Abstract
Hyaluronic acid (HA) dermal fillers, generally considered low-risk, can lead to rare late-onset reactions (LORs) manifesting between 3 and 4 months postinjection, occasionally even as early as 24 h postinjection. The Complication Assessment and Risk Evaluation (CARE) board was established to review these reactions. In this publication, the authors aims to explore the etiological hypotheses underlying LORs, associated risk factors, prevention, and management approaches suggested by the CARE board. The CARE board identified three etiological hypotheses contributing to LORs. Firstly, the physicochemical structure of the filler, particularly low molecular weight HA, which may trigger an immune response. Secondly, infection, potentially introduced during injection or by dormant biofilm activation. Lastly, an imbalance in the host immune system, caused by factors like autoimmune diseases or viral infections, may lead to extended foreign body reactions, delayed type IV hypersensitivity, or adjuvant-based reactions. Based on these hypotheses, the board categorized various risk factors as patient-related (e.g., recent dental treatment, current medical status, active autoimmune disease), product-related (e.g., molecular weight), and procedure-related (e.g., aseptic technique and trauma). To reduce the risk of LORs, the CARE board recommends diligent patient selection, including comprehensive medical history assessment and informed consent. Practitioners should maintain an effective aseptic technique, and choose an appropriate product and injection depth for the anatomical location. Post-procedure, patients should receive education on proper filler care. Management of LORs depends on the suspected etiology, and the CARE board has proposed an algorithm to determine the most appropriate treatment. Hyaluronidase is recommended for noninflammatory reactions in the absence of active infection, while watchful waiting and/or steroid treatment may be preferred for inflammatory reactions. Hyaluronidase is not recommended as a first-line treatment for infections, which require drainage, bacterial culture, and antibiotic treatment. However, the board emphasizes the need for individualized evaluation and treatment in all cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The CARE board was established to develop guidelines on how to prevent and manage complications associated with HA dermal filler injections, in this case, late-onset reactions (LORs). | |
The aim of this article was to review the etiological hypotheses underlying LORs, potential risk factors, and strategies for prevention and management. | |
The three etiological hypotheses that may contribute to LORs are the physicochemical structure of the filler, infection, and an imbalance in the host immune system. Based on these, risk factors were identified in three categories: patient-related, product-related, and procedure-related. | |
To reduce the risk of LORs, patients should be carefully selected on the basis of their medical history, aseptic technique must be maintained, and patients must be educated on proper filler care. | |
The CARE board has proposed a LOR risk assessment questionnaire and an algorithm for management of LORs depending on the suspected etiology. |
Introduction
The use of dermal fillers in cosmetic procedures has seen an increase in popularity over the past 25 years [1]. Among the wide array of fillers available, hyaluronic acid (HA) has emerged as the second most popular cosmetic minimally invasive procedure, constituting 85% of soft tissue filler use in the USA during 2022 [2].
While HA fillers have a well-established safety profile, the widespread use of these injectables has brought to light the occurrence of rare adverse events [3]. When defined in the same publication, the terms ‘delayed onset’ and ‘late onset’ are given different periods of onset, with ‘late onset’ referring to those that occur at least 2 weeks to 1 year post-injection and ‘delayed onset’ referring to those occurring over 1 year postinjection [3,4,5,6]. However, the two terms are more recently defined interchangeably between publications [7,8,9,10]. Therefore, this study adopts a distinct perspective by encompassing both under the term ‘late onset reactions’ (LORs). This decision aims to avoid confusion and draw a clear distinction between early reactions and LORs [8, 11].
The authors define early onset reactions as allergic or hypersensitivity type I reactions, which occur within minutes to hours after treatment and are characterized by an immediate immune response mediated by immunoglobulin E (IgE) antibodies. Symptoms can include hives, itching, swelling, or anaphylaxis. LORs, on the other hand, are thought to be T cell-mediated [3, 8, 12, 13] and typically manifest weeks to months following the injection of HA fillers, with a peak occurrence between 3 and 4 months. Some LORs may occur as early as 24 h postinjection [8, 13], although this is rare. These reactions include a variety of clinical manifestations, such as foreign body granulomas, edema, abscesses, postinflammatory hyperpigmentation, nodules (both inflammatory and noninflammatory), and late bacterial infections (Table 1) [13,14,15,16,17]. In terms of prevalence, inflammation and swelling/edema rank as the most common LORs, followed by nodules and induration. Reactions such as pain and tenderness, erythema, and granulomas are less common.
The array of clinical presentations highlights the complexity of LORs associated with HA fillers and the importance of a nuanced approach to understanding and managing these reactions. However, the cause of such reactions is often not well defined and initial treatment is similar regardless of etiology [11]. As such, the Complication Assessment and Risk Evaluation (CARE) board was established by Teoxane (Geneva, Switzerland) to bring together leading practitioners in Aesthetic Medicine with the goal of evaluating reactions observed following treatment with HA filler. The aim of this consensus article is to discuss the etiological hypotheses underlying LORs, the associated risk factors, and suggested approaches for prevention and management, as agreed by the CARE board. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Methods
CARE Board Development
A multidisciplinary panel of four experts comprising a dermatologist, an aesthetic doctor, a plastic surgeon, and a dental surgeon was selected to participate in the CARE advisory board, all of them with extensive experience in handling complications after HA dermal filler injection, and location of clinical practice in Aesthetic Medicine across different European countries (i.e., Poland, Spain, Switzerland, United Kingdom). The main objective of this board was to develop guidelines on how to prevent and manage complications associated with HA dermal filler injections. Initially, this involved creating a prioritized list of complications, categorized by their complexity and the varying levels of understanding and approaches to managing these specific reactions. Given the current lack of consensus in the definition and management of LORs, this adverse event was primarily selected. Then, a focused literature search was conducted to retrieve the latest research on the etiology, risk factors, prevention, and management of LORs. The CARE board members convened five separate times over presential and virtual meetings to review the current LOR literature and reach an agreement on the topics above.
Furthermore, two other significant outcomes from the CARE board discussions that can be applied in clinical settings included the development of an LOR risk assessment questionnaire, designed to determine a patient’s eligibility for treatment, and a treatment algorithm tailored to the cause of the LOR.
Literature Search
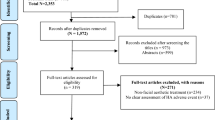
A comprehensive search of the peer-reviewed literature was conducted on 11 October 2023, using the Medline (PubMed) database to collect the most up-to-date scientific knowledge on LORs after hyaluronic acid dermal filler treatment. The focused literature review was structured using the Population, Intervention, Comparator, and Outcomes (PICO) strategy. Keywords related to HA dermal fillers and late- or delayed-onset reactions, late or delayed immune reactions, and late or delayed inflammatory reactions, were used (see Supplementary file 1).
