Abstract
Introduction
Limited access to healthcare during the COVID-19 pandemic prompted patients to seek care using telehealth. In this study, we assessed whether treatment patterns differed for patients with psoriasis (PsO) or psoriatic arthritis (PsA) initiating apremilast by either a telehealth or an in-person visit.
Methods
We estimated adherence and persistence among US patients in the Merative© MarketScan© Commercial and Supplemental Medicare Databases who newly initiated apremilast between April and June 2020, categorized by the type of visit (telehealth or in-person) when apremilast was first prescribed. Adherence was defined as the proportion of days covered (PDC), with PDC ≥ 0.80 considered to indicate high adherence. Persistence was defined as having apremilast available to take without a 60-day gap during follow-up. Factors associated with high adherence and persistence were estimated with logistic and Cox regression.
Results
Among apremilast initiators (n = 505), the mean age was 47.6 years, 57.8% were female, and the majority had PsO (79.6%). Telehealth index visits were more likely among patients residing in Northeast USA (odds ratio [OR] 3.31, 95% confidence interval [CI] 1.63–6.71) and Western USA (OR 2.52, 95% CI 1.07–5.93]), those with a prescribing rheumatologist (OR 2.27, 95% CI 1.10–4.68), and those with any baseline telehealth visit (OR 1.91, 85% CI 1.20–3.04). Those initiating apremilast with a telehealth visit (n = 141) had similar mean PDC to those initiating apremilast with an in-person visit (n = 364) (0.695 vs. 0.728; p = 0.272). At the end of the 6-month follow-up, 54.3% of the overall population had high adherence (PDC ≥ 0.80) and 65.1% were persistent. After adjusting for potential confounders, patients initiating apremilast via telehealth had similar full adherence (OR 0.80, 95% CI 0.52–1.21) and persistence as those initiating apremilast in-person.
Conclusion
Patients with PsO and patients with PsA initiating apremilast via telehealth or in-person during the COVID-19 pandemic had similar medication adherence and persistence during the 6-month follow-up period. These data suggest that patients initiating apremilast can be as effectively managed with telehealth visits as with in-person visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Limited access to healthcare during the COVID-19 pandemic prompted patients with psoriasis (PsO) and psoriatic arthritis (PsA) to seek care using telehealth. |
This study assessed whether treatment patterns differed for patients with PsO or PsA initiating apremilast by either a telehealth or an in-person visit. |
What was learned from the study? |
Apremilast initiators with a telehealth index visit were younger, more likely to reside in the Northeast and the Western USA, to have seen a rheumatologist, and to have had another telehealth visit during baseline. |
Patients initiating apremilast via a telehealth visit had similar adherence and persistence to those initiating via an in-person visit. |
Coupled with oral dosing, no pre-screening, and no laboratory monitoring requirements, these data suggest apremilast initiation can be effectively managed with telehealth visits, although future research is needed to assess the impact of additional clinical and treatment factors (e.g., type of PsO and concomitant therapy) on effective management via telehealth. |
Introduction
Psoriasis (PsO) is a chronic inflammatory skin disease that affects approximately 7.4 million adults in the USA [1], of whom as many as 42% will develop psoriatic arthritis (PsA), an inflammatory musculoskeletal disease [2, 3]. Due to the cyclical nature of the disease (flares and remission), patients with PsO and PsA endure physical and psychosocial manifestations of the disease as well as significant economic burden [1, 2, 4,5,6,7,8,9,10,11]. PsO and PsA are life-long diseases without a definitive cure, and as such, a sequence of consecutive pharmacological agents is necessary as disease progresses [12, 13].
Treatment options for PsO and PsA include oral small-molecule (OSM) therapies and biologic therapies [14]. Nonsteroidal anti-inflammatory drugs and corticosteroids are used as symptomatic therapies [15, 16]. Choice of an effective therapy for PsO and PsA is complicated due to variations in patient profiles (i.e., disease severity, contraindications of comorbidities), varied routes of administration, insurance coverage, cost, and side effect profiles of the different therapies [17,18,19].
Prior to the coronavirus disease 2019 (COVID-19) pandemic, telehealth as an add-on intervention to in-person visits had been shown to improve medication adherence among patients with diabetes, hypertension, asthma, sleep disorders, and mental illnesses [20,21,22,23]. Medication nonadherence leads to negative effects on clinical outcomes and comorbidities, drives excess healthcare utilization and costs, and may account for up to 50% of treatment failures, 125,000 deaths, and 25% of hospitalizations annually [24, 25]. During the COVID-19 pandemic, states and territories in the USA implemented stay-at-home orders and restrictions to limit the spread of the infection. These restrictions prompted many patients to seek care virtually using telehealth [26].
Apremilast is an OSM-targeted phosphodiesterase-4 (PDE4) inhibitor indicated for the treatment of plaque psoriasis, active PsA, and Behcet’s disease with oral ulcers. This drug has no pre-screening or laboratory monitoring requirements and is well-tolerated with a favorable safety profile, suggesting it may be an effective treatment option during the COVID-19 pandemic and in the telehealth setting in general.
