Abstract
Introduction
Striae distensae (SD), or stretch marks, are a common skin problem having a psychological impact and cosmetic concern, especially for women, in whom the prevalence is higher than in men. This study assessed the efficacy and safety of a single autologous micrografting treatment (AMT®) using Rigenera® technology for the management of SD.
Methods
This single-centre study included 10 healthy women between 24 and 65 years of age, with Fitzpatrick–Goldman skin types I–IV, who had visible SD in glutes/thighs. Each subject acted as their own control. The treatment procedure (microneedling + AMT) and the control procedure (no treatment) were performed on contralateral sides of the glutes/thighs, targeting matched and paired SD. Microneedling was carried out using Dermapen®, equipped with 32 needle heads set at 1.5 mm needle length. The AMT procedure involved extracting biopsies from the mastoid hair zone with a 2.5-mm dermal punch, followed by disaggregation of the biopsies in a physiological saline solution using the Rigeneracons. The disaggregated micrografts were then intradermally injected using 30G 4-mm needles, maintaining a distance of 1 cm between injection points, covering the entire marked treatment region.
Results
In the treated area, at 3 months post-procedure compared to pre-procedure, the following changes were observed, all with statistical significance (P ≤ 0.05): (a) significant reductions in skin roughness (Ra, − 15.9%; Rz, − 22.6%), skin luminance (− 2.0%), and blue-green color distribution (− 10.6%); (b) significant increases in skin microcirculation maximum value (+ 240.1%), skin hydration (+ 71.2%), skin elasticity (+ 216.5%), skin density (+ 34.3%), skin thickness (+ 26.0%), and hypodermis thickness (+ 29.9%). Furthermore, for each of the aforementioned parameters, there was a significantly greater improvement observed with the AMT procedure compared with microneedling at 3 months (all P ≤ 0.05).
Conclusion
The AMT procedure using Rigenera technology resulted in an noticeable improvement in the SD appearance after 3 months in healthy women.
Plain Language Summary
This was a study of the Autologous Micrografting Technology (AMT) procedure for management of SD. Striae distensae (SD) commonly known as stretch marks are visible linear scars on the skin arising from excessive stretching of the skin. They are a very common condition, especially in women, causing cosmetic concern and psychological discomfort. Ten healthy women with SD were included in the study and each subject acted as their own control. Matched and paired SD on contralateral sides of the glutes/thighs were identified for treatment and control. In the area identified for treatment, the skin was initially damaged by microneedling to enhance regeneration, followed by intradermal injection of disaggregated autologous micrografts. The micrografts for the AMT procedure were extracted from the mastoid hair zone and disaggregated in physiological saline solution using the Rigeneracons. In the control area, no treatment was performed. The efficacy of the AMT procedure was assessed at 1 and 3 months post-procedure using several validated methodologies. Three months after the AMT procedure, a significant increase was observed in skin hydration, elasticity, density, and thickness, as well as in hypodermis thickness and microcirculation maximum value compared with pre-procedure in the treated area. There also was a significant reduction in skin roughness, skin luminance, and blue-green color distribution at 3 months in the treated area. For each of these parameters, the improvement observed at 3 months was significantly higher with the AMT procedure compared with only microneedling. We showed that a single AMT procedure using Rigenera technology is useful in the management of SD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Striae distensae (SD) are a common skin condition, especially in women. Treatment options available have varying degrees of efficacy and no single treatment has yet proven effective. |
Autologous Micrografting Technology (AMT) is a regenerative technology that involves use of autologous micrografts to stimulate and enhance the regeneration of an impaired or damaged tissue. |
What was learned from the study? |
Treatment of SD with the AMT procedure using Rigenera technology resulted in a significant increase in skin hydration, elasticity, density, and thickness, as well as in hypodermis thickness and maximum microcirculation value. |
What were the study outcomes/conclusions? |
A single AMT procedure using Rigenera technology is useful in the management of SD. |
Introduction
Striae distensae (SD), commonly referred to as stretch marks, are a common aesthetic problem with a higher prevalence in women than in men [1]. SD are a form of dermal scarring associated with the stretching of the dermis and are mainly localized on the abdomen, breasts, and thighs in adolescents, on the thighs, buttocks, and breasts in women, and on the back in men [2]. Striae rubrae represent the acute stage of SD characterized by linear red plaques, which can be symptomatic, and striae albae signify the chronic stage when the plaques appear faded, atrophic, wrinkled, and hypopigmented [3]. Growth spurts, obesity, pregnancy, steroid application (topical or systemic), and Cushing’s syndrome are some of the known causes for SD, but their exact pathogenesis remains unknown [2, 3]. The rate of occurrence of SD is around 43–88% during pregnancy, 6–86% during puberty, and 43% in obesity [1].
The main aims of SD treatment are symptoms reduction and improvement in appearance [3, 4]. Treatment options for SD include topical agents (such as emollients, over-the-counter cosmeceuticals, silicone gel, tretinoin cream, chemical peels), laser therapy (non-ablative lasers such as pulsed-dye laser and neodymium-doped YAG, as well as traditional ablative lasers such as the carbon dioxide laser), light therapy, collagen injection, laser lipolysis, radiofrequency techniques, platelet-rich plasma injection, and microdermabrasion [3,4,5,6,7]. These treatment options have varying degrees of efficacy, and no single treatment has proven effective thus far [2, 4, 7].
