Abstract
Introduction
Pruritus is a prevalent symptom, described as one of the most bothersome of psoriasis. Specific itch management remains a challenge, for which hydrotherapy could be used as adjunct care to medical treatment. Therefore, we assessed the immediate and longer-term benefit of 3 weeks of Avène thermal spring water hydrotherapy on chronic pruritus in patients in addition to their usual psoriasis and/or pruritus management.
Methods
Twenty-six patients suffering from chronic pruritus due to psoriasis were evaluated before and after 3 weeks of hydrotherapy with a 3 and 6 month follow-up. A control group (18 patients) did not undergo hydrotherapy and continued to follow their usual skin management. Pruritus was assessed according to the numeric rating scale (NRS, pruritus intensity), the visual dynamic pruritus score (vDPS, change in pruritus intensity), and the 5-D itch scale (pruritus characteristics). Psoriasis severity was measured using the psoriasis area and severity index (PASI) score. The “itchy quality of life” (ItchQoL) scale was used to assess quality-of-life (QoL) impact related to itch. Pruritus and psoriasis gene and protein biomarkers were measured in lesional and nonlesional skin.
Results
Pruritus measurements (NRS, vDPS, and 5-D itch scale) indicated an immediate and long-lasting positive effect of hydrotherapy compared with control patients. The psoriasis area and severity index (PASI) was decreased by 40.0% by hydrotherapy, which was sustained over 6 months. The ItchQoL also improved directly after hydrotherapy, which was still much improved even 6 months later. Analysis of gene and/or protein biomarkers revealed a significant decrease of inflammation biomarkers (IL-8, IL-1α, IL-1RA, and RANTES), of psoriasis biomarkers (PI3, S100A7, and IL-17), and of pruritus biomarkers (IL-31, TRPV1, and CGRP1).
Conclusions
These findings demonstrated an immediate and long-lasting improvement of pruritus in patients with psoriasis who underwent Avène thermal spring water hydrotherapy, indicating that this would be a good complementary therapy in the management of this disease.
Trial Registration
NCT03023254.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pruritus is a prevalent symptom of psoriasis; therefore, the benefit of 3 weeks of hydrotherapy on chronic pruritus in patients was assessed. |
What was learned from the study? |
Pruritus measurements (numeric rating scale, visual dynamic pruritus score, and 5-D itch scale) indicated an immediate and long-lasting positive effect of hydrotherapy compared with control patients. |
Pruritus and psoriasis gene and protein biomarkers measured in lesional and nonlesional skin revealed a significant decrease of inflammation biomarkers (IL-8, IL-1α, IL-1RA, and RANTES), of psoriasis biomarkers (PI3, S100A7, and IL-17), and of pruritus biomarkers (IL-31, TRPV1, and CGRP1). |
This study demonstrated there was an immediate and long-lasting improvement of pruritus in patients with psoriasis who underwent hydrotherapy. |
Introduction
Psoriasis is one of the most common chronic inflammatory skin diseases, and plaque psoriasis is by far the most common clinical form of psoriasis [1, 2]. Management of psoriasis is challenging, particularly in pediatric and elderly patients, although recent reports suggest effective and safe treatments are available for moderate-to-severe forms of psoriasis in these populations [3, 4]. Although previously overlooked as a common symptom of psoriasis, it is now recognized that most patients with psoriasis suffer from pruritus [5]. Moreover, psoriatic itch has been described as the most bothersome symptom of the disease. It can occur on any part of the body, or even the entire body surface, and be limited to psoriatic plaques but often, uninvolved skin is also affected [5, 6]. Most studies in psoriasis have reported itch of moderate severity across various patient populations, although the severity can range from mild to severe. Psoriatic itch has been shown to significantly impact the quality of life, work productivity, emotional well-being, and quality of sleep [7, 8]. Indeed, clinical trials relating to psoriasis now include measurements of itching as a study outcome in addition to the psoriasis area and severity index (PASI) score [7]. The latter parameter is a common measure of psoriasis severity but it is not necessarily correlated with the level of itching [9], and thus should not be used as a stand-alone parameter for assessing clinical outcomes of psoriasis treatments.
Treatments for itch vary in their efficacy, e.g., moisturizers, antihistamines, and topical retinoids have limited efficacy in patients with psoriasis, whereas oral biopharmaceuticals and topical corticosteroids and vitamin D analogs have proved more effective [7]. However, there is no single antipruritic therapy dedicated specifically to treat itching in psoriasis [1]. One approach that may be considered as an adjunct to treatments is hydrotherapy. A source of this is Avène thermal spring water, a low mineral water used for centuries for its beneficial effects on the skin [10]. It has been shown in clinical trials to be effective in alleviating subjective and physical symptoms of chronic skin diseases or conditions when used in combination with treatments [11,12,13]. As a result, the therapeutic properties of Avène thermal spring water have been harnessed to enable alleviation of various skin conditions, such as hydrotherapy and the development of topical products from the water components [14, 15].
