Abstract
Psoriasis is a chronic, immune-mediated inflammatory disease with a worldwide prevalence ranging between 0.51 and 11.43%. It results in a large clinical and social burden, with patients frequently suffering from reduced quality of life, psychologic distress and debilitating comorbidities. Biologic agents are used to establish and maintain disease control in patients with moderate-to-severe psoriasis and are essential to improving quality of life. However, a substantial proportion of patients have limited access to therapy due to economics, health policies and clinical considerations, which creates clinical unmet needs that disadvantage both patients and healthcare professionals. Biosimilars are a cost-effective alternative to off-patent biologic therapies, and there is mounting evidence to suggest they offer a valuable pharmacoeconomic strategy to lower healthcare costs in patients with psoriasis. Furthermore, the introduction of biosimilars can increase the number of patients able to receive biologics, allowing these patients to be treated earlier in the disease course, potentially modifying the course of their disease and reducing the risk of comorbidities. In time, the emergence of additional data, particularly those related to long-term safety, efficacy in extrapolated indications and the effects of switching, should reassure physicians and help overcome the final hurdles for a wider implementation of biosimilars. This review aims to provide an overview of current treatment approaches for patients with moderate-to-severe psoriasis in the biosimilars era and explores both the current challenges and potential opportunities to improve access to high-quality, effective treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A substantial proportion of patients with moderate-to-severe psoriasis have limited access to effective biologic therapy due to economics, health policies and clinical considerations, which creates clinical unmet needs that disadvantage both patients and healthcare professionals. |
Biosimilars are a more cost-effective alternative to off-patent biologics, and mounting evidence suggests they offer a valuable pharmacoeconomic strategy to lower healthcare costs in patients with psoriasis. |
Within IMIDs, including psoriasis, biosimilars have been proven to increase access to biologic therapy, facilitate treatment earlier in the course of the disease and decrease comorbidities. |
The approval and adoption of cost-effective biosimilars more widely and earlier in the treatment armamentarium for psoriasis have the potential to significantly improve patients’ outcomes while controlling increasing healthcare costs and providing more affordable therapeutic options for patients. |
Introduction
Psoriasis is a chronic, immune-mediated inflammatory disease (IMID) of the skin that affects an estimated 7.8 million adults in Europe [1] with a worldwide prevalence ranging between 0.51 to 11.43% [2], resulting in a large clinical and social burden with patients frequently suffering from reduced quality of life (QoL), psychologic distress and debilitating comorbidities [3, 4]. The clinical burden of psoriasis increases with disease severity, high impact site involvement and level of comorbidity, and is greatest for patients with moderate-to-severe disease, which accounts for approximately 20–30% of psoriasis patients [5, 6].
A broad number of oral, subcutaneous and intravenous systemic immunomodulatory agents are currently available for psoriasis treatment within Europe [3]. These include traditional synthetic (TS), biological and modern synthetic agents, that are used to establish and maintain disease control in moderate-to-severe psoriasis (Table 1). However, a substantial proportion of patients have limited access to biologic therapy due to economics, health policies and clinical considerations [7,8,9]. Recently, biosimilars have provided a more cost-effective alternative to off-patent biologic therapies within IMIDs, including psoriasis [10, 11]. In particular, evidence is mounting to confirm the use of biosimilars as a valuable pharmacoeconomic strategy to lower healthcare cost in patients with psoriasis [6, 12, 13], thereby allowing the use of biologics by a wider group of patients and earlier in the disease course.
This review aims to provide an overview of current treatment approaches for patients with moderate-to-severe psoriasis in the biosimilars era and explore both the current challenges and potential opportunities to improve access to high-quality, effective treatments.
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Current Clinical Practice Across Europe (Assessed January 2023)
Current evidence-based European and national psoriasis guidelines recommend topical agents in mild forms of psoriasis. TS agents are considered first-line treatments in moderate-to-severe disease, with biologic therapies recommended when TS agents are not tolerated or provided inadequate disease control (Table 2).
In some countries such as Germany, Italy and Spain, the threshold for the use of biologic therapies is progressively lowering, and they are recommended first line in cases of psoriasis where TS treatments are not expected to lead to a sufficient response, e.g., particularly severe disease (Psoriasis Activity Score Index [PASI] ≥ 20; severe involvement of the nails, the genital area or the scalp), rapid worsening of disease or where there is a particularly strong impact on QoL [14]. In Italy, adalimumab is recommended as a first-line treatment for severe chronic plaque psoriasis in children (≥ 4 years old) and adolescents [15]. In Spain, the recently updated position of the Spanish Psoriasis Working Group on the use of biosimilars in moderate-to-severe psoriasis states that use of biosimilars as first-line therapies is appropriate in a high percentage of patients requiring biologic therapy, based on their ability to allow more patients to access effective treatment while reducing costs for healthcare systems [16]. However, the use of biosimilars first line must coexist with the evidence that there may be other biologics available that can provide better efficacy and safety, as demonstrated by the results of comparative clinical trials and meta-analyses. Therefore, in specific cases where no biosimilar is available, the option of using a first-line biologic drug should be available to physicians and patients [16]. Although it must be noted, the opportunity to lower the threshold only applies in countries where biologic therapies are reimbursed by the relevant National Health Service and where access may be limited.
