Abstract
Objective
Botulinum toxin serotype A (BoNT/A) is widely used for minimal invasive aesthetic treatments. Different brands of BoNT/A exhibit structural variations. The aim of this study was to compare the duration and efficacy of various BoNT/A brands available in Thailand for reducing bite force and treating wrinkles.
Methods
Fifty participants were randomly assigned to one of five groups, with each group receiving a different BoNT/A brand, namely, incobotulinumtoxinA (IncoA), onabotulinumtoxinA (OnaA), abobotulinumtoxinA (AboA), letibotulinumtoxinA (LetiA), and prabotulinumtoxinA (PraboA). BoNT/A was administered to the masseter muscle and the upper face. Bite force was measured before injection and at 2, 4, 8, 12, 16, 20, and 24 weeks post-injection. Evaluation scores for wrinkle improvement were assessed after the treatment.
Results
The most significant reduction in bite force occurred between 2 and 4 weeks post-injection. PraboA demonstrated the most substantial reduction in bite force, while IncoA had the least effect. However, the percentage of bite force reduction did not exhibit statistical significance between BoNT/A types. Additionally, the reduction in bite force for all BoNT/A types was reversed at 4 months post-injection. More than half of the participants experienced improvement beyond 16 weeks.
Conclusions
The structural differences among BoNT/A brands did not significantly affect the longevity and efficacy of bite force reduction and wrinkle treatment.
Trial Registration
ClinicalTrials.gov identifier: TCTR20211205001 (registered 4 Dec 2021).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
Botulinum toxin serotype A (BoNT/A) is widely used for minimal invasive aesthetic treatments, and the different brands currently available exhibit structural variations. |
We assessed the efficacy of different BoNT/A formulations available in the marke, with a specific emphasis on their capacity to reduce bite force and treat wrinkles. |
What was learned from this study? |
A significant decrease in bite force was noted within 2–4 weeks post-injection, with the PraboA formulation exhibiting the most substantial impact, although no statistically significant differences were observed among the different BoNT/A formulations. |
The reduction in bite force was temporary, returning to baseline levels 4 months post-injection. Nonetheless, over half of the participants maintained improved bite force beyond the 16-week period. |
Despite the structural variations among the BoNT/A formulations, these differences did not result in significant differences in the duration or effectiveness of reducing bite force and treating wrinkles. |
Introduction
Botulinum toxin (BoNT) is a protein produced by the bacterium Clostridium botulinum that induces muscle paralysis by inhibiting the release of acetylcholine at neuromuscular junctions [1]. Despite its high toxicity, BoNT is used for medical purposes due to its selectivity, lack of cytotoxicity, and limited diffusion within the body. Among its various serotypes, BoNT type A (BoNT/A) is the most commonly employed for medical applications [1]. BoNT takes effect within a few days after injection, causing a lasting blockage of acetylcholine release. However, the inhibition of muscle function is temporary, as new nerve terminals sprout and restore muscular activity within a few months [1].
BoNT/A is a complex protein composed of a neurotoxin and a complexing protein. The neurotoxin consists of a heavy and a light chain, while the complexing protein is encoded by two genes, nonhemagglutinin and hemagglutinin [2, 3]. The complexing protein is believed to stabilize the neurotoxin's biological activity, promote its adherence to muscle tissue, and/or restrict its diffusion from the target area due to the molecule’s size [4]. However, the BoNT/A which contains complexing protein might increase risk of botulinum toxin treatment failure due to neutralizing antibody formation [5, 6].
BoNT/A is utilized for various aesthetic indications, such as treating horizontal forehead lines, glabella frown lines, crow's feet, and masseter muscle hypertrophy [1]. Injection of BoNT/A into the masseter muscle reduces bite force and leads to muscle atrophy, which can be desired for aesthetic reasons, temporomandibular disorder treatment, and/or the reduction of bruxism and occlusal wear [7,8,9]. Adverse effects associated with therapeutic doses of BoNT/A injections in the masseter muscle are generally mild and transient, with most side effects resolving within 1 week [10].
