007/s13555-024-01209-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01209-w