Unmet Medical Needs and Potential Role of Biosimilars
Biologics have changed the treatment paradigm of IMIDs including psoriasis [17, 18], such that they are now firmly established in treatment guidelines and are recommended for patients with moderate-to-severe psoriasis either as first line or where initial treatment has failed [19, 20].
However, the high cost of these treatments has created clinical unmet needs that disadvantage both patients and healthcare professionals. These unmet needs include undertreatment, preventing access to treatment earlier in the disease course, which can in turn have a negative impact on the course of disease, the development of comorbidities, and the ability to sustain treatment responses [11].
Biosimilars have broadened the treatment armamentarium for a number of IMIDs and provide a more cost-effective treatment strategy for chronic diseases such as psoriasis (Table 3). The use of biosimilars could offer all eligible patients with psoriasis the opportunity to be treated in line with current guidelines and recommendations, thereby optimizing disease and comorbidity management [11, 21], including psoriatic arthritis (PsA) [13]. Furthermore, in addition to addressing the current unmet need, biosimilars could prompt considerations of their use earlier in the treatment course.
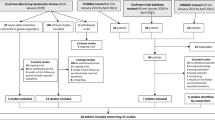
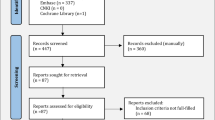
The approval of biosimilars by regulators is based on a robust biosimilarity exercise, encompassing a detailed analysis of quality attributes, functional testing and confirmatory clinical studies [22], where pharmacodynamic and pharmacokinetic similarities between the originator and its biosimilar are key to establishing biosimilarity [16]. Sufficient evidence now exists from clinical trials to demonstrate that biosimilars are as effective and safe as their reference products [23,24,25,26,27,28,29,30]. Recently, a comprehensive systemic review was conducted by Phan and colleagues to compare the efficacy and safety of biosimilars with originator biologics for the treatment of patients with psoriasis (all types). A total of 14 randomized clinical trials (10 adalimumab, 2 etanercept, 1 infliximab and 1 ustekinumab) and 3 cohort studies (1 adalimumab, 1 etanercept, 1 infliximab and etanercept) were included. The systematic analysis showed there were no clinically or statistically significant differences in rates of PASI 75 scores. Moreover, no significant difference was seen in the risks of adverse events at week 16 and week 52 between the comparators. In the cohort studies examined, no differences in effectiveness and safety outcomes between originators and biosimilars were shown in two studies, while one study reported more adverse events at 12 months in patients who switched to biosimilars of adalimumab [31].
Clinical trials are restricted by their inclusion criteria and size, which do not translate to the ‘real-world’ psoriasis population [32]. Thus, the evidence for the similarity of tolerability and efficacy of the biosimilar to the originator biologic is further strengthened through accumulating real-world evidence [10, 33,34,35,36,37,38,39,40,41]. Indeed, a substantial body of real-world evidence already exists in multiple indications, including psoriasis, providing confidence in biosimilar use in clinical practice [37,38,39,40]. Loft et al. examined the real-world effectiveness of adalimumab biosimilars (SB5 and GP2017) by assessing the 1-year drug retention in 348 patients switching to adalimumab biosimilars compared with 378 patients treated with adalimumab originator. Retention rates were 92.0% for the adalimumab biosimilar cohort and 92.1% for the adalimumab originator cohort, while hazard ratios between the cohorts were also similar (1.02 for all causes of drug discontinuation, 0.82 for insufficient effect and 1.41 for adverse events) [37]. A retrospective Spanish multicenter study was conducted to examine the real-world drug survival of adalimumab biosimilars (five adalimumab biosimilars) after 1 year in 581 patients with moderate-severe psoriasis, across 17 large hospitals representing different regions in Spain. In this study, results showed the mean (SD) PASI at the start of treatment with an adalimumab biosimilar was 7.4 (6.2) [35], which is lower than that reported in clinical trials. However, it should be noted that treatment in real-world practice is generally started with lower PASI values than those required in clinical trials because physicians are not obliged to impose a clearance interval during which the patient receives no topical or systemic therapy. Study data indicated drug survival in patients with long-standing good response to the originator who undergo non-medical switching to the corresponding biosimilar is better than in patients who start adalimumab biosimilar de novo (HR 6.146, p < 0.001) [35]. More recently, an observational cohort study in 4202 patients, utilizing data from the British Association of Dermatologists Biologics and Immunomodulators Register (BADBIR) to assess the incidence of switching to anti-TNF biosimilar agents in nine geographical regions across the UK, showed that the cumulative incidence of originator-to-biosimilar switching increased with time to 14.8%, 23.6% and 66.6% after 3 years. The 3-year switching rates varied from 0 to 43.7% for infliximab; from 0 to 40.4% for etanercept and from 12.5 to 84.3% for adalimumab. The adalimumab-naïve cohort included 528 patients of whom 67.8% started on biosimilars [42]. An Italian 72-week, real-life, retrospective study was conducted on 11 pediatric (< 18 years) and 23 geriatric (≥ 65 years) psoriasis patients treated with anti-TNF biosimilar agents (adalimumab and etanercept) to determine the efficacy and safety. The study found no statistically significant efficacy and safety differences between adalimumab and etanercept biosimilars in either children or the elderly [41].
