Abstract
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin condition that affects both children and adults. AD increases the risk of developing comorbidities like asthma, allergic rhinitis and food allergies. AD patients face difficulties, including itching, lack of effective treatments, lack of funding and discomfort in seeking a diagnosis or treatment. This study aims to identify the main barriers and opportunities to improve the experience of patients with AD and provide high-quality care.
Methods
Patients, caregivers and healthcare professionals were recruited from the Dermatology Department at Puerta de Hierro Majadahonda University Hospital (Madrid, Spain). Interviews with patients, caregivers and professionals were performed. Participants used storyboards to depict their preferred scenarios for improving healthcare interactions and create a Patient Journey Map.
Results
A total of 15 participants were included in the study. Early symptoms of AD were commonly described as undefined stages. As symptoms worsened, patients and caregivers expressed uncertainty and frustration. Patients became concerned about AD after their first serious flare and started experiencing intense itching, eczema, wounds, shedding or asthma. Topical corticosteroids were used to manage flares, but their effectiveness diminished over time, causing further frustration. Because of the ineffectiveness of their initial treatments, dermatologists observed that patients tended to downplay symptoms and how they affected their quality of life. The specialized treatment of severe AD significantly changed patients' emotional states. Despite AD's chronic nature, patients strived to enjoy remission periods and cope with flares. Psychological and emotional support was crucial for patients and caregivers, a need addressed by the Patients' School initiative at HUPHM hospital.
Conclusion
The severity of AD has a profound impact on patients' lives. Patient and caregiver emotional and social needs can be met by adequate communication, access to effective treatments and comprehensive psychological support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Atopic dermatitis (AD) is a chronic inflammatory skin disorder with a prevalence of 5–15% in children and 2–10% in adults, characterized by recurrent eczematous lesions, intense itching and discomfort. |
We aim to identify key barriers and opportunities for enhancing the experience of patients with AD by incorporating their knowledge, by enabling their active participation in research, innovation and change and by creating a Patient Journey Map to improve care quality. |
Emphasis on the pre-diagnosis phase and specialized care in dermatology and psychology are crucial for addressing emotional difficulties, improving quality of life and optimizing treatment outcomes, particularly for pediatric patients. |
Effective communication regarding the chronic nature of the condition, availability of effective treatments and comprehensive psychological support is important for the emotional and social well-being of patients and caregivers. |
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disorder, also known as atopic eczema, affecting children and adults [1]. AD is a heterogeneous disease characterized by recurrent eczematous lesions, intense itching and discomfort, symptoms that can be confused with those from other skin diseases, increasing underdiagnosis [1, 2]. Onset usually occurs in childhood, although it can manifest at any point in life. Although it is difficult to determine the prevalence of AD, it is estimated to be 5–15% in children and 2–10% in adults [3, 4], as AD persists in the adult age in approximately half of those diagnosed during childhood [5]. AD can be chronic for many years or show a relapsing-remitting nature [6]. In Spain, the estimated prevalence of severe AD is 0.1%, approximately 10% of patients with diagnosed AD [7].
Causes of AD range from genetic to environmental factors, being also associated with an increased risk of comorbidities, such as asthma, allergic rhinitis, and food allergies [8]. Environmental elements, such as diet, sleep, allergens, pollution, and humidity, significantly influence the progression of AD, given the skin's constant interaction with its surroundings. These exposomes can induce stress in the skin, thereby triggering flares and worsening the patient's overall health-related quality of life (QoL) [9, 10]. The complexity and subjectivity of disease severity measurement and the decreased treatment effectiveness are known barriers to AD management, having a high psychosocial impact on patients and caregivers [8].
Patients with AD experience multiple difficulties such as itching, lack of effective treatments and information, lack of funding for treatments and discomfort in searching for a diagnosis or treatment with different specialists. Moreover, patients’ health, QoL, sleep, productivity and interpersonal relationships are negatively impacted [11]. Similarly, children experience an impact on daily activities, school, leisure and bullying [12]. In this context, AD poses a clear burden on mental and psychological health, with nearly half of the patients with severe AD reporting anxiety or moderate-to-severe depression [13]. Understanding the patient’s experience and pain points is essential for better adherence to treatments, patient-centered prescribing, higher quality of care and higher QoL, but studies focused on the patient’s experience are limited [12, 14, 15], as most studies focus on the clinical and therapeutical process [2, 16, 17].
The objective of this research is to pinpoint the primary barriers and opportunities that could enhance the experience of patients with AD. By integrating patients' insights into the creation of solutions, we enable their active involvement as contributors in research, innovation and transformation. Our ultimate goal is to construct a Patient Journey Map, a tool designed to elevate the patient experience and ensure the delivery of high-quality care for patients with AD.