A broad range of studies were included in this literature review, including systematic reviews, consensus guidelines, retrospective studies, surveys, case series, and reports. Studies were required to meet the following additional criteria to be included in this investigation: (1) report the occurrence of late onset reactions after HA dermal filler treatment in facial aesthetic indications; (2) describe any of the following: LOR etiology, associated risk factors, prevention, and management approaches; (3) be human studies; (4) be published in English with the full text available; and (5) be published between 1 January 2022 and 11 October 2023. A narrow search period was selected to address time constraints while focusing on the most recent and relevant literature. To mitigate the overlook of relevant studies published beyond the search time limit, meticulous cross-referencing of retrieved publications’ reference lists was conducted to ensure the incorporation of all significant studies. Additionally, focused searches were further supplemented with manual searches to identify additional, relevant studies not retrieved with the literature review protocol or published after the date of the search.
The exclusion criteria considered in this literature review were as follows: (1) patients treated for therapeutic indications; (2) complications other than LORs; (3) animal and in vitro studies; and (4) economic evaluations, editorials, notes, comments or letters, narratives, and articles without abstracts.
Etiology
All dermal fillers are recognized by the immune system as foreign bodies, and inflammation around the filler is a normal reaction [12]. The reactions can range from minor, involving limited macrophage infiltration, to severe, causing a granulomatous reaction with fibrosis [12]. Foreign body reactions to implants are an immediate response and do not involve an adaptive immune response, while T-cell-mediated granulomas (i.e., due to hypersensitivity type IV) are a type of LOR [8, 12].
The etiology underlying LORs is unknown, but there were three hypotheses that the CARE board agreed could contribute to their occurrence: (1) physicochemical structure of the filler, (2) infection due to inoculation, and (3) host response (i.e., mechanical, blood contamination). The etiology of LORs is likely to be multifactorial, with all three hypotheses potentially contributing to an individual case.
Physicochemical Structure of Filler
The first hypothesis concerns the physicochemical structure of the HA filler, with a particular focus on low molecular weight HA (LMW-HA). LMW-HA is produced endogenously during the body’s inflammatory response [8, 12], and its application to the skin has been shown to trigger an immune response in some patients [8, 17]. LMW-HA is believed to play a role in the development of late-onset nodules by activating toll-like receptors and stimulating the development of reactive oxygen species [18].
While LMW-HAs may not directly provoke an immune response in the absence of an endotoxin load [19], they may induce a proinflammatory effect in the presence of endotoxins [18, 20]. Contamination with Gram-negative bacteria containing lipopolysaccharides (i.e., endotoxins) may be introduced at any stage of the HA-based medical device manufacturing process [21]. Although these agents undergo purification to reduce the endotoxin load to a level believed to be insufficient for causing LORs, the presence of bacteria introduced during injection may be adequate to drive an inflammatory reaction [22, 23].
Many HA fillers incorporate a mixture of high molecular weight HA (HMW-HA) and intermediate molecular weight HA, which are considered by some authors to be too large to elicit a proinflammatory immune response [24]. In fact, HMW-HA may actively suppress inflammation, irrespective of the presence or absence of bacteria [19, 20].
However, the cross-linking technology employed during filler manufacturing can influence the product’s ability to break down into degradation products, including proinflammatory LMW-HA molecules [18, 25, 26]. Therefore, the delay in presentation of LORs could potentially be attributed to the time required for HMW-HA fillers to degrade into LMW-HA [18, 27].
Infection
The second hypothesis is that infection plays a role in the onset of LORs. This theory is supported by studies that outline the causative role of bacteria in the development of some LORs [22, 23, 28,29,30].
Postinjection, commensal skin surface pathogens are introduced into the injection site [18, 28]. These pathogens may undergo immediate destruction by the immune system, or they might become sequestered within the implanted filler. In the latter situation, two potential pathways can lead to LORs.
Firstly, the bacteria may remain dormant until the filler begins to degrade, releasing the bacteria in the process [31, 32]. There is a possibility that the production of LMW-HA from the degraded filler could further amplify the immune response in this situation [18]. Alternatively, a bacterial colony may begin to grow, forming a biofilm that aids in evading immune recognition until reaching sufficient numbers to alert the immune system [6, 27, 28]. This causes an upregulation of the immune response and subsequent inflammation.
Host Immune Response
The final hypothesis proposes that an imbalance in the host immune system is a key mechanism behind LORs. This is supported by the CARE board’s observation that many patients with LORs also have a form of active autoimmune disease, diagnosed before or after LOR clinical manifestation [33,34,35,36,37]. Additionally, the human leukocyte antigen (HLA) polymorphisms HLA-B*08 and DRB1*03 have been associated with LORs, indicating a potential immune pathway for reactions in these patients [7]. Changes in the patient’s immune status due to flu-like symptoms and vaccinations have also been correlated to the incidence of LORs [5, 11, 27, 38,39,40,41,42,43].
A potential cause of the immune response is an extended foreign body reaction. Typically, the inflammatory phase of the reaction is gradually replaced by a healing phase that facilitates tissue regeneration and repair [27]. However, in certain individuals, the transition to the anti-inflammatory phase may be impaired, leading to chronic inflammation and granuloma formation [27, 44].
Several papers have also suggested that delayed type IV hypersensitivity could underlie the immune response observed in LORs [3, 8, 39, 45, 46]. This particular reaction is initiated by T lymphocytes, and specifically mediated by CD4+ cells, typically occurring in all injected areas simultaneously, with no systemic effects observed at presentation [3]. However, in these cases, the hypersensitivity reaction would be expected to persist upon finishing corticosteroid treatment in those who did not also receive hyaluronidase to dissolve the filler, which is not always the case [27]. This inconsistency suggests that, at least in some cases, a mechanism other than delayed hypersensitivity must be involved.
One final mechanism underlying the immune response is an adjuvant-based reaction. HA filler can function as an adjuvant, triggering both the innate and adaptive immune responses despite lacking antigenic properties [8, 27, 31]. This type of inflammation mirrors autoimmune diseases and has the potential to become systemic, a condition termed autoimmune/autoinflammatory syndrome induced by adjuvants (ASIA) [47]. The risk of developing ASIA is thought to be influenced by previous exposure to adjuvants, adjuvant characteristics, and the extent of immune activation [27, 48]. Additionally, a genetic predisposition may play a role in this process [27, 31, 48].
The CARE board believes that the etiology behind LORs is likely multifactorial, with all three of these hypotheses contributing to varying degrees in all LOR cases. However, the etiology is unknown in many individual cases. This highlights the complexity of the mechanisms involved in LORs and emphasizes the need for a holistic approach in their prevention, taking into account risk factors for LOR development.