In time, the emergence of additional effectiveness and safety data, particularly those related to long-term safety, efficacy in extrapolated indications and the effects of switching, should help overcome the final hurdles for a wider implementation of biosimilars by reassuring physicians and enabling well-informed decisions on questions such as switching [22, 43].
Cost Savings
The treatment of moderate-to-severe psoriasis with biologic agents poses a significant economic burden to healthcare systems [6, 12, 13, 44]. Despite increasing recognition of the potential of biologic therapies to reduce both direct and indirect healthcare costs in the long term, economic considerations focusing solely on drug acquisition costs mean that they often remain restricted to patients with only the most severe forms of disease. However, the cost of biosimilars in some countries is fast approaching the cost of TS agents and no longer represents an economic barrier [33]. A 2015 real-world, multinational, physician-perspective assessment of psoriasis and PsA surveying dermatologists (n = 391) and rheumatologists (n = 390) in North America (Canada and the US) and Europe (France, Germany, Italy, Spain and UK) reported one of the main reasons for not initiating biologics was related to cost [5]. A recent cost per responder analysis from the perspective of the National Health System in Italy compared adalimumab biosimilars MSB11022 and ABP 501 versus subcutaneous methotrexate (MTX) in 712 adult patients with moderate-to-severe chronic plaque psoriasis. Retention rates of ABP 501, MSB11022 and MTX at week 24 were 86%, 90% and 78%, and 81%, 82% and 63% at week 52, respectively. The cost per responder at week 24 was €674 for ABP 501, €366 for MSB11022 and €264 for MTX, respectively; at week 52, it was €1430 for ABP 501 €799 for MSB11022 and €652 for MTX, respectively. Overall, the results of this study show the 52-week cost-effectiveness of a biologic biosimilar is comparable to that of subcutaneous MTX [13].
Similarly, a cost per responder assessment of adalimumab biosimilars MSB11022, ABP 501 and MTX (either subcutaneous or oral) versus the originator for the treatment of moderate-to-severe plaque psoriasis showed the cost per responder for MSB11022 and ABP 501 compared to the originator was €500 versus €1831 and €968 versus €1949, respectively. In an indirect comparison among oral and subcutaneous MTX, MSB11022 and ABP 501, the costs per PASI75 responder at week 16 were 2%, 26%, 27% and 50% of that of the originator, respectively [6]. Another cost per responder analysis from Italy showed that the use of adalimumab biosimilars resulted in a 50–75% cost saving (€500–1000 vs €2000) after 16 weeks of treatment in patients who achieved a PASI75, PASI90 or PASI100 response from baseline [45].
A recent UK analysis followed a hypothetical cohort of patients over a lifetime to develop a cost-effectiveness model to determine the optimal placement of biologic therapies on the treatment pathway for psoriasis. Results of the list price analyses determined the optimal first-line treatment in the UK to be adalimumab biosimilar, followed by ustekinumab, secukinumab and then best supportive care. It was noted that this sequence was the most cost-effective and dominant scenario compared with other sequences tested [46].
Together these studies confirm the use of biosimilars as a valuable pharmacoeconomic strategy to lower healthcare cost in patients with psoriasis.
Access to Effective Treatment
Despite the documented benefits of biologic therapy in psoriasis, patients appear to be undertreated. In a non-interventional, multicenter study of 903 newly consulted patients with psoriasis, results showed that a low level of education was associated with greater severity of disease, and of patients with severe psoriasis, those of lower socioeconomic status and lower educational level had seen fewer physicians and had less frequently received a systemic treatment [47]. More recently, studies in Italy and Germany have shown that 50% of patients with psoriasis are still untreated and that, for those patients receiving treatment, biologics make up only a small percentage despite many patients being eligible (<5% received biologics [Italy] and 24% intravenous/subcutaneous administered therapies [Germany].) [48, 49].
Underdiagnosis may also be an issue for patients who experience psoriasis in less common locations such as the scalp, face, intertriginous areas, genitals, hands, feet and nails. Despite the often-small surface area affected, disease management can be challenging. For example, despite facial psoriasis being a marker of more severe disease, its treatment is complicated by an underappreciation of its prevalence. Similarly, a large proportion of patients with severe scalp psoriasis often present with minimal chronic plaque psoriasis on the body and thus may not receive appropriate treatment. Consequently, the QoL of patients with psoriasis affecting fewer common areas may be disproportionately impacted [36].
In addition to underdiagnosis and undertreatment, there is the issue of therapeutic inertia. In a survey study of physicians treating adolescents with moderate-to-severe plaque psoriasis, only 36% felt that they had knowledge about therapeutic optimization, approximately 50% were comfortable starting a new treatment or optimizing therapy when psoriasis was not controlled, and less than half (42%) were comfortable prescribing biologics. Better education around these topics could enable a faster escalation/modification of therapy when needed [50].