The bite force is generated by three jaw-closing masticatory muscles, with the masseter muscle making the most significant contribution, accounting for approximately 43% of the intrinsic strength [11]. Even after considering craniofacial dimensions and facial morphology, the width of the masseter muscle has the greatest impact on bite force [12].
The use of BoNT/A has been steadily growing due to its minimally invasive nature, with new brands emerging annually [13]. Each brand’s production process and BoNT/A formulation differ, with different complexing proteins [14, 15]. In Thailand, the Thai Food and Drug Administration (FDA) has approved and allowed various types of BoNT/A to be commercially available, including incobotulinumtoxinA (IncoA), onabotulinumtoxinA (OnaA), abobotulinumtoxinA (AboA), letibotulinumtoxinA (LetiA), and prabotulinumtoxinA (PraboA) [16]. While OnaA, AboA, LetiA, and PraboA contain both neurotoxin and complexing protein, the toxin complexes vary among brands [14]. OnaA, LetiA, and PraboA have a toxin complex with a relatively higher molecular weight (900 kDa), while AboA has a medium-sized toxin complex with a molecular weight of 500 kDa [14]. IncoA is unique as it contains only the 150-kDa neurotoxin, achieved through an extensive purification process that removes the complexing protein from the botulinum toxin complex [14, 17].
Taking into account the unclear role of the complexing protein in BoNT/A’s potency enhancement, we have measured the maximal voluntary bite force (MVBF) and evaluated the outcomes from injecting different BoNT/A products into the upper face using an equivalent dosage and similar injection technique. The primary objective was to observe the efficacy, longevity, and safety of using different types of BoNT/A for injections into the masseter muscle and muscles for facial expression.
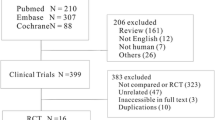
Methods
Study Design
This was a single-center prospective study involving 50 healthy male and female participants aged 25–45 years. Inclusion criteria required that participants had not received BoNT injections within the 6 months prior to the project’s commencement. Exclusion criteria included a history of stomatognathic pain, facial, or neck surgery; chronic diseases (e.g., thyroid disease, systemic lupus erythematosus, immunodeficiency disorders); or any conditions that could potentially interfere with study outcomes.
Baseline Assessment
Before the intervention, participants were photographed with various facial expressions (neutral, smile, frown, and raised eyebrows). MVBF was measured using a bite force registration apparatus (HBM Norge AS, Trollåsen, Norway). To ensure safety, a rubber cover was placed on the metal fork to prevent direct biting on metal. The fork was inserted between the first and second molars, and participants bit with MVBF three times, with 15-s intervals between bites. The highest value in Newtons (N) was recorded. This measurement was performed on both sides of the midline.
Group Allocation
All participants were randomly divided into five groups, with the participants in each group receiving a different Thai FDA-approved and commercially available BoNT/A type: IncoA (Xeomin; Merz, Frankfurt am Main, Germany), OnaA (Botox; Allergan, Irvine, CA, USA), AboA (Dysport; Galderma, Zug, Switzerland), PraboA (Nabota; Daewoong Pharmaceutical, Seoul, South Korea), and LetiA (Hugel; Hugel Inc., Seoul, South Korea). Each participant received 100 U of BoNT/A, with the exception of participants in the AboA group, who received 250 U of BoNT/A, accounting for the equivalence dosage difference of 2.5: 1 [18]. Vials containing 100 U of BoNT/A were mixed with 1 ml of isotonic saline solution, while vials containing 500 U of AboA were mixed with 2 ml of isotonic saline solution. Injections included 30 U of BoNT/A or 75 U of AboA on each side of the masseter muscle, 10 U of BoNT/A or 25 U of AboA in the orbicularis oculi muscle for crow's feet treatment, and 10 U of BoNT/A or 25 U of AboA in the corrugator supercilii and procerus muscles. The remaining 10 U of BoNT/A or 25 U of AboA was diluted 2.5-fold and injected into the frontalis muscle.