Autologous Micrografting Treatment (AMT) is an innovative, simple, and effective regenerative method that involves the use of autologous micrografts to stimulate and enhance the regeneration of an impaired or damaged tissue [8]. The key strengths of AMT are a good safety profile, non-rejection of the injected micrografts, and specificity in restoring tissues functioning through specific signaling pathways. The Rigenera technology (Regenera Activa Worldwide S.L., Barcelona, Spain, and Human Brain Wave Srl, Torino, Italy) for tissue mechanical disaggregation allows one to obtain autologous micrografts [9, 10], which are enriched in progenitor cells expressing mesenchymal stem cell-like markers and possess strong regenerative potential [8]. The AMT procedure using Rigenera technology has been successfully used worldwide for more than a decade in multiple conditions [11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Additionally, the combination of the AMT and microneedling has previously proven effective in skin rejuvenation.
The aim of this study was to assess the efficacy and safety of a single treatment with the AMT procedure using Rigenera technology for the management of SD in healthy subjects. The hypothesis for the study was that the AMT procedure by modulating the inflammatory and regenerative processes would reduce the depth of the SD and improve the skin texture.
Methods
After an informed written consent, subjects were enrolled in a controlled observational study conducted between November 5, 2022 and February 22, 2023 at Clinical Dermatologica do Arieiro and with the effectiveness evaluation performed at PhD Trials®, Lda (Clinical Center in Lisbon, Portugal. The center is certified under ISO 9001:2015 by an accredited external entity).
The study consisted of four visits: screening treatment, and two follow-up visits at 1 and 3 months post-procedure. Each subject acted as their own control.
Treatment procedure (microneedling + AMT) and control procedure (no treatment) were performed on contralateral sides of the glutes/thighs, targeting matched and paired SD.
Subjects were instructed to avoid the use of non-steroidal anti-inflammatory drugs for at least 24 h before the procedure. They were also advised not to apply hydrating products or exfoliating treatments on the test areas, and not to change their hygiene habits or level of physical activity during the study. Subjects were asked to provide information regarding any aesthetic or specific massage treatments they had undergone before the study, as well as details about past and current concomitant medications and tobacco use.
Changes in current hormonal treatment, if any, and the use of tranquillizers, antidepressants, psychotropic products, diuretics, laxatives or venotonic drugs, anti-allergic, anti-inflammatory treatment, and exfoliating agents or patent medicines containing vitamin A or its derivatives were prohibited during the study.
Treatment Protocol
The treatment procedure consisted of two steps: microneedling to initially damage the skin and enhance regeneration, followed by the AMT procedure. Both steps were performed on the identified SD treatment area, while no treatment was performed on the control SD area. Before the procedure was administered, the SD treatment area was identified and marked with a semi-permanent marker to ensure consistency in the anatomical sites for treatment. Up to three test spots were selected within the marked area.
Microneedling: The marked area was thoroughly washed immediately before the procedure and disinfected with 70% alcohol. A 5% lidocaine cream, a topical anesthetic agent, was applied. After 30 min, microneedling was carried out using Dermapen, equipped with 32 needle heads, set at 1.5 mm needle length. The needles moved perpendicular to the stretched skin to expose the base of the scar, with pressure applied point by point on all SD areas until pinpoint bleeding was observed. Any blood was wiped away with sterile gauze, and the skin was cleaned with sterile saline.
Autologous micrografting: Three biopsy samples for micrografting were obtained from the mastoid hair zone, a highly vascularized and sun-protected area that contains hair follicles rich in skin progenitor cells. The area for biopsies was first cleaned, then marked using a standard dermal marker. It was then cleaned with an antiseptic solution, and hair in that area was shaved using a single-use razor. A 2% lidocaine solution without a vessel constrictor was applied as a peripheral block around the tissue to be biopsied. Biopsies were extracted using a 2.5-mm dermal punch. After the procedure, a blister plaster was applied, and subjects were advised not to wash their hair during the first 24 h and, if necessary, to change the blister plaster the next day.
The biopsies were transferred to the Rigeneracons (Human Brain Wave srl, Turin, Italy) using forceps. Then, 1.5 ml of injectable physiological saline solution was added through the specific Rigeneracons connector using a syringe, ensuring that the biopsies were slightly flooded, but not fully submerged. The Rigeneracons was attached to the Sicurlid and Sicurstick, and loaded into the Rigenera N4SA machine, where it was processed for 2 min. Afterward, the tissue disaggregation cartridge was removed from the tissue system, and the cell suspension was aspirated from the syringe port using a disposable 3-ml syringe (without a needle). The procedure was repeated by injecting another 1.5 ml of injectable physiological saline solution and manually rotating the rotor a few turns. The micrograft solution was completely recovered from the tissue disaggregation cartridge and diluted to a total volume of up to 6 ml with physiological saline solution, ensuring full coverage of the entire S treatment area. The micrograft solution was then intradermally injected into the marked SD treatment area using 30G 4-mm needles, maintaining a consistent 1-cm distance between injection points, covering the whole region.
All procedures were conducted under sterile conditions, and the Rigeneracons, intended for single use, was safely disposed of following local guidelines. Subjects were advised to expect some redness, swelling, and bruising at the treatment sites for 2–3 days. They were instructed not to wash the treated area for 24 h following the procedure, and to avoid applying topical antibiotic cream or exposing the area to sunlight for at least 7 days after the procedure. The subjects were also instructed to use sunscreen before sun exposure.
