Abstract
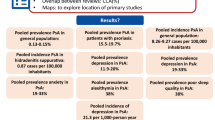
Psoriasis is associated with various comorbidities with a notable psychosocial burden. This systematic literature review explores the burden of depression in patients with psoriasis, comparing it with that experienced by patients with other chronic medical conditions. Embase via Ovid, PubMed, and Cochrane Database of Systematic Reviews via Ovid were searched for peer-reviewed studies published in English between January 1, 2016 and December 6, 2021 that reported real-world evidence or observational studies involving at least 100 adults (age ≥ 18 years) with general (unspecified) or plaque psoriasis experiencing symptoms of depression (but not restricted to patients with a clinical diagnosis). Any report of depression or suicidality was eligible for inclusion. Systematic literature reviews reporting depression/suicidality in other chronic medical conditions were also included. Statistical analysis was not performed; the study was descriptive only. A total of 1744 records were identified, and after several defined screenings by two independent reviewers for publication year, relevance, and sample size, 82 publications were included. Psoriasis was significantly associated with depression. The prevalence of depression in patients with psoriasis ranged from 0.2% to 74.6%, with incidence from 4.83 to 91.9 per 1000 person-years. The prevalence of depression was generally higher among patients with more severe psoriasis than those with less severe disease (as determined by Psoriasis Area Severity Index [PASI] scoring system) and was more prevalent among women than men with psoriasis. Depression in psoriasis significantly reduced quality of life, including factors such as sexual dysfunction, sleep difficulties, subjective well-being, and addictions. Comorbid hypertension, hyperlipidemia, psoriatic arthritis, obesity, inflammatory bowel disease, diabetes, and statin use were all associated with increased depression risk in patients with psoriasis. This systematic literature review found that the burden of depression in psoriasis is no lower than in other chronic medical conditions. Greater awareness of the psychological impact of psoriasis would improve care and management, which should incorporate psychological interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This systematic review explored the burden of depression in patients with psoriasis, comparing this with other chronic medical conditions. |
Psoriasis was significantly associated with depression: the prevalence of depression in patients with psoriasis ranged from 0.2% to 74.6%, and the incidence from 4.83 to 91.9 per 1000 person-years. |
The impact of psoriasis on health and well-being should not be underestimated. |
Clinical management of patients with psoriasis should include psychological interventions. |
Introduction
Psoriasis is a chronic and relapsing immune-mediated skin disease associated with a variety of comorbidities, including dyslipidemia, hypertension, diabetes, Crohn’s disease, and cerebrovascular disease [1]. It bears a notable psychosocial burden, with higher rates of depression and suicidal ideation reported in those with psoriasis than the general population [2].
The estimated prevalence of psoriasis in adults ranges from 0.5% [3] to 11.4% [4], with wide geographic variation [3,4,5]. Higher rates have been reported in Western countries and those more distant from the equator [6]. Psoriasis can occur at any age, but its first presentation often follows a bimodal distribution with peaks of onset at 20–30 and 50–60 years of age [7].
Although primarily a disease of the skin, treatments focused on physical symptoms alone are insufficient for managing psoriasis-associated comorbidities and their psychosocial impact. Psoriasis is associated with social stigmatization [8], as well as impaired self-esteem and interpersonal relationships [9]. The resulting social and emotional burden can impact quality of life. Despite these damaging effects, the psychosocial impact of psoriasis is often overlooked and underestimated by healthcare professionals [10]. Identifying and addressing the factors that contribute to depression and suicidal ideation in patients with psoriasis would enhance the quality of care and help optimize treatment plans by incorporating psychosocial interventions.
This systematic literature review (SLR) aims to understand the burden of depression in patients with psoriasis and compare it with that experienced by patients with other chronic medical conditions.
Methods/Literature Search
Searches were run in PubMed and, via Ovid, in Embase®, Cochrane Database of Systematic Reviews, and Cochrane Central Register of Controlled Trials for peer-reviewed, English-language articles (excluding conference abstracts) published between January 1, 2016 and December 6, 2021. References from relevant publications were hand searched to identify articles not appearing in database hits.