The aim of this study was to assess the benefit of Avène thermal spring water hydrotherapy on chronic pruritus associated with plaque psoriasis in addition to the patients’ usual psoriasis and/or pruritus management (i.e., treatments and/or skin care products). The clinical benefits of hydrotherapy were evaluated with respect to its impact on pruritus according to several clinical assessment methods [numeric rating scale (NRS), dynamic pruritus score (vDPS), and 5-D itch scale], as well as psoriasis severity using the PASI score. Several markers for itching have been linked to neuronal mechanisms, e.g., nerve growth factor [16], substance P [17], and neuropeptide Y [18]; inflammatory mediators (e.g., IL-31 [19]; and other factors, e.g., opioid and GABA receptors, adhesions molecules, etc. [7]. Measurements of biomarkers can thus be used to evaluate the outcome of therapies in clinical trials. Here, pruritus and psoriasis biomarkers were measured in lesional and nonlesional skin using a noninvasive sample collection method.
Methods
Ethical Approval
The study was conducted as an international, interventional, multicenter, open-label trial carried out in adults with plaque psoriasis associated with moderate-to-very-severe chronic pruritus.
The patients in this manuscript have given written informed consent to participate in the study. The trial was conducted according to the Declaration of Helsinki (1964) and its subsequent amendments, Good Clinical Practices (CPMP/ICH/135/95), and national regulations. This protocol and related documents (including the informed consent form) have been subjected to independent ethics committee and competent authority before the study setup. This clinical study began only after getting the favorable opinion of the ethics committee and the authorization of the competent authority. All security measures required for this type of study have been implemented according to the procedures applicable in the centers. The trial was registered with ClinicalTrials.gov (trial number NCT03023254).
Inclusion and Exclusion Criteria
The main inclusion criteria were chronic pruritus for at least 6 weeks due to plaque psoriasis, moderate-to-very-severe chronic pruritus [numerical rating scale (NRS) score ≥ 4] over the previous 3 days, and stable systemic and/or topical treatments for psoriasis and/or pruritus until the end of the hydrotherapy period. Main exclusion criteria were patients with an acute, chronic or progressive disease other than plaque psoriasis that could be the origin of the pruritus according to investigator’s assessment, with any other systemic or topical treatment or skin care product liable to interfere with pruritus, and psoriasis established or modified.
The choice of group was made according to the subject’s availability for hydrotherapy, providing the subjects met the eligibility criteria described below. The decision and criteria were verified by the investigator.
Hydrotherapy Group
In the hydrotherapy group, the patients had to undergo 3 weeks of Avène thermal spring water hydrotherapy at the Avène hydrotherapy center, in addition to their usual management of psoriasis and/or pruritus. The hydrotherapy care included a complete individualized set of treatments including general and specific cares. For most subjects, the daily hydrotherapy was on the whole body (71%), using general showers (100% of subjects), general sprays (96%), hydromassage baths (92%), and filiform showers (85%). Some subjects (29%) underwent hydrotherapy on a specific body area, e.g., the scalp [using scalp spraying (73% of subjects) or scalp wraps (23%)].
Control Group
The control group did not undergo hydrotherapy and continued to follow their usual daily management of psoriasis and/or pruritus.
Concomitant Treatments between Visit 1 and 2 (V1 and V2; Hydrotherapy Period)
For both groups, the following treatments and skin care products were prohibited: biotherapy treatment, phototherapy or psoralen and ultraviolet A (PUVA) therapy treatment, psoriasis treatment by laser, establishment or modification (i.e., a change of dose and/or frequency) of systemic or topical treatment taken/applied for psoriasis or pruritus management, modification or establishment of skin care product applied for psoriasis or pruritus management for other reason than hydrotherapy medical care. For the control group, hydrotherapy was prohibited.
For both groups, from V1 to V2, patients had to keep their usual treatments and/or skin care products taken/applied for psoriasis and pruritus management, as well as treatments and/or skin care products liable to interfere with pruritus or psoriasis.
Concomitant Treatments between V2 and V4 (Follow-Up Period)
From V2 to V4, all treatments and/or skin care products were authorized. Treatments and/or skin care products for psoriasis and pruritus management were permitted if required, according to medical opinion and usual medical practice.