Risk Factors
Understanding the risk factors for LORs is crucial for minimizing the incidence of LORs in individuals undergoing filler treatments. These risk factors can be broadly categorized into three main groups: patient-related, product-related, or procedure-related (Fig. 1).
Patient-Related Risk Factors
The patient’s medical history plays a key role in determining the likelihood of LORs. This includes medications, previous filler, other procedures, infections, health conditions, and allergies (including allergy to bee stings).
Firstly, a documented, confirmed allergy or hypersensitivity to any component of the filler is a contraindication, including lidocaine used as an anesthetic [49].
In terms of prescribed medications, the use of immunosuppressants can heighten the risk of infection and biofilm formation, while immunotherapy can increase the likelihood of inflammatory reactions [8, 50]. Careful consideration of drug interactions is also crucial [17]. In particular, the CARE board expressed concerns about bruising caused by blood thinners and recommends that patients on these medications be informed about their increased risk of bruising following the procedure [51].
Existing permanent fillers (non-HA), particularly silicones and polyacrylamides, have higher infection and inflammation risks when other fillers are layered on top. Inflammation may arise from trauma or disruption to the existing filler, provoking an immune response and potentially leading to long lasting granulomas [4, 5], while infection can result from a needle-induced disruption in the surrounding bacteria [4]. Cross-brand layering is also advised against to minimize potential complications [5, 11].
Previous or elective dental, invasive diagnostic, and surgical procedures present an increased risk of hematogenous seeding of bacteria and biofilm formation, potentially leading to infection [5, 52]. This risk extends to all dental procedures, including teeth whitening [5]. Notably, in one study, six out of seven patients who developed late-onset nodules following HA filler injection had recently undergone dental treatment [53].
The risk of LORs can also be influenced by current infections, including remote infections such as those affecting the urinary tract, sinuses, or oral cavity, as well as viral or flu-like illnesses [5, 11, 38, 39]. The presence of an existing infection can trigger an inflammatory response preceding the formation of late onset nodules [5]. Interestingly, there may be a seasonal variation in LORs, with an increase in the winter flu season [17, 54], as suggested by the observation that up to 71% of LORs occur between September and December [53].
Patient factors that predispose to biofilm formation constitute another risk factor for LORs [30, 55], as filler material can facilitate the growth of bacterial biofilms [22, 23]. This includes patients that have a condition involving implantation of a foreign body, or those with cystic fibrosis [30, 55]. As previously mentioned, the HLA polymorphisms HLA-B*08 and DRB1*03 also contribute to the risk of developing LORs by altering the immune response [30].
A substantial proportion of patients who develop LORs are also affected by autoimmune disease [33,34,35,36,37]. Active autoimmune disease is often considered a contraindication for filler treatment [5, 14], given its association with an elevated risk of an immunogenic reaction [8]. Additionally, several autoimmune diseases are associated with higher blood concentrations of HA, contributing to inflammation [33, 36, 56]. Certain autoimmune diseases pose a higher risk (Fig. 2), and in some cases a genetic predisposition to autoimmune disease alone can lead to LORs.
Patients with rheumatoid arthritis and cutaneous vasculitis are at the highest risk of developing LORs, primarily due to the severity of inflammation and the need for corticosteroids (Fig. 2) [5, 57]. Various confounding factors make it challenging to determine the risk in these patients, including the treatment type, time on treatment, and severity of disease, making them poor candidates for HA treatment. HA filler is also generally discouraged in systemic lupus erythematosus, psoriatic arthritis, and systemic scleroderma [58]. However, HA treatment may be considered if the disease is not active. The CARE board has observed that the disease state is often able to be considered inactive when the condition is stable, and the patient has not experienced any flare-ups for at least two years [59]. To assess this, dermatology consultation records and antibody markers may be considered. In cases of systemic scleroderma where the disease is not active, the use of HA filler is considered beneficial to reduce scarring [58].
Localized scleroderma and Hashimoto disease are considered medium risk factors and use of HA filler in these patients should be approached with caution (Fig. 2) [60, 61]. In particular, high levels of antithyroid peroxidase and antithyroglobulin in Hashimoto disease are considered a contraindication.
Diseases characterized by a low grade of fibrosis are deemed low-risk and there is no specific recommendation against HA filler use in these patients (Fig. 2). This includes vitiligo and alopecia areata [52, 62]. Type I diabetes is not considered a contraindication, provided that the disease is well controlled and the patient has normal wound healing [52, 63]. The CARE board emphasizes that this list is not exhaustive, and caution should always be exercised when considering HA filler injection in individuals with autoimmune diseases.
Inflammatory skin conditions such as acne, rosacea, and dermatitis disrupt the barrier function of the skin, potentially allowing the penetration of infective agents [5]. Acne affects a much greater surface area of the skin than is visible and therefore the ‘safe distance’ for filler injection from an area of acne is unknown, suggesting that it may be preferable to delay treatment in patients with this condition [5]. Additionally, Cutibacterium acnes is present in inflammatory lesions, increasing the risk of biofilm formation [64]. The board also wishes to highlight the need for caution when injecting patients with hypertrophic scars or fibrotic tissue due to the abnormal wound healing observed in these individuals.
Late onset reactions may also be triggered by vaccines [40], including the coronavirus disease 2019 (COVID-19) vaccine [41, 65]. The mechanism behind the association between LORs and the COVID-19 vaccine involves a downregulation of the angiotensin converting enzyme 2 (ACE2), which is elevated in the filler implant sites, in homeostatic conditions. Exposure to the COVID-19 spike protein blocks ACE2, resulting in a localized proinflammatory response and subsequent inflammation, oxidative stress, and fibrosis [40, 66]. Similarly, LORs have been reported following administration of influenza and chickenpox vaccines [42, 43].
Product-Related Risk Factors
The properties of the HA filler itself can also contribute to the risk of LORs. Variation in risk observed between products may stem from how the body recognizes the filler or how readily the filler is degraded into fragments that can provoke an immune response.
The filler should not be chemically modified to the extent that it would no longer be recognized as HA, as this could cause prolonged foreign body reactions [3]. However, the acceptable limit of modifications remains unknown [3].
As mentioned previously, LMW-HA alerts the immune system to tissue damage and induces proinflammatory changes in macrophages [8, 12]. As a result, LMW-HA is associated with a higher incidence of LORs [8]. In fact, an online survey targeted to practitioners from ten regions in the Asia–Pacific area showed that more than half of practitioners believe that a higher composition of LMW-HA is a major factor associated with LORs [67]. Some HA fillers use 90% LMW-HA and have a risk of LORs ranging from 0.5% to 4%, which is higher than that observed with other fillers [11, 12, 38, 54, 68]. Among the newer HA fillers approved between 2016 and 2020, these LMW-HA fillers had the highest incidence of LORs, particularly inflammatory and noninflammatory nodules [9].