Inclusion and exclusion criteria are outlined in Table S1 in the electronic supplementary material. Publications were included if they reported real-world evidence from studies involving at least 100 adults with general (unspecified) or plaque psoriasis who were experiencing depression. Some of the general populations could have included patients with psoriatic arthritis but these patients were not specially identified. Studies in patients with psoriatic arthritis only were excluded. We chose the figure of at least 100 adults so as to exclude case series, and also to only include well-powered studies. Interventional studies were excluded. The studies were not restricted to those only involving patients with a diagnosis of depression. No specific criteria for depression were required for inclusion to illustrate the range of different measures used to assess depression in different studies. Studies included measures of prevalence and/or incidence of depression, psoriasis severity, outcomes, suicidal ideation, completed suicide, or suicide attempts.
Targeted searching identified SLRs reporting on depression/suicidality outcomes in other chronic conditions. SLRs reporting outcomes from non-interventional studies in adults were eligible. Where at least two SLRs were available for one condition, the most recent was assessed.
Duplicate and out-of-scope publications were removed after verification by a second researcher. Titles and abstracts, then full texts, were screened for eligibility by two independent researchers. Reasons for exclusion were cross-checked by both reviewers, with a third consulted in instances of discrepancies. Data from full-text articles were extracted by one reviewer and assessed for accuracy by a second.
Longitudinal and case–control studies were assessed for risk of bias using the Newcastle–Ottawa Scale (NOS) [11]. The quality of observational cross-sectional studies was assessed using the modified NOS and scored out of 10 for bias.
Statistical analysis was not performed; the study was descriptive only. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Characteristics of Included Studies
Searches identified 1744 publications. After duplicates and out-of-scope records were removed, remaining publications (n = 1071) were screened by title and abstract, and 925 excluded. A further 64 were excluded following full-text screening, leaving 82 publications (Fig. 1) of which 55 (67%) were cross-sectional and 26 (32%) longitudinal studies (16 retrospective, 10 prospective). One study used both retrospective cohort and annual cross-sectional analyses for different outcomes and was categorized as cross-sectional. The largest proportions of both cross-sectional and longitudinal studies were of European participants (54% and 42%), followed by studies from Asia (21% and 23%), USA (9% and 23%), and elsewhere (16% and 12%). Sample sizes ranged from 100 to almost 14 million. The characteristics of the included studies are summarized in Table S2 (cross-sectional studies) and Table S3 (longitudinal studies).
Patient Characteristics
In 21 publications reporting the psoriasis subtype, plaque psoriasis/psoriasis vulgaris was most common, comprising 81–100% of participants. The Psoriasis Area Severity Index (PASI) scoring system was most frequently used to measure psoriasis. PASI scores reported in 29 publications ranged from 3.43 to 18.27 (mean) and 5.3 to 22 (median). Disease duration, reported in 41 publications, ranged from 0.25 to 68 years. Studies specifically reporting mean disease duration ranged 3.87 to 24.63 years (26 publications).
Depression Among Patients with Psoriasis
There was considerable variation in the prevalence of depression as a result of variations in study design and settings. Self-reported instruments were the most common tools for measuring depression: Hospital Anxiety and Depression Scale (HADS), Beck Depression Inventory (BDI), and Patient Health Questionnaire were used in 16, 9, and 9 studies, respectively (Fig. 2). Prevalence of depression in patients with psoriasis (Fig. 3; Table S4) ranged from 0.2% in a large cohort study in Taiwan [12] to 74.6% in a cross-sectional study in South Korea [13]. For studies reporting HADS scores, prevalence ranged from 6% to 38%. In studies in patients with plaque psoriasis only, prevalence ranged from 5.8% to 28.5%. Where reported, the incidence rate of depression in psoriasis ranged from 4.83 to 91.9 per 1000 person-years (Fig. 4; Table S4).
Assessment tools used to measure depression. BDI Beck Depression Inventory, CES-D Center for Epidemiologic Studies Depression Scale, DASS-42 Depression Anxiety and Stress Scale, DSM-5 Diagnostic and Statistical Manual of Mental Disorders 5th Edition, HADS Hospital Anxiety and Depression Scale, HRDS Hamilton Depression Rating Scale, MADRS Montgomery-Asberg Depression Rating Scale, MINI Mini-International Neuropsychiatric Interview, PHQ-2/9 2-item/9-item Patient Health Questionnaire, SCL-90-R Symptom Checklist-90 Revised, WHO-5 World Health Organization—Five Well-Being Index, Zung-SDS Zung Self-Rating Depression Scale
Of 14 studies comparing prevalence of depression in psoriasis versus controls (including adults with no diagnosis of psoriasis or healthy individuals), most (n = 12) found a significantly higher prevalence of depression in patients with psoriasis.