Study Design
The study consisted of five visits for the hydrotherapy group (V0, and V1–V4; V0 was a visit to select the patients before the hydrotherapy). There were four visits for the control group (V1–V4). For both groups, visit 1 (V1) was the inclusion visit on day 1 (baseline) and was the start of hydrotherapy (for the hydrotherapy group only). Visit 2 (V2) was after 3 weeks with or without hydrotherapy, at which time, hydrotherapy stopped. There were two subsequent follow-up visits, 3 and 6 months after hydrotherapy, during which patients were allowed to take/apply any treatment or product (in contrast to the first 3 week period). Visits V1 and V2 were conducted at the Avène hydrotherapy center for the hydrotherapy group, all other visits were conducted at the “peripheral centers” (French and Spanish dermatological centers).
Efficacy Endpoints
Pruritus Clinical Criteria
Pruritus NRS [20] was used to measure (1) the mean and (2) the worst pruritus intensity over the previous 3 days on V1, V2, V3, V4, and weekly at home between V2 and V4, and (3) the mean NRS over the previous 24 h between V1 and V2.
The vDPS was used to assess the change of pruritus intensity compared with the baseline (on V1) [21].
Pruritus characteristics reported by the patients regarding the degree, duration, direction, disability, and distribution of itching were assessed using the five dimensions (5-D) itch scale as described previously [22].
Psoriasis Clinical Criterion
The PASI was used as a quantitative rating score for measuring the severity of psoriatic lesions based on area coverage and plaque appearance [23].
Quality-of-Life Criterion
The “itchy quality of life” (ItchQoL) scale was used to assess quality-of-life (QoL) impact related to itch [24].
Biomarker Analyses
A panel of biomarkers present in lesional and nonlesional skin were measured using transcriptomic analysis and protein detection using enzyme-linked immunosorbent assay (ELISA) . A list of the biomarkers, their role in itching and immune responses, and their reported modulation (up- or downregulation) in psoriasis lesions are listed in Supplementary Table 1.
Samples were collected using micro-abrasive (two nail files of a 5 cm2 area per zone) and noninvasive (four cotton swabs of a 10 cm2 area per zone) sampling of lesional skin and nonlesional skin on V1, V2, and V3 (six samples per donor per visit).
Transcriptomic analysis was conducted by droplet digital PCR (ddPCR), as a sensitive, precise and absolute nucleic acid quantification of low-abundance targets. The extraction protocols of nucleic acids, as well as the reverse transcriptase and ddPCR steps are listed in Supplementary Table 2. The amount of each gene was normalized to the reference housekeeping gene.
Proteins involved in psoriasis and pruritus were analyzed by ELISA/multiplex. Proteins were extracted from swabs using phosphate-buffered saline (PBS)/Triton buffers. The proteins were quantified using the Procartaplex kit (Cytokine 10-Plex Human Panel; ThermoFischer, France). The amount of protein was expressed in pg/ml.
Statistical Analyses
The full analysis set consisted of all patients included with an evaluation on V2. This set was used to perform the analyses of efficacy. To estimate the change between groups, a mixed model repeated measures was made with group, visit, and interaction group × visit as a fixed factor, patient and center as random factors, and baseline as covariate, on changes between V1 and other visits. Comparisons at each time were made using the differences on estimated means. The statistical analyses described were the same for all endpoints, including the biomarkers.
Results
Patient Demographics and History of Psoriasis and Pruritus
All patients suffered from chronic pruritus due to plaque psoriasis at enrollment, according to the inclusion criteria. Pruritus was only located at the plaque psoriasis for most patients (87.0% and 66.7% of the hydrotherapy and control patients, respectively). Most patients reported that the evening or night was the time of day when itching was the most frequent (77.2% and 80.0% of the hydrotherapy and control patients, respectively).
Both groups were comparable in terms of demographics (see Table 1 for a summary of the characteristics of both groups). The “hydrotherapy group” consisted of 26 patients [13 males, 13 females, 29–80 years (mean 57.8 years)] and the control group consisted of 18 patients [9 males, 9 females, 32–74 years (mean 52.7 years)]. The groups had comparable phototypes: patients in the hydrotherapy group were phototype II (38.5%) and III (38.5%) and patients in the control group were phototype II (44.4%) and III (44.4%). The groups were also comparable regarding psoriasis and pruritus characteristics, and plaque psoriasis location at inclusion. Finally, the psoriasis severity of hydrotherapy patients was marginally higher than the control patients (the PASI was 14.1 in the hydrotherapy group and 11.9 in the control group).
Treatments at Inclusion and during the Study
The most common treatment for psoriasis and pruritus management at inclusion was topical corticosteroid and/or vitamin D analog treatment (at least one topical treatment for 46% of patients in the hydrotherapy group and 67% in the control group). Few patients took oral treatments [respectively for hydrotherapy and control groups: apremilast (4% and 6%), methotrexate (4% and 6%), acitretin (8% and 0%), antihistaminic (8% and 0%)].