Post-intervention Assessments
Immediately following the injection, participants were asked to evaluate their pain scores on a 10-point scale. At subsequent visits, participants were photographed again with and without facial expressions, and MVBF was recorded at 2, 4, 8, 12, 16, 20, and 24 weeks post-intervention. Participants assessed their wrinkle improvement at each visit using a 5-point scale (0 = worse, 1 = little improvement or not improved, 2 = fairly improved, 3 = improved, 4 = very improved). Board-certified dermatologists, who were double-blinded to avoid bias, assessed the wrinkle improvement from standard photographs at the end of the study. Side effects, including pain, erythema, swelling, and facial asymmetry, were documented.
Statistical Analysis
Demographic data were analyzed descriptively. Bite force data, patient evaluation scores, and physician evaluation scores were subjected to statistical analyses between baseline and various assessment time points using unpaired-sample t-tests and repeated-measures analysis of variance (ANOVA) for normal distribution data, and Mann–Whitney test and Kruskal–Wallis test for non-normal distribution. Data were analyzed using GraphPad Prism version 9.2.0 (GraphPad Software, San Diego, CA, USA), and P-values < 0.05 were considered to be statistically significant.
Ethical Considerations
The study was approved by the Ethics Committee of the Siriraj Institutional Review Board (No. SI746/2021). Written informed consent was obtained for the publication and use of all patients’ images prior to their enrollment in the study. The study adhered to the Helsinki Declaration of 1964 and its subsequent amendments. It was registered on ClinicalTrials.gov and assigned NCT number TCTR20211205001.
Results
Participant Population and Characteristics
A total of 50 volunteers were initially recruited, consisting of 39 women and 11 men, with a mean age of 36.1 years (Table 1). Of the initial participants, 48 individuals (96%) successfully completed the study protocol and were included in the final analysis. Two participants from the AboA and LetiA subgroups were withdrawn from the study due to their inability to attend the last follow-up session. It should be noted that all participants were of Thai ethnicity and had Fitzpatrick skin types III to IV.
Bite Force
Since each participant had a unique MVBF baseline value, the bite force reduction was reported as a ratio (Fig. 1). The bite force reduction persisted for up to 16 weeks post-injection in participants in the AboA and PraboA groups (Fig. 1d, e), while the participants in the other BoNT/A groups exhibited a reduction lasting 12 weeks. Notably, although the MVBF reduction persisted longer for AboA and PraboA, the bite force reduction at 16 weeks was significantly less than at 12 weeks. Our results indicate that MVBF minimally declined immediately after injection and returned to baseline 24 weeks after the intervention (Fig. 1a). In contrast, the bite force in the AboA and LetiA groups fell immediately after injection (Fig. 1d, f). We also compared the bite force from each BoNT/A brand to each other, as illustrated in Fig. 1g; however, no statistically significant differences in the effect on bite force were detected. The details of bite force reduction for each type of BoNT/A are shown in supplemental table (Table S1).
Bite force reduction compared to baseline. The y-axis represents the proportion of bite force relative to the baseline (pre-treatment), and the x-axis shows the duration of elapsed time post-toxin injection. Asterisks indicate statistically significant differences between baseline and post-treatment measurements at *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, and ****P ≤ 0.0001
Subjects and Physician Assessment Scale
A quartile scale was employed to assess both participants’ satisfaction and physicians’ evaluations. The participants’ assessment scale is presented in Fig. 2, while the physicians’ assessment scale is depicted in Fig. 3. Figure 4 displays images of participants raising their eyebrows.
Based on the evaluation scores from both participants and physicians, > 50% of the participants experienced improvement for up to 20 weeks with every type of BoNT/A, with the exception of the AboA group, which exhibited a duration of 16 weeks. Moreover, dermatologists noted that more than 50% of the participants with every type of BoNT/A continued experienced the effects of BoNT/A for wrinkle treatment over 20 weeks.
