Abstract
Introduction
Despite improved treatment options for plaque psoriasis within the last decades, some patients still have an inadequate response to treatment. Direct clinical evaluation between therapies used after biologic failure could facilitate physicians’ choice of treatment.
Methods
COBRA (NCT04533737) was a randomized (1:1), blinded (patient and assessor), 28-week, active-comparator trial conducted in Europe from December 2020 to December 2022. The objective was to compare the efficacy and safety of brodalumab versus guselkumab in adults with moderate-to-severe plaque psoriasis and inadequate response to ustekinumab. Patients received either brodalumab 210 mg or guselkumab 100 mg. The primary [having Psoriasis Area and Severity Index (PASI)-100 response at week 16] and key secondary (time to PASI-100 response) endpoints were tested in a fixed sequence.
Results
Due to delays and enrollment challenges, recruitment was terminated with 113 patients enrolled of 240 planned. The proportion of patients having PASI-100 at week 16 for brodalumab was 53.4% compared with 35.9% for guselkumab [odds ratio (OR) 2.05; 95% confidence interval (CI) 0.95, 4.44; p = 0.069]. As this was not statistically significant, the hierarchical testing procedure was stopped. All other secondary PASI endpoints had nominal p-values below 0.05 in favor of brodalumab. In the time to PASI response analyses, brodalumab separated from guselkumab in estimated cumulative incidence of patients achieving a response from week 2 onward, suggesting fast onset of action with brodalumab. Quality of life measures improved in both treatment groups. The safety findings were consistent with the known safety profiles.
Conclusions
Brodalumab showed a tendency toward better and earlier effect than guselkumab in patients who had failed ustekinumab. Thus, this trial provides important information in assisting physicians in their choice of therapy for patients who have failed their prior anti-interleukin (IL)-12/23 treatment.
Trial Registration
ClinicalTrials.gov identifier NCT04533737.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With increasing availability of novel biologics with new targets for psoriasis, the complexity of choosing the appropriate biologic treatment is ever more challenging for physicians. |
Recent evidence suggests that the persistence of psoriasis may also involve an IL-23-independent pathway, which could explain the lack of efficacy seen in some patients. |
The primary objective of this trial was to compare the efficacy of brodalumab (an IL-17 receptor antagonist) with that of guselkumab (an IL-23p19 inhibitor) in patients with plaque-type psoriasis switching from ustekinumab (an IL-12/23p40 inhibitor) failure. |
Brodalumab showed a tendency toward better and earlier effect than guselkumab in patients who had failed ustekinumab and was well tolerated. |
This trial thus provides important information to assist physicians in their choice of therapy for patients who have failed their prior anti-IL-12/23 treatment. |
Introduction
With increasing availability of novel biologics with new targets for psoriasis, the complexity of choosing the appropriate biologic treatment is ever more challenging for physicians. This applies not only to choosing the most appropriate treatment for the patient, but also to deciding on subsequent treatment options if the patient has failed a biologic treatment.
It is well known that the interleukin (IL)-17 signaling pathway plays a key role in the pathophysiology of psoriasis and includes the IL-23-dependent activation of Th17 cells. Therefore, ustekinumab, an IL-12/23 subunit p40 inhibitor, is one of the preferred treatment options for moderate-to-severe psoriasis [1]. However, recent evidence suggests that the persistence of the disease may also involve an IL-23-independent pathway, which could explain the lack of efficacy seen in some patients [2]. In the ARROW trial, direct inhibition of IL-17A by secukinumab modulated a greater proportion of psoriasis disease transcriptome genes and resulted in more histological responders than did guselkumab, a selective IL-23p19 inhibitor, in patients who had failed ustekinumab [3]. Similarly, brodalumab, an IL-17 receptor antagonist (IL-17RA) that blocks the signaling of IL-17A, IL-17C, IL-17F, IL-17A/F, and IL-17E, has been shown to result in lesional skin resembling non-lesional skin on a cellular and molecular level after 12 weeks of treatment, changes that were also reflected in clinical improvement [4].
The primary objective of this trial was to compare the efficacy of brodalumab with that of guselkumab in patients with plaque-type psoriasis switching from ustekinumab failure (primary or secondary). The recruitment was terminated due to delays and slow recruitment that significantly jeopardized the trial timelines, and 113 patients of the planned 240 were randomized. This led to a reduction in the statistical power. There were no safety concerns related to the termination of the trial.