During the first period of the study (hydrotherapy period), more patients in the control group (22%) started a treatment for the psoriasis and/or pruritus management (17% of patients started to apply corticosteroid–calcipotriol combination and 6% corticosteroids) than in the hydrotherapy group (4% of patients took antihistamines), despite the protocol recommendations to keep the usual treatments during the first period. More patients in the hydrotherapy group (85%) started skin care products (including emollients and protectives), which was expected because these care products are mainly applied and/or prescribed during the usual hydrotherapy care, than in the control group (11%) (Supplementary Table 3). Treatments started during the second period are described in Supplementary Table 3.
Efficacy
Pruritus Numerical Rating Scale (NRS)
In the control group, the mean pruritus intensity (on average over the previous 3 days) assessed on V2, V3, and V4 was decreased compared with V1 by 2.6%, 20.6%, and 19.6%, respectively, which was statistically significant only on V3 (p = 0.0392) and V4 (p = 0.0347) (Fig. 1i). In the hydrotherapy group, the mean pruritus intensity was more markedly decreased and was evident at the end of the 3 week hydrotherapy on V2, an effect which was sustained over the remaining visits (the mean pruritus intensity was statistically significantly decreased (p = 0.0001) on V2, V3, and V4 compared with V1 by 50.4%, 53.4%, and 47.7%, respectively). The decrease in mean pruritus intensity was also statistically significantly higher in the hydrotherapy group compared with the control group on V2 (p = 0.0002), V3 (p = 0.0053), and V4 (p = 0.0228).
Change in (i) the mean and (ii) the worst pruritus intensity over the previous 3 days using the pruritus numerical rating scale (NRS). Values are a mean, with statistical differences (intragroup and intergroup statistical analyses) shown as *p < 0.05, **p < 0.001. HYDRO hydrotherapy group, CON control group, V1–4 visits 1–4
In the control group, there was a small decrease of 3.4% in the worst pruritus intensity (over the previous 3 days) on V2 compared with V1; however, this was not statistically significant (p > 0.0500). On V3 and V4, there was a higher decrease compared with V1 of 27.2% and 19.6%, respectively, which was only statistically significant on V3 (p = 0.0129) (Fig. 1ii). In the hydrotherapy group, decreases in the worst pruritus intensity on V2, V3, and V4 compared with V1 were 44.0%, 49.0%, and 48.4%, respectively, all of which were statistically significant from V1 (p < 0.0001). The decreases in worst pruritus intensity were also statistically significantly higher in the hydrotherapy group compared with the control group on V2 (p = 0.0018) and V4 (p = 0.0185).
On V2, the mean pruritus intensity on average over the previous 24 hours had significantly decreased by 50.8% in the hydrotherapy group (p = 0.0124) and increased by 10.4% in the control group (not significant).
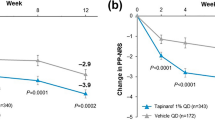
Pruritus: vDPS
Based on the vDPS, hydrotherapy was reported by the patients to have a positive impact on changes in their pruritus intensity, which was significantly improved on V2 by +58.2% (p < 0.0001) (Fig. 2). By contrast, patients in the control group reported a significant worsening of the mean pruritus intensity by −31.0% on V2 (p = 0.0143). The improvement in the hydrotherapy group was also observed on V3 and V4, with statistically significant pruritus intensity changes of +57.9% (p < 0.0001) and +23.6% (p = 0.0230), respectively. Patients in the control group reported the pruritus intensity to have marginally but not statistically significantly improved on V3 (+8.6%, p > 0.0500) but worsened on V4 (−10.7%, p > 0.0500). All changes reported by the patients were also statically significantly higher in the hydrotherapy group compared with the control group on V2, V3, and V4.
Change of pruritus intensity compared with baseline assessed with the visual dynamic pruritus score (vDPS). Values are a % change, with statistical differences (intragroup and intergroup statistical analyses) shown as *p < 0.05, **p < 0.001. HYDRO hydrotherapy group, CON control group, V2–4 visits 2–4
Pruritus Characteristics: 5-D Itch Scale
Figure 3 shows the impact of hydrotherapy on pruritus characteristics according to the 5-D itch scale evaluated on different visits. In the hydrotherapy group, the 5-D score was statically significantly improved (p < 0.001) on V2, V3, and V4 compared with V1 by 33.0%, 33.7%, and 30.7%, respectively. By contrast, there was no statically significant change in the 5-D score in the control group. The decrease in the 5-D score was statistically significantly higher in the hydrotherapy group compared with the control group on each visit.