Methods
Participant Selection
To gather diverse experiences of AD, patients, caregivers and healthcare professionals were recruited for the interviews. The inclusion criteria comprised adults with moderate-to-severe AD who were being followed up at the Dermatology Department at Puerta de Hierro Majadahonda University (HUPHM) Hospital (Madrid, Spain), caregivers for the pediatric patients and healthcare professionals from Dermatology, Pharmacy, Primary Care and Psychology units. Underaged patients or participants who, because of their physical or cognitive characteristics, could not conduct an interview orally online were excluded. All healthcare professionals were recruited at this hospital. The sample size was determined based on the saturation principle for qualitative research [18].
Ethical Considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki and its amendments. The study was approved by the Ethics Committee of the Puerta de Hierro Majadahonda University (HUPHM) Hospital (Madrid, Spain) with code PI 145/22. All participants provided written informed consent before the interviews and after receiving information about the study.
Study Design
Interviews
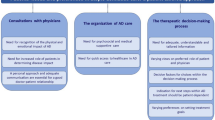
Interviews were conducted with open-ended questions and in-depth questions without interference from the interviewer to gather subjective information and perceptions. To guide the interviews, five dimensions were considered (Fig. 1). Patients, caregivers and healthcare professionals were interviewed for a period of 30–45 min. Interviews were done remotely using Google Meet and were recorded and transcribed for analysis.
Patient Journey Map
Based on the information collected during the in-depth interviews, a Patient Journey Map was developed to illustrate the different stages a patient goes through, capturing emotions, interactions with healthcare services and experiences (Fig. 2). This Patient Journey Map was structured representing key experiences and recommendations over the duration of AD, as previously described [19, 20], focused on the five dimensions described in Fig. 1.
Workshop
A workshop was conducted in person in a room at the HUPHM Hospital in November 2022. A series of visual resources, such as Patient Journey Maps, barrier and opportunity cards and storyboard panels, was provided to the participants, and notes were taken on the key insights generated. The workshop consisted of three activities: the Patient Journey Map, barrier detection and exploration of opportunities and the storyboard. For the Patient Journey Map, patients, caregivers and professionals explored different stages of the AD experience with the care process. Participants identified key pain points and barriers and validated the initial draft generated with the information obtained from the interviews. A discussion was then held among patients, caregivers and professionals regarding potential barriers and opportunities for improvement. In the final step, the participants used storyboards to narrate situations illustrating the identified barriers and depict their preferred scenarios for improving healthcare interactions.
Results
A total of 15 participants were enrolled. Seven patients and two caregivers participated in the study. The median age of the adult patients was 38 years, and 67% were male (Table 1). Healthcare professionals participating in the study were three dermatologists, one clinical psychologist of the Dermatology Department itself with previous experience in AD patients, one primary care physician and one professional from the Hospital Pharmacy, who participated only in the workshop.
Pre-Diagnosis and Referral to Specialized Care
First Symptoms
Early AD symptoms were frequently described as an undefined stage, without specific moments or events that defined them. Patients often became aware of AD through their parents and had lived with these symptoms since childhood, perceiving them as a normal part of their lives, while only recalling scratches and minor injuries. Caregivers generally attributed the first symptoms to skin dryness or irritation, and even if they sought advice from primary care physicians, the symptoms were attributed to allergies or diaper dermatitis.
As symptoms continued to worsen, despite receiving a first diagnosis and instructions, patients and caregivers expressed uncertainty and frustration (Fig. 3). Usually, caregivers would seek alternative care or visit the emergency room (ER) when symptoms worsened.
First Flares
Several patients had been aware of their disease since childhood, but they began to connect AD with their lives after the first severe flare, which was often the moment when they had their first AD consultation. The first flares were described as sudden and drastic episodes, sometimes occurring in response to significant events such as injuries, diseases or during the COVID-19 pandemic. As a result of flares, patients’ lives were disrupted by intense itching, eczema, wounds, shedding or asthma, which made daily tasks such as sleeping or showering particularly challenging and demanding (Fig. 3).
In many cases, the first flare led to social withdrawal resulting from the observed symptoms and the associated stigma. Patients reported feeling uncomfortable scratching in public as a result of misconceptions such as contagiousness or reduction of the condition to mere itching. Similarly, caregivers pointed out that dealing with inquiries and misunderstandings about AD was challenging in the scholarly environment.
