Abstract
Introduction
Port-wine stains (PWS) are congenital capillary abnormalities caused by immature, venule-like vasculature that progressively dilates due to poor endothelial cell differentiation. PWS affects between 0.3% and 0.9% of newborns, with 90% of cases occurring on the face. Individuals with facial PWS and their parents had a significant negative impairment on their quality of life (QoL) and also suffered from psychological disabilities.
Methods
This was a cross-sectional questionnaire-based survey study in Thailand from July 2021 to April 2022. The questionnaires included demographic data, subjective evaluation (SE), and the Dermatology Life Quality Index (DLQI). The questionnaire was performed with a full scale and adjusted scale of validity and reliability test of DLQI using factor analysis and Cronbach’s alpha. The study outcome was a subjective evaluation and DLQI in patients who received pulsed dye laser (PDL) treatment.
Results
Of the 54 patients, 35.2% (19) are male, and 64.8% (35) are female. Regarding age groups, 64.8% (35) are below 5 years old, and 35.2% (19) are older than 5 years. SE results showed that males evaluated an improvement of the facial PWS lesion significantly better than females (P < 0.05). The older age group graded the percentage of improvement better than the younger age group (P < 0.01). The result of the DLQI showed no difference in DLQI between gender. Older age result resulted in a significantly different DLQI compared with younger age (P < 0.01). Parent-reported DLQI improvement was less than self-reported DLQI improvement in patients with PWS treated with PDL (P < 0.05). Concerning the instrument of the study, the validity and reliability analysis of the DLQI questionnaire using factor analysis and Cronbach’s alpha have been performed. The adjusted scale with the 5-item DLQI questionnaire is more appropriate in terms validity and reliability.
Conclusion
This study demonstrates that facial PWS reduces the QoL as measured by DLQI. We discovered that the QoL of patients and parents with PWS was significantly impaired. The main influencing factors were older age, the improved perception between gender, and PDL treatments. In addition, we found only five questions that are reliable for PWS. The adjusted five-item DLQI questionnaires are more appropriate regarding validity and reliability.
Trial Registration Number
TCTR20230210001, COA no. si 1059/2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Individuals with facial port-wine stains (PWS) had a significant negative impairment on their quality of life (QoL). |
To date, there is no standardized evaluation method for the QoL of PWS. |
What was learned from the study? |
The adjusted 5-item Dermatology Life Quality Index (DLQI) questionnaires are more appropriate regarding validity and reliability. |
This study supported that facial PWS reduces the QoL as assessed by DLQI. |
The QoL of the parents of children with PWS was impaired significantly. |
Introduction
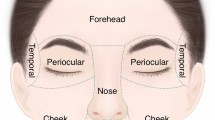
Port-wine stains (PWS) or port-wine birthmarks are congenital capillary abnormalities caused by immature, venule-like vasculature that dilate progressively [1, 2]. PWS affects between 0.3% and 0.9% of neonates [3], with 90% of cases occurring on the face [4]. At first, the lesions begin as pink or red macules, which do not resolve spontaneously and may darken and grow proportionally to age, leading to the formation of papules and nodules or hypertrophic PWS [5]. In addition to cosmetic deformity, PWS hypertrophy can affect vision, speaking, nasal breathing, and hearing [6].
Port-wine stains have been treated with lasers for almost 30 years [7]. The introduction of the pulsed dye laser (PDL) has transformed the treatment of PWS within the past 3 decades. According to the selective photothermolysis concept, the PDL targets oxyhemoglobin as its primary chromophore with minimum nonspecific thermal damage to the surrounding structures [8]. Following PDL therapy, PWS lightens due to a decrease in the quantity and size of blood vessels [9]. Multiple treatments are necessary for the greatest recovery, but no set number of treatment sessions has been defined [10]. Based on the estimated fixed effects model, we predicted the clinical improvement from the laser therapy sessions in our prior study. The first five treatments should result in a 40% improvement, and treatments 6–10 should yield an additional 20% improvement. The third five treatments (visits 11–15) will only result in an additional 10% improvement, and the fourth five treatments (visits 16–20) will result in less than 5% improvement due to the rapid decline in the clinical efficacy of the treatment [11].
