Abstract
Introduction
Psoriasis ranges from mild to severe with the majority of patients having mild disease. Mild to moderate disease is often treated with topical therapies while photo-, oral, and biologic therapies are generally reserved for moderate-to-severe disease. There is a strong scientific rationale for the combination of calcipotriene (CAL) and betamethasone dipropionate (BDP) with respect to mode of action, efficacy, and safety and CAL/BDP has shown an inhibitory effect on key pathogenic cytokines in psoriasis including tumor necrosis factor-α, interleukin (IL)-17, and IL-23.
Methods
The objective of this pooled post hoc analysis is to investigate the efficacy of CAL/BDP polyaphron dispersion (PAD)-cream in subgroups of patients with moderate-to-severe psoriasis from two completed phase 3 studies conducted in the USA and Europe.
Results
The proportion of patients achieving Physician Global Assessment (PGA) treatment success as well as a modified Psoriasis Area and Severity Index (mPASI)75 response was higher in the subgroup with a body surface area > 10% and mPASI > 10 and Dermatology Life Quality Index > 10 at baseline compared to the overall patient population. Furthermore, the numerical difference in treatment efficacy between CAL/BDP PAD-cream and CAL/BDP topical suspension/gel increased in patient subgroups with higher baseline severity. Similar patterns were shown for the patient-reported outcomes.
Conclusion
In this subgroup analysis, patients who had higher disease severity at baseline achieved greater efficacy than the total patient population when treated with 8 weeks of CAL/BDP PAD-cream as compared to a currently marketed active comparator. Additionally, as indicated by this analysis, CAL/BDP PAD-cream treatment may also be more convenient and less greasy, which may reduce the burden of daily treatment and improve adherence to therapy.
Trial Registration
NCT03308799 and NCT03802344.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a need for topical psoriasis treatments that in addition to being highly efficacious also are convenient and easy to use, as this could reduce the burden of daily treatment and improve adherence to therapy and real-life outcome. |
The objective of this pooled post hoc analysis is to investigate the efficacy of calcipotriene (CAL)/betamethasone dipropionate (BDP) polyaphron dispersion (PAD)-cream in patients with moderate-to-severe psoriasis from two completed phase 3 studies conducted in the USA and Europe. |
The proportion of patients achieving Physician Global Assessment treatment success as well as a modified Psoriasis Area and Severity Index (mPASI)75 response was higher in the subgroup with a body surface area > 10% and mPASI > 10 and Dermatology Life Quality Index > 10 at baseline compared to the overall patient population. |
As indicated by this subgroup analysis, patients who had higher disease severity at baseline achieved greater efficacy than the total patient population when treated with 8 weeks of CAL/BDP PAD-cream as compared to a currently marketed active comparator. |
CAL/BDP PAD-cream is a non-greasy, easy spreadable cream that is scored high in convenience even by patients with moderate-to-severe disease, which makes it an option for some patients with moderate-to-severe psoriasis either as monotherapy or as adjunctive therapy to systemic/biologic agents. |
Introduction
Psoriasis is a common, chronic, immune-mediated, inflammatory skin disease. The prevalence of diagnosed psoriasis in the USA and Europe is approximately 3% [1,2,3]. Chronic stable plaque psoriasis (psoriasis vulgaris) is the most common form of the disease, accounting for 85–90% of cases [4] and manifests as raised, red patches or plaques with silvery scales. Psoriasis ranges from mild to severe with the majority of patients having mild disease (> 80%) [5]. The severity of chronic plaque psoriasis is generally assessed according to the Psoriasis Area and Severity Index (PASI), the body surface area (BSA), and the Physician Global Assessment (PGA). A patient’s quality of life (QoL) is commonly assessed by questionnaires including the Dermatology Life Quality Index (DLQI) [6]. Psoriasis severity can be categorized by BSA as mild (< 3%), moderate (3–10%), or severe (> 10%) [7]. Further, a PASI of > 10 is indicative of severe psoriasis [8] and with a DLQI of > 10 a skin disease is having a very severe impact on the patient’s QoL [9]. Based on this, the rule of tens (BSA > 10% or PASI > 10 or DLQI > 10) has been proposed as a criterion to identify patients with severe psoriasis [8].