Methods
Trial Design
COBRA (NCT04533737) was a phase 4, 28-week, randomized, blinded (patient and assessor), active-comparator trial conducted in Europe from December 2020 to December 2022. The trial had a 16-week induction phase (primary endpoint) and a 12-week maintenance phase (Fig. 1). After the patients completed the trial, they were treated at the investigator’s discretion according to standard practice. Patients who discontinued the trial early were asked to return to an early termination visit within 2 weeks after last dose of investigational medicinal product (IMP). The investigators were required to follow up on serious adverse events (SAEs) until final outcome. Patients were randomized 1:1 to receive brodalumab 210 mg every 2 weeks or guselkumab 100 mg every 8 weeks. Randomization was performed using an interactive response technology system and was stratified by baseline body weight (≤ 100 kg and > 100 kg) to further ensure comparability of the treatment groups.
Placebo to mimic brodalumab and guselkumab was used to blind patients and assessor to treatment allocation, and three substantial amendments were issued. Further details regarding the blinding and the protocol amendments are available in the Supplementary Material.
The trial was conducted in accordance with the Declaration of Helsinki and International Council of Harmonisation (ICH) Good Clinical Practice (GCP), including archiving of essential documents. The trial protocol was approved by the relevant institutional review boards/ethics committees before commencement and patients provided written informed consent before trial-related procedures.
Eligibility Criteria
Patients (aged ≥ 18 years) who had plaque psoriasis that was inadequately controlled with ustekinumab were eligible. Ustekinumab had been administered ≥ 3 times at or higher than the approved dose or frequency before randomization, and the patients had an Investigator’s Global Assessment (IGA) score ≥ 2 and an absolute Psoriasis Area and Severity Index (PASI) score > 3 at screening and baseline. Patients were ineligible if they had a clinically important active, chronic, recurrent, or latent infection, if they had severe depression within the last 2 years, a Patient Health Questionnaire-8 (PHQ-8) score ≥ 10 at baseline or screening, or a history of suicidal ideation and behavior on the basis of the Columbia-Suicide Severity Rating Scale (C-SSRS) at screening or baseline. For further details including the list of prohibited medication, see the Supplementary Material.
Endpoints and Estimands
The primary endpoint was PASI-100 response at week 16 and the key secondary endpoint was the time to PASI-100 response, where PASI-100 means 100% improvement from baseline in PASI score.
Secondary and exploratory efficacy endpoints were based on assessments performed throughout the trial of PASI [5] and Investigator’s Global Assessment [6]. Quality of life (QoL) endpoints were based on Dermatology Life Quality Index (DLQI) [7], 36-Item Short Form Health Survey version 2 acute recall (SF-36v2) [8], pruritus numeric rating scale (NRS), and pain NRS. In patients with palmoplantar (PP) psoriasis, PP-PASI [9] and PP-IGA [6] were assessed, and in patients with genital involvement, static Physician’s Global Assessment of Genitalia (sPGA-G) [10] was assessed. p-Values presented for secondary and exploratory endpoints are nominal p-values.
Safety was evaluated as the occurrence of treatment-emergent adverse events (TEAEs) from baseline to week 28.
For each efficacy endpoint, the treatment effect was described through specification of a corresponding primary estimand. The primary estimand for the primary endpoint summarized outcomes using the odds ratio and least squares mean risk difference of having PASI-100 response at week 16 without prior permanent discontinuation of investigational medicinal product (IMP) independent of pandemic restrictions. The primary estimand for the key secondary endpoint summarized outcomes using the difference in cumulative incidence functions for the time to PASI-100 response prior to permanent discontinuation of IMP independent of pandemic restrictions. Moreover, analysis strategies for addressing unblinding of patients and permanent discontinuation of IMP due to pandemic restrictions were defined for each estimand on the basis of the introduction of a coronavirus disease 2019 (COVID-19) pandemic contingency plan. The primary estimands for the primary and key secondary endpoints were both specified to ignore occurrences of patients becoming unblinded and to envisage what the outcomes would have been in a hypothetical scenario where patients would not permanently discontinue IMP due to pandemic restrictions. Full details on endpoints and statistical analyses are provided in the Supplementary Material.