The sleep-related question in the 5-D itch scale indicated that hydrotherapy improved sleep for 72.0% of patients on V2, with the remaining 28.0% reporting no change (Fig. 4). By contrast, only 11.8% of patients in the control group reported an improvement in sleep on V2. Moreover, 17.7% of patients in the control group reported a worsening of sleep on V2. A similar finding was observed on V3 and V4, whereby 65.4% and 60.9% of the patients in the hydrotherapy group reported improved sleep, respectively, compared with only 25.0% and 23.5% of the patients in the control group, respectively.
Impact of hydrotherapy on the quality of sleep evaluated in the 5-D itch scale questionnaire. Values are the % of patients in the hydrotherapy (HYDRO) and control (CON) groups reporting a worsening (red), no change (gray), or improved (green) sleep on different visits. HYDRO hydrotherapy group, CON control group, V2–4 visits 2–4
Psoriasis Severity: PASI
The PASI value was statistically significantly decreased by 40.0% compared with V1 after the 3 week hydrotherapy treatment (p < 0.0001) (Fig. 5). The severity was also statistically significantly decreased on V3 and V4 compared with V1 in the hydrotherapy group (p < 0.0001, by 47.2% and 40.8%, respectively). The PASI was also statistically significantly decreased on V2, V3, and V4 compared with V1 in the control group, with no statistical difference in the change in PASI between control and hydrotherapy groups. Patients undergoing hydrotherapy had to maintain their usual treatment during this period, whereas over the same period, 22% of patients in the control group used, mainly for a short duration, a topical treatment (corticosteroid or corticosteroid–calcipotriol combination). This was notable since the psoriasis severity on V1 of the control group was lower than the hydrotherapy group (11.89 in the control compared with 14.14 in the hydrotherapy group).
Change of psoriasis severity measured using the psoriasis area and severity index (PASI) score. Values are a mean, with statistical differences (intragroup and intergroup statistical analyses) shown as *p < 0.05, **p < 0.001, ns not significant p > 0.05. HYDRO hydrotherapy group, CON control group, V1–4 visits 1–4
Quality of Life (QoL)
The QoL of patients in the hydrotherapy group was statistically significantly improved by V2, according to the ItchQoL questionnaire (the mean ItchQoL value was decreased by 35.7% compared with V1, p < 0.0001) (Fig. 6). By contrast, the QoL of patients in the control group was not statistically different on V2 compared with V1. The ItchQoL value was also statistically significantly lower (p < 0.0001) on V3 and V4 compared with V1 in the hydrotherapy group (with a decrease of 32.5% and 26.7%, respectively). The decreases on V3 and V4 compared with V1 in the control group were only 13.7% and 6.1%, respectively, and only reached statistical significance on V3 (p = 0.0224). All ItchQoL value were also statically significantly lower in the hydrotherapy group compared with the control group on V2, V3, and V4 (p < 0.0500).
Biomarkers
The expression of mRNA biomarkers linked to itch (IL31, SEMA3A, TRPV1, and CGRP1/CALCA), as well as the cytokines, IL17A and IL8 and the AMPs for anti-microbial peptides (AMPs), PI3, and S100A7, in lesional and nonlesional skin is shown in Fig. 7i. The expression of all biomarker genes, except TRPV1, was much higher in lesional than nonlesional skin on all visits. In addition, the changes of expression levels of all biomarkers in nonlesional skin were similar in hydrotherapy and control patients on all visits (except PI3 and S100A7on V2). In lesional skin, the expression levels of biomarkers in hydrotherapy and control patients were similar or marginally higher on V2 compared with V1. By contrast, on V3, the expression levels in lesional skin decreased compared with V1 in patients who underwent hydrotherapy but not in control patients. In addition, the biomarker expression levels of three biomarkers (IL8, PI3, and S100A7) were lower than those in control patients on V3.
The protein biomarker expression of the cytokines, IL17A/F, IL8, IL1α, IFNγ, and IL1RA and the chemokine, RANTES, in lesional and nonlesional skin is shown in Fig. 7ii. In accordance with the gene expression, protein levels of IL17A/F and IL8 were higher in lesional than nonlesional skin. Likewise, the protein expression of IL1RA and RANTES were also higher in lesional than nonlesional skin. In lesional skin, the biomarker protein levels in hydrotherapy and control patients were similar or marginally higher on V2 compared with V1. By V3, the protein levels of all except one biomarker in lesional skin of hydrotherapy patients decreased compared with V1. The exception was IFNγ, which remained at a low level in hydrotherapy patients but increased in lesional skin of control patients. The levels of IL17A/F, IL8, IFNγ, and RANTES on V3 were all lower in lesional skin of hydrotherapy patients compared with control.