Diagnosis
Typically, patients were aware of their condition but did not seek medical attention until the condition worsened, only seeking medical attention after their first severe flare. There were many cases in which patients lacked accurate or complete diagnoses. One of the primary pain points experienced by patients during their first flares was the lack of information about the chronic nature of AD. Other barriers are presented in Fig. 3. Only after patients gained access to specialized care did they receive substantial information regarding the severity of AD and its chronicity.
First Treatments
In several cases, after AD was diagnosed, patients began applying topical corticosteroids during severe flares to manage them. Patients reported that these treatments became less effective over time, with no ability to break the cycles of remission and flares, causing frustration and emotional distress. A major pain point for patients was the lack of adequate follow-up and support, perceiving a lack of involvement from the primary care professionals. Patients claimed that the use of creams was prescribed without consideration of symptom progression or explanation of potential adverse reactions, which also led to a financial burden. As a result, patients resorted to alternative strategies, including homemade remedies, which proved to be ineffective, leading to more frustration (Fig. 3). In several cases, patients were not referred to specialists until several treatment alternatives had failed, but by this time, AD was already severe.
Coordination and Communication Between Primary and Specialized Care
The primary point of referral for patients with AD was primary care, followed by ER and other specialties such as allergology. Dermatologists reported that patients often arrived with preexisting diagnoses and were referred because of the challenge of treating AD. Remote consultations were noted as a useful tool by primary care physicians, as they allowed dermatologists to evaluate lesions through images and decide whether the patient should be referred. Dermatologists, however, found these consultations less useful because of the reliance on images and time constraints. All in all, professionals stressed the importance of collaboration between primary care and dermatology departments (Fig. 3). Furthermore, dermatologists indicated that ER referrals were becoming more frequent because of the ineffectiveness of treatment and severe flares.
Diagnosis Determination
The diagnosis of AD was primarily based on clinical evaluation; however, similar symptoms in other conditions could complicate the process, making it difficult to differentiate AD from other dermatitis. The presence of eczema and itching, along with other factors such as specific locations and medical history, all helped to determine the diagnosis, although other tests such as biopsies may be performed if necessary. Dermatologists believed that active listening was crucial for diagnosis, as they paid close attention to the language used in explicit statements. For instance, patients could recall when symptoms first appeared and mention related conditions such as asthma or food allergies. According to patients and caregivers, dermatologists played an active role for patients, allowing them to share their experiences. This is in stark contrast to what patients and caregivers indicated for other specialties.
Treatment and Flare-Remission Cycles
Expectations
Dermatologists observed that patients often experienced a profound sense of resignation because of the ineffectiveness of their initial treatments, thereby influencing their threshold of well-being through treatments because of the lack of effectiveness in the past. It was also observed that patients tended to downplay symptoms and how they affected their QoL.
The patients’ major concern in treatment was the elimination of itching and eczema; however, they also stressed the importance of living a normal life without the burden of social stigma associated with AD (Fig. 4). Eczema reduction or disappearance was highlighted as a positive outcome, along with an increase in happiness and a better body perception.
Application and Adherence to Biologic Treatments
Biologic treatments were limited to patients with severe AD. In the opinion of some healthcare professionals, this situation left some needs unmet, particularly for patients with moderate AD. In the experience of patients and caregivers, biologic treatments were a transformative experience that exceeded expectations. Symptoms, especially itching, were reported to be relieved rapidly, allowing patients to resume their daily activities. The effectiveness of these treatments was described as miraculous by some patients, even when the use of these treatments presented challenges.
Injections administered by patients or caregivers autonomously were described as overwhelming and unpleasant. Even though patients acknowledged that there is no pain associated with injections, the act of self-administration held a symbolic significance. Despite the apprehension associated with syringes, patients and their caregivers emphasized the positive impact on their QoL. Compared to pens, pre-filled syringes were preferred by patients because they were more convenient and caused less discomfort and pain. Additionally, prior instructions and supervised practice at the hospital eased the implementation of home-based treatments as well as dermatologic and psychologic follow-ups (Fig. 4).
Other Treatments
Oral and topical treatments were reported to be common among patients with severe AD. Patients indicated that these treatments had some limitations relating to adverse reactions as well as their own circumstances, such as conflicts with recommended limits on sun exposure. Healthcare professionals reported that patients were less likely to adhere to oral treatments since daily medication reminders were challenging for the patients. Patients also highlighted these challenges, particularly when taking medication interrupted their daily activities.
On top of rapid tolerance development, patients also continued to hold negative views regarding the use of corticosteroids, attributing side effects such as weight gain or rheumatic pain to their use. Additionally, patients found it difficult to use creams, which resulted in a lack of adherence (Fig. 4). As a result, patients indicated they preferred sprays, which they considered convenient and did not require a large amount of material for application.