Other filler-related factors that have been suggested to affect LOR risk include the introduction of impurities from cross-linking and biofermentation, HA concentration, and particle characteristics such as surface area and charge [3]. However, this product information often remains confidential by the respective companies; therefore, it is difficult to establish any correlation to LORs [3].
Procedure-Related Risk Factors
Practitioners identified an ineffective aseptic technique as the third biggest risk factor for LORs, with 61% acknowledging its importance [67]. While complete skin sterilization is impossible due to the presence of bacteria in deep skin layers that are impenetrable by topical antiseptics [8], maintaining adequate aseptic technique can effectively reduce the risk of nodules with a bacterial etiology [14].
Concerning injection technique, bolus and pillar injections have been linked to granulomas [6]. Additionally, rapid injection speed, an aggressive fanning technique, and a large bolus size increase the risk of LORs in general [5]. The use of large filler volumes can induce significant inflammation, presenting another risk factor [4, 5]. The CARE board also emphasized the importance of trauma in triggering inflammatory responses, potentially due to its role in heightening the immune status of the individual [12]. Trauma can also activate quiescent biofilms, further exacerbating the inflammatory response and potentially leading to infection [12].
Regarding injection depth, injection into the mid-dermis or deep dermis is associated with the highest overall incidence of inflammatory events [69]. However, dermal or subdermal injections are associated with a higher risk of immune-mediated delayed granulomas [12]. Dermal injection is also associated with an increased incidence of nodules [69]. In terms of injection location, the lips are a common site for late onset nodules [12], while intramuscular injection is associated with LORs in general [3].
Prevention
It is generally acknowledged in the literature that patient selection, the injection procedure and technique, and post-treatment care play crucial roles in mitigating the risk of LORs [14, 17, 38, 67, 70].
Patient Selection
Patient selection holds great importance in reducing the risk of LORs. This should involve a comprehensive medical review of the subject and assessment of the presence of previous permanent and nonpermanent filler (this may be supplemented with the use of ultrasound) [14, 38]. This could involve giving the patient a risk assessment checklist, inquiring about recent vaccinations and procedures, current medications and dietary supplements, allergies, skin conditions, inflammatory conditions, and systemic diseases [5]. The CARE board has developed a questionnaire to give to patients prior to injection, to assess their suitability for treatment (Supplementary file 2).
The treatment should be delayed or canceled if the patient recently underwent dental procedures, had a recent procedure compromising the skin barrier, or has an active systemic or skin infection, inflammation, or autoimmune as well as granulomatous disease [14, 67]. Additionally, patients with an allergy to bee or wasp stings may also have an allergy to hyaluronidase [71]. This may prevent effective treatment in the event of an LOR and so treatment of these individuals should also be avoided. In the future, screening patients for their HLA status could identify predispositions to LORs, although larger trials are required to confirm the link between HLA genotype and immune-mediated reactions [7]. At least 1 week prior to injection, patients should be contacted to ensure they understand selection criteria and that they have received instructions on medication and food to avoid before injection [5]. Medications that impair the ability of platelets to function (i.e., nonsteroidal anti-inflammatories), anticoagulants, and certain foods (e.g., grapefruit) contribute to an increased risk of bruising [72], and patients should be informed of this before undergoing treatment with HA dermal fillers. The CARE board particularly emphasizes the importance of educating patients about the procedure and its associated risks, and subsequently obtaining detailed and comprehensive informed consent.
Injection Procedure and Technique
The anatomical location influences the level of risk associated with the procedure [14]. For instance, as mentioned previously, injection into the lips is associated with late-onset nodules, while intramuscular injection is associated with LORs in general [3, 12]. To mitigate the risk of LORs, product selection should carefully consider anatomical location and injection depth, with a caution against intramuscular injection recommended by the CARE board [14]. Avoiding products linked to LORs, such as those utilizing LMW-HA, is recommended by 90% of practitioners in an Asia–Pacific survey as a means of reducing LORs [67] and is also advised by the CARE board experts. Additionally, using the smallest possible bolus is advised to prevent mechanical irritation and inflammatory cascade activation [5, 14, 38, 67]. It is critical that the injector must thoroughly understand the product’s rheological properties [67] and refrain from mixing products of different rheology as it makes it difficult to determine the cause of an issue in the event of an LOR. Any areas of localized active inflammation or inflammatory skin conditions should be avoided, or treatment should be delayed in these individuals [38].
The injector’s aseptic technique is one of the most important preventative measures against LORs [14, 67]. Disinfecting the skin with alcohol alone is not sufficient and other antiseptic cleansers should be considered [14, 38]. The decision between chlorhexidine and isopropyl alcohol is highly debated; some believe that chlorhexidine is superior due to its continued antimicrobial effect when dry compared with alcohol, which needs reapplying during the procedure [4, 14, 17, 73, 74]. All make-up should be removed from the patient’s face prior to the procedure [14, 38]. Whether facial hair should be removed prior to injection is more controversial. On one hand, facial hair removal allows for a more accurate assessment of the patient’s anatomy and any potential active skin conditions; however, shaving in particular can cause skin lesions that increase the risk of infection following surgery [75]. Other methods of facial hair removal are under-explored [76]. The CARE board suggests that facial hair should be removed 3 days prior to filler injection to allow skin lesions to heal. During injections, practitioners must avoid touching the needle or cannula on the hair of the patient, and the needle/cannula should be changed regularly [5, 14, 38]. Extra care is necessary when injecting perioral areas, due to the high level of skin and oral bacteria present, and injection through the oral mucosa must be avoided [14, 67]. When treating multiple sites, perioral areas should be injected last to avoid potential contamination of other areas. Following the procedure, an antiseptic cream can also be applied to further reduce risk of infection [67]. The board advocates for standardized approaches across injectors and procedures to minimize the risk of contamination.
Regarding the injection procedure, the injector should always have a good knowledge of facial anatomy and be extensively trained in the procedure and available products. This includes knowledge of the appropriate injection procedure, including depth and plane of injection, based on the product and anatomic location [14]. For many procedures, both needles and cannulas can be used, but trauma should always be avoided to prevent excessive inflammatory responses and biofilm formation [12]. The number of injections and entry sites should be kept to a minimum [22, 67], whether using needles or cannulas. Additionally, regular injections should be avoided as this can trigger granuloma formation [77]. The CARE board emphasizes that injections every three months are too frequent and should be avoided.