Discussion
This study evaluated the beneficial effects of Avène thermal spring water hydrotherapy on patients with pruritic plaque psoriasis. To our knowledge, this is the first time such an evaluation has been reported. The mean pruritus intensity of the patients at inclusion was moderate but greater than 6; moreover, the worst pruritus intensity was severe to very severe, both reflecting the significant prevalence of this unpleasant symptom in psoriasis.
Results from the NRS, vDPS, and 5-D itch scale measurement indicated an immediate, marked, and long-lasting positive effect of hydrotherapy on the pruritus intensity compared with the intensity recorded at inclusion and compared with control patients. By contrast, pruritus intensity in control patients tended to worsen over the visits according to the vDPS. The QoL assessed by the patients according to ItchQoL scale was also shown to improve directly after hydrotherapy and was still much improved even 6 months later. By contrast, the QoL of patients in the control group was only minimally affected, if at all. Of note, one of the questions in the ItchQoL questionnaire relates to sleep quality, which is reported to be impacted in patients with psoriasis [7]. Indeed, control patients in this study reported no change or even a worsening of the quality of sleep over the four visits. By contrast, hydrotherapy had a positive impact on sleep, with most patients in this group reporting an improvement in their quality of sleep.
Merial-Kieny et al. previously conducted a large clinical efficacy trial over 8 years in atopic and/or psoriatic patients to determine the impact of 3 weeks of Avène thermal spring water hydrotherapy on their disease [12]. They showed a significant reduction in PASI by 54.4% directly after the 3 week hydrotherapy in a cohort of 4487 patients with psoriasis. This study provided good evidence that the condition of the skin was improved by hydrotherapy. The current study includes a concurrent control, i.e., patients using their normal treatments and skin products but without hydrotherapy, and the persistence of the effects on parameters relating to pruritus, psoriasis, and the QoL over 6 months. In accordance with the findings of Merial-Kieny et al., there was a marked decrease in the PASI at the end of 3 weeks hydrotherapy. The initial improvement of psoriasis severity by hydrotherapy observed on V2 was shown to be sustained over time, with similar decreases in the PASI after the 3 and 6 month follow-up visits to that measured immediately after the 3 week hydrotherapy. There was no statistically significant difference between the hydrotherapy and control groups, while a marked difference in the evolution of PASI was observed, which was decreased on V2 by 40% in the hydrotherapy group compared with only 16.5% in the control group. Of note, the PASI in the control group was lower than the hydrotherapy group on V1 (11.89 in the control compared with 14.14 in the hydrotherapy group) and 22% of patients in the control group used a topical treatment during the hydrotherapy period, even though the management of the condition was required to be maintained in this period. Another indication of the beneficial effects of hydrotherapy was indicated by the treatments used by patients during the follow-up period. Indeed, more patients in the control than in the hydrotherapy group started at least one systemic and/or topical treatment for psoriasis and/or pruritus management (data not shown). Therefore, the improvement in pruritus and associated QoL in this period could not be attributed to medical treatment but to hydrotherapy.
Analysis of gene and/or protein biomarkers revealed a significant decrease of inflammation biomarkers (IL-8, IL-1α, IL-1RA, and RANTES), of psoriasis biomarkers (PI3, S100A7, and IL-17), and of pruritus biomarkers (IL-31, TRPV1, and CGRP1). These effects were mainly observed after a 3 month follow-up period (V3), rather than being an immediate effect (i.e., after hydrotherapy on V2). One consideration for future studies is the nature of the sampling (which was noninvasive in these studies) as well as the state of the skin during the sampling (hyperkeratosis versus nonlesional skin), which could explain a smaller difference between the presence of some targets in lesional compared with nonlesional skin. In addition, measurement of biomarkers on the skin surface could be impacted by exposure to nucleases (mRNA) or their half-life (protein). All but one of the biomarkers measured were expected (based on the literature) to be upregulated in lesional skin of patients with psoriasis, which was confirmed in this study, and they were positively modulated by hydrotherapy during a long-term effect. The exception to this is SEMA3A, which is reported to be downregulated in lesional psoriasis skin [25, 26]; however, the gene expression of this biomarker was generally higher in patients with lesional than nonlesional skin. The reason for the expression of this biomarker being different from literature findings may be due to the nature of the lesional skin (e.g., hyperkeratosis), as well as differences in the method of analysis, i.e., gene expression in these studies compared with immunohistochemistry detection of the protein by others [25, 26].
A particular strength of this study is that it includes concurrent control patients with similar characteristics upon inclusion to patients in the hydrotherapy group, so that changes in clinical and subjective observations could be better attributed to hydrotherapy. In addition, the gene expression information in this study provided a nonsubjective insight into the mechanisms by which hydrotherapy may work, e.g., by decreasing inflammation. The main weakness of the study is the small number of patients in both groups, which impacts the statistical robustness. However, since this was intended to be an initial pilot study, it was considered to be sufficiently informative to lead the way to further, more comprehensive, studies to confirm the beneficial effects of hydrotherapy. Another weakness is that the study was not randomized as the hydrotherapy group depended on the subjects’ availability; nevertheless, the characteristics of the patients in both groups at baseline were comparable.