Pain Score and Adverse Effect
Pain scores on a 10-point scale was not significantly difference between each type of BoNT/A. The mean pain score for IncoA, OnaA, AboA, PraboA, and LetiA was 2.4, 3.7, 2.6, 2.9, and 3.5, respectively. Bruise and asymmetry of eyebrows were found during the study for IncoA, OnaA, and AboA.
Discussion
The utilization of botulinum toxin (BoNT) injections for aesthetic purposes has witnessed a surge in popularity in recent years, with numerous pharmaceutical companies offering various brands of BoNT/A. These brands exhibit distinct structures of complexing proteins or, in some cases, lack such proteins [19,20,21]. The role of complexing proteins has been a subject of discussion for over a decade, as they are believed to facilitate muscle tissue adherence and may influence the diffusion of BoNT/A from the target area [4].
While injection of the AboA and PraboA brands resulted in significant reductions in MVBF (MVBF) that persisted longer than injection with the other brands, the reduction in bite force at 16 weeks was significantly higher at the 16-week post-injection time point compared to 12 weeks. One possible explanation is that the masseter muscle regained normal function, while the reduced bite force compared to baseline could be attributed to the disuse atrophy effect of BoNT/A. Consequently, it would appear that the longevity of BoNT/A injections for masseter hypertrophy does not significantly differ among the different BoNT/A types. However, the initiation of the effect may vary.
Although reduction in MVBF between each type of BoNT/A was not statistically significant, there were notable distinctions. PraboA achieved a 45% reduction in bite force, while IncoA achieved a 35% reduction. These findings align with previous studies on the efficacy of BoNT/A for facial wrinkle treatment, where a similar pattern was observed [20,21,22]. The peak in MVBF reduction was typically observed at 2–4 weeks after the intervention, consistent with previous studies showing that the effects of BoNT/A peaked during this timeframe and lasted approximately 12 weeks after injection [23, 24].
Intriguingly, the physician evaluation and the participants’ assessments scale for wrinkle evaluation did not reveal differences between the various types of BoNT/A, as more than half of the participant still experienced the effect of the BoNT/A for up to 16–20 weeks after the treatment.
In terms of the pain score and adverse events associated with BoNT/A injection, no significant differences among the various BoNT/A types were reported in this study. Pain scores may primarily result from the needle puncture through the skin, rather than being related to the type of BoNT/A used. Adverse events, such as bruises and asymmetrical eyebrows, were less likely to be attributed to the type of BoNT/A and were more likely to be associated with the injection site. Importantly, no severe complications were reported during the study, consistent with previous research, indicating the overall safety of BoNT/A for this indication.
However, it is important to acknowledge the study's limitations. The small number of participants in each subgroup limits the depth of exploration into the potency and longevity of each BoNT/A type. A larger cohort undergoing BoNT/A treatment would provide more robust insights. Additionally, the assessment technique for facial wrinkle treatment relied solely on subjective evaluations.
Conclusion
In conclusion, the presence of complexing proteins in BoNT/A brands appears to have minimal impact on the longevity of BoNT/A treatment and its potency for reducing bite force and treating facial wrinkles. The results indicate that the longevity of BoNT/A treatment for facial wrinkles and bite force reduction typically lasts for at least 12 weeks following injection.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pirazzini M, Rossetto O, Eleopra R, Montecucco C. Botulinum neurotoxins: biology, pharmacology, and toxicology. Pharmacol Rev. 2017;69(2):200–35. https://doi.org/10.1124/pr.116.012658.
Brin MF. Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Suppl. 1997;6:S146–68.
Hauser D, Eklund MW, Boquet P, Popoff MR. Organization of the botulinum neurotoxin C1 gene and its associated non-toxic protein genes in Clostridium botulinum C 468. Mol Gen Genet. 1994;243(6):631–40. https://doi.org/10.1007/BF00279572.