Treatment Earlier in the Course of the Disease
IMIDs such as psoriasis are systemic in nature and have the potential to insidiously affect multiple organ systems, leading to complications and comorbidities if not treated effectively early in the disease course [51, 52]. Unfortunately, evidence suggests that the treatment of psoriasis is often approached conservatively, resulting in delayed clearance [53]. In a recent retrospective UK study of over 25,000 patients with psoriasis, conducted to examine the trends in healthcare events before a diagnosis of psoriasis, results showed that patients with psoriasis were up to eight times more likely to be misdiagnosed with pityriasis rosea at 6 months, and the diagnosis of psoriasis may be missed or delayed in a UK primary care setting for up to 5 years for some individuals, leading to a potentially detrimental delay in treatment [26].
The systemic inflammation and chronic immune dysregulation associated with moderate-to-severe psoriasis has been linked with a number of comorbidities including PsA, metabolic syndrome, depression, diabetes mellitus, cardiovascular diseases, myocardial infarction, atherosclerosis, obesity and cancer [54,55,56,57]. A strong association between psoriasis, Crohn’s disease (CD) and ulcerative colitis (UC) has been demonstrated in a number of epidemiologic studies, with an increased risk of CD and UC seen in patients with psoriasis and vice versa [58]. Approximately 30% of patients with psoriasis will have musculoskeletal involvement, which can be heterogeneous in its presentation and severity [59, 60].
It is thought that the use of biologics earlier in the disease course may reverse the inflammatory consequences associated with psoriasis comorbidities, influencing long-term outcomes [52, 61]. Since most patients who are destined to develop PsA will have antecedent skin psoriasis, dermatologists are ideally placed to detect PsA and intervene with immunomodulatory therapy at the earliest opportunity to limit the deterioration of physical function [6], risk of cumulative life-course impairment and psychologic distress [62,63,64]. To halt the progression of the disease and mitigate the risk of physical and psychosocial morbidity, expert opinion generally advises the introduction of biologic therapies earlier in the course of psoriasis [11, 51, 53, 65]. The higher efficacy of biologic over non-biologic therapies may allow more robust and earlier disease control preventing life quality impairment.
Interestingly, three recent retrospective studies investigated the impact of early interventions with biologics compared with TS therapies or phototherapy on the incidence of PsA in patients with psoriasis [66,67,68]. Collectively, results showed that early treatment with biologics may delay or reduce the risk of incident PsA in patients with moderate-to-severe psoriasis with risk factors for PsA [66,67,68] including older age [66], nail psoriasis [67], psoriasis duration > 10 years [66] and a higher body mass index [67]. Notably, anti-TNF agents should be avoided in patients with heart failure or demyelinating disease, and inhibitors of IL 17A, IL-17A/F and anti-IL 17R should be used with caution in patients with CD or UC because of the potential risk of worsening inflammatory bowel disease [69].
Thus, introduction of biosimilars could promote the revision of recommendations reflecting the evolving regulatory and clinical experience with biosimilars and allowing the use of biologics earlier in the disease course. This was the case in the UK when the availability of cost-effective anti-TNF biosimilars promoted a reconsideration by NICE of the criteria regarding when biologic therapies could be given in patients with rheumatoid arthritis so that patients with moderate disease are now eligible [70, 71].
Maintenance of Response
While current biologic therapies for psoriasis are highly effective, real-world registries demonstrate that a proportion of patients (up 30–60% at 5 years) will discontinue treatment for a variety of reasons including diminished efficacy, adverse events, the patients’ desire to reduce treatment burden, specific circumstances such as pregnancy and inability to cover treatment costs [72,73,74,75,76].
Dose escalation or interval reduction can be undertaken when there is a primary non-response or a secondary loss of response where prescribing regulations allow. Failure or loss of response can be identified through assessment of cutaneous manifestations or monitoring of drug levels [77], the latter being an adjunct to therapeutic decision making if anti-drug antibodies are considered a possibility. Dose escalation may improve efficacy but can also be associated with an increased risk of adverse events and may also represent a significant economic burden [78]. This increase in burden can be mitigated if a biosimilar is used.
Doses of biologics can also be tapered or discontinued when patients achieve clear skin or low disease activity to reduce adverse effects and financial burden. However, this approach carries a risk of relapse for a significant proportion of patients with treatment needing to be reinstated at their standard doses [79]. Recently, a retrospective study by Armstrong et al. evaluated switch patterns among 11,526 patients with psoriasis who initiated treatment with targeted (biologic or Apremilast) therapy and subsequently switched to another non-targeted therapy. They found that among patients who switched, 52.6% reinitiated treatment with targeted therapy. Additionally, for all patients on non-targeted therapies, the probability of reinitiating any targeted therapy was 60.7% at 24 months [80].