Conclusions
These results demonstrated the subjective and objective beneficial effects of Avène thermal spring water hydrotherapy on moderate-to-severe pruritus and the associated QoL in plaque psoriasis after a 3 week course. The improvement persisted for 6 months after the end of the hydrotherapy, which was demonstrated using several clinical efficacy and biomarker measurements. These findings support the inclusion of hydrotherapy as a complementary therapy in the management of pruritus of patients with psoriasis.
References
Szepietowski JC, Reich A. Pruritus in psoriasis: an update. Eur J Pain. 2016;20(1):41–6.
Menter A, Gottlieb A, Feldman SR, Van Voorhees AS, Leonardi CL, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58(5):826–50.
Megna M, Camela E, Battista T, Genco L, Martora F, Noto M, et al. Efficacy and safety of biologics and small molecules for psoriasis in pediatric and geriatric populations. Part II: focus on elderly patients. Expert Opin Drug Saf. 2023;22(1):43–58.
Megna M, Camela E, Battista T, Genco L, Martora F, Noto M, et al. Efficacy and safety of biologics and small molecules for psoriasis in pediatric and geriatric populations. Part I: focus on pediatric patients. Expert Opin Drug Saf. 2023;22(1):25–41.
Yosipovitch G, Goon A, Wee J, Chan YH, Goh CL. The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br J Dermatol. 2000;143(5):969–73.
Szepietowski JC, Reich A, Wiśnicka B. Itching in patients suffering from psoriasis. Acta Dermatovenerol Croat. 2002;10(4):221–6.
Elewski B, Alexis AF, Lebwohl M, Stein Gold L, Pariser D, Del Rosso J, et al. Itch: an under-recognized problem in psoriasis. J Eur Acad Dermatol Venereol. 2019;33(8):1465–76.
Stull C, Grossman S, Yosipovitch G. Current and emerging therapies for itch management in psoriasis. Am J Clin Dermatol. 2016;17(6):617–24.
Roblin D, Wickramasinghe R, Yosipovitch G. Pruritus severity in patients with psoriasis is not correlated with psoriasis disease severity. J Am Acad Dermatol. 2014;70(2):390–1.
Guerrero D, Garrigue E. Avène’s thermal water and atopic dermatitis. Ann Dermatol Venereol. 2017;144(Suppl 1):S27-s34.
Nocera T, Jean-Decoster C, Georgescu V, Guerrero D. Benefits of Avène thermal hydrotherapy in chronic skin diseases and dermatological conditions: an overview. J Eur Acad Dermatol Venereol. 2020;34(Suppl 5):49–52.
Merial-Kieny C, Mengual X, Guerrero D, Sibaud V. Clinical efficacy of Avène hydrotherapy measured in a large cohort of more than 10,000 atopic or psoriatic patients. J Eur Acad Dermatol Venereol. 2011;25(Suppl 1):30–4.
Goldman MP, Merial-Kieny C, Nocera T, Mery S. Comparative benefit of two thermal spring waters after photodynamic therapy procedure. J Cosmet Dermatol. 2007;6(1):31–5.
Selas B. History of thermalism at Avène-les-Bains and genesis of the Avène thermal spring water. Ann Dermatol Venereol. 2017;144(Suppl 1):S21–6.
Ribet V, Mielewczyk E, Sirvent A, Georgescu V, Rossi AB. A novel dermo-cosmetic product containing thermal spring water, sucralfate, copper sulfate, and zinc sulfate in the management of hand eczema. Clin Cosmet Investig Dermatol. 2018;11:373–81.
Nakamura M, Toyoda M, Morohashi M. Pruritogenic mediators in psoriasis vulgaris: comparative evaluation of itch-associated cutaneous factors. Br J Dermatol. 2003;149(4):718–30.
Chang SE, Han SS, Jung HJ, Choi JH. Neuropeptides and their receptors in psoriatic skin in relation to pruritus. Br J Dermatol. 2007;156(6):1272–7.
Reich A, Orda A, Wiśnicka B, Szepietowski JC. Plasma neuropeptides and perception of pruritus in psoriasis. Acta Derm Venereol. 2007;87(4):299–304.
Czarnecka-Operacz M, Polańska A, Klimańska M, Teresiak-Mikołajczak E, Molińska-Glura M, Adamski Z, et al. Itching sensation in psoriatic patients and its relation to body mass index and IL-17 and IL-31 concentrations. Postepy Dermatol Alergol. 2015;32(6):426–30.