Flare Control
Healthcare professionals reported an improvement in their ability to convey hope and confidence to patients following the introduction of new treatments (Fig. 4). Both patients and caregivers expressed satisfaction with the level of communication and personalized treatment approaches.
Emotional Experiences and Psychologic Support
A substantial number of patients with severe AD reported experiencing significant changes in their emotional state after accessing specialized care. Despite the decreasing intensity and duration of flares, social stigma and stereotypes about hygiene and contagion were common concerns, as they claimed to always be in a state of tension and exhaustion.
During stable periods, patients did not require psychologic support; however, this support was essential during flares (Fig. 4). Anyhow, patients noted that although AD is chronic, they tried to enjoy the remission periods and deal with flares as best as they could.
Parallel to this, healthcare professionals insisted on the importance of addressing the chronic nature of AD and patients’ expectations regarding treatment effectiveness (Fig. 4).
Patient Experience in Flare Control Within Specialized Care
Flare experiences within specialized care were significantly different from those in other healthcare settings. Patients described past flares as emotionally distressing, losing contact with healthcare professionals and resorting to alternative treatments as relevant pain points. In specialized care, however, the approach ensured that the patient and the professionals were in constant contact, employing different strategies to prevent flares. As a result of this situation, the patients felt empowered with autonomy and knowledge to make decisions about their treatment and daily activities and were better prepared to deal with their symptoms (Fig. 4).
Follow-Up
Organization
Despite the lack of established protocols for follow-ups, healthcare professionals highlighted the progress that was being made towards standardization. However, patients and caregivers often felt isolated and without support outside of specialized care, which emphasized the importance of consistent follow-up.
Several factors determined the frequency and type of follow-up, including the severity and type of treatment. For example, biologic treatments required frequent visits, and, in some cases, specific treatments required regular blood tests (Fig. 5).
Communication Between Patients and Healthcare Professionals
In the opinion of patients and caregivers, communication with healthcare professionals was seamless and consistent. In general, they were pleased with the level of availability and support provided. However, some patients noted coordination issues among specialists (Fig. 5). Dermatologists observed that some patients did not always discuss their experiences with their physicians (Fig. 5). Patients, however, believed that they had the right to decide whether to communicate side effects with their dermatologist, sharing them only when they exceeded the threshold for tolerance.
Emotional Support of Patients and Caregivers
Throughout the course of their journey, patients expressed a strong need for emotional and psychologic support. The HUPHM Hospital established the Patients’ School initiative to address this need, as a space for patients and healthcare professionals to gather and share their experiences. The Patients’ School provided an opportunity to explore issues and experiences that could not be adequately addressed during regular consultations.
According to patients, the Patients’ School provided them with emotional support and assisted them in addressing discouraging expectations, improving their QoL. This view was shared by healthcare professionals, who also emphasized the possibility of explaining technical aspects of AD through this space. Caregivers, on the other hand, reported that managing AD was challenging (Fig. 5).
Patient Journey Map
Based on the analysis of the data obtained in this study, we were able to identify the barriers, limitations, preferences and motivations encountered by patients during their care process, as well as opportunities for improving their experience. Figure 6 presents the various stages of the journey that patients with AD go through, highlighting the patient experience, their contact with healthcare professionals and their needs.
Discussion
The burden of AD is multi-dimensional and associated with a variety of factors [10, 21]. Guidelines are limited [22] and differ in therapeutic recommendations [23]. The physical and care dimensions of healthcare are often considered in clinical settings, while the emotional, social, and symbolic and cultural dimensions are overlooked, although the impact of AD on mental health and QoL has been previously described [24,25,26,27]. To our knowledge, there is no previous study analyzing the complete patient journey in AD. Because of this limited perspective, treatment adherence and patient engagement are poorly understood. All these dimensions must be considered to gain a deeper understanding of how patients experience AD. Consequently, healthcare providers will be able to offer a more holistic and patient-centered approach, resulting in improved patient outcomes, enhanced satisfaction and a better overall healthcare experience. In this context, we developed a Patient Journey Map considering the stages of pre-diagnosis and diagnosis, treatment and flare-remission cycles and follow-up. The Patient Journey Map presented in this study underscores the principal challenges and potential improvements that could improve the patient experience, thereby ensuring the provision of comprehensive, high-quality care. This tool is designed to incorporate the perspectives and concerns of patients with AD, thereby ensuring that all dimensions of care are patient-centered and responsive to their specific needs and experiences.