The study protocol and all relevant study-related documents were approved by an independent ethics committee (PhD Trials Ethics Committee). The study was conducted in accordance with the protocol, the Helsinki Declaration of 1964 and its later amendments, the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use—Good Clinical Practice principles, and applicable Portuguese laws and regulations. Subjects provided written informed consent before the start of the study.
Eligibility Criteria
Healthy women aged 24–65 with Fitzpatrick–Goldman skin type I–IV and visible SD (zone: glutes /thighs; type: striae rubrae or striae albae) were included.
Exclusion Criteria
Fitzpatrick–Goldman skin type V–VI; any dermal/epidermal damage or disorder in the treated area; prior treatment in the area to be treated within 3 months before study; any other surgery in the area to be treated within 9 months before study; keloid or any other type of hypertrophic scar formation or poor wound healing in a previously injured skin area; symptoms of hormonal disorders (such as melasma, chloasma, Cushing’s syndrome [corticosteroids]); active herpes simplex at the time of treatment or three or more episodes of herpes simplex eruption within a year of study; multiple dysplastic nevi in the area to be treated; bleeding disorder or use of anticoagulation medications; immunosuppression/immune deficiency disorders; any form of active cancer at the time of enrolment and during the study or history of skin cancer; significant concurrent illnesses, such as uncontrolled diabetes; active infections in the treated area; tattoo or permanent makeup in the treatment area; mental incompetence; prisoner; active substance or alcohol abuse; heavy smoker; pregnant, intending to become pregnant during the study, less than 3 months postpartum or less than 6 weeks after breastfeeding; or any condition which, in the investigator’s opinion, would make it unsafe for the subject or for the study personnel to treat the subject.
Assessments
Efficacy
Efficacy assessments included the following:
(a) Assessment of skin roughness: 3D images of the skin topography on the SD, inside the striae and in the adjacent skin were obtained by a stereo camera combined with a fringe projection system (AEVA-HE, Eotech, France). The AEVA system is a universal platform for acquisition, analysis, and evaluation of 3D data of the skin. A fringe standard was projected onto the skin and detected by the dual cameras of the optical system. The 3D effect was calculated by the deflection in the fringes and by the stereo-combination of the image projected by both cameras. The standard roughness of stretch marks was defined as Ra, which is the arithmetic mean of the skin surface, and Rz, which is the mean of the five biggest peaks and the five lowest valleys in the image area.
(b) Assessment of skin elasticity: Biomechanical evaluation of the skin on the SD (test and control areas) was performed using a Cutometer® dual MPA 580 (Courage & Khazaka Electronic GmbH, Koln, Germany), equipped with an 8-mm diameter probe. The instrument generated 450 mbars negative pressure allowing the upper layers of the skin to be stretched vertically. The probe was located on an adhesive ring to perfectly immobilize the skin site. The measuring principle was based on the suction method and allowed one to obtain information about the elastic and mechanical properties of the skin surface. The skin was drawn into the aperture of the probe for 3 s and then released. Inside the probe, the penetration depth was determined by a non-contact optical measuring system which consisted of a light source and a light receptor, as well as two prisms facing each other, which projected the light from transmitter to receptor. The light intensity changes as a result of the penetration depth of the skin. The resistance of the skin to the negative pressure (firmness) and its ability to return to its original position (elasticity) were displayed as curves (penetration depth in mm/time) in real time during the measurement. From this recording, the mean (standard deviation [sd]) R2 (Ua/Uf, in %) was calculated, which is the ratio between the ability of returning to the original position and the maximum amplitude. R2 is a standard parameter of elasticity, and the closer the value is to 1 (100%) the more elastic the skin.
(c) Assessment of skin hydration: Hydration content of the skin on the SD (test and control area) was obtained with a Corneometer® CM 825 probe connected to a Cutometer dual MPA 580 or Multi Probe Adapter MPA 6 (Courage + Khazaka Electronic GmbH, Koln, Germany). The assessment was based on the “capacitance” measurement, which allowed the calculation of the water dielectric constant. The measuring probe had an interdigital grid of gold-covered electrodes covered by a low dielectric vitrified material. Because of this probe design, there was no galvanic contact between the electrode and skin surface enabling them to behave as a capacitor. A constant application pressure was applied on the skin surface through a spring system, and measurements were obtained in arbitrary units (AU) as referenced to a factory standard.
(d) Assessment of skin microcirculation: This was measured on the SD (test and control area) using laser Doppler flowmetry (LDF, System LDPM PF5000 with a Periflux laser channel PF 5010, Perimed, Sweden). The tissue was illuminated by a monochromatic laser of 780 nm wavelength which led the light to the skin through an optical fiber. A similar fiber received the reflected and non-reflected light and conveyed it to a photodetector. This technique allowed one to detect the movement of cells in the vessels of the peripheral circulation and microcirculation, with a section between 0.002 and 0.008 mm2. In these vessels, the red blood cells move at speeds from 0.01 to 10 mm/s. The average penetration depth was 1.5 mm, which allowed evaluation of the superficial dermal plexus. The units of measurement were AU or BPU (blood perfusion units), since it is impossible to determine the volume of tissue illuminated, as well as the exact depth.
(e) Assessment of skin color: Skin color on the SD (test and control area) was obtained using a tristimulus color analyzer (Chromameter CR-400, Minolta, Japan) that measured reflected color. The system used high sensitivity photocells filtered to match the Commission Internationale d’Éclairage (CIE) standard. The measuring head contained a high-power xenon arc lamp which provided diffuse illumination from a controlled angle for vertical viewing and constant lighting on the object and detected any slight deviation in the xenon’s light spectral distribution. The system provided data for L* (luminance), a* (red-green) and b* (blue-yellow) color distribution.