Frevert J, Dressler D. Complexing proteins in botulinum toxin type A drugs: a help or a hindrance? Biologics. 2010;4:325–32. https://doi.org/10.2147/BTT.S14902.
Park JY, Corduff N, Frevert J, Wanitphakdeedecha R, Chao YYY. Immunogenicity associated with aesthetic botulinumtoxin a: a survey of Asia-Pacific physicians’ experiences and recommendations. Plast Reconstr Surg Glob Open. 2022;10(4): e4217. https://doi.org/10.1097/GOX.0000000000004217.
Park JY, Sunga O, Wanitphakdeedecha R, Frevert J. Neurotoxin impurities: a review of threats to efficacy. Plast Reconstr Surg Glob Open. 2020;8(1): e2627. https://doi.org/10.1097/GOX.0000000000002627.
Agren M, Sahin C, Pettersson M. The effect of botulinum toxin injections on bruxism: a systematic review. J Oral Rehabil. 2020;47(3):395–402. https://doi.org/10.1111/joor.12914.
Wanitphakdeedecha R, Ungaksornpairote C, Kaewkes A, Sathaworawong A, Lektrakul N, Manuskiatti W. The efficacy of two formulations of botulinum toxin type A for masseter reduction: a split-face comparison study. J Dermatol Treat. 2017;28(5):443–6. https://doi.org/10.1080/09546634.2016.1263382.
Wanitphakdeedecha R, Ungaksornpairote C, Kaewkes A, Sathaworawong A, Vanadurongwan B, Lektrakul N. A pilot study comparing the efficacy of two formulations of botulinum toxin type A for muscular calves contouring. J Cosmet Dermatol. 2018;17(6):984–90. https://doi.org/10.1111/jocd.12787.
Lee WK, Bae JH, Hu KS, Kato T, Kim ST. Anatomical recommendations for safe botulinum toxin injection into temporalis muscle: a simplified reproducible approach. Surg Radiol Anat. 2017;39(3):263–9. https://doi.org/10.1007/s00276-016-1739-1.
Weijs WA, Hillen B. Cross-sectional areas and estimated intrinsic strength of the human jaw muscles. Acta Morphol Neerl Scand. 1985;23(3):267–74.
Raadsheer MC, van Eijden TM, van Ginkel FC, Prahl-Andersen B. Contribution of jaw muscle size and craniofacial morphology to human bite force magnitude. J Dent Res. 1999;78(1):31–42. https://doi.org/10.1177/00220345990780010301.
American Society of Plastic Surgeons. Plastic surgery statistics report 2020. https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-report-2020.pdf. Accessed 6 Aug 2021.
Choudhury S, Baker MR, Chatterjee S, Kumar H. Botulinum toxin: an update on pharmacology and newer products in development. Toxins (Basel). 2021;13(1):58. https://doi.org/10.3390/toxins13010058.
Chung SK, Kwan YS, Kyoung MM, Yeong DA. Method for production of botulinum toxin. https://patents.google.com/patent/WO2015016462A1/en. Accessed 1 Apr 2023.
Thai Food and Drug administration. https://www.fda.moph.go.th/Pages/HomeP_D2.aspx. Accessed 1 Apr 2023.
Kerscher M, Wanitphakdeedecha R, Trindade de Almeida A, Maas C, Frevert J. IncobotulinumtoxinA: a highly purified and precisely manufactured botulinum neurotoxin type A. J Drugs Dermatol. 2019;18(1):52–7.
Scaglione F. Conversion ratio between Botox(R), Dysport(R), and Xeomin(R) in clinical practice. Toxins (Basel). 2016;8(3):65. https://doi.org/10.3390/toxins8030065.
Hanna E, Pon K. Updates on botulinum neurotoxins in dermatology. Am J Clin Dermatol. 2020;21(2):157–62. https://doi.org/10.1007/s40257-019-00482-2.