The pre-diagnosis phase is crucial in improving the care and management of patients with AD. Early recognition of symptoms, accurate diagnoses and timely interventions are necessary for better outcomes and improved QoL [28]. Additionally, healthcare professionals should be aware of the impact of first flares on patients’ lives, including the stigma and difficulties in social and educational settings [29], a present concern among patients and caregivers. Emotional difficulties were expressed by patients and caregivers, closely related to factors such as the absence of a cure and the emotional and social burden of AD. Acknowledging the experiences faced by patients and caregivers can enhance communication, provide accurate information and develop appropriate treatment plans.
Effective communication is also essential, as one major barrier detected was inadequate communication regarding the chronic nature of AD. Patients and caregivers should be informed that effective treatments do exist, but there is no cure for AD, and symptoms will vary over time. Similarly, adequate information about treatments and support is vital to avoid patient dissatisfaction and exploration of ineffective or potentially harmful treatments, as the effectiveness of treatments is a significant concern for patients. Moreover, barriers to accessing specialized care should be removed to facilitate an efficient referral process and ensure timely and appropriate management of AD. Despite some challenges in diagnosis, assessment and treatments identified in previous studies [30], the effectiveness of new treatments raised new expectations among patients, caregivers and healthcare professionals.
Our study found a contrast in active listening practices during consultations in dermatology compared to other healthcare areas. Patients and caregivers often encountered a lack of engagement in achieving accurate diagnoses, leading to concerns and misconceptions about AD. These findings emphasize the importance of promoting active listening and improving communication to enhance patient-centered care in dermatology.
Emotional difficulties faced by patients and caregivers can be mitigated through specialized care considering the emotional and social aspects of AD. The QoL of patients with AD depends not only on symptom disappearance but also on how AD affects their daily lives. Specialized care provides access to a wide variety of treatments, transforming patients’ emotional experience and perception of treatment efficacy. Exposome factors can exacerbate AD and impact the patients’ QoL [10, 31]. These factors can also affect the perceived efficacy of AD treatments. Therefore, it is crucial to consider these elements when developing comprehensive AD management strategies, highlighting the importance of considering holistic well-being and the need for specialized care in dermatology and psychology to address AD and improve treatment outcomes, especially with pediatric patients [32].
The goal of AD treatments is to eliminate the symptoms and prevent future flares or complications, improving patients’ QoL. For mild AD, moisturization and intermittent use of topical treatments are recommended, while for moderate-to-severe severe AD, systemic treatments are usually required [2, 23, 33, 34], as is the case for the study participants. These systemic treatments have varying degrees of effectiveness and can be associated with adverse events that require close monitoring according to the participants and in line with previous reports [35, 36]. For biologic treatments, correct education is key to support self-administration of injections in patients. We observed that the application of injections presents challenges for some patients, even if the treatments are highly effective. On the other hand, oral and topical treatments are perceived as less effective by the patients and present adherence challenges as previously described in other studies [37, 38]. Patients’ actual and past experiences are important to facilitate treatment adherence and improved effectiveness. Recent advances in communication and AD control offer a more optimistic outlook and decreased sense of helplessness among patients who claimed to be very satisfied with the effectiveness of biologics [39].
The organization of follow-ups can be challenging and needs to be individualized, considering treatment types, comorbidities, emotional well-being and other specific characteristics before designing an effective follow-up plan. Patients value follow-ups, but there are still coordination issues that need to be addressed. Special attention should be put on underaged patients and their caregivers [40], as adequate support is challenging, and it will be crucial for adherence during adolescence and should be adapted to their own point of view. Patient’s autonomy plays an important role in their active involvement during follow-ups. Initiatives such as the Patients’ School at Puerta de Hierro Hospital provide emotional and psychologic support for patients.
This study presents several limitations. The experience of healthcare professionals could bias the answers provided during the interviews, as they may fail to highlight certain information that has been presented in other studies or is relevant from the patient’s perspective. Since patients were recruited at the hospital and interviews were conducted online, their representation was also limited. The study was qualitative, and therefore no statistical analyses were performed. Although we tried to minimize our interference by asking open-ended questions, the interviewer may have influenced the answers. Lastly, as the study was performed in one hospital, it may be difficult to extrapolate the results to other locations.
Conclusion
Severe AD has a profound impact on patients’ lives. Adequate communication about the chronic nature of the disease, access to effective treatments and comprehensive psychologic support are essential in addressing the emotional and social needs of patients and caregivers. Further qualitative and quantitative follow-up studies could expand the knowledge base by including more patients and performing telephone interviews. Moreover, since the Patient Journey Map is a dynamic process that changes over time as patients and healthcare professionals interact, it should be evaluated and adapted in the future. By addressing these challenges, it is possible to improve the overall experience and well-being of patients with severe AD.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. 2018;4(1):1. https://doi.org/10.1038/s41572-018-0001-z.