(f) Ultrasonography: Ultrasound images of the SD (test and control area) were captured using a Dermascan C® ultrasound system (Cortex technology, Denmark) with a specially modified 20-MHz ultrasound probe. Echo dense tissue was detected, and a B-ultrasound image generated. The subcutaneous fat thickness, the dermis–hypodermis junction length, edema area, SLEB (subepidermal low echogenic band), hypodermal, dermal, and epidermal thickness and density, were calculated from the B-scan image of each area.
(g) Clinical evaluation of stretch marks: The SD (test and control area) were clinically evaluated by the treating dermatologist and scored using the Individual Clinical Stretch marks Score (ICSS) with a score range between 0 to 5 (0 = no stretch marks, 1 to ≤ 2 = slight stretch marks, > 2 to ≤ 3 = moderate stretch marks, > 3 to ≤ 4 = important stretch marks, > 4 to ≤ 5 = severe stretch marks). The ICSS was determined on the basis of the three parameters of color, thickness, and depth. Each parameter was individually scored between 0 to 5 as follows: P1, color of the stretch marks (0 = no stretch marks, 1 = red stretch marks, 2 = red to pinkish stretch marks, 3 = pinkish stretch marks, 4 = pinkish to white stretch marks, 5 = white stretch marks); P2 ,thickness of the stretch marks (0 = no stretch marks, 1 = very thin stretch marks, 2 = thin stretch marks, 3 = moderately thick stretch marks, 4 = thick stretch marks, 5 = very thick stretch marks); P3, depth of the stretch marks (0 = no stretch marks, 1 = not deep stretch marks, 2 = light depth of the stretch marks, 3 = light to moderate depth of the stretch marks, 4 = moderate depth of the stretch marks, 5 = important depth of the stretch marks). ICSS = \(\sum {\left( {{\text{P1}}\, + \,{\text{P2}}\, + \,{\text{P3}}} \right)/3}\) .
(h) Self-assessment by the subjects: The SD (test and control area) were self-evaluated by the subjects and scored between 0 to 4 as follows: 0 = no stretch marks, 1 = slight stretch marks, 2 = moderate stretch marks, 3 = important stretch marks, 4 = severe stretch marks.
(i) Standardized photos for illustrative purposes: Images of the SD (test and control area) were obtained with the fully automated IntelliStudio® photographic stand, equipped with a 50-megapixel digital single-lens reflex camera and a motorized programmable lift (Canfield, USA).
The assessments were performed before the procedure and at 1 month and 3 months post-procedure by qualified and experienced personnel who were blinded to whether they were assessing the test or control areas.
All evaluations took place in a controlled environment with a minimum 15-min acclimatization period. The room maintained a controlled temperature of 21 ± 2 °C and a relative humidity of 55 ± 10%.
Safety
Safety assessment consisted of monitoring for adverse events throughout the study.
Statistical Analysis
Data for all assessments (except photos) were presented as absolute values of the parameter for each experimental time, variation of the parameter against pre-procedure for each experimental time, and percent change of the parameter values and area variation of each experimental time compared to pre-procedure.
Difference in values between pre-procedure and at 1 and 3 months post-procedure were analyzed using Student’s t test or Wilcoxon signed rank test, performed with IBM® SPSS® 23 software. A significance level of 5% was adopted. A total of 10 subjects was considered sufficient to demonstrate a significant difference between AMT procedure and control. We planned to recruit 12 subjects to allow for potential dropouts.
Characteristics of Enrolled Subjects
Twelve subjects were included in the study, of whom two dropped out after day 28. The mean age of the remaining 10 subjects was 30.2 (range 21–47) years. Eight (66.7%) subjects had phototype III skin and the remaining 4 (33.3%) subjects had phototype II skin. The skin sensitivity was normal for 9 (75%) subjects and sensitive for 3 (25%) subjects. The condition of skin was normal for 5 (41.7%) subjects, dry for 3 (25.0%) subjects, combined for 3 (25.0%) subjects and oily for 1 (8.3%) subject (Table 1).
Results
Efficacy
Skin Roughness
At 1 and 3 months post-procedure, the roughness parameters (Ra and Rz) decreased in the treated area and increased in the control area compared with pre-procedure (Fig. 1). The decrease in the treated area at 3 months post-procedure was statistically significant compared with pre-procedure (Table 2). The decrease in Ra and Rz in the treated area at 3 months post-procedure was also statistically significantly higher compared with control area (P ≤ 0.05).
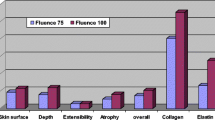
Skin Elasticity
At 3 months post-procedure, a statistically significant inprovement in skin elasticity compared with pre-procedure was observed in the treated area, while the difference was not statistically significant in the control area (Table 2). There was a 16.5% increase in skin elasticity in the treated area at 3 months post-procedure compared to pre-procedure (Fig. 2). The improvement in skin elasticity in treated area at 3 months post-procedure was also statistically significantly higher compared to the control area (P ≤ 0.05). Even at 1 month post-procedure, an improvement in skin elasticity from pre-procedure was observed in the treated area, but the difference was not significant (Table 2). Nevertheless, it is important to highlight that, within our study, a participant failed to attend the scheduled follow-up appointment 1 month after the procedure.