Statistical Analysis
Sample size calculations were based on cross-study comparisons of results from previous brodalumab [11] and guselkumab trials [12]. Further details are available in the Supplementary Material.
All randomized patients with at least one post-baseline PASI assessment were included according to their planned treatment in efficacy analyses, and all patients who received IMP were included according to the treatment they actually received in safety analyses.
To control the family-wise error rate, the primary and key secondary endpoints were specified to be tested in a fixed sequence. Initially, the primary endpoint was to be evaluated by testing for superiority of brodalumab over guselkumab at the two-sided significance level of 0.05. If the null hypothesis for the primary endpoint was rejected, the key secondary endpoint was to be assessed. Otherwise, the hierarchical testing procedure was to stop.
The primary endpoint was analyzed on the basis of a logistic regression model, adjusted for baseline body weight (≤ 100 kg, > 100 kg) and baseline PASI score. Missing data were imputed using multiple imputation on the basis of a missing at random assumption within treatment groups. The primary endpoint was tested on the basis of the odds ratio between the two treatment groups. Sensitivity analyses investigated robustness of results with respect to assumptions on missing data, treatment group–body weight interaction, and use of prohibited medication and procedures.
The key secondary endpoint was analyzed on the basis of a competing risks model with PASI-100 response as the event of interest and with permanent discontinuation of IMP independent of pandemic restrictions as the single competing event. Cumulative incidence functions for the model were estimated for the groups defined by treatment group and baseline body weight (≤ 100 kg, > 100 kg) on the basis of the Aalen–Johansen estimator. In addition, sub-distribution hazard ratios comparing treatment groups were estimated on the basis of a Fine–Gray model, stratified by baseline body weight (≤ 100 kg, > 100 kg) and adjusted for baseline PASI score. Gray’s test, stratified by baseline body weight (≤ 100 kg, > 100 kg), was used for testing the key secondary endpoint. The analysis imputed the time to PASI-100 response on the basis of the trial visit in which the response was first observed. A sensitivity analysis investigated the robustness of this imputation strategy by accounting for the intermittent observation process.
Similar statistical methods were used for analysis of other endpoints, which included calculation of nominal p-values. These hypothesis tests were not controlled for multiplicity.
Details on estimands, imputation strategies, and sensitivity analyses are provided in the Supplementary Material.
Results
Patient Population
A total of 141 patients were screened and 113 patients were randomized to brodalumab (N = 56) or guselkumab (N = 57). In total, six patients from each treatment group permanently discontinued IMP, and six patients in the brodalumab group and seven patients in the guselkumab group withdrew from the trial (Fig. 2).
The mean number of patient-years of observation was similar in the two treatment groups, as was the mean number of patient-years of exposure. 53 patients in the brodalumab group and 50 patients in the guselkumab group were exposed for ≥ 16 weeks.
Patient demographics and baseline disease characteristics were similar across treatment groups except for disease severity, where the patients in the brodalumab group had lower mean ± SD PASI score (9.98 ± 6.61) than those in the guselkumab group (12.93 ± 8.04) and more patients in the brodalumab group (35.7%) than in the guselkumab group (15.8%) had a baseline IGA score of 2 (mild). The difference in baseline PASI score was more pronounced in the patients with baseline weight > 100 kg (Table 1). As all other baseline characteristics were well balanced between the two treatment groups, this apparently skewed distribution in disease severity was considered to be a random occurrence and to not impact the interpretation of the trial results.
Efficacy Results
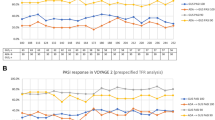
The proportion of PASI-100 responders in the brodalumab and guselkumab groups at week 16 (the induction phase) was estimated to be 53.4% and 35.9%, respectively, with an estimated treatment difference of 17.5% [95% confidence interval (CI) −1.2%, 36.2%]. The odds ratio of having PASI-100 at week 16 in the brodalumab group compared with guselkumab was estimated to be 2.05 (95% CI 0.95, 4.44) (p = 0.069) (Fig. 3a). As this was not statistically significant, the hierarchical testing procedure was stopped. The likelihood of having PASI-100 was higher in the brodalumab group than in the guselkumab group at weeks 4 and 8 (odds ratios (95% CI): 15.91 (1.97, 128.6), p = 0.009 and 3.50 (1.39, 8.80), p = 0.008, respectively; Table S1). Following the maintenance phase (week 28), the proportion of PASI-100 responders in the brodalumab and guselkumab groups was 61.4% and 36.8%, respectively, with an estimated treatment difference of 24.6% and an odds ratio (95% CI) of 2.73 (1.24, 5.98) (p = 0.012) (Table S1).