Arkwright PD, Motala C, Subramanian H, Spergel J, Schneider LC, Wollenberg A, et al. Management of difficult-to-treat atopic dermatitis. J Allergy Clin Immunol Pract. 2013;1(2):142–51. https://doi.org/10.1016/j.jaip.2012.09.002.
Kowalska-Oledzka E, Czarnecka M, Baran A. Epidemiology of atopic dermatitis in Europe. J Drug Assess. 2019;8(1):126–8. https://doi.org/10.1080/21556660.2019.1619570.
Barbarot S, Auziere S, Gadkari A, Girolomoni G, Puig L, Simpson EL, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy. 2018;73(6):1284–93. https://doi.org/10.1111/all.13401.
Mortz CG, Andersen KE, Dellgren C, Barington T, Bindslev-Jensen C. Atopic dermatitis from adolescence to adulthood in the TOACS cohort: prevalence, persistence and comorbidities. Allergy. 2015;70(7):836–45. https://doi.org/10.1111/all.12619.
Garmhausen D, Hagemann T, Bieber T, Dimitriou I, Fimmers R, Diepgen T, et al. Characterization of different courses of atopic dermatitis in adolescent and adult patients. Allergy. 2013;68(4):498–506. https://doi.org/10.1111/all.12112.
Sicras-Mainar A, Navarro-Artieda R, Armario-Hita JC. Severe atopic dermatitis in Spain: a real-life observational study. Ther Clin Risk Manag. 2019;15:1393–401. https://doi.org/10.2147/TCRM.S226456.
Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–60. https://doi.org/10.1016/S0140-6736(20)31286-1.
Stefanovic N, Flohr C, Irvine AD. The exposome in atopic dermatitis. Allergy. 2020;75(1):63–74. https://doi.org/10.1111/all.13946.
Passeron T, Zouboulis CC, Tan J, Andersen ML, Katta R, Lyu X, et al. Adult skin acute stress responses to short-term environmental and internal aggression from exposome factors. J Eur Acad Dermatol Venereol. 2021;35(10):1963–75. https://doi.org/10.1111/jdv.17432.
Girolomoni G, Luger T, Nosbaum A, Gruben D, Romero W, Llamado LJ, et al. The economic and psychosocial comorbidity burden among adults with moderate-to-severe atopic dermatitis in Europe: analysis of a cross-sectional survey. Dermatol Ther (Heidelb). 2021;11(1):117–30. https://doi.org/10.1007/s13555-020-00459-8.
Stingeni L, Belloni Fortina A, Baiardini I, Hansel K, Moretti D, Cipriani F. Atopic dermatitis and patient perspectives: insights of bullying at school and career discrimination at work. J Asthma Allergy. 2021;14:919–28. https://doi.org/10.2147/JAA.S317009.
Luger T, Romero WA, Gruben D, Smith TW, Cha A, Neary MP. Clinical and humanistic burden of atopic dermatitis in Europe: analyses of the national health and wellness survey. Dermatol Ther (Heidelb). 2022;12(4):949–69. https://doi.org/10.1007/s13555-022-00700-6.
Ortiz de Frutos FJ, Torrelo A, de Lucas R, Gonzalez MA, Alomar A, Vera A, et al. Patient perspectives on triggers, adherence to medical recommendations, and disease control in atopic dermatitis: the DATOP study. Actas Dermosifiliogr. 2014;105(5):487–96. https://doi.org/10.1016/j.ad.2014.01.004.
Armario-Hita JC, Artime E, Vidal-Vilar N, Huete T, Diaz-Cerezo S, Moro RM, et al. Patient-reported outcome measures in real-world atopic dermatitis studies in spain: a systematic review. Actas Dermosifiliogr. 2022;113(7):685–704. https://doi.org/10.1016/j.ad.2022.01.025.
Cuervo MM, Sanclemente G, Barrera LM. Clinical and sociodemographic features and quality of life in patients with atopic dermatitis who attended dermatology teaching clinics in Medellin, Antioquia and its metropolitan area. Biomedica. 2021;41(4):676–91. https://doi.org/10.7705/biomedica.5978.
Silverberg JI, Thyssen JP, Fahrbach K, Mickle K, Cappelleri JC, Romero W, et al. Comparative efficacy and safety of systemic therapies used in moderate-to-severe atopic dermatitis: a systematic literature review and network meta-analysis. J Eur Acad Dermatol Venereol. 2021;35(9):1797–810. https://doi.org/10.1111/jdv.17351.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. https://doi.org/10.1007/s11135-017-0574-8.