We reviewed 17 relevant articles with 2135 patients with PWS, and the results demonstrated that individuals with facial PWS had a substantial negative impact on their quality of life (QoL) and psychological impairments. The PWS lesion tends to deteriorate with age and may create further social adaptation issues, particularly in children [12]. Many outcome measurement instruments are utilized in PWS studies. However, the quality of evidence for content validity of these instruments was low [13]. Currently, 36 measuring tools have been used to assess the QoL and psychological impacts among patients with PWS [11]. The Dermatology Life Quality Index (DLQI) was the first health-related quality of life questionnaire tailored to dermatology [14]. The DLQI’s overall grades for content validity (and its three subcomponents, relevance, comprehensiveness, and understandability) were adequate. Further measurement evaluation for PWS is needed due to insufficient data to guide outcome selection [13].
Early laser therapy, psychological aid, and patient support are the most effective treatments for enhancing the quality of life of patients with PWS. Continual evaluation of the improvement in QoL following laser therapy is essential [12]. It would be more useful to develop a standardized evaluation method for the QoL of PWS. This study aims to assess the DLQI in patients with facial PWS treated with PDL. To the best of our knowledge, this is the first study to validate the DLQI for patients with facial PWS.
Methods
In this cross-sectional study, using a questionnaire we gathered the information of patients with PWS at Siriraj Hospital, Mahidol University, Bangkok, Thailand, from July 2021 to April 2022. The questionnaire had three components: demographic data, subjective evaluation (SE), and the DLQI. The participants were asked to rate their SE using a photograph and DLQI at the 6th treatment, 11th treatment, and 16th treatment, or at least at two time points. The inclusion criteria were patients of all ages with a clinical diagnosis of facial PWS. The exclusion criteria were patients or parents who were unwilling or unable to answer the questionnaire.
From the population (total number of patients, N = 118) [11], by setting the proportion p = 0.5, the margin of error d = 0.1, and confidence level α = 0.05, the number of samples of the study is equal to 54 patients.
The study’s primary outcome was a subjective evaluation and DLQI in PDL treatment patients. DLQI is evaluated by patients using a questionnaire and measures the impact of PWS on their health-related quality of life (HRQoL). The DQLI scores were adjusted from 0 to 100 with higher scores meaning higher impairment. Descriptive analysis was used for the demographic data, including gender and age. The subsample analysis was categorized by age (≤ 5 years or > 5 years), gender (male or female), and those who reported the questionnaire (self or parent).
We performed a full scale and adjusted scale of validity and reliability test of DLQI using factor analysis and Cronbach’s alpha. A Cronbach’s alpha of 0.70 or above indicates acceptable internal consistency.
Descriptive statistics were performed to describe the demographic data. An independent sample t-test and chi-square square were performed to find the difference between samples categorized by age groups and gender. The primary outcome was analysis using linear fixed effects panel data models for subjective evaluation perception. The statistical analysis was performed using Stata (Stata-Corp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP,) and a P-value < 0.05 was considered statistically significant.
The study was approved by the ethics committee of the Siriraj Institutional Review Board (SIRB protocol no. 941/2563/COA no. si 1059/2020). Written informed consent was obtained for the publication and use of all patients’ data prior to their enrollment in the study. This study was performed in accordance with the Helsinki Declaration of 1964 and its subsequent amendments.
Results
Demographic characteristics (Table 1) showed samples categorized by age groups and gender. Of the 54 patients, 35.2% (19) are male, and 64.8% (35) are female. Regarding age groups, 64.8% (35) are below 5 years old, and 35.2% (19) are older than 5 years.
Concerning the instrument of the study, the validity and reliability analysis of the DLQI questionnaire using factor analysis and Cronbac’s alpha have been performed. Table 2 indicates that 10 items of the DLQI questionnaire needed to be more valid in determining the QoL of facial dermatology patients due to the low value of percentage of total variance (0.4264, which is much lower than the acceptable threshold of 0.7). Table 3 shows that the adjusted scale with the 5-item DLQI questionnaire is more appropriate regarding validity and reliability (high value of percentage of total variance, factor loadings, Cronbach’s alpha, and composite reliability, which are all greater than the threshold of 0.7). Therefore, quality of life in this study is determined by the adjusted 5-item DLQI scale.