Conclusions
Biologic therapies are highly effective for the treatment of moderate-to-severe psoriasis, but access limitations mean that unmet clinical needs remain. A large proportion of patients who would benefit do not have access to biologic therapy, are not able to access biologic therapies early enough in the disease course to impact outcomes or are unable to stay on therapy once a stable response is achieved. Although biosimilars may have limitations in efficacy and drug survival compared with more recent biologic options within psoriasis [72, 81], they are increasing the opportunity of access to biologic treatment for patients with psoriasis who may historically have been undertreated. Moreover, the earlier use of biosimilars could help to optimize disease and comorbidity management. The approval and adoption of cost-effective biosimilars more widely and earlier in the treatment armamentarium for psoriasis has the potential to significantly improve patients’ outcomes while controlling increasing healthcare costs and providing more affordable therapeutic options for patients.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Pharmacy Times. New Treatment for Plaque Psoriasis Approved in Europe, J. Barrett, Editor. 2018. p. https://www.pharmacytimes.com/view/new-treatment-for-plaque-psoriasis-approved-in-europe.
Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31(2):205–12.
Griffiths CEM, et al. Psoriasis. Lancet. 2021;397(10281):1301–15.
Parisi R, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369: m1590.
van de Kerkhof PC, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29(10):2002–10.
Gisondi P, et al. Cost per responder of Adalimumab biosimilars MSB11022 and ABP 501 versus the originator and methotrexate in chronic plaque psoriasis. Expert Opin Biol Ther. 2022;22(12):1579–84.
Armstrong AW, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5.
Strober B, et al. Recategorization of psoriasis severity: Delphi consensus from the International Psoriasis Council. J Am Acad Dermatol. 2020;82(1):117–22.
Strober B, et al. Characterization of disease burden, comorbidities, and treatment use in a large, US-based cohort: results from the Corrona Psoriasis Registry. J Am Acad Dermatol. 2018;78(2):323–32.
Ruda RC, Kelly KA, Feldman SR. Real-world outcomes following switching from anti-TNF reference products to biosimilars for the treatment of psoriasis. J Dermatol Treat. 2023;34(1):2140569.
Rezk MF, Pieper B. Unlocking the value of anti-TNF biosimilars: reducing disease burden and improving outcomes in chronic immune-mediated inflammatory diseases: a narrative review. Adv Ther. 2020;37(9):3732–45.
Gisondi P, et al. Cost per responder analysis of Secukinumab versus adalimumab in the treatment of psoriatic disease. Vaccines (Basel). 2022;10(5):646.
Maurelli M, Girolomoni G, Gisondi P. Cost per responder of adalimumab biosimilars versus methotrexate in patients with psoriasis: a real-life experience. J Dermatol Treat. 2023;34(1):2218504.
Nast A, et al. German S3-Guideline on the treatment of Psoriasis vulgaris, adapted from EuroGuiDerm—Part 1: treatment goals and treatment recommendations. J Dtsch Dermatol Ges. 2021;19(6):934–150.
Fortina AB, et al. Treatment of severe psoriasis in children: recommendations of an Italian expert group. Eur J Pediatr. 2017;176(10):1339–54.
Ruiz-Villaverde R, et al. Updated position of the Spanish Psoriasis Group (GPs) on the use of biosimilar drugs in moderate to severe psoriasis. Actas Dermosifiliogr. 2023;114(6):T494–501.
Rønholt K, Iversen L. Old and new biological therapies for psoriasis. Int J Mol Sci. 2017;18(11):2297.
Carrascosa JM, et al. Biosimilar drugs for psoriasis: principles, present, and near future. Dermatol Ther (Heidelb). 2018;8(2):173–94.
Menter A, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Nast A, et al. EuroGuiDerm guideline on the systemic treatment of Psoriasis vulgaris—Part 2: specific clinical and comorbid situations. J Eur Acad Dermatol Venereol. 2021;35(2):281–317.
Baumgart DC, et al. Biological therapies in immune-mediated inflammatory diseases: Can biosimilars reduce access inequities? Front Pharmacol. 2019;10:279.
Ebbers HC. Biosimilarity and interchangeability of biologic drugs-general principles, biophysical tests, and clinical requirements to demonstrate biosimilarity. In: Biologics, Biosimilars, and Biobetters. 2020. p. 109–24.
Ruiz-Villaverde R, Galán-Gutierrez M. Biosimilars in psoriasis: what should your positioning be? Expert Opin Biol Ther. 2021;21(1):81–6.
Puig L. Biosimilars in the treatment of psoriasis: an update. Actas Dermosifiliogr (Engl Ed). 2020;111(10):809–14.
Griffiths CEM, et al. The EGALITY study: a confirmatory, randomized, double-blind study comparing the efficacy, safety and immunogenicity of GP2015, a proposed etanercept biosimilar, vs. the originator product in patients with moderate-to-severe chronic plaque-type psoriasis. Br J Dermatol. 2017;176(4):928–38.
Abo-Tabik M, et al. Mapping opportunities for the earlier diagnosis of psoriasis in primary care settings in the UK: results from two matched case-control studies. Br J Gen Pract. 2022;72(724):e834–41.