Skin Hydration
Both at 1 and 3 months post-procedure, a statistically significant improvement in skin hydration was observed compared with pre-procedure in the treated area; in the control area, the improvement was statistically significant at 1 month but not at 3 months (Table 1). The percentage improvement in skin hydration in the treated and control area is shown in Fig. 3. At 3 months post-procedure, the improvement in skin hydration in the treated area was significantly higher compared with the control area (P ≤ 0.05).
Skin Microcirculation
There was a statistically significant increase in skin microcirculation maximum value in the treated area at 1 and 3 months post-procedure compared with pre-procedure. The changes were nonsignificant in the control area (Table 1). The changes in skin microcirculation basal values at 1 and 3 months post-procedure were nonsignificant compared with pre-procedure in both the treated and control areas (Table 1). The percentage improvement in microcirculation maximum values post-procedure is shown in Fig. 4. The increase in skin microcirculation in the treated area was significantly higher compared with the control area at 1 and 3 months post-procedure (both P ≤ 0.05).
Skin Color
In the treated area, there was a statistically significant decrease in luminance (L*) at 1 and 3 months post-procedure compared with pre-procedure. In the control area, the L* increased from pre-procedure at 1 and 3 months post-procedure; the increase at 3 months was statistically significant (Table 1). The red-green color distribution (a*) increased from pre-procedure at 1 and 3 months post-procedure in both the treated and control areas. In both areas, the increase compared with pre-procedure was significant at 1 month and not significant at 3 months post-procedure (Table 1). The blue-green color distribution (b*) decreased significantly from pre-procedure at 3 months post-procedure in both areas (Table 1). The mean percentage change from pre-procedure at 1 and 3 months post-procedure is shown in Fig. 5.
The decrease in L* at 1 and 3 months post-procedure, and in b* at 3 months post-procedure in the treated area was significantly higher compared with the control area (both P ≤ 0.05). The difference between the two areas was not significant in a* at both time points post-procedure and in b* at 1 month post-procedure.
Ultrasonography
In the treated area, there was a statistically significant increase in skin thickness and hypodermis thickness at 1 and 3 months post-procedure compared with pre-procedure; the increase in skin density was statistically significant only at 3 months (Table 3). In the control area, the differences at 1 month post-procedure compared with pre-procedure were not significant for all three parameters; at 3 months post-procedure, only the increase in skin thickness was statistically significant (Table 3). However, it is noteworthy to mention that, in our study, one participant did not attend the scheduled follow-up appointment after 1 month. At 3 months post-procedure, the increase in all three parameters in the treated area was significantly higher compared with the control area (all P ≤ 0.05).
The mean percentage change in hypodermis thickness from pre-procedure at 1 and 3 months post-procedure is shown in Fig. 6. The ultrasonography images of the treated area pre-procedure and post-AMT procedure are shown in Fig. 7.
Individual Clinical Stretch Marks Score
The mean (sd) ICSS decreased at 1 and 3 months post-procedure compared with pre-procedure in both treated and control areas. The decrease in mean (sd) ICSS at 3 months (but not at 1 month) compared with pre-procedure was statistically significant in both the treated area (2.8 [0.4] vs 3.2 [0.4]) and control area (2.8 [0.2] vs 3.1 [0.3]), with p ≤ 0.05 for both areas. Furthermore, the decrease in mean scores at 3 months post-procedure was statistically significantly higher in the treated area compared with the control area (Fig. 8).
Subject Self-Assessment
In the treated area, the mean (sd) subject self-assessment score was 2.2 (1.1) at pre-procedure, 2.2 (1.2) at 1 month, and 1.6 (0.5) at 3 months post-procedure. In the control area, the mean (sd) subject self-assessment score was 2.7 (1.1) at pre-procedure, 2.6 (1.0) at 1 month post-procedure, and 2.7 (1.1) at 3 months post-procedure. Neither area showed a statistically significant difference from pre-procedure at 1 or 3 months; and there was no statistically significant difference between the two areas at either time point.
Analysis of Pre- and Post-Treatment Images
A thorough assessment of the treatment outcomes in both the treated and control groups was conducted through a comparative analysis of images taken before and after the procedures (Fig. 9). This investigation aimed to provide a visual representation of the changes and improvements observed in the subjects who underwent the treatment.
Discussion
The skin structure of SD is qualitatively and quantitatively different compared to normal skin [25]. SD skin is significantly less firm, less elastic, and less deformable than normal skin because of the disruption of the elastin fiber network, and it exhibits lower light scattering as a result of altered collagen fiber structure in the dermis [26, 27]. Hydration and pigmentation are lower, while skin roughness is higher in SD compared to normal skin [25,26,27]. Surface texture analysis has shown that the skin in the SD area is more anisotropic than the adjacent skin [25]. These changes were similar between striae rubrae and striae albae [28].
Hence, treatments for SD aim to increase dermal collagen production and fibroblastic activity, reduce lesional vascularity, wrinkling and skin roughness, increase skin pigmentation, skin elasticity, skin hydration and blood perfusion, improve cell proliferation, and enhance anti-inflammatory activity. However, most available treatment options work mainly on collagen synthesis [7]. As a result, management of SD remains a challenge [7].