Patients with more severe psoriasis generally had a higher prevalence of depression than those with less severe disease. Compared with patients without psoriasis, patients with psoriasis had a higher prevalence of depression regardless of disease severity [14,15,16,17], with one study reporting that more severe forms of psoriasis associated with an increased risk (adjusted hazard ratio (HR) 1.28, 95% confidence interval [CI] 1.07–1.54) [16]. The prevalence of depression was statistically significantly higher in women with psoriasis than men (7/10 studies).
Suicidality Among Patients with Psoriasis
In studies reporting suicidal ideation, prevalence ranged from 0.4% to 21.0% (Fig. 5; Table S5). Four studies compared prevalence of suicidal ideation in patients with psoriasis with healthy age- and sex-matched controls; three of these studies reported significantly higher rates of suicidal ideation in patients with psoriasis [18,19,20].
The incidence of suicidal ideation was reported in five studies and ranged from 0.31 per 10,000 to 23 per 10,000 person-years (Table S6). Two of three studies where incidence was compared found a significantly higher incidence of suicidal ideation in patients with psoriasis versus those without [17, 19]. In one study, there was no significantly increased risk for suicidal ideations or suicide attempt among patients with psoriasis [12].
The prevalence of attempted suicide ranged from 0.4% to 6.6%. The prevalence of attempted suicide in patients with psoriasis was compared with age- and sex-matched control subjects without psoriasis in three studies [18, 19, 21], two of which found a significantly higher prevalence among those with psoriasis [18, 19].
A 12-year Korean cohort study measured the association between suicide risk across all ICD-10 disorders [18]. Compared with non-suicidal controls, patients with psoriasis had the second highest increased risk of completed suicide (after schizophrenia) of all ICD-10 disorders (adjusted odds ratio [OR] 15.45, 95% CI 8.14–29.29; P < 0.01). In the same study, a subgroup analysis found a significantly increased risk of suicide in all age groups, except < 19 years, with the strongest association in patients > 65 years (adjusted OR 44.70, 95% CI 8.93–223.63; P < 0.01) [18].
The incidence rate of suicide attempt or completed suicide ranged from 1.1 to 2.16 per 10,000 person-years [16, 19]. Two studies compared patients with psoriasis and controls (one conducted in adult patients with psychiatric disease from a Korean national health insurance registry [16], the other using administrative data of patients with a diagnosis of psoriasis from two large healthcare organizations in the USA) [17]; neither reported a significant difference between groups. Subgroup analyses for non-fatal self-harm by gender and age (< 40 and ≥ 40 years) were assessed in one UK primary care database study [19] of 56,961 diagnosed patients with psoriasis, and 876,919 controls matched for age, sex, and general practice. There were no significant differences according to sex, and no association between age and self-harm. Psoriasis severity was not significantly associated with incidence of suicidal ideation/suicide attempt [19].
Comorbidities Associated with Depression in Psoriasis
In 36 studies evaluating the association between depression in psoriasis and other emotional, psychiatric, and physical comorbidities, there was a significant association between depression and quality of life in studies with available data [22,23,24,25,26]. One descriptive, cross-sectional study of patients with psoriasis (n = 219) reported high levels of psychological distress quadrupled the chances of depression (OR 4.17, 95% CI 1.79–9.71; P < 0.001) [27].
Comorbid depression in psoriasis was also associated with sexual dysfunction [28], sleep difficulties [29], and subjective well-being [30]. One cross-sectional, non-interventional study [31] of 502 participants with psoriasis in Germany reported that patients with psoriasis show a greater likelihood of some addictions compared to representative samples of the general German population, including alcohol dependency (8.6% vs. 3.1%), smoking daily (30.3% vs. 15.1%), legal or illegal drug abuse (6.0% vs. 3.2–5.2%), and pathological gambling (1.2% vs. 0.2%). Depression was significantly associated with drug addiction and alcohol.