Post-Treatment Care
Comprehensive patient education is essential to minimize the risk of LORs post-injection. They should be informed to wait at least 2 weeks before undergoing dental work, invasive diagnostic procedures, and surgical procedures [14, 67], as the risk of bacterial contamination is highest during this period [4]. Patients must avoid touching the treated area to prevent the introduction of bacteria [67]. Patients should also refrain from applying make-up and avoid exposure of the wound to tap water following injection [14, 38]. The recommended time to wait before applying make-up varies from 5 min to 24 h, but patients should ideally use clean, unopened make-up where possible [14]. The patient must also be informed about the potential requirement for off-label hyaluronidase treatment in the event of a LOR. Similarly, patients should be informed about the potential risks and complications following hyaluronidase treatment. These may include the potential loss of treatment effect and the occurrence of adverse reactions, such as itching, burning, swelling, redness, bruising, spread of infection, and, although rare, allergic reactions [78]. Patients are also recommended to avoid intensive physical exercise, sunbathing, sauna and tanning bed use, facial massage, laser treatment, radiofrequency, and ultrasound facial therapy.
Management
The management of LORs should be tailored towards the suspected etiology of the reaction. The expected symptoms by etiology are shown in Table 2. An algorithm for recommended treatment options is illustrated in Fig. 3.
Prior to treatment, a full medical history of the patient should be taken by the injector. To ensure all relevant medical and treatment history is taken into consideration and that information is easily passed on to new doctors, the questionnaire described earlier can be used (Supplementary file 2). An ultrasound may also be used to determine the presence of previous filler.
For noninflammatory (noninfection) reactions, such as nodules, administration of hyaluronidase is a reasonable first-line treatment, followed by oral steroids if the LOR is not responsive to hyaluronidase [11]. When the LOR is inflammatory, watchful waiting and/or treatment tapered oral steroids may be preferred, to avoid unnecessary use of hyaluronidase. In the case of infections, hyaluronidase may spread the infection further and should be avoided, instead, in fluctuant infections (i.e., lesion containing liquid, often related to infections or inflammatory processes), the abscess should be drained, and a culture should be conducted using the aspirated material. In nonfluctuant infections (i.e., solid, fibrotic nodules, such as granulomas), a punch biopsy should be conducted and cultured. In both cases, broad-spectrum antibiotics should be given to cover the infection until culture results are returned.
However, the CARE board emphasizes that this algorithm is a recommendation, and cases should be evaluated individually, ensuring to establish a working diagnosis rather than resorting to a treatment plan involving multiple medications. Please note that some recommended treatments may not be available in all countries and investigators should use their best judgement to prescribe a suitable alternative treatment. Cases should be referred to a local expert or dermatologist if symptoms persist after recommended treatment interventions.
Case Study 1
The patient received a total of 1 mL of HA dermal filler in the lips, as well as 1 mL in the chin. After 3 weeks, they experienced fever, chills, headache, weakness, muscle and joint pain, hands and feet edema, sleep disturbances, memory loss, and dry mouth. Concurrently, the patient suffered from swelling, redness, and pain at the lips and chin injection site (Fig. 4), along with sensations of burning and itching.
The patient underwent treatment with 32 mg of methylprednisolone tapered over a period of 2 months, along with hyaluronidase injections administered every 3–5 days, totaling six rounds, until no HA was detectable by ultrasound. Clarithromycin and antihistamines were also prescribed by the treating physician for 2 weeks. This treatment alleviated the symptoms, but after 2 weeks, all systemic symptoms returned. The patient was admitted to the hospital and underwent magnetic resonance imaging (MRI), which detected swelling of the mental nerve. Additional tests, including lab work, echography, and ultrasound, showed normal results. Based on the clinical symptoms and procedure results, a diagnosis of ASIA syndrome was made. An injection of 10 mg/ml of triamcinolone was given to the right side of the chin, which resulted in a gradual remission of systemic symptoms. Pain on the right side of the chin subsided after 2 months, and there were no symptoms present at the 8-month follow-up.
The occurrence of LOR at multiple injection sites indicated a moderate to severe, immune-mediated response. The CARE board agreed that this case represented an effective treatment of ASIA syndrome, in which the patient developed both systemic and local symptoms along with neurological disturbances, all triggered by an external factor, namely the HA dermal filler injection. Given the recurrence of symptoms following antibiotic and antihistamine treatment, yet resolution upon glucocorticoid administration, the CARE board recommends initiating steroid therapy as the first line intervention for such moderate to severe reactions.
Case Study 2
The patient received 1 ml of HA dermal filler for lip augmentation. A total of 2 months later, they developed urticaria in the whole body (Fig. 5), in combination with weakness, sleep disturbances, and muscle and joints pain. Antinuclear antibody (ANA) testing with HEp-2 cells revealed a titer of 1:1280, indicating a substantial presence of antinuclear antibodies, which may suggest an autoimmune condition. Additionally, reduced levels of complement component C3 were observed, pointing to a compromised immune system. All other laboratory tests were reported as normal. Based on the clinical symptoms and procedure results, a diagnosis of ASIA syndrome was made. Three years prior, the patient experienced anaphylactic shock following hyaluronidase administration, precluding its use to treat the current immune-mediated reaction.
The patient was given oral cyclosporin A for 6 months with no recurrence observed at 6 months follow-up.
The CARE board therefore emphasizes the importance of evaluating the significance of the titer in the context of the patient’s medical history and other diagnostic findings, as well considering the patient medical history to establish a working diagnosis and adapted treatment plan.
Case Study 3
The patient received 1 mL of HA dermal filler injections in the suborbicularis oculi fat and deep medial cheek areas for midface volumization. A total of 2 months later, the patient was administered a COVID-19 vaccine and, shortly after vaccination, they developed swelling and redness, more pronounced on the right cheek than the left (Fig. 6).
To address these symptoms, the patient was prescribed an oral treatment of prednisolone at a dosage of 20 mg per day for 3 days. This proved to be effective, as the symptoms fully resolved within the treatment period. Following the initial episode, the patient had two subsequent occurrences with milder symptoms at 3 and 5 months. No treatment was advised as the symptoms resolved within 3 days. The patient has been symptom-free since.
The CARE board highlights the potential for postvaccination inflammatory reactions in areas previously treated with dermal fillers and underscores the effectiveness of corticosteroids and watchful waiting in managing such complications as a first line of treatment.
Conclusions
The CARE board believes that there are three main etiological hypotheses underlying LORs: the physicochemical structure of the filler, infection, and an imbalance in the host immune response leading to inflammation. Reactions are likely to be multifactorial, with all three contributing to varying degrees in individual cases.
Many factors can increase the risk of LORs; these can be grouped into patient-, product-, and procedure-related factors. Most notably, recent dental interventions, active autoimmune disease, products containing LMW-HA, and poor aseptic technique are associated with development of LORs.