Immunological and genetic studies have identified interleukin (IL)-17 and IL-23 as key drivers of psoriasis pathogenesis [10, 11] and multiple biologic therapies targeting these cytokines and tumor necrosis factor (TNF)-α are available. However, there is no cure for psoriasis. The goal of treatment is to reduce or eliminate its signs, symptoms, and impact on QoL. Mild to moderate disease is often treated with topical therapies while photo-, oral, and biologic therapies are generally reserved for moderate-to-severe disease [12]. Further, topical medications are frequently used as adjunctive therapies for patients on phototherapy or systemic therapy [13]. Of notice, some patients with severe psoriasis (BSA > 10%) are even treated with topicals alone [14]. Among topical therapies, the fixed combination treatment of a vitamin D analogue and a corticosteroid is commonly used [15, 16]. There is strong scientific rationale for the combination of vitamin D and corticosteroids with respect to mode of action, efficacy, and safety [17,18,19], and the combination of calcipotriene (CAL) and betamethasone dipropionate (BDP) is superior to each of the single agents [20,21,22]. Furthermore, CAL/BDP has an inhibitory effect on key pathogenic cytokines in psoriasis including TNFα, IL-17, and IL-23, and CAL normalizes keratinocyte differentiation and proliferation [17, 23]. The combination treatment with a vitamin D analogue and a topical corticosteroid is recommended in both American and European guidelines [24,25,26,27,28].
Application of topical therapies can be cumbersome, messy, and time-consuming. Thus, there is a need for topical psoriasis treatments that in addition to being highly efficacious also are convenient and easy to use, as this could reduce the burden of daily treatment and improve adherence to therapy and real-life outcome [29]. A CAL/BDP polyaphron dispersion (PAD)-cream has been developed, which contains a fixed dose combination of 0.005 w/w% CAL and 0.064 w/w% BDP using the proprietary PAD Technology™ that protects the drug substances from degradation during storage [30]. PAD Technology is a novel formulation and delivery system with enhanced drug penetration and high local tolerability [30]. Further, CAL/BDP PAD-cream is a non-greasy, easily spreadable white cream with a high patient satisfaction and treatment convenience [31,32,33]. CAL/BDP PAD-cream has been approved as Wynzora® both by the US Food and Drug Administration and several European Regulatory Agencies.
The objective of this pooled post hoc analysis is to investigate the efficacy of CAL/BDP PAD-cream in patients with moderate-to-severe psoriasis from two completed phase 3 studies conducted in the USA (NCT03308799) and Europe (NCT03802344).
Methods
Study Design
Study MC2-01-C2 (registered at ClinicalTrials.gov, NCT03308799) and study MC2-01-C7 (NCT03802344) were both phase III, randomized, investigator-blinded, multicenter, vehicle and comparator controlled, parallel-group, three-arm studies.
The studies comprised three periods (screening, treatment, and follow-up) as illustrated in Supplementary Fig. S1. Participants were randomly assigned into three treatment groups with a ratio of 3:1:3 for treatment with CAL/BDP PAD-cream (calcipotriene/betamethasone dipropionate, 0.005%/0.064 cream), matching vehicle and active comparator, respectively. Active comparators were marketed products in the USA and Europe: Taclonex® Topical Suspension (TS) and Dovobet®/Daivobet® Gel, respectively, with the exact same composition, that were approved for 8 weeks of treatment. The studies were investigator blinded as a result of differences in formulation, storage conditions, and packaging.
Subjects were to apply the investigational products (IPs) topically once daily preferable in the evening for 8 weeks to affected areas on the trunk (including the neck), the limbs, i.e., arms (including the back of the hands), the legs (including the buttocks and the top of the feet) and, in MC2-01-C7 only, and out of scope of this analysis, on the scalp.
Study Participants
Eligible subjects were generally healthy adults ages 18 years or above with mild-to-moderate chronic plaque psoriasis (according to PGA) of at least 6 months duration, involving the trunk and/or limbs, involving 2–30% of BSA, and a modified PASI (mPASI) ≥ 2 in MC2-01-C2 and an mPASI ≥ 3 in MC2-01-C7.