PASI response. Top: Proportion of patients with PASI-100 response assessed separately at weeks 1, 2, 4, 6, 8, 10, 12, 14, 16, and 28 (a) and PASI-90 response assessed separately at weeks 4, 8, 16, and 28 (b), LS-mean response rate plot, main analyses of primary estimands. The primary estimand addresses permanent discontinuation of IMP independent of pandemic restrictions using a ‘composite’ strategy, permanent discontinuation of IMP due to pandemic restrictions using a ‘hypothetical’ strategy, and unblinding of patients using a ‘treatment policy’ strategy. The main analysis imputes missing data using multiple imputation under a missing at random assumption within treatment arms and is based on a logistic regression model, adjusted for baseline body weight (≤ 100 kg, > 100 kg), and baseline PASI score. Least squares mean estimates are based on the observed margins. Analysis for week 1 not done due to no responders. Analysis for week 2 not done due to possible quasi-complete separation of data points. Bottom: Time to PASI-100 (c) and PASI-90 (d) response, cumulative incidence function, main analysis of the primary estimand. The primary estimand addresses permanent discontinuation of IMP independent of pandemic restrictions using a ‘while on treatment’ strategy, permanent discontinuation of IMP due to pandemic restrictions using a ‘hypothetical’ strategy, and unblinding of patients using a ‘treatment policy’ strategy. In a competing risks setting, the main analysis estimates cumulative incidence functions on the basis of the Aalen–Johansen estimator. The cumulative incidence functions presented at the top describe the probability of having achieved the time-to-event endpoint by a given timepoint, accounting for permanent discontinuation of IMP independent of pandemic restrictions as a competing risk. Likewise, the cumulative incidence functions presented at the bottom describe the probability of having permanently discontinued IMP independently of pandemic restrictions by a given timepoint, accounting for the presence of the time-to-event endpoint. The numbers shown below the graphs are the number of patients at risk at each timepoint. CB confidence band (pointwise), CI confidence interval, FAS full analysis set, IMP investigational medicinal product, LS-mean least squares mean, N number of subjects in the analysis set, PASI Psoriasis Area and Severity Index, PASI-100 100% improvement from baseline in PASI score, PASI-90 at least 90% improvement from baseline in PASI score
The cumulative incidence of achieving PASI-100 was estimated higher for brodalumab than for guselkumab at all timepoints from week 2 onward to week 28, indicating that at any of these timepoints, patients receiving brodalumab were estimated more likely to have achieved PASI-100 than patients receiving guselkumab, irrespective of their baseline weight (≤ 100 kg or > 100 kg) (Fig. 3c and Table S3).
Similarly, the cumulative incidence of achieving PASI-90 was estimated higher for brodalumab than for guselkumab at all timepoints from week 2 onward (Fig. 3d). The likelihood of having PASI-90 was higher in the brodalumab group than in the guselkumab group at weeks 4, 8, 16, and 28 (Fig. 3b and Table S4).
The likelihood of having IGA-0 response was higher in the brodalumab group than in the guselkumab group at weeks 4, 8, 16, and 28, while the likelihood of having IGA-0/1 response was higher in the brodalumab group than in the guselkumab group at weeks 4, 8, and 16. At week 28, the likelihood of having IGA-0/1 was also estimated higher in the brodalumab group than in the guselkumab group, but at this timepoint the nominal p-value was not below the 5% significance level (Table S1).
Clinically relevant improvements in QoL measures were seen from week 4 onward when assessed by DLQI, SF-36v2 and pruritus or pain NRS, with little difference between treatment groups (Table S2). Only a few patients had palmoplantar or genital psoriasis and all comparisons of treatment groups based on PP-PASI, PP-IGA, or sPGA-G led to nominal p values > 0.05 (Fig. 4 and Table S1).