Rzany BJ, et al. A multicenter, randomized, double-blind, placebo-controlled, single-dose, phase III, non-inferiority study comparing prabotulinumtoxinA and onabotulinumtoxinA for the treatment of moderate to severe glabellar lines in adult patients. Aesthet Surg J. 2020;40(4):413–29. https://doi.org/10.1093/asj/sjz110.
Walker TJ, Dayan SH. Comparison and overview of currently available neurotoxins. J Clin Aesthet Dermatol. 2014;7(2):31–9.
Yoo KH, Park SJ, Han HS, Won CH, Lee YW, Kim BJ. Randomized, double-blind, active-controlled, multicentre, phase III clinical trial with two stages to assess the safety and efficacy of letibotulinum toxin a vs. onabotulinum toxin a for subjects with moderate to severe crow’s feet. J Eur Acad Dermatol Venereol. 2021;35(7):1587–94. https://doi.org/10.1111/jdv.17217.
Agren M, et al. Duration of bite force reduction following a single injection of botulinum toxin in the masseter muscle bilaterally: a one-year non-randomized trial. J Oral Rehabil. 2023;50(5):343–50. https://doi.org/10.1111/joor.13434.
Sitnikova V, Kamppi A, Teronen O, Kemppainen P. Effect of botulinum toxin injection on EMG activity and bite force in masticatory muscle disorder: a randomized clinical trial. Toxins (Basel). 2022;14(8):545. https://doi.org/10.3390/toxins14080545.
Acknowledgements
The authors extend their heartfelt gratitude to Dr. Pitchaya Maneeprasopchoke, Ms. Onjira Meethong, Ms. Pornsuk Yamlexnoi, Mr. Thitiwat Junpunyawong, Ms. Apichaya Jutaphonrakul, and Ms. Navinee Wongmanee for their dedicated assistance in participant recruitment and database management. The authors also extend their sincere thanks to the participants whose valuable contributions made this publication possible.
Medical Writing and Editorial Assistance
The authors did not receive any medical writing or editorial assistance.
Funding
This research, including open access fee, was generously supported by the Faculty of Medicine at Siriraj Hospital, Mahidol University, Thailand.
Author information
Authors and Affiliations
Contributions
Conceptualization: Rungsima Wanitphakdeedecha. Data curation: Surachet Sirisuthivoranunt, Supisara Wongdama, and Phumithep Phumariyapong. Formal analysis: Surachet Sirisuthivoranunt. Investigation: Surachet Sirisuthivoranunt, Supisara Wongdama, and Phumithep Phumariyapong. Methodology: Rungsima Wanitphakdeedecha, Mattias Pettersson, and Margin Agren. Supervision: Rungsima Wanitphakdeedecha. Writing–original draft preparation: Surachet Sirisuthivoranunt and Rungsima Wanitphakdeedecha. Critical review and editing: all authors.
Corresponding author
Ethics declarations
Conflict of Interest
All authors, including Surachet Sirisuthivoranunt, Supisara Wongdama, Phumithep Phumariyapong, Ya-Nin Nokdhes, Panwadee Thongjaroensirikul, Thanya Techapichetvanich, Mattias Pettersson, Martin Agren, and Rungsima Wanitphakdeedecha, affirm that there are no conflicts of interest pertaining to any aspect of this study.
Ethical Approval
The study was approved by the Ethics Committee of the Siriraj Institutional Review Board (No. SI746/2021). Written informed consent was obtained for the publication and use of all patients’ images prior to their enrollment in the study. The study adhered to the Helsinki Declaration of 1964 and its subsequent amendments. It was registered on ClinicalTrials.gov and assigned NCT number TCTR20211205001.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sirisuthivoranunt, S., Wongdama, S., Phumariyapong, P. et al. Comparative Study on the Duration and Efficacy of Various Botulinum Toxin Type A Injections for Reducing Masseteric Muscle Bite Force and Treating Facial Wrinkles. Dermatol Ther (Heidelb) 14, 1315–1325 (2024). https://doi.org/10.1007/s13555-024-01177-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01177-1