The studies were performed in accordance with the Helsinki Declaration of 1964 and its later amendments. The study protocols were approved by institutional review boards at each site, and all participants provided written informed consent prior to any study-related procedures. Both studies were designed to show therapeutic non-inferiority of CAL/BDP PAD-cream to the active comparator.
Study Assessments
The full analysis of the two phase III studies are presented elsewhere [34, 35]. This post hoc analysis focused on the following efficacy parameters in patients with moderate-to-severe psoriasis:
-
PGA success at week 8—defined as a PGA score of 0 (clear) or 1 (almost clear) and with a minimum 2-point improvement from baseline.
-
mPASI75 at week 8—proportion of subjects achieving ≥ 75% reduction from baseline in mPASI.
-
DLQI satisfaction (0/1) at week 8—indicating the disease burden has no impact on QoL.
-
Psoriasis Treatment Convenience Scale (PTCS) total score (the sum of question 1–5) at weeks 1 and 8—the scale evaluates treatment convenience and satisfaction and consists of 6 disease-specific, self-reported questions with a recall period of 1 week and rated on a numerical scale from 1 to 10.
-
The score of the 6 disease-specific PTCS questions at week 8.
Baseline characteristics that were used for the subgroup analysis of patients with moderate-to-severe psoriasis included the following:
-
BSA—The total psoriatic involvement on the trunk and limbs (excluding genital and intertriginous areas) was recorded as a percentage of the total BSA, estimating that the surface of the subject’s full, flat palm (including the five digits) correlating to approximately 1% of the total BSA.
-
The DLQI total score, which is the sum of the 10 equal-weighted questions relating to the degree to which the participants’ skin condition affects their daily activities. The scores from DLQI range between 0 and 30 with lower scores indicating better QoL. The DLQI is a validated patient-reported outcome where a score of 0 or 1 indicates that the disease burden has no impact on QoL (defined as DLQI satisfaction).
-
mPASI—the extent and severity of the subjects’ psoriasis on the body (trunk and/or limbs) excluding the scalp using an mPASI scoring system.
Analysis Methods
Patients in the “all patients” population (n = 1271) were from the pooled modified intention-to-treat (MITT) dataset and included subjects who were:(1) randomly assigned to any IP; (2) treated with the IP; and (3) had at least one assessment of PGA after starting treatment. For the subgroup analysis, subjects were grouped according to baseline severity; one group with subjects who had a BSA of > 10% at baseline (n = 321), one group with a mPASI of > 10 at baseline (n = 289), and one group with subjects who had a DLQI of > 10 at baseline (n = 505). Moderate-to-severe MITT patients were based on the rule of tens and included subjects who had BSA > 10% or mPASI > 10 or DLQI > 10 at baseline (n = 705) [8]. The “high severity” subgroup of patients (n = 104) was defined as patients who had all three of the severe baseline characteristics at baseline (BSA > 10% and mPASI > 10 and DLQI > 10) (Fig. 1). Post-baseline missing or invalid data were multiply imputed within treatment groups.
Results
Study Participants
A total of 796 participants were enrolled at 55 clinical sites in the US study, and 490 participants were enrolled at 32 clinical sites in the European study.
Demographic data (age, sex, and race) for the pooled MITT population was comparable between treatment arms. Baseline BSA, mPASI, PGA, Subject’s Global Assessment (SGA), and DLQI were also comparable between treatment arms [35]. Patient demographics were similar between the all patients (pooled MITT) population (n = 1271) and the subgroups, except that the baseline disease characteristics for the subgroups as expected showed increasing severity in all parameters compared to the all patients population (Table 1). The baseline disease characteristics of the BSA, mPASI, and DLQI for the high severity subgroup consisting of patients with baseline BSA > 10, mPASI > 10, and DLQI > 10 was approximately twice the level found in the all patients group.