Hoffmann-Vold AM, Bendstrup E, Dimitroulas T, Hesselstrand R, Morais A, Peltomaa R, et al. Identifying unmet needs in SSc-ILD by semi-qualitative in-depth interviews. Rheumatology (Oxford). 2021;60(12):5601–9. https://doi.org/10.1093/rheumatology/keab154.
Davies EL, Bulto LN, Walsh A, Pollock D, Langton VM, Laing RE, et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review. J Adv Nurs. 2023;79(1):83–100. https://doi.org/10.1111/jan.15479.
Elsawi R, Dainty K, Smith Begolka W, Barta K, Butler L, Capozza K, et al. The multidimensional burden of atopic dermatitis among adults: results from a large National survey. JAMA Dermatol. 2022;158(8):887–92. https://doi.org/10.1001/jamadermatol.2022.1906.
Sidbury R, Kodama S. Atopic dermatitis guidelines: Diagnosis, systemic therapy, and adjunctive care. Clin Dermatol. 2018;36(5):648–52. https://doi.org/10.1016/j.clindermatol.2018.05.008.
Van Halewijn KF, Lahnstein T, Bohnen AM, Van Den Berg PJ, Gma Pasmans S, Je Bindels P, et al. Recommendations for emollients, bathing and topical corticosteroids for the treatment of atopic dermatitis: a systematic review of guidelines. Eur J Dermatol. 2022;32(1):113–23. https://doi.org/10.1684/ejd.2022.4197.
Cheng BT, Silverberg JI. Depression and psychological distress in US adults with atopic dermatitis. Ann Allergy Asthma Immunol. 2019;123(2):179–85. https://doi.org/10.1016/j.anai.2019.06.002.
Sato Y, Hiyoshi A, Melinder C, Suzuki C, Montgomery S. Asthma and atopic diseases in adolescence and antidepressant medication in middle age. J Health Psychol. 2018;23(6):853–9. https://doi.org/10.1177/1359105316660181.
Marron SE, Cebrian-Rodriguez J, Alcalde-Herrero VM, Garcia-Latasa de Aranibar FJ, Tomas-Aragones L. Psychosocial impact of atopic dermatitis in adults: a qualitative study. Actas Dermosifiliogr (Engl Ed). 2020;111(6):513–7. https://doi.org/10.1016/j.ad.2019.03.018.
Xie QW, Dai X, Tang X, Chan CHY, Chan CLW. Risk of mental disorders in children and adolescents with atopic dermatitis: a systematic review and meta-analysis. Front Psychol. 2019;10:1773. https://doi.org/10.3389/fpsyg.2019.01773.
Oliveira C, Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29(3):250–8. https://doi.org/10.1684/ejd.2019.3557.
Chernyshov PV. Stigmatization and self-perception in children with atopic dermatitis. Clin Cosmet Investig Dermatol. 2016;9:159–66. https://doi.org/10.2147/CCID.S91263.
Artime E, Serra E, Mert C, Diaz-Cerezo S, Huete T, Hernandez-Subira I, et al. Real-world treatment patterns, resource use and costs in adult patients with atopic dermatitis receiving systemic treatment: derma-atopic study in Spain. Actas Dermosifiliogr. 2023;114(1):T9–18. https://doi.org/10.1016/j.ad.2022.08.025.
Stefanovic N, Irvine AD, Flohr C. The role of the environment and exposome in atopic dermatitis. Curr Treat Options Allergy. 2021;8(3):222–41. https://doi.org/10.1007/s40521-021-00289-9.
Xu X, van Galen LS, Koh MJA, Bajpai R, Thng S, Yew YW, et al. Factors influencing quality of life in children with atopic dermatitis and their caregivers: a cross-sectional study. Sci Rep. 2019;9(1):15990. https://doi.org/10.1038/s41598-019-51129-5.
Mayba JN, Gooderham MJ. Review of atopic dermatitis and topical therapies. J Cutan Med Surg. 2017;21(3):227–36. https://doi.org/10.1177/1203475416685077.
Rodriguez-Le Roy Y, Ficheux AS, Misery L, Brenaut E. Efficacy of topical and systemic treatments for atopic dermatitis on pruritus: a systematic literature review and meta-analysis. Front Med (Lausanne). 2022;9:1079323. https://doi.org/10.3389/fmed.2022.1079323.
Johnson BB, Franco AI, Beck LA, Prezzano JC. Treatment-resistant atopic dermatitis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:181–92. https://doi.org/10.2147/CCID.S163814.