Comorbid hypertension, hyperlipidemia, psoriatic arthritis, and obesity were also associated with an increased risk of depression in psoriasis [32, 33]. In a study of 247,755 patients with psoriasis [32], patients with comorbid inflammatory bowel disease (IBD), diabetes, hypertension, and those using statins had an increased risk of depression compared with the general population (all P < 0.0001).
Depression Prevalence in Other Chronic Medical Conditions
SLRs evaluating the prevalence of depression in peripheral arterial disease (PAD), heart failure (HF), chronic obstructive pulmonary disease (COPD), and IBD were identified to compare with the prevalence of depression in psoriasis (Fig. 6). The prevalence of depression varied widely as a result of the heterogeneity across individual studies, particularly where the number of studies included was high. The prevalence of depression in patients with PAD was reported in an SLR of 28 publications (all observational) ranging from 3% to 48% [34]. Depression prevalence ranged from 7.5% to 100% among patients with HF (94 studies [35]) and from 15.2% to 35.7% among patients with COPD (8 studies [36]). One SLR included patients with IBD; of 75 studies included (including Crohn’s disease, ulcerative colitis, and mixed populations), the prevalence of depression ranged from 10.5% to 88.9% [37].
Quality and Risk of Bias in Included Studies
A summary of quality assessment for publications is shown in Table S7. All longitudinal studies assessed by NOS, except one [38], scored ≥ 5 points. Six studies scored 9, indicating a low risk of bias. Eighteen cross-sectional studies scored ≥ 8 (two scored 10 points) [39, 40]. Four studies scored between 5 and 7, and six studies received a score of 4, suggesting a high risk of bias. One case–control study scored 9 points [41]. Four studies scored between 6 and 8, indicating a medium risk of bias. One study had a score of 4 points [28], suggesting a high risk of bias.
Discussion
The objective of this SLR was to develop a wider understanding of the burden of depression in patients with psoriasis. Eighty-two observational studies were included, with the largest proportion of studies conducted in Europe and Asia. The prevalence and incidence of depression varied widely, mostly due to heterogeneity in study design. However, depression was significantly more common in patients with versus without psoriasis (whether healthy controls or those with other chronic diseases). Depression prevalence ranged from 0.2% in a large retrospective cohort study of 169,909 patients with psoriasis in Taiwan [12] to 74.6% in a cross-sectional study of 118 patients with psoriasis from South Korea [13]. Although the prevalence reported in the Taiwanese study was low, it was significantly higher than the 0.13% reported for age- and sex-matched non-psoriatic controls [12].
Of nine studies reporting depression outcomes using HADS, two were compared with a control group [42, 43]. The mean score in both studies was significantly higher in patients with psoriasis. Similar results were observed when depression severity was measured using the 9-item Patient Health Questionnaire (PHQ-9) [44]. HADS and PHQ, along with the BDI, were the most used tools for measuring depressive burden among the studies included in this review and are commonly used in the clinic [45, 46].
Among patients with psoriasis, female sex and having more severe psoriasis were risk factors associated with depression. Women with psoriasis reported a higher overall prevalence of depression than male patients in all but one study out of 19 reporting data on the prevalence of depression in psoriasis by gender. However, in studies comparing patients of both sexes with psoriasis versus a control group of patients without psoriasis, men with psoriasis still had increased prevalence compared with their non-psoriatic counterparts. This suggests prevalence of depression is higher for those with psoriasis regardless of gender, although being female may pose an additional risk.
The prevalence of suicidal ideation or suicide attempts varied widely but was higher among patients with versus without psoriasis. All but one study comparing prevalence of suicidal ideation in psoriasis with controls found patients with psoriasis are at a significantly higher risk of suicidal ideation than those without psoriasis. In the one study [32] that did not find an increased risk of current suicidal ideation in patients with psoriasis, the authors used patients with other dermatological disorders as a reference group, which may not have compared reliably with psoriasis. These results suggest that compared with the general population, suicidal ideation tends to be more common among patients with psoriasis.