PGA Treatment Success
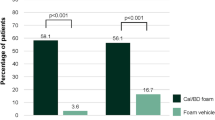
As shown in Fig. 2, the CAL/BDP PAD-cream treatment group had a statistically higher proportion of patients achieving PGA treatment success as compared to CAL/BDP TS/gel treatment in the all patients population at week 8 (43.2% vs. 31.9%, respectively) [35]. Significantly higher efficacy in favor of CAL/BDP PAD-cream compared to CAL/BDP TS/gel was also observed for all subgroups analyzed (Fig. 2). Further, the proportion of patients achieving PGA treatment success with CAL/BDP PAD-cream was higher in the high severity subgroup compared to the all patients population. In contrast, fewer patients in the high severity subgroup achieved PGA treatment success in the CAL/BDP TS/gel group compared to the all patients population. The numerical difference in treatment efficacy between CAL/BDP PAD-cream and CAL/BDP TS/gel was most pronounced in the high severity subgroup (difference of 28.6%, i.e., 48.1% (95% CI 34.5, 61.7) − 19.5% (95% CI 6.2, 32.8)).
Physician Global Assessment (PGA) treatment success at week 8. Proportion of patients (%) achieving PGA treatment success after 8 weeks of treatment with calcipotriene (CAL)/betamethasone dipropionate (BDP) polyaphron dispersion (PAD)-cream, CAL/BDP topical suspension (TS)/gel, or vehicle in the all patient population and higher severity subgroups
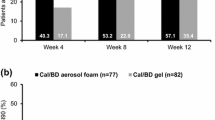
Proportion of Subjects Achieving mPASI 75
In the all patients population, the CAL/BDP PAD-cream treatment group had a statistically higher proportion of subjects who achieved a mPASI75 response at week 8 as compared to active CAL/BDP TS/gel treatment (44.3% vs. 34.5%, respectively; Fig. 3) [35]. Significantly higher efficacy in favor of CAL/BDP PAD-cream compared to CAL/BDP TS/gel was also observed for all subgroups analyzed in this study (Fig. 3). Further, the proportion of patients achieving mPASI75 at week 8 was higher in the high severity subgroup compared to the all patients population. The numerical difference in treatment efficacy between CAL/BDP PAD-cream and CAL/BDP TS/gel increased in patient subgroups with a higher baseline severity. The largest numerical difference in efficacy was observed in the high severity subgroup (difference of 36.0%) with the CAL/BDP PAD-cream treatment group having a mPASI75 of 54.6 (95% CI 40.9, 68.2) at week 8 versus a mPASI75 of 18.6% (95% CI 5.4, 31.8) in the CAL/BDP TS/gel group.
Modified Psoriasis Area and Severity Index (mPASI)75 at week 8. Proportion of subjects achieving mPASI75 after 8 weeks of treatment with CAL/BDP PAD-cream, CAL/BDP TS/gel, or vehicle in the all patients population and higher severity subgroups. CAL calcipotriene, BDP betamethasone dipropionate, TS topical suspension, PAD polyaphron dispersion
Patient-Reported Outcomes
Patient-reported outcomes in the combined phase 3 studies included DLQI and PTCS. PTCS was used to evaluate treatment convenience and overall patient satisfaction with treatment.
As shown in Fig. 4, CAL/BDP PAD-cream treatment had a significantly higher proportion of patients achieving a DLQI satisfaction (score of 0/1) at week 8 (p = 0.0005) as compared to the CAL/BDP TS/gel group. As would be expected, a trend towards a lower proportion of patients achieving DLQI satisfaction was present among the higher baseline severity subgroups. The numerical differences between the CAL/BDP PAD-cream and CAL/BDP TS/gel treatments were greater in the rule of tens subgroup and the high severity subgroup than in the all patients population with the highest numerical difference in the high severity subgroup (difference of 17.4%, i.e., 27.7% (95% CI 15.4, 40.1) − 10.3% (95% CI − 0.3, 20.9)). Interestingly, a significantly higher proportion of patients in the CAL/BDP PAD-cream arm achieved a DLQI of 0 or 1 compared to CAL/BDP TS/gel when looking at patients with a DLQI > 10 at baseline.
Dermatology Life Quality Index (DLQI) satisfaction at week 8. Proportion of subjects achieving DLQI of 0 or 1 (DLQI satisfaction) after 8 weeks of treatment with CAL/BDP PAD-cream, CAL/BDP TS/gel, or vehicle in the all patients population and higher severity subgroups. CAL calcipotriene, BDP betamethasone dipropionate, TS topical suspension, PAD polyaphron dispersion
Patients assessed the impact and convenience of the psoriasis treatment using the PTCS during the phase 3 studies. The scale consisted of six disease-specific, self-reported questions with a recall period of 1 week and rated on a numerical scale from 1 to 10. The PTCS total score was the sum of questions 1–5 and question 6 related to satisfaction with the treatment [36].