Hercogová J, et al. AURIEL-PsO: a randomized, double-blind phase III equivalence trial to demonstrate the clinical similarity of the proposed biosimilar MSB11022 to reference adalimumab in patients with moderate-to-severe chronic plaque-type psoriasis. Br J Dermatol. 2020;182(2):316–26.
Papp K, et al. Clinical similarity of the biosimilar ABP 501 compared with adalimumab after single transition: long-term results from a randomized controlled, double-blind, 52-week, phase III trial in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2017;177(6):1562–74.
Dapavo P, et al. The infliximab biosimilar in the treatment of moderate to severe plaque psoriasis. J Am Acad Dermatol. 2016;75(4):736–9.
Gisondi P, et al. Infliximab biosimilar CT-P13 in the treatment of chronic plaque psoriasis: data from the Psobiosimilars registry. Br J Dermatol. 2017;177(6):e325–6.
Phan DB et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159(7):763–71.
Warren RB, et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Invest Dermatol. 2015;135(11):2632–40.
Gisondi P, et al. TNF-α inhibitors biosimilars as first line systemic treatment for moderate-to-severe chronic plaque psoriasis. Expert Rev Clin Immunol. 2020;16(6):591–8.
Egeberg A, et al. Real world SB4 (Etanercept Biosimilar) use in patients with psoriasis: data from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Drugs Dermatol. 2020;19(3):316–8.
López-Ferrer A, et al. Drug survival of adalimumab biosimilars in real-world treatment of psoriasis: a Spanish multicenter study. Dermatol Ther. 2022;35(11): e15831.
Giunta A, et al. A single-centre, observational, retrospective, real-life study evaluating adalimumab biosimilar ABP 501 in the treatment of plaque-type psoriasis and psoriatic arthritis in originator-naïve patients and in patients undergoing non-medical switch from originator. Curr Med Res Opin. 2021;37(7):1099–102.
Loft N, et al. Outcomes following a mandatory nonmedical switch from adalimumab originator to adalimumab biosimilars in patients with psoriasis. JAMA Dermatol. 2021;157(6):676–83.
Killion L, Alsharqi A, Kirby B. Switching from adalimumab originator to biosimilar: a 3-year retrospective cohort analysis. Clin Exp Dermatol. 2023;48(4):397–8.
Girolomoni G. Long-term real-world data of SB5 (Adalimumab Biosimilar) treatment in patients with moderate-to-severe psoriasis from the British Association of Dermatologists Biologic and Immunomodulators Register (BADBIR). In: Abstract No: 539 EADV Congress. 2022: Milan.
Bellinato F, et al. Real-life effectiveness of adalimumab biosimilars in patients with chronic plaque psoriasis. Dermatol Ther (Heidelb). 2022;12(6):1303–11.
Megna M, et al. Efficacy and safety of anti-TNF biosimilars for psoriasis in pediatric and geriatric populations: a 72-week real-life study. Psoriasis (Auckl). 2022;12:199–204.
Phan DB, et al. Uptake of tumour necrosis factor-alpha inhibitor biosimilars for psoriasis: a drug utilization study from the British Association of Dermatologists Biologic and Immunomodulators Register (BADBIR). Br J Dermatol. 2023;189(1):62–70.
Edgar BS, et al. Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative. J Manag Care Spec Pharm. 2021;27(8):1129–35.
Esposti LD, et al. Analysis of drug utilization and health care resource consumption in patients with psoriasis and psoriatic arthritis before and after treatment with biological therapies. Biologics. 2018;12:151–8.
Gisondi P, et al. Treat-to-target approach for the management of patients with moderate-to-severe plaque psoriasis: consensus recommendations. Dermatol Ther (Heidelb). 2021;11(1):235–52.
Barker J, et al. health economic assessment of optimal biological treatment for moderate-to-severe psoriasis. Clin Drug Investig. 2021;41(11):1011–20.
Mahé E, et al. Socioeconomic inequalities and severity of plaque psoriasis at a first consultation in dermatology centers. Acta Derm Venereol. 2017;97(5):632–8.
Ingrasciotta Y, et al. Are patients with psoriasis and psoriatic arthritis undertreated? A population-based study from southern Italy. J Clin Med. 2021;10(15):3431.
Pilz AC, et al. Despite large choice of effective therapies: Individuals with psoriasis still seem undertreated. J Dtsch Dermatol Ges. 2021;19(7):1003–11.
Melin A, et al. Therapeutic inertia in the management of moderate-to-severe plaque psoriasis in adolescents. Acta Derm Venereol. 2021;101(6): adv00475.
Reich K. The concept of psoriasis as a systemic inflammation: implications for disease management. J Eur Acad Dermatol Venereol. 2012;26(Suppl 2):3–11.
Korman NJ. Management of psoriasis as a systemic disease: what is the evidence? Br J Dermatol. 2020;182(4):840–8.
Girolomoni G, et al. Early intervention in psoriasis and immune-mediated inflammatory diseases: a hypothesis paper. J Dermatolog Treat. 2015;26(2):103–12.
Mansouri B, et al. Comparison of coronary artery calcium scores between patients with psoriasis and type 2 diabetes. JAMA Dermatol. 2016;152(11):1244–53.