Table 4 shows the results of subjective evaluation (SE) and DLQI Score (0–100) categorized by age and gender. The mean age of the self-report group was 30 ± 12.6 years, and the parent-report group was 5 ± 3.3 years. DQLI scores were adjusted to a maximum of 100 to estimate the percentage of improvement. Subjective evaluation results showed that males evaluated an improvement of the facial PWS lesion significantly better than females, with a mean difference of 3.78 (P < 0.05). The older age group (age > 5 years) graded the percentage of improvement better than the younger age group, with a mean difference of −6.26 (P < 0.01). Patients’ reported improvement of subjective evaluation in those with PWS who had received PDL treatment was better than the parent-report DLQI (mean difference −3.78, P < 0.05). The result of DLQI showed no difference in DLQI between gender (mean difference 0.68). Still, the older age result had a significantly different DLQI compared with younger age result (mean difference −18.89, P < 0.01), aligning with the result of the SE. The DQLI was significantly different from baseline, with a mean difference of −14.82 (P < 0.01) compared with after PDL treatment at approximately 8.4 visits from gathering data of overall respondents. Meanwhile, parent-report improvement of DLQI in patients with PWS who had received PDL treatment was lower than the self-report DLQI (mean difference 18.28, P < 0.01).
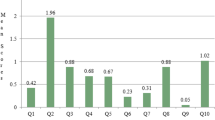
The trend of SE and DQLI are shown in Fig. 1. At visits 6, 8, and 10, the subjective evaluation improvement was 40%, 50%, and 60%, respectively, and DLQI showed 25%, 30%, and 35% improvement at visits 4, 6, and 8, respectively.
Linear fixed effects panel data models for patients’ subjective evaluations are shown in Table 5. The percentage of subjective evaluation in age > 5 years was better than in age ≤ 5 years, with a percentage of subjective improvement of 25.56% and 21.07%, respectively, in each visit to PDL laser treatment. Subjective improvement in females (27.59%) was better than in males (19.65%) in each PDL laser treatment visit.
Linear fixed effects panel data models for the patient percentage of DLQI improvement (0–100) are shown in Table 6. The percentage of DLQI improvement in age > 5 years was better than in age ≤ 5 years, with the percentage of DLQI improvement of 15.04% and 13.80%, respectively, in each PDL laser treatment visit. DLQI improvement was 16.51% in males and 11.29% in females in each PDL laser treatment visit.
Discussion
The face is intimately associated with social interactions and personal identity [15]. Several studies have demonstrated a deleterious impact on QoL and psychological adjustment in individuals with facial PWS [16, 17]. Patients with facial PWS experience a significant psychological burden that does not diminish with advancing age. Thus, PWS generates long-term self-stigma, low self-esteem, and emotional stress [18]. We discovered that facial PWS had statistically significant unfavorable consequences for patients. Specifically, these negative impacts result from the patients’ self-stigma and experiences with discriminating behaviors due to their skin condition. This implies that facial PWS restricts the patients’ integration into society, reducing their overall QoL [19]. This study provides evidence that facial PWS reduces the QoL. We utilized the DLQI to evaluate QoL. The DQLI was substantially different from the baseline compared with after treatment with PDL at approximately 8.4 visits. The trend of subject evaluation and DQLI are shown in Fig. 1. Subjective evaluation improvement was 40%, 50%, and 60% at visits 6, 8, and 10, respectively, while the DLQI improved by 25%, 30%, and 35% at visits 4, 6, and 8, respectively. Interestingly, the subjective evaluation pattern is the same as the physician rating in our prior study. In our previous study, we calculated the prediction of the improvement from the laser treatment sessions based on the estimated fixed effects model. It is anticipated that the first five treatments will result in a 40% improvement, while the subsequent five treatments (treatments 6–10) will result in an additional 20% improvement. Due to its rapid decline in clinical effectiveness, the third five treatments (visits 11–15) will only add 10% more improvement, and the fourth five treatments (treatments 16–20) will add less than 5% improvement [11]. Initiating laser treatment before 5 years could be an excellent strategy to improve the QoL and prevent future stigma.