Regenerative medicine involves replacing damaged tissue while maintaining its original function or, alternatively, stimulating self-regeneration of the tissue while respecting the original histological hierarchy [29]. The AMT procedure is based on stimulating self-regeneration by activating native progenitor cells located in homologous tissues. Autologous micrografts derived through mechanical tissue disaggregation with a cutoff of 80 µm are considered the gold standard of graft materials. They are enriched in progenitor cells expressing mesenchymal stem cell-like markers and possessing strong regenerative potential [8]. Progenitor cells, like stem cells, can differentiate, but their differentiation is specific to the target cell [8]. Human scalp tissues and hair follicles, easily accessible as a source of autologous grafts, contain progenitor cells located in the bulge area which have shown promising plasticity in ex vivo and in vitro conditions [30].
In this study, micrografts from the mastoid hair zone were used for the AMT procedure in women with SD. Among the 10 subjects included, most had normal phototype III skin. At 3 months post-AMT procedure, significant improvements were observed in most of the efficacy parameters studied compared to pre-procedure. Skin roughness, calculated on the basis of 3D images, decreased significantly. Similarly, the L* of the skin decreased significantly, indicating darkening of the skin on the SD area, making it appear less pronounced. During the same period, there was a significant increase in skin elasticity, skin hydration, and skin microcirculation maximum value. An R2 value of 1 is considered as 100%, indicating normal elasticity, and at 3 months, the value was 1.013 in the treated SD area, indicating a return to normalcy in skin elasticity. The AMT procedure resulted in significantly better improvement in each of the aforementioed parameters at 3 months compared to only microneedling. Ultrasonography images demonstrated a significant increase in skin thickness, hypodermis thickness, and skin density in the treated area at 3 months post-AMT procedure compared to pre-procedure. The AMT procedure resulted in significantly higher increases at 3 months compared to only microneedling. The mean ICSS scores decreased at 3 months post-procedure in both areas, but the score was significantly higher for the AMT procedure compared to only microneedling. Subject self-assessment scores did not differ significantly from pre-procedure at 1 and 3 months post-procedure with both procedures.
Current available treatments for stretch marks include topical creams, laser therapy, and microdermabrasion, but their efficacy varies. Notably, the Rigenera technology stands out as a promising approach, offering a superior alternative. Its innovative regenerative capabilities, as demonstrated in our study, suggest a potential breakthrough in addressing stretch marks compared to existing treatments. Similar favorable results with the AMT procedure for SD were reported by Horie et al. [31]. In Japanese subjects (7 women and 1 man) with SD on different areas of the body, in whom carbon dioxide gas laser treatments once every 3 weeks (for a total of 12–14 treatments) had failed, the AMT procedure using micrografts extracted from the scalp area resulted in an improvement in skin texture and roughness at 1 and 12 months post-procedure, without any negative impact. There was no overgrowth of skin regeneration in the region where the skin was rough, no dimple or bulge, and the skin texture resembled normal skin [31]. In comparison to the previously published Japanese study, our current work addresses several critical advancements in the field. Notably, our study includes a larger cohort, with the number of subjects increasing from 8 to 10, enhancing the statistical robustness of our findings. Furthermore, in addition to the test group undergoing the AMT procedure, we have incorporated a control group within the same patients, allowing for a direct intraindividual comparison. This design provides a more controlled and rigorous evaluation of the effectiveness of the Rigenera technology. Unlike the prior study, our approach involves a comprehensive assessment, with numerous clinical tests conducted to objectively evaluate the improvement in the condition of stretch marks before and after treatment with Rigenera. This multifaceted analysis contributes to a more nuanced understanding of the therapeutic impact of the regenerative procedure, offering a valuable extension to the existing body of literature and further establishing the significance of our findings.
Striae have a very similar evolution and histology to those of wound healing and scar formation [32,33,34]. In both SD and scars, the collagen fibers are altered and highly concentrated along the dermal and hypodermal layers, leading to thickness and rigidity of the dermis and hypodermis [35]. Several clinical studies have demonstrated the effectiveness of the AMT procedure using Rigenera technology in the management of complex wounds, chronic ulcers, and pathological scars [9, 16, 17, 36,37,38].
On the basis of the positive results from this study and the study by Horie et al. [31] in SD, as well as the favorable results from previous studies in wound healing and scars, it can be hypothesized that AMT procedure using Rigenera technology enables tissue regeneration and tissue remodeling. Further well-controlled studies with a larger number of subjects are needed to confirm this hypothesis.
In this study, all efficacy assessments were based on non-invasive methods, and the validity of these methodologies is supported by many previous studies [39,40,41,42,43,44,45]. Non-invasive methods, in general, are considered relevant and useful tools in studies assessing the efficacy of SD treatment options because the findings from these methods have been reported to be consistent with histological findings [25].
A strength of the study is that subjects acted as their own controls, enhancing the accuracy of the results by avoiding interperson variability. A limitation of the study is the small number of subjects. Additionally, the study did not differentiate between the effects on striae rubrae and striae albae.
In conclusion, the novelty of our work lies in its comprehensive approach to treating SD through the innovative Autologous Micrografting Technology procedure. The AMT procedure stimulates self-regeneration by activating native progenitor cells within homologous tissues, particularly those derived from the mastoid hair zone. This study expands upon the existing body of literature by presenting significant improvements in various efficacy parameters for SD treatment, such as skin roughness, L*, elasticity, hydration, and microcirculation. Importantly, we introduce a novel aspect by incorporating a control group within the same patients, allowing for a direct intraindividual comparison and enhancing the robustness of our findings. Furthermore, our study builds upon the positive outcomes observed in the context of wound healing and pathological scars, extending the application of AMT and Rigenera technology to address the unique challenges posed by striae distensae. The multifaceted analysis presented herein contributes to a deeper understanding of the therapeutic potential of this regenerative procedure, providing a novel perspective in the landscape of stretch mark management.