DLQI, pruritus NRS, PP-PASI-100 response, and sPGA-G-0/1 response—FAS. LS-mean response rate plot, main analyses of primary estimands. The primary estimand addresses permanent discontinuation of IMP independent of pandemic restrictions using a ‘composite’ strategy, permanent discontinuation of IMP due to pandemic restrictions using a ‘hypothetical’ strategy, and unblinding of patients using a ‘hypothetical’ (a, b) or ‘treatment policy’ (c, d) strategy. The main analysis imputes missing data using multiple imputation under a missing at random assumption within treatment arms and is based on a logistic regression model, adjusted for baseline body weight (≤ 100 kg, > 100 kg), and baseline score. Least squares mean estimates are based on the observed margins. b: The 11-point pruritus NRS ranges between 0 and 10 with 0 indicating ‘no itch’ and 10 indicating ‘worst possible itch’. c: Analysis for week 4 not done due to possible quasi-complete separation of data points. CI confidence interval, DLQI Dermatology Life Quality Index, FAS full analysis set, IMP investigational medicinal product, LS-mean least squares mean, N number of subjects in analysis set (a, b), N number of subjects in the analysis set who have a positive PP-PASI score at baseline (c), N number of subjects in the analysis set who have a positive sPGA-G value at baseline (d); NRS numeric rating scale, PASI Psoriasis Area and Severity Index, PP-PASI palmoplantar PASI, sPGA-G static Physician’s Global Assessment of Genitalia
Safety Results
During the 28 weeks treatment period, 42 patients (75.0%) in the brodalumab group and 31 patients (55.4%) in the guselkumab group had TEAEs. The majority of events were non-serious, of mild or moderate intensity, and assessed as not related to IMP by the investigator. The most frequent TEAEs reported (> 10% in any treatment group) were arthralgia, COVID-19, and nasopharyngitis. There were no cases of Crohn’s disease or diarrhea (Table 2).
In the brodalumab group, the greatest increase in reporting of TEAEs occurred during the initial approximately 5 weeks, at which point the mean number of events per patient reached 1. In the guselkumab group, a mean of 1 TEAE per patient was reached at week 14 (Fig. 5a). Despite this difference between the treatment groups, only three patients in the brodalumab group and two patients in the guselkumab group permanently discontinued IMP due to TEAEs. In the brodalumab group, two patients reported 13 and 20 TEAEs, respectively, thus two patients accounted for 18% of the TEAEs reported for brodalumab (Fig. 5b).
A total of four patients in each treatment group had one serious adverse event each. All but one of these were not related to IMP. The latter case was a patient who had suicidal ideation approximately 5 months after starting brodalumab. The patient had a history of anxiety, depression, and suicidal ideation, and was being followed by a psychiatrist and receiving treatment. During the trial, the patient reported a worsening of anxiety, which resolved after 2 weeks, experienced work stress, and had an intragastric balloon procedure. At week 20, the patient had a PHQ-8 score of 2 and no suicidal ideation was reported, but 5 days later, the depressive symptoms worsened with suicidal ideation corresponding to category 2 of the C-SSRS. The event ‘suicidal ideation’ was severe in intensity, serious, and the patient withdrew from the trial. The patient recovered. Two patients in each treatment group had one adverse event of special interest (AESI) each. The AESIs were not grouped in a particular type (Table 2).
Discussion
In this 28-week, randomized, blinded, active-comparator trial, brodalumab demonstrated a trend toward better efficacy than guselkumab in patients who had failed ustekinumab. In the induction phase, brodalumab showed a tendency toward greater PASI response rates than guselkumab at all timepoints, though the primary endpoint (having PASI-100 response at week 16) was not statistically significant. Following the maintenance phase, the estimated treatment difference between the groups had increased. At baseline, the patients in the brodalumab group had a lower observed mean PASI score than those in the guselkumab group, but as baseline PASI score was adjusted for as a covariate in the analyses, the difference would not affect the interpretation of the results.
All other PASI and IGA endpoints were in favor of brodalumab with nominal p-values below 0.05 at week 4, suggesting fast onset of effect of brodalumab; this was supported by the time to PASI response analyses in which brodalumab separated from guselkumab as early as week 2. This fast onset of action has been consistently observed with brodalumab treatment [13, 14], and importantly, the observed effect is sustained during long-term treatment [13, 15, 16].
The fast onset for PASI-100 and PASI-90 was seen irrespective of the patients’ baseline weight (≤ 100 kg or > 100 kg). However, due to the low number of patients with a baseline weight > 100 kg, this should be interpreted with caution.