The Dermatology Life Quality Index is the most widely used QoL questionnaire in dermatology. In the 25 years after its publication, it has become the most used instrument for measuring QoL in dermatology and is currently used in over 40 skin disorders worldwide [20]. The DLQI consists of 10 items (symptoms and feelings, activities, daily activities, leisure, school, work, personal relationships, and treatment) [14]. The prevalence of patient-reported symptoms in several skin disorders justifies the presence of these instruments. However, others have contended that the DLQI cannot measure the complete spectrum of QoL in some circumstances [20]. No content validity studies performed in patients with PWS were found [13]. To the best of our knowledge, this is the first study validating the DLQI for facial PWS. We found only five questions were reliable for facial PWS. Some questions need to be more reliable for facial PWS. Concerning the study’s instrument, a validity and reliability analysis of the DLQI questionnaire was conducted using factor analysis and Cronbach’s alpha. Table 2 indicated that the 10 items of the DLQI questionnaire are not valid and reliable in determining the QoL of patients with facial PWS. The adjusted 5-item DLQI questionnaire is more appropriate regarding validity and reliability (Table 3). Therefore, the QoL in this study is determined by the adjusted 5-item DLQI questionnaires. Surprisingly, all patients answered “Not at all” to the question “How much has your sleep been affected by your skin problem?”. We concluded that sleep does not impact QoL for facial PWS. The DLQI is not a disease-specific questionnaire. This discovery might be used in future DLQI questionnaires for nevus of Ota, congenital melanocytic nevus, and other visible facial conditions.
Port-wine stains do not improve with time and may pose further adaptation concerns to their social environment [18]. Generally, children with PWS experience peer discrimination [21]. Children with noticeable facial disorders such as PWS, infantile hemangioma, burn scars, and congenital melanocytic are most likely to have diminished QoL and psychological well-being relative to the norm. Still, these findings were not seen in preschool children [16]. This asymptomatic disorder has no negative consequences when the patient is young and socially isolated. However, as the patient develops and matures, the distinctive look of the lesion influences the child’s sense of self and emotional and psychological growth, which impacts day-to-day activities [15], leading to a future stigma. Our earlier study demonstrated that younger children were less concerned about PWS than adolescents and young adults [19]. We discovered a comparable outcome in the current study. Patients with an age over 5 years had a superior subjective assessment and DLQI improvement than those ≤ 5 years in each PDL laser session. The result was consistent with our prior study. We discovered that young children were either unconcerned or less concerned about PWS than adolescents and adults. Patients older than 5 years were more likely to pay attention and spend more time than patients ≤ 5 years [22]. QoL is multidimensional and subjective, comprising physical, mental, and social elements of well-being [23]. The QoL might be anticipated to differ at different ages [24].
Port-wine stains afflict males and females equally [3]. According to Wang et al.[25], skin hypertrophy, female sex, and lesion size greater than 30 cm2 were the key influencing variables that affected patients with PWS’ QoL. For particular patients with PWS, females have considerably greater median stress levels than patients than males [3]. Subjective improvement in females (27.59%) was better than in males (19.65%) in each PDL laser treatment visit. The DLQI improvement was 16.51% in males and 11.29% in females in each PDL laser treatment visit. Patients with facial PWS were considerably less satisfied with treatment improvements than those with non-facial PWS [3]. Our study found that the DLQI improvement in females was lower than in males in each PDL treatment, even though the subjective improvement was higher in females. The patient’s level of treatment satisfaction is anticipated to be more deeply influenced by their impression of the degree of improvement rather than the actual improvement [3]. We found the degree of DLQI improvement might differ between males and females, which may be related to female patients experiencing more PWS-related stress [3].
Recent studies reported that their children’s chronic skin problems significantly impact parents’ mental health and QoL [26,27,28,29]. PWS deleteriously affects the QoL of the affected child and their family members [30]. Similar to recent studies mentioned above, we found the QoL of the parents of children with PWS was significantly impaired. Parent-reported subjective evaluation improvement was better than parent-reported DLQI in PWS treated with PDL. Parent-reported DLQI improvement was less than self-reported DLQI improvement in PWS treated with PDL. In the present investigation, we observed that the parents were substantially more affected than the patients. Appropriate support and treatment should help parents adjust their expectations and manage the condition [30].
There are some important limitations of this study. The sample size was limited, and it was conducted in a single-center study, which considerably limits the generalizability of the results. Therefore, it is recommended that future studies with large sample sizes and multicenter studies be conducted. We found that the proposed 5-items adjusted scale of DLQI is more reliable for patients with PWS. Verifying the proposed 5-item adjusted scale of DLQI on a broader study population and in multicenter studies is still necessary since the 10-item questionnaire of DLQI is widely used in other dermatological conditions and allows an adequate assessment of QoL.