To prevent these reactions, patients should be carefully selected on the basis of a comprehensive medical history taken prior to injection. The procedure must be fully explained to the patient and informed consent should be obtained. Injectors should avoid products that are associated with LORs and ensure that a stringent aseptic technique is maintained throughout the procedure. Following the procedure, the patient should be educated on posttreatment care.
In the event of an LOR, the CARE board have proposed an algorithm to assist in treatment, including a questionnaire used to evaluate the patient’s medical history. The recommended treatment depends on the etiology of the reaction; however, cases should always be evaluated individually and treated within the scope of the injectors clinical practice.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
De Pasquale A, Russa G, Pulvirenti M, Di Rosa L. Hyaluronic acid filler injections for tear-trough deformity: injection technique and high-frequency ultrasound follow-up evaluation. Aesthet Plast Surg. 2013;37(3):587–91.
Surgeons ASoP (2022) Plastic Surgery Statistics Report 2022 [Available from: https://www.plasticsurgery.org/documents/News/Statistics/2022/plastic-surgery-statistics-report-2022.pdf, Assessed in November 2023
Bhojani-Lynch T. Late-onset inflammatory response to hyaluronic acid dermal fillers. Plast Reconstr Surg Glob Open. 2017;5(12): e1532.
Ibrahim O, Overman J, Arndt KA, Dover JS. Filler nodules: inflammatory or infectious? A review of biofilms and their implications on clinical practice. Dermatol Surg. 2018;44(1):53–60.
Heydenrych I, Kapoor KM, De Boulle K, Goodman G, Swift A, Kumar N, Rahman E. A 10-point plan for avoiding hyaluronic acid dermal filler-related complications during facial aesthetic procedures and algorithms for management. Clin Cosmet Investig Dermatol. 2018;11:603–11.
Rohrich RJ, Bartlett EL, Dayan E. Practical approach and safety of hyaluronic acid fillers. Plast Reconstr Surg Glob Open. 2019;7(6): e2172.
Decates TS, Velthuis PJ, Schelke LW, Lardy N, Palou E, Schwartz S, et al. Increased risk of late-onset, immune-mediated, adverse reactions related to dermal fillers in patients bearing HLA-B*08 and DRB1*03 haplotypes. Dermatol Ther. 2021;34(1): e14644.
Convery C, Davies E, Murray G, Walker L. Delayed-onset nodules (DONs) and considering their treatment following use of Hyaluronic acid (HA) fillers. J Clin Aesthet Dermatol. 2021;14(7):E59–67.
Cohen JL, Hicks J, Nogueira A, Lane V, Andriopoulos B. Postmarket safety surveillance of delayed complications for recent FDA-approved hyaluronic acid dermal fillers. Dermatol Surg. 2022;48(2):220–4.
Kroumpouzos G, Harris S, Bhargava S, Wortsman X. Complications of fillers in the lips and perioral area: prevention, assessment, and management focusing on ultrasound guidance. J Plast Reconstr Aesthet Surg. 2023;84:656–69.
Artzi O, Cohen JL, Dover JS, Suwanchinda A, Pavicic T, Landau M, et al. Delayed inflammatory reactions to hyaluronic acid fillers: a literature review and proposed treatment algorithm. Clin Cosmet Investig Dermatol. 2020;13:371–8.
Funt DK. Treatment of delayed-onset inflammatory reactions to hyaluronic acid filler: an algorithmic approach. Plast Reconstr Surg Glob Open. 2022;10(6): e4362.
Urdiales-Gálvez F, Delgado NE, Figueiredo V, Lajo-Plaza JV, Mira M, Moreno A, et al. Treatment of soft tissue filler complications: expert consensus recommendations. Aesthet Plast Surg. 2018;42(2):498–510.
Philipp-Dormston WG, Goodman GJ, De Boulle K, Swift A, Delorenzi C, Jones D, et al. Global approaches to the prevention and management of delayed-onset adverse reactions with hyaluronic acid-based fillers. Plast Reconstr Surg Glob Open. 2020;8(4): e2730.
Snozzi P, van Loghem JAJ. Complication management following rejuvenation procedures with hyaluronic acid fillers-an algorithm-based approach. Plast Reconstr Surg Glob Open. 2018;6(12): e2061.
Lee JM, Kim YJ. Foreign body granulomas after the use of dermal fillers: pathophysiology, clinical appearance, histologic features, and treatment. Arch Plast Surg. 2015;42(2):232–9.
Kokoska RE, Lima AM, Kingsley MM. Review of delayed reactions to 15 hyaluronic acid fillers. Dermatol Surg. 2022;48(7):752–7.
Goodman GJ, McDonald CB, Lim A, Porter CE, Deva AK, Magnusson M, et al. Making sense of late tissue nodules associated with hyaluronic acid injections. Aesthet Surg J. 2023;43(6):NP438–48.
Baeva LF, Lyle DB, Rios M, Langone JJ, Lightfoote MM. Different molecular weight hyaluronic acid effects on human macrophage interleukin 1β production. J Biomed Mater Res Part A. 2014;102(2):305–14.
Lyle DB, Breger JC, Baeva LF, Shallcross JC, Durfor CN, Wang NS, Langone JJ. Low molecular weight hyaluronic acid effects on murine macrophage nitric oxide production. J Biomed Mater Res Part A. 2010;94A(3):893–904.
Baeva LF, Sarkar Das S, Hitchins VM. Bacterial endotoxin detection in hyaluronic acid-based medical devices. J Biomed Mater Res B Appl Biomater. 2017;105(5):1210–5.
Saththianathan M, Johani K, Taylor A, Hu H, Vickery K, Callan P, Deva AK. The role of bacterial biofilm in adverse soft-tissue filler reactions: a combined laboratory and clinical study. Plast Reconstr Surg. 2017;139(3):613–21.
Beer K, Avelar R. Relationship between delayed reactions to dermal fillers and biofilms: facts and considerations. Dermatol Surg. 2014;40(11):1175–9.
Lee BM, Park SJ, Noh I, Kim CH. The effects of the molecular weights of hyaluronic acid on the immune responses. Biomater Res. 2021;25(1):27.
Moran M, Nieto-Lopez F, Rueda-Carrasco J. Lipoteichoic acid and molecular weight of hyaluronic acid could explain the late inflammatory response trigger by hyaluronic acid fillers. J Cosmet Dermatol. 2022;21(11):5610–3.
Lee W, Shah-Desai S, Rho NK, Cho J. Etiology of delayed inflammatory reaction induced by hyaluronic acid filler. Arch Plast Surg. 2024;51(1):20–6.
Decates T, Kadouch J, Velthuis P, Rustemeyer T. Immediate nor delayed type hypersensitivity plays a role in late inflammatory reactions after hyaluronic acid filler injections. Clin Cosmet Investig Dermatol. 2021;14:581–9.