As shown in Table 2, the mean PTCS total score at week 1 of the CAL/BDP PAD-cream treatment group was significantly greater compared to the CAL/BDP TS/gel group both in the all patients population and in all individual subgroups. The significant differences in PTCS total scores between the treatment groups were maintained at week 8. Additionally, numerical differences between the CAL/BDP PAD-cream and CAL/BDP TS/gel treatments were greater in all higher baseline severity subgroups than the all patients population. The highest preference for CAL/BDP PAD-cream versus CAL/BDP TS/gel at week 8 was driven mainly by the individual PTCS questions concerning greasiness (questions 2 and 4) both for the all patients population and the rule of tens subgroup (Table 3).
Discussion
As shown in this post hoc subgroup analysis, the proportion of patients achieving PGA treatment success as well as an mPASI75 response was higher in the high severity subgroup compared to the all patients population. Furthermore, the numerical difference in treatment efficacy between CAL/BDP PAD-cream and CAL/BDP TS/gel increased in patient subgroups with higher baseline severity with the high severity subgroup having the highest numerical difference. Similar patterns were shown for the patient-reported outcomes.
Indicated by the investigator-evaluated efficacy data, patients who had greater disease severity at baseline achieved greater efficacy than the total pooled patient population when treated with 8 weeks of CAL/BDP PAD-cream treatment and the difference in treatment efficacy compared to CAL/BDP TS/gel generally increased as well.
Topical therapies can be used as a treatment option for moderate-to-severe psoriasis as indicated by previous studies [37, 38]. In a post hoc subgroup analysis of a phase 3 study, patients with baseline severity according to the rule of tens achieved numerically or statistically significant improvements with CAL/BDP foam compared to CAL/BDP TS/gel in PGA treatment success, mPASI75, and DLQI [39]; however, this was mainly at similar treatment success rates (32.0% for CAL/BDP foam) relative to the total mild-to-severe population (38.3%) [39, 40] in contrast to what we have shown here.
PASI75 is a measure of relative improvement with respect to baseline and therefore better treatment responses seen in the high severity subgroup compared to the all patients population may at least in part be explained as a function of the sensitivity of the measure. It is easier for an effective treatment to achieve a mPASI75 response in patients with a high PASI at baseline compared to patients with a lower PASI at baseline. However, the sensitivity of the measure cannot explain the observed differences between the PAD-cream and the gel formulation of CAL/BDP.
The high satisfaction and convenience of CAL/BDP PAD-cream demonstrated in this analysis may lead to better adherence to therapy and thereby potentially contribute to the better efficacy outcomes for this patient population. This may also translate into the real world, as seen in a non-interventional study with a topical agent where efficacy was higher in severe patients (Investigator’s Global Assessment = 4) compared to the total population of mild-to-severe patients [41]. In a survey, the most cited reason from the patient’s perspective for using topical therapy alone was fewer adverse effects than other treatments [14]. The safety profile of CAL/BDP PAD-cream is favorable and on par with other CAL/BDP products with no adverse drug reactions reported at a frequency > 1%. Another common reason for discontinuation is lack of effectiveness [14]. The efficacy outcomes we have shown here may contribute to the increased satisfaction with the treatment observed in this population.
Applying topical agents to a large BSA can be challenging. However, CAL/BDP PAD-cream is a non-greasy, easy spreadable cream that is scored high in convenience even by patients with moderate-to-severe disease, which makes it an option for some patients with moderate-to-severe psoriasis either as monotherapy or as adjunctive therapy to systemic/biologic agents. The high convenience of CAL/BDP PAD-cream is important. A survey conducted in 1281 European patients with psoriasis confirmed that cosmetic acceptability together with efficacy and safety is a very important aspect of a successful psoriasis treatment [42].
Limitations of this study include that it was a subgroup post hoc analysis of two pooled studies, which were not specifically designed for this analysis. Furthermore, the subgroups in this analysis are based on the rule of tens, although there is little consensus on the categorization and severity criteria of psoriasis.