Conclusion
Treatment with the AMT procedure using Rigenera technology resulted in an improvement in SD appearance after 3 months in healthy women. Findings suggest the AMT procedure could be a promising new approach for managing SD, but further validation is needed through well-controlled studies with a larger population.
References
Oakley AM, Patel BC. Stretch Marks. [Updated 7 August 2023]. Treasure Island: StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK436005/. Accessed 25 Sept 2023.
Borrelli MR, Griffin M, Ngaage LM, Longaker MT, Lorenz HP. Striae distensae: scars without wounds. Plast Reconstr Surg. 2021;148(1):77–87.
Forbat E, Al-Niaimi F. Treatment of striae distensae: an evidence-based approach. J Cosmet Laser Ther. 2019;21(1):49–57.
Ud-Din S, McGeorge D, Bayat A. Topical management of striae distensae (stretch marks): prevention and therapy of striae rubrae and albae. J Eur Acad Dermatol Venereol. 2016;30(2):211–22.
Al-Himdani S, Ud-Din S, Gilmore S, Bayat A. Striae distensae: a comprehensive review and evidence-based evaluation of prophylaxis and treatment. Br J Dermatol. 2014;170(3):527–47.
Lu H, Guo J, Hong X, Chen A, Zhang X, Shen S. Comparative effectiveness of different therapies for treating striae distensae: a systematic review and network meta-analysis. Medicine. 2020;99(39):e22256.
Verdelli A, Bonan P, Fusco I, Madeddu F, Piccolo D. Striae distensae: clinical results and evidence-based evaluation of a novel 675 nm laser wavelength. Medicina (Kaunas). 2023;59(5):841.
Trovato L, Monti M, Del Fante C, et al. A new medical device Rigenera®cons allows to obtain viable micro-grafts from mechanical disaggregation of human tissues. J Cell Physiol. 2015;230:2299–303.
Giaccone M, Brunetti M, Camandona M, Trovato L, Graziano A. A new medical device, based on Rigenera® protocol, in the management of complex wounds. J Stem Cells Res Rev Rep. 2014;1(3):1013.
Purpura V, Bondioli E, Graziano A, et al. Tissue characterization after a new disaggregation method for skin micro-grafts generation. J Vis Exp. 2016;4(109):e53579.
Graziano A, Carinci F, Scolaro S, D’Aquino R. Periodontal tissue generation using autologous dental ligament micro-grafts: case report with 6 months follow-up. Ann Oral Maxillofac Surg. 2013;1(2):20.
Zanzottera F, Lavezzari E, Trovato L, Icardi A, Graziano A. Adipose derived stem cells and growth factors applied on hair transplantation. Follow-up of clinical outcome. J Cosmet Dermatol Sci Appl. 2014;04:268–74.
Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V. A combined use of chondrocytes micro grafts (CMG) mixed with platelet rich plasma (PRP) in patients affected by pinch nose deformity. J Regen Med. 2016;5:2.
Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V. Reconstruction of alar nasal cartilage defects using a tissue engineering technique based on a combined use of autologous chondrocyte micrografts and platelet-rich plasma: preliminary clinical and instrumental evaluation. Plast Reconstr Surg Glob Open. 2016;4(10):e1027.
Marcarelli M, Trovato L, Novarese E, Riccio M, Graziano A. Rigenera® protocol in the treatment of surgical wound dehiscence. Int Wound J. 2016;14(1):277–81.
Svolacchia F, De Francesco F, Trovato L, Graziano A, Ferraro GA. An innovative regenerative treatment of scars with dermal micrografts. J Cosmet Dermatol. 2016;15(3):245–53.
De Francesco F, Graziano A, Trovato L, et al. A regenerative approach with dermal micrografts in the treatment of chronic ulcers. Stem Cell Rev. 2017;13(1):139–48.
Ceccarelli G, Gentile P, Marcarelli M, et al. In vitro and in vivo studies of alar-nasal cartilage using autologous micro-grafts: the use of the Rigenera® protocol in the treatment of an osteochondral lesion of the nose. Pharmaceuticals (Basel). 2017;10(2):53.
Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V. Stem cells from human hair follicles: first mechanical isolation for immediate autologous clinical use in androgenetic alopecia and hair loss. Stem Cell Investig. 2017;4:58.
Fernández AD, Luengo AB. Biostimulation of knee cartilage using autologous micro-grafts: a preliminary study of the Rigenera® protocol in osteochondral lesions of the knee. Rehabil Sci. 2018;3(1):8–12.
Riccio M, Marchesini A, Zingaretti N, et al. A multicentre study: the use of micrografts in the reconstruction of full-thickness posttraumatic skin defects of the limbs—a whole innovative concept in regenerative surgery. Stem Cells Int. 2019;2019:5043518.
Gentile P, Scioli MG, Cervelli V, Orlandi A, Garcovich S. Autologous micrografts from scalp tissue: trichoscopic and long-term clinical evaluation in male and female androgenetic alopecia. Biomed Res Int. 2020;2020:7397162.
Zari S. Short-term efficacy of autologous cellular micrografts in male and female androgenetic alopecia: a retrospective cohort study. Clin Cosmet Investig Dermatol. 2021;14:1725–36.