Decates TS, Budding AE, Velthuis PJ, Bachour Y, Wolters LW, Schelke LW, et al. Bacterial contamination is involved in the etiology of soft-tissue filler, late-onset, inflammatory adverse events. Plast Reconstr Surg. 2023;151(5):971–8.
Marusza W, Olszanski R, Sierdzinski J, Szyller K, Ostrowski T, Gruber-Miazga J, Netsvyetayeva I. The impact of lifestyle upon the probability of late bacterial infection after soft-tissue filler augmentation. Infect Drug Resistance. 2019;12:855–63.
Marusza W, Olszanski R, Sierdzinski J, Ostrowski T, Szyller K, Mlynarczyk G, Netsvyetayeva I. Treatment of late bacterial infections resulting from soft-tissue filler injections. Infect Drug Resistance. 2019;12:469–80.
Owczarczyk-Saczonek A, Zdanowska N, Wygonowska E, Placek W. The immunogenicity of hyaluronic fillers and its consequences. Clin Cosmet Investig Dermatol. 2021;14:921–34.
Constantine RS, Constantine FC, Rohrich RJ. The ever-changing role of biofilms in plastic surgery. Plast Reconstr Surg. 2014;133(6):865e–72e.
Chang LM, Maheshwari P, Werth S, Schaffer L, Head SR, Kovarik C, Werth VP. Identification and molecular analysis of glycosaminoglycans in cutaneous lupus erythematosus and dermatomyositis. J Histochem Cytochem. 2011;59(3):336–45.
Cylwik B, Gruszewska E, Gindzienska-Sieskiewicz E, Kowal-Bielecka O, Chrostek L. Comparison of hyaluronic acid in patients with rheumatoid arthritis, systemic sclerosis and systemic lupus erythematosus. Biochemia Medica. 2021;31(2): 020701.
Mathieu S, Maillet B, Ristori J-M, Soubrier M. Rheumatoid arthritis induced by labial injection of hyaluronic acid: just a coincidence? Joint Bone Spine. 2007;74(5):512–3.
Wang JY, Roehrl MH. Glycosaminoglycans are a potential cause of rheumatoid arthritis. Proc Natl Acad Sci USA. 2002;99(22):14362–7.
Ledon JA, Savas JA, Yang S, Franca K, Camacho I, Nouri K. Inflammatory nodules following soft tissue filler use: a review of causative agents, pathology and treatment options. Am J Clin Dermatol. 2013;14(5):401–11.
Jones DH, Fitzgerald R, Cox SE, Butterwick K, Murad MH, Humphrey S, et al. Preventing and treating adverse events of injectable fillers: evidence-based recommendations from the American Society for dermatologic surgery multidisciplinary task force. Dermatol Surg. 2021;47(2):214–26.
Turkmani MG, De Boulle K, Philipp-Dormston WG. Delayed hypersensitivity reaction to hyaluronic acid dermal filler following influenza-like illness. Clin Cosmet Investig Dermatol. 2019;12:277–83.
Munavalli GG, Guthridge R, Knutsen-Larson S, Brodsky A, Matthew E, Landau M. COVID-19/SARS-CoV-2 virus spike protein-related delayed inflammatory reaction to hyaluronic acid dermal fillers: a challenging clinical conundrum in diagnosis and treatment. Arch Dermatol Res. 2022;314(1):1–15.
Munavalli GG, Knutsen-Larson S, Lupo MP, Geronemus RG. Oral angiotensin-converting enzyme inhibitors for treatment of delayed inflammatory reaction to dermal hyaluronic acid fillers following COVID-19 vaccination-a model for inhibition of angiotensin II-induced cutaneous inflammation. JAAD Case Rep. 2021;10:63–8.
Witt J, Hooper D, Munavalli GG. Delayed inflammatory reaction to hyaluronic acid filler following Shingrix and Fluzone vaccines treated with lisinopril. JAAD Case Rep. 2022;23:133–5.
Cavallieri FA, de Almeida Balassiano LK, de Bastos JT, da Fontoura GHM, de Almeida AT. Persistent, intermitent delayed swelling PIDS: late adverse reaction to hyaluronic acid fillers. CEP. 2017;22440:040.
Mariani E, Lisignoli G, Borzì RM, Pulsatelli L. Biomaterials: foreign bodies or tuners for the immune response? Int J Mol Sci. 2019;20(3):636.
Lowe NJ, Maxwell CA, Lowe P, Duickb MG, Shah K. Hyaluronic acid skin fillers: adverse reactions and skin testing. J Am Acad Dermatol. 2001;45(6):930–3.
Chung KL, Convery C, Ejikeme I, Ghanem AM. A Systematic review of the literature of delayed inflammatory reactions after hyaluronic acid filler injection to estimate the incidence of delayed type hypersensitivity reaction. Aesthet Surg J. 2020;40(5):NP286–300.
Cohen Tervaert JW, Martinez-Lavin M, Jara LJ, Halpert G, Watad A, Amital H, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) in 2023. Autoimmun Rev. 2023;22(5): 103287.
Alijotas-Reig J, Fernández-Figueras MT, Puig L. Late-onset inflammatory adverse reactions related to soft tissue filler injections. Clin Rev Allergy Immunol. 2013;45(1):97–108.
Lafaille P, Benedetto A. Fillers: contraindications, side effects and precautions. J Cutan Aesthet Surg. 2010;3(1):16–9.
Descamps V, Landry J, Francès C, Marinho E, Ratziu V, Chosidow O. Facial cosmetic filler injections as possible target for systemic sarcoidosis in patients treated with interferon for chronic hepatitis c: two cases. Dermatology. 2008;217(1):81–4.
Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Plastic Surg Nurs. 2015;35(1):13–32.
De Boulle K, Heydenrych I. Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol. 2015;8:205–14.
Rivers JK. Incidence and treatment of delayed-onset nodules after VYC filler injections to 2139 patients at a single Canadian clinic. J Cosmet Dermatol. 2022;21(6):2379–86.
Beleznay K, Carruthers JDA, Carruthers A, Mummert ME, Humphrey S. Delayed-onset nodules secondary to a smooth cohesive 20 mg/mL hyaluronic acid filler: cause and management. Dermatol Surg. 2015;41(8):929–39.
Høiby N, Bjarnsholt T, Moser C, Bassi GL, Coenye T, Donelli G, et al. ESCMID∗ guideline for the diagnosis and treatment of biofilm infections 2014. ESCMID 2014 Guideline for the diagnosis and treatment of biofilm infections. 2015 ;21:S1–S25
Victorino AA, Silva MG, Shinjo SK. High levels of serum hyaluronic acid in adults with dermatomyositis. Acta Reumatologica Portuguesa. 2015;40(2):150–5.