Conclusions
In this subgroup analysis, patients who had higher disease severity at baseline achieved greater efficacy than the total patient population when treated with 8 weeks of CAL/BDP PAD-cream as compared to a currently marketed active comparator. Additionally, as indicated by this analysis, CAL/BDP PAD-cream treatment may also be more convenient and less greasy, which may reduce the burden of daily treatment and improve adherence to therapy.
References
Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003–2004. J Am Acad Dermatol. 2009;60(2):218–24.
Chandran V, Raychaudhuri SP. Geoepidemiology and environmental factors of psoriasis and psoriatic arthritis. J Autoimmun. 2010;34(3):J314–21.
Schafer T. Epidemiology of psoriasis. Review and the German perspective. Dermatology. 2006;212(4):327–37.
Nestle FO, Kaplan DH, Barker J. Mechanisms of disease: psoriasis. N Engl J Med. 2009;361(5):496–509.
Vanderpuye-Orgle J, Zhao Y, Lu J, et al. Evaluating the economic burden of psoriasis in the United States. J Am Acad Dermatol. 2015;72(6):961–7 (e5).
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) - simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Psoriasis Statistics: National Psoriasis Foundation. https://www.psoriasis.org/psoriasis-statistics/. Accessed 31 May 2023
Finlay AY. Current severe psoriasis and the rule of tens. Br J Dermatol. 2005;152(5):861–7.
Hongbo Y, Thomas CL, Harrison MA, Salek MS, Finlay AY. Translating the science of quality of life into practice: what do dermatology life quality index scores mean? J Invest Dermatol. 2005;125(4):659–64.
Hawkes JE, Chan TC, Krueger JG. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017;140(3):645–53.
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker J. Psoriasis. Lancet. 2021;397(10281):1301–15.
Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Elmets CA, Korman NJ, Prater EF, et al. Joint AAD-NPF Guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2021;84(2):432–70.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5.
Hoegsberg T, Iversen L, Lange MM, et al. Topical treatment of psoriasis: questionnaire results on topical therapy as long-term continuous treatment and use on specific body sites. J Dermatolog Treat. 2021;32(8):916–21.
Iversen L, Lange MM, Bissonette R, et al. Topical treatment of psoriasis: questionnaire results on topical therapy accessibility and influence of body surface area on usage. J Eur Acad Dermatol Venereol. 2017;31(7):1188–95.
Lovato P, Norsgaard H, Tokura Y, Ropke M. Calcipotriol and betamethasone dipropionate exert additive inhibitory effects on the cytokine expression of inflammatory dendritic cell-Th17 cell axis in psoriasis. J Dermatol Sci. 2016;81(3):153–64.
Gniadecki R, Gniadecka M, Serup J. Inhibition of glucocorticoid-induced epidermal and dermal atrophy with KH 1060–a potent 20-epi analogue of 1,25-dihydroxyvitamin D3. Br J Pharmacol. 1994;113(2):439–44.
Norsgaard H, Kurdykowski S, Descargues P, et al. Calcipotriol counteracts betamethasone-induced decrease in extracellular matrix components related to skin atrophy. Arch Dermatol Res. 2014;306(8):719–29.
Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomised, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20(4):465–71.
Kaufmann R, Bibby AJ, Bissonnette R, et al. A new calcipotriol/betamethasone dipropionate formulation (Daivobet) is an effective once-daily treatment for psoriasis vulgaris. Dermatology. 2002;205(4):389–93.
Lebwohl M, Tyring S, Bukhalo M, et al. Fixed combination aerosol foam calcipotriene 0.005% (Cal) plus betamethasone dipropionate 0.064% (BD) is more efficacious than Cal or BD aerosol foam alone for psoriasis vulgaris: a randomized, double-blind, multicenter, three-arm, phase 2 study. J Clin Aesthet Dermatol. 2016;9(2):34–41.
Segaert S, Shear NH, Chiricozzi A, et al. Optimizing anti-inflammatory and immunomodulatory effects of corticosteroid and vitamin D analogue fixed-dose combination therapy. Dermatol Ther (Heidelb). 2017;7(3):265–79.
Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 3. Guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60(4):643–59.
Samarasekera E, Sawyer L, Parnham J, Smith CH. Assessment and management of psoriasis: summary of NICE guidance. BMJ. 2012;345:e6712.