Gelfand JM, et al. Risk of myocardial infarction in patients with psoriasis. JAMA. 2006;296(14):1735–41.
Aurangabadkar SJ. Comorbidities in psoriasis. Indian J Dermatol Venereol Leprol. 2013;79(Suppl 7):S10–7.
Augustin M, et al. Co-morbidity and age-related prevalence of psoriasis: analysis of health insurance data in Germany. Acta Derm Venereol. 2010;90(2):147–51.
Egeberg A, et al. Incidence and risk of inflammatory bowel disease in patients with psoriasis—a nationwide 20-year cohort study. J Investig Dermatol. 2019;139(2):316–23.
Menter MA, et al. Common and not-so-common comorbidities of psoriasis. Semin Cutan Med Surg. 2018;37(2s):S48-s51.
FitzGerald O, et al. Psoriatic arthritis. Nat Rev Dis Primers. 2021;7(1):59.
Jiang Y, et al. Biologic and small-molecule therapies for moderate-to-severe psoriasis: focus on psoriasis comorbidities. BioDrugs. 2023;37(1):35–55.
Kimball AB, et al. Psoriasis: is the impairment to a patient’s life cumulative? J Eur Acad Dermatol Venereol. 2010;24(9):989–1004.
Augustin M. Cumulative life course impairment: identifying patients at risk. Curr Probl Dermatol. 2013;44:74–81.
Nielsen ML, et al. Delay in diagnosis and treatment of patients with psoriasis: a population-based cross-sectional study. Br J Dermatol. 2022;187(4):590–1.
Kerdel F, Don F. The importance of early treatment in psoriasis and management of disease progression. J Drugs Dermatol. 2018;17(7):737–42.
Gisondi P, et al. Biological disease-modifying antirheumatic drugs may mitigate the risk of psoriatic arthritis in patients with chronic plaque psoriasis. Ann Rheum Dis. 2022;81(1):68–73.
Acosta Felquer ML, et al. Treating the skin with biologics in patients with psoriasis decreases the incidence of psoriatic arthritis. Ann Rheum Dis. 2022;81(1):74–9.
Rosenthal YS, et al. Incidence of psoriatic arthritis among patients receiving biologic treatments for psoriasis: a nested case-control study. Arthritis Rheumatol. 2022;74(2):237–43.
Conforti C, et al. Spotlight on the treatment armamentarium of concomitant psoriasis and inflammatory bowel disease: a systematic review. J Dermatolog Treat. 2022;33(3):1279–86.
NICE. Adalimumab, etanercept, infliximab, certolizumab pegol, golimumab, tocilizumab and abatacept for rheumatoid arthritis not previously treated with DMARDs or after conventional DMARDs only have failed. 2016. [January 2023]; Available from: https://www.nice.org.uk/guidance/ta375.
NICE. Adalimumab, etanercept, infliximab and abatacept for treating moderate rheumatoid arthritis after conventional DMARDs have failed. 2021. [January 2023]; Available from: https://www.nice.org.uk/guidance/ta715.
Doshi JA, et al. Biologic therapy adherence, discontinuation, switching, and restarting among patients with psoriasis in the US Medicare population. J Am Acad Dermatol. 2016;74(6):1057-1065.e4.
Egeberg A, et al. Safety, efficacy and drug survival of biologics and biosimilars for moderate-to-severe plaque psoriasis. Br J Dermatol. 2018;178(2):509–19.
Masson Regnault M, et al. Time to relapse after discontinuing systemic treatment for psoriasis: a systematic review. Am J Clin Dermatol. 2022;23(4):433–47.
Michielsens CAJ, et al. Dose tapering of biologics in patients with psoriasis: a scoping review. Drugs. 2021;81(3):349–66.
Gulliver SR, Gulliver W. Investigation of prevalence of biologic use and discontinuation rates in moderate-to-severe psoriasis patients in Newfoundland and Labrador using real-world data. Dermatol Ther. 2021;34(3): e14944.
Liau MM, Oon HH. Therapeutic drug monitoring of biologics in psoriasis. Biologics. 2019;13:127–32.
Gambardella A, Licata G, Sohrt A. Dose adjustment of biologic treatments for moderate-to-severe plaque psoriasis in the real world: a systematic review. Dermatol Ther (Heidelb). 2021;11(4):1141–56.
Shi L, et al. Tapering and discontinuation of systemic medications in psoriasis patients with low disease activity. Dermatol Ther. 2020;33(4): e13599.
Armstrong A, et al. Treatment patterns for targeted therapies, non-targeted therapies, and drug holidays in patients with psoriasis. Dermatol Ther (Heidelb). 2022;12(9):2087–103.
Yiu ZZN, et al. Drug Survival Associated with effectiveness and safety of treatment with Guselkumab, Ixekizumab, Secukinumab, Ustekinumab, and Adalimumab in Patients With Psoriasis. JAMA Dermatol. 2022;158(10):1131–41.
EMA, Bimzelx® summary of product characteristics (SPC). 2021.