When compared with controls, patients with psoriasis had significantly higher odds of suicide than those without psoriasis. The percentage of those with psoriasis who had attempted suicide ranged from 0.4% in a German questionnaire-based study [23] of 228 patients with psoriasis in an outpatient setting to 6.6% in an Italian questionnaire-based study including 91 patients with psoriasis, also in an outpatient setting [21]. The latter study included patients with melanoma and other allergic dermatological conditions as the reference group. Although no significance in current suicidal ideation was observed between the psoriasis and control groups, this is not an accurate indication of significance, as the study may have been confounded as a result of the possibility of patients with melanoma and other dermatological conditions also having an elevated risk of suicide.
Depression in psoriasis is associated with several other emotional, psychiatric, and physical comorbidities. These include type D personality [38, 45] (tendency toward negative affect such as worry, irritability, and gloom along with social inhibition, reticence, and lack of self-assurance [46]), obesity [43], cardiovascular comorbidity [32, 33], and sleep difficulties [29]. Comorbid depression in psoriasis is associated with sexual dysfunction [28], sleep difficulties [29], and subjective well-being [30].
Results from this SLR suggest that depression is correlated with reduced quality of life in patients with psoriasis. One study reported that depression was significantly associated with lower self-esteem and body satisfaction [47]. Another found that the presence and severity of depression in patients with psoriasis could negatively impact physical health, as measured by the 12-item Short Form Survey [43]. These findings suggest that depression adversely affects physical health, further reducing quality of life.
Although prevalence varied widely among individual studies for all chronic medical conditions assessed (PAD, HF, IBD, and COPD), the prevalence of depression in patients with psoriasis was comparable with these conditions. Further, this psoriasis-focused SLR reports a wider range of depression prevalence than that reported for COPD (15.2–35.7%) and PAD (3–48%); however, the highest observed depression prevalence values were in psoriasis populations. A recent systematic review and meta-analysis also reports that the risk of depression is greater for patients with psoriasis or psoriatic arthritis, compared with non-psoriasis controls [48].
The burden of psoriasis has often been overlooked and/or underestimated by healthcare professionals. However, this SLR provides evidence that depression is no less of a burden for patients with psoriasis than for those with other chronic medical conditions. Increased awareness of the association of the comorbidity of depression in patients with psoriasis will enable better quality of care and management incorporating psychosocial interventions to reduce the symptoms of depression and the overall patient burden.
This review has identified several evidence gaps regarding the burden of depression in patients with psoriasis. A large proportion of studies were conducted in Europe and Asia, suggesting geographic variation in the recognition and management of the psychological impact of psoriasis. There was a lack of studies conducted in the USA and Canada, and only one study each conducted in Latin America (Brazil) and Africa (Egypt); evidence from patients in these regions is therefore under-represented. None of these studies assessed the incidence of suicidal ideation/suicide attempt based on psoriasis severity, and only one reported incidence by age and sex.
Limitations of this review include the heterogeneity across studies, in terms of the depression assessments used, cutoff points, and methods (including patient health records, patient surveys, administrative claims databases) for obtaining data. Secondly, data on depression according to psoriasis subtype and disease severity were lacking. In many studies, the measure and cutoff point used to assess psoriasis severity were not reported. Finally, the prevalence and incidence of depression were not always adjusted for confounders that may affect the relationship between psoriasis and depression. Although many studies reported adjusted data, the variables included in multiple regression models were often unclear.
Conclusions
Where data were available, most studies found an increased prevalence and incidence of depression among patients with psoriasis compared to age- and sex-matched controls without psoriasis, as well as reduced quality of life. This study provides evidence showing that the burden of depression is as high in patients with psoriasis as in those with other chronic medical conditions, such as IBD and COPD. Greater awareness of the psychological impact of psoriasis would enhance patient care and is vital for improving clinical outcomes and health-related quality of life in this population.
Data Availability
All data presented are publicly available.
References
World Health Organization (WHO). Global report on psoriasis. https://apps.who.int/iris/handle/10665/204417. Accessed Nov 21 2022.
Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol. 2014;134:1542–51. https://doi.org/10.1038/jid.2013.508.
Danielsen K, Olsen AO, Wilsgaard T, Furberg AS. Is the prevalence of psoriasis increasing? A 30-year follow-up of a population-based cohort. Br J Dermatol. 2013;168:1303–10. https://doi.org/10.1111/bjd.12230.
Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135:2955–63. https://doi.org/10.1038/jid.2015.296.
Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31:205–12. https://doi.org/10.1111/jdv.13854.
Parisi R, Symmons DP, Griffiths CE, et al. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377–85. https://doi.org/10.1038/jid.2012.339.
Armstrong AW. Psoriasis. JAMA Dermatol. 2017;153:956. https://doi.org/10.1001/jamadermatol.2017.2103.
Hrehorów E, Salomon J, Matusiak L, Reich A, Szepietowski JC. Patients with psoriasis feel stigmatized. Acta Derm Venereol. 2012;92:67–72. https://doi.org/10.2340/00015555-1193.
Young M. The psychological and social burdens of psoriasis. Dermatol Nurs. 2005;17:15–9.
Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y. The psychosocial burden of psoriasis. Am J Clin Dermatol. 2005;6:383–92. https://doi.org/10.2165/00128071-200506060-00005.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. https://doi.org/10.1007/s10654-010-9491-z.
Wang SH, Wang J, Chi CC, et al. Risk for suicidal behavior among psoriasis patients: a nationwide cohort study. Am J Clin Dermatol. 2020;21:431–9. https://doi.org/10.1007/s40257-019-00489-9.
Park SY, Kim KH. What factors influence on dermatology-related life quality of psoriasis patients in South Korea? Int J Environ Res Public Health. 2021;18. https://doi.org/10.3390/ijerph18073624.
Dregan A, Matcham F, Harber-Aschan L, et al. Common mental disorders within chronic inflammatory disorders: a primary care database prospective investigation. Ann Rheum Dis. 2019;78:688–95. https://doi.org/10.1136/annrheumdis-2018-214676.
Jensen P, Ahlehoff O, Egeberg A, Gislason G, Hansen PR, Skov L. Psoriasis and new-onset depression: a Danish nationwide cohort study. Acta Derm Venereol. 2016;96:39–42. https://doi.org/10.2340/00015555-2183.
Oh J, Jung KJ, Kim TG, Kim HW, Jee SH, Lee MG. Risk of psychiatric diseases among patients with psoriasis in Korea: a 12-year nationwide population-based cohort study. J Dermatol. 2021;48(11):1763–71. https://doi.org/10.1111/1346-8138.16115.
Wu JJ, Penfold RB, Primatesta P, et al. The risk of depression, suicidal ideation and suicide attempt in patients with psoriasis, psoriatic arthritis or ankylosing spondylitis. J Eur Acad Dermatol Venereol. 2017;31:1168–75. https://doi.org/10.1111/jdv.14175.
Na EJ, Lee H, Myung W, et al. Risks of completed suicide of community individuals with ICD-10 disorders across age groups: a nationwide population-based nested case-control study in South Korea. Psychiatry Investig. 2019;16:314–24. https://doi.org/10.30773/pi.2019.02.19.
Parisi R, Webb RT, Kleyn CE, et al. Psychiatric morbidity and suicidal behaviour in psoriasis: a primary care cohort study. Br J Dermatol. 2019;180:108–15. https://doi.org/10.1111/bjd.17004.
Geale K, Henriksson M, Jokinen J, Schmitt-Egenolf M. Association of skin psoriasis and somatic comorbidity with the development of psychiatric illness in a nationwide Swedish study. JAMA Dermatol. 2020;156:795–804. https://doi.org/10.1001/jamadermatol.2020.1398.
Pompili M, Innamorati M, Trovarelli S, et al. Suicide risk and psychiatric comorbidity in patients with psoriasis. J Int Med Res. 2016;44:61–6. https://doi.org/10.1177/0300060515593253.
Patel P, Rosen CF, Chandran V, Ye YJ, Gladman DD. Addressing comorbidities in psoriatic disease. Rheumatol Int. 2018;38:219–27. https://doi.org/10.1007/s00296-017-3895-y.
Sondermann W, Fiege O, Korber A, Scherbaum N. Psychological burden of psoriatic patients in a German university hospital dermatology department. J Dermatol. 2021;48:794–806. https://doi.org/10.1111/1346-8138.15721.