Storck M, Sandmann S, Bruland P, Pereira MP, Steinke S, Riepe C, et al. Pruritus Intensity Scales across Europe: a prospective validation study. J Eur Acad Dermatol Venereol. 2021;35(5):1176–85.
Fritz F, Blome C, Augustin M, Koch R, Ständer S. Differences in patient and physician assessment of a dynamic patient reported outcome tool for chronic pruritus. J Eur Acad Dermatol Venereol. 2016;30(6):962–5.
Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. Br J Dermatol. 2010;162(3):587–93.
Mattei PL, Corey KC, Kimball AB. Psoriasis Area Severity Index (PASI) and the Dermatology Life Quality Index (DLQI): the correlation between disease severity and psychological burden in patients treated with biological therapies. J Eur Acad Dermatol Venereol. 2014;28(3):333–7.
Patel KR, Singam V, Vakharia PP, Chopra R, Sacotte R, Patel N, et al. Measurement properties of three assessments of burden used in atopic dermatitis in adults. Br J Dermatol. 2019;180(5):1083–9.
Kou K, Nakamura F, Aihara M, Chen H, Seto K, Komori-Yamaguchi J, et al. Decreased expression of semaphorin-3A, a neurite-collapsing factor, is associated with itch in psoriatic skin. Acta Derm Venereol. 2012;92(5):521–8.
Tominaga M, Ogawa H, Takamori K. Decreased production of semaphorin 3A in the lesional skin of atopic dermatitis. Br J Dermatol. 2008;158(4):842–4.
Acknowledgements
We thank the participants of the study.
Editorial assistance
Pierre Fabre funded the editorial assistance of Nicola J. Hewitt (SWS, Wingertstrasse 25, 64390 Erzhausen, Germany).
Author contributions
Marie-Dominique Thouvenin, Adeline Bacquey, Marine Babin, Fabrice Lestienne, Christophe Lauze, Eléonore Gravier, Diana Placintescu, and Sonja Ständer contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Marie-Dominique Thouvenin, Adeline Bacquey, Marine Babin, Fabrice Lestienne, Christophe Lauze, Eleonore Gravier, and Ariadna Ortiz-Brugués. The draft of the manuscript was revised and commented on by all authors. All authors read and approved the final manuscript. The authors would also like to thank the following people: Catherine Jean Decoster,Victor Georgescu and Cécile Delsol (Medical Direction, Laboratoires Dermatologiques Avène, Lavaur, France), and Jennifer Theunis (Pierre Fabre Dermo-Cosmétique), for thoughtful discussions about the study design and/or the manuscript review; Marie Bosredon, Emeline Laborel (Pierre Fabre Dermo-Cosmétique), Marielle Magras, Sophie Douet-Pagnon, and Monique Anguissa (EURAXIPHARMA) for monitoring the study; Dominique NDeli (Axiodis) and the Soladis team for the data management; and all the study investigators and their co-investigators for recruiting and evaluating the patients. Scientific writing was provided by Nicola J. Hewitt and funded by Pierre Fabre Dermo-Cosmétique.
Funding
This study was funded by Pierre Fabre. The Rapid Service Fee was funded by Pierre Fabre.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Marie-Dominique Thouvenin, Adeline Bacquey, Marine Babin, Fabrice Lestienne, Christophe Lauze, Eléonore Gravier, and Ariadna Ortiz-Brugués are employees of Pierre Fabre Dermo-Cosmétique. Sonja Ständer is an employee of the University Hospital Münster, Germany. The authors report no other conflicts of interest in this work.
Ethical approval
The patients in this manuscript have given written informed consent to participate in the study. The trial was conducted according to the Declaration of Helsinki (1964) and its subsequent amendments, Good Clinical Practices (CPMP/ICH/135/95) and national regulations. This protocol and related documents (including the informed consent form) have been subjected to independent ethics committee and competent authority before the study setup. This clinical study began only after getting the favorable opinion of ethics committee and the authorization of competent authority. All security measures required for this type of study have been implemented according to the procedures applicable in the centers. The Trial was registered with ClinicalTrials.gov (trial number NCT03023254).
Additional information
Prior Presentation
Dubai World Dermatology and Laser Conference and Exhibition–Dubai Derma. Dubai, United Arab Emirates, 2021. Journées Nationales Provinciales de Dermatologie. Rennes, France, 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Thouvenin, MD., Bacquey, A., Babin, M. et al. Efficacy of Avène Hydrotherapy on Chronic Pruritus in Patients with Plaque Psoriasis. Dermatol Ther (Heidelb) 13, 3137–3151 (2023). https://doi.org/10.1007/s13555-023-01047-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01047-2