Conclusions
In conclusion, this study proves that facial PWS reduces the QoL assessed by DLQI. We found the QoL of the parents of children with PWS was impaired significantly. The analysis of the DLQI questionnaire using factor analysis and Cronbach’s alpha showed that the main influencing factors were older age, the improvement perception between gender, and PDL treatments. Initiating laser treatment before 5 years of age could be an excellent strategy to improve the QoL and prevent future stigma. In addition, we found only five questions that are reliable for PWS. The adjusted 5-item DLQI questionnaires are more appropriate regarding validity and reliability. The DLQI is not a disease-specific questionnaire. Therefore, this finding could be incorporated into future DLQI questionnaires for visible facial conditions.
References
Tan W, Wang J, Zhou F, Gao L, Yin R, Liu H, et al. Coexistence of Eph receptor B1 and ephrin B2 in port-wine stain endothelial progenitor cells contributes to clinicopathological vasculature dilatation. Br J Dermatol. 2017;177(6):1601–11.
Nguyen V, Hochman M, Mihm MC Jr, Nelson JS, Tan W. The pathogenesis of port wine stain and Sturge Weber syndrome: complex interactions between genetic alterations and aberrant MAPK and PI3K activation. Int J Mol Sci. 2019;20(9):2243.
van Raath MI, Bambach CA, Dijksman LM, Wolkerstorfer A, Heger M. Prospective analysis of the port-wine stain patient population in the Netherlands in light of novel treatment modalities. J Cosmet Laser Ther. 2018;20(2):77–84.
Klein A, Bäumler W, Landthaler M, Babilas P. Laser and IPL treatment of port-wine stains: therapy options, limitations, and practical aspects. Lasers Med Sci. 2011;26(6):845–59.
van Drooge AM, Beek JF, van der Veen JW, van der Horst CM, Wolkerstorfer A. Hypertrophy in port-wine stains: prevalence and patient characteristics in a large patient cohort. J Am Acad Dermatol. 2012;67(6):1214–9.
Heiser A, Jowett N, Occhiogrosso J, Tessler O, Tan OT. Societal-perceived health utility of hypertrophic facial port-wine stain and laser treatment. Facial Plast Surg Aesthetic Med. 2020;22(5):327–35.
De Borgie C, Bossuyt P, van der Horst C, van Gemert M. Introduction of the flash-lamp pulsed-dye laser treatment of facial port-wine stains in childhood: a case of health care technology assessment. Lasers Surg Med. 2001;28(2):182–9.
Sarig O, Kimel S, Orenstein A. Laser treatment of venous malformations. Ann Plast Surg. 2006;57(1):20–4.
Garden JM, Polla LL, Tan OT. The treatment of port-wine stains by the pulsed dye laser: analysis of pulse duration and long-term therapy. Arch Dermatol. 1988;124(6):889–96.
Sommer S, Sheehan-Dare RA. Pulsed dye laser treatment of port-wine stains in pigmented skin. J Am Acad Dermatol. 2000;42(4):667–71.
Wanitphakdeedecha R, Jantarakolica T, Ng JNC, Yan C, Nanchaipruek Y, Jantanapornchai N, et al. The cost-effectiveness of pulsed-dye laser therapy among Thai patients with facial port-wine stain: a retrospective study and economic evaluation. Dermatol Ther (Heidelb). 2021;11(2):465–73.
Wanitphakdeedecha R, Ng JNC, Yan C, Manuskiatti W, Sudhipongpracha T, Jantarakolica T. Quality of life and psychological effects of port-wine stain: a review of literature. Clin Cosmet Investig Dermatol. 2021;14:681.
van Raath MI, Chohan S, Wolkerstorfer A, van der Horst CM, Limpens J, Huang X, et al. Treatment outcome measurement instruments for port wine stains: a systematic review of their measurement properties. Dermatology. 2021;237(3):416–32.
Finlay AY, Khan G. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Hagen SL, Grey KR, Korta DZ, Kelly KM. Quality of life in adults with facial port-wine stains. J Am Acad Dermatol. 2017;76(4):695–702.
Masnari O, Schiestl C, Rössler J, Gütlein SK, Neuhaus K, Weibel L, et al. Stigmatization predicts psychological adjustment and quality of life in children and adolescents with a facial difference. J Pediatr Psychol. 2013;38(2):162–72.
van der Horst CM, De Borgie CA, Knopper JL, Bossuyt PM. Psychosocial adjustment of children and adults with port wine stains. Br J Plast Surg. 1997;50(6):463–7.