Bakar RS, Jaapar SZS, Azmi AF, Aun YC. Depression and anxiety among patients with psoriasis: a correlation with quality of life and associated factors. J Taibah Univ Med Sci. 2021;16:491–6. https://doi.org/10.1016/j.jtumed.2021.02.008.
Gerdes S, Wilsmann-Theis D, Celis D, Kromer C, Mossner R. Two questions may be enough—screening for depression in patients with psoriasis: a multicenter study. J Dtsch Dermatol Ges. 2020;18:1115–25. https://doi.org/10.1111/ddg.14203.
Pollo CF, Miot HA, Matos TDS, et al. Prevalence and factors associated with depression and anxiety in patients with psoriasis. J Clin Nurs. 2021;30:572–80. https://doi.org/10.1111/jocn.15577.
Wojtyna E, Lakuta P, Marcinkiewicz K, Bergler-Czop B, Brzezinska-Wcislo L. Gender, body image and social support: biopsychosocial determinants of depression among patients with psoriasis. Acta Derm Venereol. 2017;97:91–7. https://doi.org/10.2340/00015555-2483.
Gunduz A, Topcuoglu V, Usta Gunduz EB, Ergun T, Gencosmanoglu DS, Sungur MZ. Significant effects of body image on sexual functions and satisfaction in psoriasis patients. J Sex Marital Ther. 2020;46:160–9. https://doi.org/10.1080/0092623X.2019.1654582.
Jensen P, Zachariae C, Skov L, Zachariae R. Sleep disturbance in psoriasis: a case-controlled study. Br J Dermatol. 2018;179:1376–84. https://doi.org/10.1111/bjd.16702.
Schuster B, Peifer C, Ziehfreund S, et al. Happiness and depression in psoriasis: a cross-sectional study in Germany. Qual Life Res. 2022;31:1761–73. https://doi.org/10.1007/s11136-021-02991-2.
Schielein MC, Tizek L, Knobloch L, Maassen D, Biedermann T, Zink A. Psoriasis and addiction: assessing mental health based on a cross-sectional study in Germany. Eur J Dermatol. 2021;31:722–9. https://doi.org/10.1684/ejd.2021.4146.
Egeberg A, Thyssen JP, Wu JJ, Skov L. Risk of first-time and recurrent depression in patients with psoriasis: a population-based cohort study. Br J Dermatol. 2019;180:116–21. https://doi.org/10.1111/bjd.17208.
Carr E, Mahil SK, Brailean A, et al. Association of patient mental health status with the level of agreement between patient and physician ratings of psoriasis severity. JAMA Dermatol. 2021;157:413–20. https://doi.org/10.1001/jamadermatol.2020.5844.
Brostow DP, Petrik ML, Starosta AJ, Waldo SW. Depression in patients with peripheral arterial disease: a systematic review. Eur J Cardiovasc Nurs. 2017;16:181–93. https://doi.org/10.1177/1474515116687222.
Moradi M, Doostkami M, Behnamfar N, Rafiemanesh H, Behzadmehr R. Global prevalence of depression among heart failure patients: a systematic review and meta-analysis. Curr Probl Cardiol. 2022;47: 100848. https://doi.org/10.1016/j.cpcardiol.2021.100848.
Matte DL, Pizzichini MM, Hoepers AT, et al. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med. 2016;117:154–61. https://doi.org/10.1016/j.rmed.2016.06.006.
Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359–70. https://doi.org/10.1016/s2468-1253(21)00014-5.
Aguayo-Carreras P, Ruiz-Carrascosa JC, Ruiz-Villaverde R, Molina-Leyva A. Four years stability of type D personality in patients with moderate to severe psoriasis and its implications for psychological impairment. An Bras Dermatol. 2021;96:558–64. https://doi.org/10.1016/j.abd.2021.02.005.
Hu SC, Chen GS, Tu HP. Epidemiology of depression in patients with psoriasis: a nationwide population-based cross-sectional study. Acta Derm Venereol. 2019;99:530–8. https://doi.org/10.2340/00015555-3145.
Cai Q, Teeple A, Wu B, Muser E. Prevalence and economic burden of comorbid anxiety and depression among patients with moderate-to-severe psoriasis. J Med Econ. 2019;22:1290–7. https://doi.org/10.1080/13696998.2019.1638788.