Hendriks AG, Keijsers RR, de Jong EM, Seyger MM, van de Kerkhof PC. Efficacy and safety of combinations of first-line topical treatments in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2013;27(8):931–51.
Elmets CA, Korman NJ, Prater EF, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2020;84(2):432–70.
Maul JT, Anzengruber F, Conrad C, et al. Topical treatment of psoriasis vulgaris: the Swiss treatment pathway. Dermatology. 2021;237(2):166–78.
Bewley A, Page B. Maximizing patient adherence for optimal outcomes in psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 4):9–14.
Praestegaard M, Steele F, Crutchley N. Polyaphron dispersion technology, a novel topical formulation and delivery system combining drug penetration, local tolerability and convenience of application. Dermatol Ther (Heidelb). 2022;12(10):2217–31.
Reich A, Selmer J, Galván J, et al. Efficacy, quality of life, and treatment satisfaction: an indirect comparison of calcipotriol/betamethasone dipropionate cream versus foam for treatment of psoriasis. Curr Med Res Opin. 2022;38(9):1521–9.
Bewley A, Barker E, Baker H, et al. An anchored matching-adjusted indirect comparison of fixed-dose combination calcipotriol and betamethasone dipropionate (Cal/BDP) cream versus Cal/BDP foam for the treatment of psoriasis. J Dermatolog Treat. 2022;33(8):3191–8.
Armstrong A, Pinter A, Selmer J, Praestegaard M, Reich A, Koo J. Pooled analysis demonstrating superior patient-reported psoriasis treatment outcomes for calcipotriene/betamethasone dipropionate cream versus suspension/gel. J Drugs Dermatol. 2022;21(3):242–8.
Stein Gold L, Green LJ, Dhawan S, Vestbjerg B, Praestegaard M, Selmer J. A phase 3, randomized trial demonstrating the improved efficacy and patient acceptability of fixed dose calcipotriene and betamethasone dipropionate cream. J Drugs Dermatol. 2021;20(4):420–5.
Pinter A, Green LJ, Selmer J, et al. A pooled analysis of randomized, controlled, phase 3 trials investigating the efficacy and safety of a novel, fixed dose calcipotriene and betamethasone dipropionate cream for the topical treatment of plaque psoriasis. J Eur Acad Dermatol Venereol. 2022;36(2):228–36.
Feldman SR, Præstegaard M, Andreasen AH, Selmer J, Holm-Larsen T. Validation of the self-reported psoriasis treatment convenience scale (PTCS). Dermatol Ther (Heidelb). 2021;11(6):2077–88.
Iversen L, Kurvits M, Snel-Prentø AM, Menter A. Calcipotriol/betamethasone dipropionate cutaneous foam treatment for psoriasis in patients with BSA 5–15% and PGA ≥ 3: post-hoc analysis from three randomized controlled trials. Dermatol Ther (Heidelb). 2020;10(5):1111–20.
Pinter A, Thormann H, Angeletti F, Jalili A. Calcipotriol/betamethasone dipropionate aerosol foam for the treatment of psoriasis vulgaris: case series and review of the literature. Clin Cosmet Investig Dermatol. 2018;11:451–9.
Paul C, Leonardi C, Menter A, et al. Calcipotriol plus betamethasone dipropionate aerosol foam in patients with moderate-to-severe psoriasis: sub-group analysis of the PSO-ABLE study. Am J Clin Dermatol. 2017;18(3):405–11.
Kircik L, Gold LS, Teng J, Moore A, Cantrell W, Alonso-Llamazares JKJ. Fixed combination calcipotriene and betamethasone dipropionate (Cal(BD) foam for beyond-mild psoriasis: a possible alternative to systemic medication. J Drugs Dermatol. 2020;19(8):723.
Gerdes S, Krakor M, Anger T, Hutt HJ, Korber A. Prospective, observational, non-interventional, multicentre study on the efficacy and tolerability of a new calcipotriol/Betamethasone Aerosol Foam (Enstilar®) in patients with plaque psoriasis under daily practice conditions. Dermatology. 2017;233(6):425–34.
Fouere S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(Suppl 3):2–6.