Psoriasis prevalence is similar in male and female patients and there is currently no clear evidence of differences in disease manifestation between male and female patients [17]. In this trial, more male patients than female patients were recruited, though not by design, and no subgroup analysis by sex was performed.
A fast clinical response is important to patients, even when considering a chronic disease such as psoriasis, and this is reflected in a rapid positive impact on QoL. DLQI improvement was seen already after 4 weeks of treatment and the DLQI response rates in the brodalumab group were in alignment with previous DLQI observations for brodalumab, mirroring the improvements in efficacy [14, 18]. Improvements in PP-PASI and sPGA-G scores were seen in both treatment groups, but the number of patients was low.
Treatment success in EMA guidance is defined as achieving PASI-90 or IGA-0/1 [19]. In this trial, treatment success was defined as PASI-100 (complete skin clearance) and still showed a large proportion of patients achieving response. This is in alignment with a matching-adjusted indirect comparison (MAIC), in which brodalumab showed significantly better efficacy than guselkumab in patients who had failed ustekinumab [20].
Additionally, this trial provides further support to the emerging evidence that IL-17, independently of IL-23 activation2, represents an effective alternative target in disease management to IL-23, thus providing information that can help physicians decide on the best choice of therapy for their patient.
The rate of TEAEs observed for brodalumab in this trial was in line with that previously observed [21, 22], and as also observed by Reich et al. [21], the greatest increase in reporting of TEAEs occurred during the initial weeks of treatment. The types of events in the brodalumab group were in alignment with the known safety profile and no safety concerns were identified.
Throughout the treatment period, there were more patients in the brodalumab group than in the guselkumab group who reported TEAEs. This may reflect the different mechanisms of action of brodalumab and guselkumab as already described in the literature. A meta-analysis of AEs with IL-23 inhibitors and IL-17 inhibitors during treatment of patients with psoriasis and psoriatic arthritis [23] showed that the proportion of patients with any AEs was lower in patients treated with IL-23 inhibitors compared with those treated with IL-17 inhibitors.
The main limitation of this randomized, active-comparator, double-blind trial was the small sample size. The trial was terminated after having recruited approximately half of the planned patients. This affected the statistical power in the efficacy analyses, but it may also have affected the safety evaluation as outliers have a larger impact on the results.
Conclusions
Brodalumab treatment showed a tendency toward better and earlier effect than guselkumab treatment in patients who had failed ustekinumab. Thus, this trial provides important information to assist physicians in their choice of therapy for patients who have failed their prior anti-IL-12/23 treatment.
Data Availability
Qualified researchers may request data from LEO Pharma clinical trials. Complete details are available at Clinical trial disclosure|LEO Pharma (leo-pharma.com).
References
Torres T, Puig L, Vender R, Lynde C, Piaserico S, Carrascosa JM, Gisondi P, Daudén E, Conrad C, Mendes-Bastos P, et al. Drug survival of IL-12/23, IL-17 and IL-23 inhibitors for psoriasis treatment: a retrospective multi-country, multicentric cohort study. Am J Clin Dermatol. 2021;22(4):567–79.
Kim BR, Kim M, Yang S, Choi CW, Lee KS, Youn SW. Persistent expression of interleukin-17 and downstream effector cytokines in recalcitrant psoriatic lesions after ustekinumab treatment. J Dermatol. 2021;48(6):876–82.
Krueger J, Langley RG, Nigen S, Kasparek T, Comite GD, Ortmann CE, Garcet S, Kolbinger F, Reich K. Secukinumab versus guselkumab in the complete resolution of ustekinumab-resistant psoriatic plaques: the ARROW study. Exp Dermatol. 2023. https://doi.org/10.1111/exd.14828.
Tomalin LE, Russell CB, Garcet S, Ewald DA, Klekotka P, Nirula A, Norsgaard H, Suàrez-Fariñas M, Krueger JG. Short-term transcriptional response to IL-17 receptor-A antagonism in the treatment of psoriasis. J Allergy Clin Immunol. 2020;145(3):922–32.
Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Ann Rheum Dis. 2005;64(Suppl 2):ii65-68.
Langley RG, Feldman SR, Nyirady J, van de Kerkhof P, Papavassilis C. The 5-point Investigator’s Global Assessment (IGA) Scale: a modified tool for evaluating plaque psoriasis severity in clinical trials. J Dermatol Treat. 2015;26(1):23–31.