EMA. SmPC SOTYKTU 6 mg film coated tablets. 2023; Available from: https://www.ema.europa.eu/en/documents/product-information/sotyktu-epar-product-information_en.pdf.
Amatore F, et al. French guidelines on the use of systemic treatments for moderate-to-severe psoriasis in adults. J Eur Acad Dermatol Venereol. 2019;33(3):464–83.
Nast A, et al. German S3-Guideline on the treatment of Psoriasis vulgaris, adapted from EuroGuiDerm—Part 2: treatment monitoring and specific clinical or comorbid situations. J Dtsch Dermatol Ges. 2021;19(7):1092–115.
Puig L, et al. Spanish evidence-based guidelines on the treatment of psoriasis with biologic agents, 2013. Part 1: on efficacy and choice of treatment. Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Actas Dermosifiliogr. 2013;104(8):694–709.
Carrascosa JM, et al. Practical update of the Recommendations Published by the Psoriasis Group of the Spanish Academy of Dermatology and Venereology (GPS) on the Treatment of Psoriasis with Biologic Therapy. Part 1. Concepts and General Management of Psoriasis with Biologic Therapy. Actas Dermosifiliogr. 2022;113(3):261–77.
SSDV. SSDV:s behandlingsrekommendationer för systemisk behandling av psoriasis. 2022.
Smith CH, et al. British Association of Dermatologists guidelines for biologic therapy for psoriasis 2020: a rapid update. Br J Dermatol. 2020;183(4):628–37.
Gisondi P, et al. State of the art and pharmacological pipeline of biologics for chronic plaque psoriasis. Curr Opin Pharmacol. 2019;46:90–9.
EMA. Medicines. Search results for medicine type = 'biosimilar'. 2023. Available from: https://www.ema.europa.eu/en/medicines/field_ema_web_categories%253Aname_field/Human/ema_group_types/ema_medicine/field_ema_med_status/authorised-36/ema_medicine_types/field_ema_med_biosimilar/search_api_aggregation_ema_medicine_types/field_ema_med_biosimilar.
EMA. Amsparity product information. 2020 January 2023]. Available from: https://www.ema.europa.eu/en/documents/product-information/amsparity-epar-product-information_en.pdf.
Acknowledgements
Medical Writing and/or Editorial Assistance
Medical writing support was provided by Olive Denneny, MSc, and Iain Bartlett, PhD, of Springer Healthcare Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Funding
Medical writing support and the Rapid Service Fee was funded by Biogen International GmbH, Baar, Switzerland.
Author information
Authors and Affiliations
Contributions
Giampiero Girolomoni, Laura Savage, Paolo Gisondi, Åke Svensson, Emmanuel Mahé, Matthias Augustin, and Luis Puig contributed to conception, planning, drafting, critical revision, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
GG has received personal fees from AbbVie, Abiogen, Almirall, Amgen, Biogen, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli-Lilly, Leo Pharma, Merck Serono, Novartis, Pfizer, Samsung and Sanofi. LS has received honoraria and/or received research funding from the following pharmaceutical companies: AbbVie, Almirall, Amgen, Aspire Pharma, Biogen, Boehringer-Ingelheim, Bristol-Myers-Squibb, Celgene, Celltrion, Fresensius Kabi, Galderma, Janssen, Leo, Lilly, Novartis, Pfizer, MSD, Sanofi, Takeda, UCB. PG has been a consultant and/or speaker for Abbvie, Almirall, Celgene, Ducray, Janssen, LEO Pharma, Eli Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Pierre Fabre, Sandoz, UCB. ÅS has no disclosures to declare. EM has received grants or contracts from Sanofi and Abbvie; Consulting fees from Sanofi and Abbvie. MA has received research grants from AbbVie, Almirall, Beiersdorf, Eli Lilly, Galderma, Incyte, LEO, Menlo, MSD, Novartis, Pfizer, Regeneron, Sanofi‐Genzyme and Trevi; served as a consultant for AbbVie, Almirall, Beiersdorf, Eli Lilly, Galderma, Incyte, LEO, Menlo, MSD, Novartis, Pfizer, Regeneron, Sanofi‐Genzyme and Trevi; and as a lecturer for AbbVie, Almirall, Beiersdorf, Eli Lilly, Galderma, Incyte, LEO, Menlo, MSD, Novartis, Pfizer, Regeneron, Sanofi‐Genzyme and Trevi. LP has received consultancy/speaker’s honoraria from and/or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, Baxalta, Biogen, Boehringer- Ingelheim, Celgene, Gebro, Janssen, JSC BIOCAD, Leo-Pharma, Lilly, Merck-Serono, MSD, Mylan, Novartis, Pfizer, Regeneron, Roche, Sandoz, Samsung-Bioepis, Sanofi and UCB.
Ethical Approval
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Girolomoni, G., Savage, L., Gisondi, P. et al. Increasing Access to Effective Systemic Treatments in Patients with Moderate-to-Severe Psoriasis: Narrative Review. Dermatol Ther (Heidelb) 13, 2171–2185 (2023). https://doi.org/10.1007/s13555-023-01014-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01014-x