Acknowledgements
We thank study participants for their involvement in the study.
Funding
Studies presented herein as well as the Rapid Service Fee were funded by MC2 Therapeutics.
Medical Writing, Editorial and Other Assistance
We thank Frank Freischläger, Founder and Senior Principal Statistical Writer at Estimondo for performing all the statistical analyses for this paper. This assistance was funded by MC2 Therapeutics.
Anja Snel-Prentø, MedLink, provided medical writing and editorial assistance in preparation of this article, which was funded by MC2 Therapeutics.
Author Contributions
Morten Præstegaard contributed to the study conception and design. Morten Præstegaard and Lars Iversen contrbuted to the analysis and interpretation of the data. As investigators, data collection was performed by Linda Stein Gold, Andreas Pinter, April Armstrong, Matthias Augustin, Petr Arenberger, Neil Bhatia, Adam Reich. All authors reviewed draft versions of the manuscript and read and approved the final manuscript.
Disclosures
Linda Stein Gold is an investigator, advisor and/or speaker for MC2, EPI, Ortho Derm, Dermavant, Arcutis, Pfizer, Lilly, Abbvie, Novartis, BMS, and UCB. Andreas Pinter has served as an advisor and/or paid speaker for and/or participated in clinical trials sponsored by: AbbVie, Almirall-Hermal, Amgen, Biogen Idec, Biontec, BMS, Boehringer-Ingelheim, Celgene, Celltrion, GSK, Eli-Lilly, Eva Pharma, Galderma, Hexal, Janssen, Klinge Pharma, LEO-Pharma, MC2, Medac, Merck Serono, Mitsubishi, Moonlake, MSD, Novartis, Pascoe, Pfizer, Tigercat Pharma, Regeneron, Roche, Sandoz Biopharmaceuticals, Sanofi-Genzyme, Schering-Plough, UCB Pharma and Zuellig Pharma. April Armstrong has served as a research investigator and/or scientific advisor to AbbVie, Almirall, Arcutis, ASLAN, Beiersdorf, BI, BMS, EPI, Incyte, Leo, UCB, Janssen, Lilly, Nimbus, Novartis, Ortho Dermatologics, Sun, Dermavant, Dermira, Sanofi, Regeneron, Pfizer, and Modmed. Matthias Augustin received consultant fees, speaker's honoraries and/or research grants from companies that manufacture drugs used for the treatment of psoriasis, including Abbvie, Almirall, Amgen, Biogen, BMS, Boehringer Ingelheim, Celgene, Celltrion, Eli-Lilly, Hexal, Janssen-Cilag, LEO, MC2 therapeutics, Medac, Milan, Novartis, Pfizer, Sandoz and UCB. Petr Arenberger declares that he has no competing interests. Neil Bhatia has served as an advisor and investigator with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, J&J, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, P&G, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Morten Praestegaard and Lars Iversen are employees of MC2 Therapeutics. Adam Reich has worked as a consultant or speaker for AbbVie, Bioderma, Celgene, Chema Elektromet, Eli Lilly, Galderma, Janssen, Leo Pharma, Medac, Menlo Therapeutics, Novartis, Pierre-Fabre, Sandoz, and Trevi, and participated as Principal Investigator or Subinvestigator in clinical trials sponsored by AbbVie, Drug Delivery Solutions Ltd, Galderma, Genentech, Janssen, Kymab Limited, Leo Pharma, Menlo Therapeutics, MetrioPharm, MSD, Novartis, Pfizer, and Trevi.
Compliance with Ethics Guidelines
The studies were performed in accordance with the Helsinki Declaration of 1964 and its later amendments. The study protocols were approved by institutional review boards at each site, and all participants provided written informed consent prior to any study-related procedures. A list of study sites is available as Supplementary Table 1.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Stein Gold, L., Pinter, A., Armstrong, A. et al. Calcipotriene and Betamethasone Dipropionate PAD-Cream Demonstrates Greater Treatment Efficacy in Patients with Moderate-to-Severe Psoriasis Compared to Topical Suspension/Gel: A Subgroup Analysis of Two Phase 3 Studies. Dermatol Ther (Heidelb) 13, 2031–2044 (2023). https://doi.org/10.1007/s13555-023-00979-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-00979-z