Siegels D, Heratizadeh A, Abraham S, Binnmyr J, Brockow K, Irvine AD, et al. Systemic treatments in the management of atopic dermatitis: a systematic review and meta-analysis. Allergy. 2021;76(4):1053–76. https://doi.org/10.1111/all.14631.
Frantz T, Wright EG, Balogh EA, Cline A, Adler-Neal AL, Feldman SR. Topical and oral therapies for childhood atopic dermatitis and plaque psoriasis. Children (Basel). 2019. https://doi.org/10.3390/children6110125.
Puar N, Chovatiya R, Paller AS. New treatments in atopic dermatitis. Ann Allergy Asthma Immunol. 2021;126(1):21–31. https://doi.org/10.1016/j.anai.2020.08.016.
Zhou S, Qi F, Gong Y, Zhang J, Zhu B. Biological therapies for atopic dermatitis: a systematic review. Dermatology. 2021;237(4):542–52. https://doi.org/10.1159/000514535.
Kobusiewicz AK, Tarkowski B, Kaszuba A, Lesiak A, Narbutt J, Zalewska-Janowska A. The relationship between atopic dermatitis and atopic itch in children and the psychosocial functioning of their mothers: a cross-sectional study. Front Med (Lausanne). 2023;10:1066495. https://doi.org/10.3389/fmed.2023.1066495.
Acknowledgements
We sincerely thank the participants for their generous participation and for providing the insights that were essential to this research. Their invaluable contributions and willingness to share their experiences have been instrumental in the successful completion of this research.
Medical Writing/Editorial Assistance.
Medical writing support was provided by Carmela García Doval at Evidenze Health España S.L.U. during the preparation of this paper. Contribution to the workshop development and in-depth interviews were provided by Carlos Bezos and Claudia Peña from Instituto de Experiencia del Paciente. Responsibility for opinions, conclusions and interpretation of data lies with the authors. The medical writing support was funded by Laboratorios Galderma S.A.
Funding
This study and the Rapid Service Fee were funded by Laboratorios Galderma S.A.
Author information
Authors and Affiliations
Contributions
Conceptualization: Catalina Peña, Olga Isidoro; Methodology: Gastón Roustán, Marta Loro, Ángel Rosell, Belén Menchen, Olga Vicente, Marta Elosua-González, Juan L. Castaño; Supervision: Gastón Roustán, Marta Loro, Ángel Rosell, Belén Menchen, Olga Vicente, Marta Elosua-González, Juan L. Castaño; Formal analysis: Gastón Roustán, Marta Loro, Ángel Rosell, Belén Menchen, Olga Vicente, Marta Elosua-González, Juan L. Castaño; Visualization: Catalina Peña, Olga Isidoro; Writing – review & editing: Gastón Roustán, Marta Loro, Ángel Rosell, Belén Menchen, Olga Vicente, Marta Elosua-González, Juan L. Castaño, Catalina Peña, Olga Isidoro. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Gastón Roustán has been an investigator and/or speaker for Galderma, Pfizer, Abbvie and Sanofi. Marta Loro received speaker honoraria from Sanofi, Novartis, Janssen and Almirall, took part in clinical trials sponsored by Sanofi, Abbvie and Lilly and has received honoraria for her participation in this study. Ángel Rosell received speaker honoraria from Sanofi, Leo Pharma and Abbvie, took part in clinical trials sponsored by Sanofi, Pfizer and Novartis and has received honoraria for his participation in this study. Belén Menchen has participated in conferences, presentations, studies and expert committees organized and funded by Janssen, Leo Pharma, Pfizer, UCB and Novartis. Olga Vicente has received honoraria for her participation in this study and declares no other conflict of interest. Marta Elosua-González has been an investigator and/or speaker for AbbVie, Lilly, Galderma, LEO Pharma, Pfizer, UCB Pharma, and Sanofi Genzyme and has received honoraria for her participation in this study. Juan L. Castaño has received honoraria for his participation in this study and declares no other conflict of interest. Catalina Peña is an employee of Instituto de Experiencia del Paciente. Olga Isidoro is an employee of Laboratorios Galderma.
Ethical Approval
This study was performed in accordance with the ethical standards of the Declaration of Helsinki and its amendments. The study was approved by the Ethics Committee of the Puerta de Hierro Majadahonda University (HUPHM) Hospital (Madrid, Spain) with code PI 145/22. All participants provided written informed consent before the interviews and after receiving information about the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Roustán, G., Loro, M., Rosell, Á. et al. Development of a Patient Journey Map for Improving Patient Experience and Quality of Atopic Dermatitis Care. Dermatol Ther (Heidelb) 14, 505–519 (2024). https://doi.org/10.1007/s13555-024-01100-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01100-8