Duvetorp A, Mrowietz U, Nilsson M, Seifert O. Sex and age influence the associated risk of depression in patients with psoriasis: a retrospective population study based on diagnosis and drug-use. Dermatology. 2021;237:595–602. https://doi.org/10.1159/000509732.
Demirci O, Ates B, Sagaltici E, Ocak Z, Altunay I. Association of the attachment styles with depression, anxiety, and quality of life in patients with psoriasis. Dermatol Sin. 2020;38:81–7. https://doi.org/10.4103/ds.ds_35_19.
Innamorati M, Quinto RM, Imperatori C, et al. Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr Psychiatry. 2016;70:200–8. https://doi.org/10.1016/j.comppsych.2016.08.001.
Cohen BE, Martires KJ, Ho RS. Psoriasis and the risk of depression in the US population: National Health and Nutrition Examination Survey 2009–2012. JAMA Dermatol. 2016;152:73–9. https://doi.org/10.1001/jamadermatol.2015.3605.
Aguayo-Carreras P, Ruiz-Carrascosa JC, Molina-Leyva A. Type D personality is associated with poor quality of life, social performance, and psychological impairment in patients with moderate to severe psoriasis: a cross-sectional study of 130 patients. Indian J Dermatol Venereol Leprol. 2020;86:375–81. https://doi.org/10.4103/ijdvl.IJDVL_114_19.
Emons WH, Meijer RR, Denollet J. Negative affectivity and social inhibition in cardiovascular disease: evaluating type-D personality and its assessment using item response theory. J Psychosom Res. 2007;63:27–39. https://doi.org/10.1016/j.jpsychores.2007.03.010.
Hassani F, Koraei A, Yaghoobi R, Zarea K. An evaluating of the relationship between body image, body satisfaction, depression, marital quality, and self-esteem in patients with psoriasis. Psychol Health Med. 2021;26:467–77. https://doi.org/10.1080/13548506.2020.1766093.
Lukmanji A, Basmadjian RB, Vallerand IA, Patten SB, Tang KL. Risk of depression in patients with psoriatic disease: a systematic review and meta-analysis. J Cutan Med Surg. 2021;25:257–70. https://doi.org/10.1177/1203475420977477.
Acknowledgments
Medical Writing, Editorial, and Other Assistance
The authors thank Lauren Moubarak, MPharm, of Curo Consulting, Envision Pharma Group, for reference screening, data collection, and data processing, which was funded by Pfizer. Medical writing support was provided by David Sunter, PhD, of Engage Scientific Solutions and was funded by Pfizer.
Funding
This work was supported by Pfizer. The rapid service and open access fee were funded by Pfizer.
Author information
Authors and Affiliations
Contributions
Paula C Luna, Chia-Yu Chu, Mohammad Fatani, Cecilia Borlenghi, Anna Adora, Lyndon Q Llanado, and James Wee contributed to the conception of this work, contributed to and reviewed draft manuscripts, and approved the final article for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Paula C. Luna has served as investigator, speaker, and advisor for AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Janssen, Novartis, Pfizer, Sandoz, and Sanofi. Chia-Yu Chu is an investigator for AbbVie, Amgen, Lilly, Novartis, Oneness Biotech, Pfizer, Regeneron, Roche, Sanofi, and United BioPharma; a consultant for AbbVie, Janssen, Lilly, Novartis, Pfizer, Roche, Sanofi, United BioPharma, and Viatris; a speaker for AbbVie, Lilly, Mylan, Novartis, Pfizer, Roche, Sanofi, and Viatris; and an advisory board member for AbbVie, Janssen, Lilly, Mylan, Novartis, Pfizer, Roche, Sanofi, and Viatris. Mohammad Fatani has received honoraria for speaking and serving as a consultant for AbbVie, Novartis, Eli Lilly, and Newbridge. Cecilia Borlenghi, Anna Adora, Lyndon Q. Llamado, and James Wee are employees and stockholders of Pfizer.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Luna, P.C., Chu, CY., Fatani, M. et al. Psychosocial Burden of Psoriasis: A Systematic Literature Review of Depression Among Patients with Psoriasis. Dermatol Ther (Heidelb) 13, 3043–3055 (2023). https://doi.org/10.1007/s13555-023-01060-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01060-5