Finlay AY, Khan GK. Dermatology life quality index (DLQI)–a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Ware JEJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Morales-Munera C, Vilarrasa E, Puig L. Efficacy of ustekinumab in refractory palmoplantar pustular psoriasis. Br J Dermatol. 2013;168(4):820–4.
Merola JF, Bleakman AP, Gottlieb AB, Menter A, Naegeli AN, Bissonnette R, Guenther L, Sullivan J, Meeuwis K, See K, Duffin KC. The static physician’s global assessment of genitalia: a clinical outcome measure for the severity of genital psoriasis. J Drugs Dermatol. 2017;16(8):793–9.
Langley RG, Armstrong AW, Lebwohl MG, Blauvelt A, Hsu S, Tyring S, Rastogi S, Pillai R, Israel R. Efficacy and safety of brodalumab in patients with psoriasis who had inadequate responses to ustekinumab: subgroup analysis of two randomized phase III trials. Br J Dermatol. 2019;180(2):306–14.
Langley RG, Tsai TF, Flavin S, Song M, Randazzo B, Wasfi Y, Jiang J, Li S, Puig L. Efficacy and safety of guselkumab in patients with psoriasis who have an inadequate response to ustekinumab: results of the randomized, double-blind, phase III NAVIGATE trial. Br J Dermatol. 2018;178(1):114–23.
Papp K, Menter A, Leonardi C, Soung J, Weiss S, Pillai R, Jacobson A. Long-term efficacy and safety of brodalumab in psoriasis through 120 weeks and after withdrawal and retreatment: subgroup analysis of a randomized phase III trial (AMAGINE-1). Br J Dermatol. 2020;183(6):1037–48.
Philipp S, Hansen J, Nielsen V, Chiricozzi A. Poster: immediate onsent of action of brodalumab compared with ustekinumab: results from the phase 3 AMAGINE-2 and -3 studies. In 6th Congress of the Skin Inflammation & Psoriasis International Network. Paris-France. 2019.
Lebwohl MG, Blauvelt A, Menter A, Papp KA, Guenthner S, Pillai R, Israel RJ, Jacobson A. Efficacy, safety, and patient-reported outcomes in patients with moderate-to-severe plaque psoriasis treated with brodalumab for 5 years in a long-term, open-label, phase ii study. Am J Clin Dermatol. 2019;20(6):863–71.
Puig L, Lebwohl M, Bachelez H, Sobell J, Jacobson AA. Long-term efficacy and safety of brodalumab in the treatment of psoriasis: 120-week results from the randomized, double-blind, placebo- and active comparator-controlled phase 3 AMAGINE-2 trial. J Am Acad Dermatol. 2019. https://doi.org/10.1016/j.jaad.2019.05.095.
Guillet C, Seeli C, Nina M, Maul LV, Maul JT. The impact of gender and sex in psoriasis: what to be aware of when treating women with psoriasis. Int J Womens Dermatol. 2022;8(2): e010.
Strober B, Papp KA, Lebwohl M, Reich K, Paul C, Blauvelt A, Gordon KB, Milmont CE, Viswanathan HN, Li J, et al. Clinical meaningfulness of complete skin clearance in psoriasis. J Am Acad Dermatol. 2016;75(1):77-82.e77.
EMA. European Medicines Agency. Guideline on Clinical Investigation of Medicinal Products indicated for the Treatment of Psoriasis. 2004.
Hampton P, Borg E, Hansen JB, Augustin M. Efficacy of brodalumab and guselkumab in patients with moderate-to-severe plaque psoriasis who are inadequate responders to ustekinumab: a matching adjusted indirect comparison. Psoriasis (Auckl). 2021;11:123–31.
Reich K, Thaçi D, Stingl G, Andersen JS, Hiort LC, Lexner MO, Winkler D, Paul C. Safety of brodalumab in plaque psoriasis: integrated pooled data from five clinical trials. Acta Derm Venereol. 2022;102:adv0683.
Pinter A, Hoffmann M, Reich K, Augustin M, Kaplan K, Gudjónsdóttir SD, Delvin T, Mrowietz U. A phase 4, randomized, head-to-head trial comparing the efficacy of subcutaneous injections of brodalumab to oral administrations of fumaric acid esters in adults with moderate-to-severe plaque psoriasis (CHANGE). J Eur Acad Dermatol Venereol. 2021;35(3):701–11.