Marcarelli M, Zappia M, Rissolio L, et al. Cartilage micrografts as a novel non-invasive and non-arthroscopic autograft procedure for knee chondropathy: three-year follow-up study. J Clin Med. 2021;10:322.
Bertin C, Lopes-DaCunha A, Nkengne A, Roure R, Stamatas GN. Striae distensae are characterized by distinct microstructural features as measured by non-invasive methods in vivo. Skin Res Technol. 2014;20(1):81–6.
Stamatas GN, Lopes-DaCunha A, Nkengne A, Bertin C. Biophysical properties of striae distensae evaluated in vivo using non-invasive assays. Skin Res Technol. 2015;21(2):254–8.
Wollina U, Goldman A. Management of stretch marks (with a focus on striae rubrae). J Cutan Aesthet Surg. 2018;10:124–9.
Cho C, Cho E, Kim N, et al. Biophysical properties of striae rubra and striae alba in human skin: comparison with normal skin. Skin Res Technol. 2019;25(3):283–8.
Astarita C, Arora C, Trovato L. Tissue regeneration: an overview from stem cells to micrografts. J Int Med Res. 2020;48(6):300060520914794.
Yu H, Fang D, Kumar SM, et al. Isolation of a novel population of multipotent adult stem cells from human hair follicles. Am J Pathol. 2006;168:1879–88.
Horie Y, Notoya S, Matsuda M, Trovato L. Use of autologous micrografting in the treatment of stretch marks. Dermatol Ther. 2020;33(2):e13217.
Arem AJ, Kischer CW. Analysis of striae. Plast Reconstr Surg. 1980;65(1):22–9.
Elsaie M, Baumann L, Elsaaiee L. Striae distensae (stretch marks) and different modalities of therapy: an update. Dermatol Surg. 2009;35(4):563–73.
Safonov I. Atrophic scars and stretch marks. In: Safonov I, editor. Atlas of scar treatment and correction. Berlin: Springer; 2012. p. 1–95. https://doi.org/10.1007/978-3-642-29196-8_1. Accessed 28 Sept 2023.
Veronese S, Picelli A, Zoccatelli A, et al. The pathology under stretch marks? An elastosonography study. J Cosmet Dermatol. 2022;21(2):859–64.
Trovato L, Failla G, Serantoni S, Palumbo FP. Regenerative surgery in the management of the leg ulcers. J Cell Sci Ther. 2016;7:238.
Baglioni E, Trovato L, Marcarelli M, Frenello A, Bocchiotti MA. Treatment of oncological post-surgical wound dehiscence with autologous skin micrografts. Anticancer Res. 2016;36(3):975–9.
Marcarelli M, Trovato L, Novarese E, Riccio M, Graziano A. Rigenera® protocol in the treatment of surgical wound dehiscence. Int Wound J. 2017;14(1):277–81.
Berardesca E. European group for efficacy measurements on cosmetics and other topical products (EEMCO). EEMCO guidance for the assessment of stratum corneum hydration: electrical methods. Skin Res Technol. 1997;3(2):126–32.
Zur Mühlen A, Klotz A, Weimans S, et al. Using skin models to assess the effects of a protection cream on skin barrier function. Skin Pharmacol Physiol. 2004;17(4):167–75.
Zhai H, Maibach H. Micro wound healing models. In: Rovee DT, Maibach HI, editors. The epidermis in wound healing, 1st ed. Boca Raton: CRC; 2004. p. 141–151. https://doi.org/10.1201/b14246.
Hexsel DM, Dal’forno T, Hexsel CL. A validated photonumeric cellulite severity scale. J Eur Acad Dermatol Venereol. 2009;23(5):523–8.
Rosado C, Pinto P, Rodrigues LM. Assessment of moisturizers and barrier function restoration using dynamic methods. Skin Res Technol. 2009;15(1):77–83.
Lenasi H. Assessment of human skin microcirculation and its endothelial function using laser doppler flowmetry. In: Erondu OF, editor. Medical imaging. InTech; 2011. p. 271–96. https://www.intechopen.com/chapters/25172.
Hexsel D, Mazzuco R. Cellulite. In: Tosti A, Hexsel D, editors. Update in cosmetic dermatology. Berlin: Springer; 2013. https://doi.org/10.1007/978-3-642-34029-1_2.
Acknowledgements
We thank the study participants for their involvement in the study.
Medical Writing, Editorial, And Other Assistance
Lakshmi Venkatraman, PhD provided medical writing support.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Investigation of the clínical background of the study, selection of the skin area to be treated, clínical treatments and follow-up, and paper review were performed by Leonor Girão. Conceptualization, methodology, statistical analysis, writing—original draft preparation, and supervision were performed by Pedro Pinto.
Corresponding author
Ethics declarations
Conflict of Interest
Leonor Girão has nothing to disclose. Petro Pinto has nothing to disclose.
Ethical Approval
The study protocol and all relevant study-related documents were approved by an independent ethics committee (PhD Trials Ethics Committee). The study was conducted in accordance with the protocol, the Helsinki Declaration of 1964 and its later amendments, the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use—Good Clinical Practice principles, and applicable Portuguese laws and regulations. Subjects provided written informed consent before the start of the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Girão, L., Pinto, P. Efficacy and Safety of an Autologous Micrografting Procedure for Management of Striae Distensae in Women. Dermatol Ther (Heidelb) 14, 469–488 (2024). https://doi.org/10.1007/s13555-023-01096-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01096-7