Lanigan S, Cotterill J. Psychological disabilities amongst patients with port wine stains. Br J Dermatol. 1989;121(2):209–15.
Wanitphakdeedecha R, Sudhipongpracha T, Ng JNC, Yan C, Jantarakolica T. Self-stigma and psychosocial burden of patients with port-wine stain: a systematic review and meta-analysis. J Cosmet Dermatol. 2021;20(7):2203–10.
Rencz F, Szabó Á, Brodszky V. Questionnaire modifications and alternative scoring methods of the dermatology life quality index: a systematic review. Value Health. 2021;24(8):1158–71.
Demellweek C, Humphris GM, Hare M, Brown J. Children’s perception of, and attitude towards, unfamiliar peers with facial port-wine stains. J Pediatr Psychol. 1997;22(4):471–85.
Jantarakolica T, Wanitphakdeedecha R, Yan C, Yogya Y, Sirisuthivoranunt S, Wongdama S, et al. Willingness to pay and time trade-off in Thai patients with port-wine stains. ClinicoEcon Outcomes Res. 2022;14:635–42.
Craig BM, Greiner W, Brown DS, Reeve BB. Valuation of child health-related quality of life in the United States. Health Econ. 2016;25(6):768–77.
Ravens-Sieberer U, Karow A, Barthel D, Klasen F. How to assess quality of life in child and adolescent psychiatry. Dialogues Clin Neurosci. 2022.
Wang J, Zhu Y-Y, Wang Z-Y, Yao X-H, Zhang L-F, Lv H, et al. Analysis of quality of life and influencing factors in 197 Chinese patients with port-wine stains. Medicine. 2017;96(51): e9446.
Gånemo A, Wahlgren CF, Svensson Å. Quality of life and clinical features in Swedish children with psoriasis. Pediatr Dermatol. 2011;28(4):375–9.
Hamann C, Egeberg A, Silverberg J, Gislason G, Skov L, Thyssen J. Exploring the association between parental psychiatric disease and childhood atopic dermatitis: a matched case–control study. J Eur Acad Dermatol Venereol. 2019;33(4):725–34.
Cazeau C, Blei F, Gonzáles Hermosa MRF, Cavalli R, Boccara O, Fölster-Holst R, et al. Burden of infantile hemangioma on family: an international observational cross-sectional study. Pediatr Dermatol. 2017;34(3):295–302.
Andrade G, Rangu S, Provini L, Putterman E, Gauthier A, Castelo-Soccio L. Childhood vitiligo impacts emotional health of parents: a prospective, cross-sectional study of quality of life for primary caregivers. J Patient-Report Outcomes. 2020;4(1):1–5.
Jiang F, Shao J, Chen L, Yang N, Liu J, Li Z. Influence of port-wine stains on quality of life of children and their parents. Acta Derm Venereol. 2021;101(8): adv00516.
Acknowledgements
We thank the participants of the study.
Medical Writing, Editorial, and Other Assistance
The authors wish to thank Ms. Phonsuk Yamlexnoi, Ms. Chutikan Kiatphansodsai, Ms. Apichaya Jutaphonrakul, and Dr. Surachet Sirisuthivoranunt for their assistance in recruiting subjects and managing the database.
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contribution
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Tatre Jantarakolica, Tatchalerm Sudhipongpracha, and Woraphong Manuskiatti. Rungsima Wanitphakdeedecha had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The first draft of the manuscript was written by Chadakan Yan and Yuri Yogya, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research project and the journal’s Rapid Service Fee was funded by the Faculty of Medicine Siriraj Hospital, Mahidol University.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tatre Jantarakolica, Rungsima Wanitphakdeedecha, Chadakan Yan, Yuri Yogya, Woraphong Manuskiatti, Tatchalerm Sudhipongpracha declare that they have no conflicts of interest.
Ethical Approval
The study was approved by the ethics committee of the Siriraj Institutional Review Board (SIRB protocol no. 941/2563/COA no. si 1059/2020). Written informed consent was obtained for the publication and use of all patients’ data prior to their enrollment in the study. This study was performed in accordance with the Helsinki Declaration of 1964 and its subsequent amendments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jantarakolica, T., Wanitphakdeedecha, R., Yan, C. et al. Dermatology Life Quality Index in Thai Patients with Facial Port-Wine Stains. Dermatol Ther (Heidelb) 13, 2375–2386 (2023). https://doi.org/10.1007/s13555-023-01011-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01011-0