Loft ND, Vaengebjerg S, Halling AS, Skov L, Egeberg A. Adverse events with IL-17 and IL-23 inhibitors for psoriasis and psoriatic arthritis: a systematic review and meta-analysis of phase III studies. J Eur Acad Dermatol Venereol. 2020;34(6):1151–60.
Acknowledgements
The authors thank the patients who participated in this trial and the COBRA investigator group.
Medical Writing Assistance.
The authors would like to acknowledge Helle Harder Birkeslund, of Harder Medical Writing, a freelance medical writer contracted by LEO Pharma for medical writing support in accordance with Good Publications Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Funding
Sponsorship for this trial and Rapid Service Fee were funded by LEO Pharma A/S, Ballerup, Denmark.
Author information
Authors and Affiliations
Contributions
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for all aspects of the work, and have given their approval for this version to be published. KR, LB, AK, J-TM, AT, CMS, and LP served as investigators in the trial and provided input to, reviewed, and approved the final version of the manuscript. KR provided input to the trial protocol as signatory investigator. KP and MMN were the trial statistician and medical expert, respectively, and contributed to the interpretation of trial results and provided input to, reviewed, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
K Reich has served as advisor and/or paid speaker for and/or participated in clinical trials sponsored by Abbvie, Almirall, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Forward Pharma, Gilead, Galderma, Janssen-Cilag, Kyowa Kirin, Leo, Lilly, Medac, Novartis, Ocean Pharma, Pfizer, Sanofi, UCB; Professor Reich is co-founder of Moonlake Immunotherapeutics. L Bianchi has been a consultant for and/or has received honoraria and/or investigator fees from AbbVie, Almirall, Amgen, Biogen Idec, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Janssen, LEO Pharma, Novartis, Pfizer, Sanofi, Sun Pharma, and UCB Pharma. A Khemis has been a consultant for and/or has received honoraria and/or investigator fees from AbbVie, Actelion, Almirall, Amgen, Basilea, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Eli Lilly, Forward Pharma, GlaxoSmithKline, Galderma, Genentec, Janssen, La Roche Posay, LEO Pharma, Medac, Merck Sharp & Dohme, Novartis, Pierre Fabre Dermatologie, Pfizer, Regeneron, Roche, Sanofi and UCB Pharma. JT Maul has served as advisor and/or received speaking fees and/or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, BMS, Celgene, Eli Lilly, LEO Pharma, Janssen-Cilag, MSD, Novartis, Pfizer, Pierre Fabre, Roche, Sanofi, and UCB. A Tsianakas has received honoraria and investigator fees from LEO Pharma A/S. CM Schempp has been a consultant for and/or has received honoraria and/or investigator fees from Abbvie Inc, Allmirall, Biofrontera, Boehringer Ingelheim, Birken AG, CassellaMed GmbH & Co KG, Celgene GmbH, Essex Pharma GmbH, Janssen-Cilag GmbH, LEO Pharma A/S, Medac, Novartis AG, Lilly GmbH, Pfizer, Sanofi Regeneron, Therakos, UCB Pharma. K Petersen and MM Noergaard are employees of LEO Pharma A/S. L Puig has received consultancy/speaker’s honoraria from and/or participated in clinical trials sponsored by Abbvie, Almirall, Amgen, Baxalta, Biogen, Boehringer Ingelheim, Celgene, Gebro, Janssen, JS BIOCAD, LEO Pharma, Lilly, Merck-Serono, MSD, Mylan, Novartis, Pfizer, Regeneron, Roche, Sandoz, Samsung-Bioepis, Sanofi and UCB.
Ethical Approval
The trial was conducted in accordance with the Declaration of Helsinki and ICH GCP, including archiving of essential documents. The trial protocol was approved by the institutional review boards/ethics committees before commencement and patients provided written informed consent before trial-related procedures.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Reich, K., Bianchi, L., Khemis, A. et al. Brodalumab Versus Guselkumab in Patients with Moderate-to-Severe Psoriasis with an Inadequate Response to Ustekinumab: A Randomized, Multicenter, Double-Blind Phase 4 Trial (COBRA). Dermatol Ther (Heidelb) 14, 453–468 (2024). https://doi.org/10.1007/s13555-023-01092-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01092-x