Alijotas-Reig J, Esteve-Valverde E, Gil-Aliberas N, Garcia-Gimenez V. Autoimmune/inflammatory syndrome induced by adjuvants-ASIA-related to biomaterials: analysis of 45 cases and comprehensive review of the literature. Immunol Res. 2018;66(1):120–40.
Pieretti G, Rafaniello C, Fraenza F, Donniacuo M, Cuomo R, Lanzano G, et al. Hyaluronic acid-based fillers in patients with autoimmune inflammatory diseases. J Cosmet Dermatol. 2023;22(9):2420–3.
Creadore A, Watchmaker J, Maymone MBC, Pappas L, Vashi NA, Lam C. Cosmetic treatment in patients with autoimmune connective tissue diseases: best practices for patients with lupus erythematosus. J Am Acad Dermatol. 2020;83(2):343–63.
Sharad J. Hyaluronic acid filler injection for localized scleroderma - case report and review of literature on filler injections for localized scleroderma. Clin Cosmet Investig Dermatol. 2022;15:1627–37.
Adamczyk K, Rusyan E, Franek E. Safety of aesthetic medicine procedures in patients with autoimmune thyroid disease: a literature review. Medicina. 2022;58(1):30.
Rork JF, Rashighi M, Harris JE. Understanding autoimmunity of vitiligo and alopecia areata. Curr Opin Pediatr. 2016;28(4):463–9.
Wu Y, An H-T, Hsu N-J, Loh D, Malaithong L, Park J-Y, et al. Expert recommendations on the assessment and management of complications due to hyaluronic acid soft tissue filler injections in Asians. J Cosmet Dermatol. 2022;21(9):3779–86.
Cavallo I, Sivori F, Truglio M, De Maio F, Lucantoni F, Cardinali G, et al. Skin dysbiosis and Cutibacterium acnes biofilm in inflammatory acne lesions of adolescents. Sci Rep. 2022;12(1):21104.
Azzouz S, Lanoue D, Champagne K, Genest G. Delayed hypersensitivity reaction to cosmetic filler following two COVID-19 vaccinations and infection. Allergy Asthma Clin Immunol. 2023;19(1):31.
Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Critical Care (London, England). 2020;24(1):422.
Corduff N, Juniarti L, Lim TS, Lin F, Mariwalla K, Pavicic T, et al. Current practices in hyaluronic acid dermal filler treatment in Asia Pacific and practical approaches to achieving safe and natural-looking results. Clin Cosmet Investig Dermatol. 2022;15:1213–23.
Sadeghpour M, Quatrano NA, Bonati LM, Arndt KA, Dover JS, Kaminer MS. Delayed-onset nodules to differentially crosslinked hyaluronic acids: comparative incidence and risk assessment. Dermatol Surg. 2019;45(8):1085–94.
Nayfeh T, Shah S, Malandris K, Amin M, Abd-Rabu R, Seisa MO, et al. A systematic review supporting the american society for dermatologic surgery guidelines on the prevention and treatment of adverse events of injectable fillers. Dermatol Surg. 2021;47(2):227–34.
Trinh LN, McGuigan KC, Gupta A. Delayed complications following dermal filler for tear trough augmentation: a systematic review. Facial Plastic Surg FPS. 2022;38(3):250–9.
Murray G, Convery C, Walker L, Davies E. Guideline for the safe use of hyaluronidase in aesthetic medicine, including modified high-dose protocol. J Clin Aesthet Dermatol. 2021;14(8):E69–75.
Di Minno A, Frigerio B, Spadarella G, Ravani A, Sansaro D, Amato M, et al. Old and new oral anticoagulants: Food, herbal medicines and drug interactions. Blood Rev. 2017;31(4):193–203.
Alam M, Cohen JL, Petersen B, Schlessinger DI, Weil A, Iyengar S, Poon E. Association of different surgical sterile prep solutions with infection risk after cutaneous surgery of the head and neck. JAMA Dermatol. 2017;153(8):830–1.
Dumville J, McFarlane E, Edwards P, Lipp A, Holmes A. Preoperative skin antiseptics for preventing surgical wound infections after clean surgery. Cochrane Database of Syst Rev. 2013. https://doi.org/10.1002/14651858.CD003949.pub3.
Tanner J, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database of Syst Rev. 2021. https://doi.org/10.1002/14651858.CD004122.pub5.
Cutteridge J, Garrido P, Staniland T, Lathan R, Smith G, Chetter I. The clinical effectiveness of waxing or epilation compared with other methods of hair removal in reducing the incidence of surgical site infections: a protocol for a systematic review. 2023;3(1):52-5
Modarressi A, Nizet C, Lombardi T. Granulomas and nongranulomatous nodules after filler injection: Different complications require different treatments. J Plastic Reconstr Aesthet Surg JPRAS. 2020;73(11):2010–5.
Kroumpouzos G, Treacy P. Hyaluronidase for dermal filler complications: review of applications and dosage recommendations. JMIR Dermatol. 2024;7: e50403.
Acknowledgements
We are grateful to Stefania Ballarini and Caroline Gauche for the organization and moderation of CARE board meetings. We also thank Bárbara Magalhães for their literature search and manuscript development assistance and Ines Moreno Pons for their insights on treatment plans.
Medical Writing, Editorial, or Other Assistance
Medical Writing assistance was provided by Lauren Owens from Infinity Communications.
Funding
The authors received no financial support for the research, authorship, and publication of this article. Teoxane SA funded the journal’s Rapid Service and Open Access fees for this publication.
Author information
Authors and Affiliations
Contributions
Drs Wioletta Baranska-Rybak, José V Lajo-Plaza, Lee Walker, and Navid Alizadeh attended CARE board meetings and offered opinions and recommendations to be included in the manuscript. Drs Wioletta Baranska-Rybak, José V Lajo-Plaza, Lee Walker, and Navid Alizadeh also reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
Professor Barańska-Rybak serves as a medical consultant for Teoxane SA in Poland. Dr Lajo-Plaza serves as a medical consultant for Teoxane SA in Spain. Dr Walker acts as a global key opinion leader for Teoxane SA and medical education consultant for Revance Therapeutics Inc. Dr Alizadeh serves as a medical consultant for Teoxane SA and for Relife (Menarini Group company, Italy) in Switzerland.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. All individuals depicted in published photographs provided informed consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Baranska-Rybak, W., Lajo-Plaza, J.V., Walker, L. et al. Late-Onset Reactions after Hyaluronic Acid Dermal Fillers: A Consensus Recommendation on Etiology, Prevention and Management. Dermatol Ther (Heidelb) (2024). https://doi.org/10.1007/s13555-024-01202-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13555-024-01202-3