Studies in other disease areas, both prior to and during the COVID-19 pandemic, have shown that telehealth can be used to effectively manage patients’ treatment [27, 28]. However, it is unknown how telehealth during the pandemic impacted the medication use in patients with PsO or PsA treated with apremilast. The objective of this study was to assess if treatment patterns differed for patients with PsO and patients with PsA who initiated apremilast after a telehealth visit versus an in-person visit in a real-world setting.
Methods
Study Design and Data Source
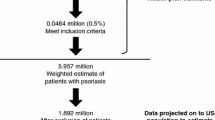
This study employed a retrospective cohort design using administrative claims data from the Merative® MarketScan® Commercial and Medicare Supplemental databases from 1 October 2019 to 31 December 2020. The index date was the date of the first claim for apremilast during the identification period (1 April 2020 to 30 June 2020). The baseline period was 6 months before the index date, and the follow-up period was 6 months after the index date. We also used an identification period from 1 April 2019 to 30 June 2019 to benchmark pre-pandemic treatment patterns. The study schema is presented in Fig. 1.
Study schema. This study used administrative claims data from 1 October 2019 to 31 December 2020. The index date was the date of the first claim for apremilast during the identification period (1 April 2020 to 30 June 2020). The baseline period was 6 months before the index date, and the follow-up period was 6 months after the index date
The MarketScan Commercial and Medicare Supplemental Databases include data on health services for > 43.6 million employees, dependents, and retirees in the USA with primary or Medicare supplemental coverage through privately insured fee-for-service, point-of-service, or capitated health plans. The databases include enrollment information and claims with healthcare utilization information (e.g., inpatient and outpatient services, and prescription drug claims). Institutional Review Board approval to conduct this study was not necessary, as this study used de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data. The datasets generated during and/or analyzed during the current study are not publicly available as they were licensed by the authors’ institution for use only in this study. In order to access the claims data used in this study, a license between PHAR and the data vendor was required, as noted in the current data availability statement, and PHAR was only able to access the data from the data vendor after signing a licensed agreement with the data vendor.
Patient Population
Patients diagnosed with PsO or PsA were identified based on the presence of: (1) at least one diagnosis by a dermatologist or rheumatologist for plaque PsO (International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] diagnosis codes L40.0, L40.8, L40.9), or (2) at least one diagnosis for PsA (ICD-10-CM codes L40.50, L40.51, L40.52, L40.53, L40.59) recorded by a dermatologist or rheumatologist during the entire study period (1 October 2019 to 31 December 2020). Similar ICD-10-CM diagnosis codes have been used to identify patients with PsO and patients with PSA in previous research [29, 30]. Patients were included if they initiated apremilast during the identification period. Patients were required to be at least 18 years of age on the index date (apremilast initiation date), have continuous enrollment for at least 6 months prior to (baseline period) and 6 months after (follow-up period) the index date, and have at least one of the diagnosis claims for PsO or PsA within 90 days prior to or on the index date. The claim closest to the index date was used to assign patients to an index visit type, i.e., in-person or telehealth. The index setting was identified via an algorithm utilizing Current Procedural Terminology (CPT®) codes, the Healthcare Common Procedural Coding System (HCPCS), National Drug Code (NDC) codes, and other modifiers (see Electronic Supplementary Material [ESM] Table S1).
Patients were excluded if they had other biologic-indicated conditions (e.g., ulcerative colitis, Crohn's disease, rheumatoid arthritis and other inflammatory polyarthropathies, ankylosing spondylitis, giant cell arteritis, non-radiographic axial spondyloarthritis, uveitis, or hidradenitis suppurativa) [31, 32] during baseline or follow-up periods, or had newly started apremilast along with another systemic treatment for PsO or PsA on the index date.
Study Measures and Analysis
The outcomes were adherence and persistence to apremilast therapy. Adherence to apremilast therapy was measured as the proportion of days covered (PDC) during the follow-up period. PDC is a preferred method of measuring medication adherence and was calculated by the number of days with apremilast available divided by the number of days of follow-up period (180 days) [33]. Full adherence was defined as PDC ≥ 0.80. Apremilast therapy persistence was defined as continuous use from the index date to the end of available days’ supply of apremilast therapy without a gap of ≥ 60 days [18]. We reported the proportion of patients that persisted with apremilast during the follow-up period. Demographic characteristics, diagnosis of index visit (PsA vs. PsO), prescriber specialty (defined as the specialty on the medical claim closest in time to the index date), comorbidities, including the Charlson Comorbidity Index, and medication use were measured in the baseline period.
Descriptive statistics, including means and standard deviations (SD) for continuous data and relative frequencies and percentages for categorical data, were reported. Chi-square tests and t-tests were used to compare proportions and means, respectively, between those initiating apremilast via a telehealth visit or via an in-person visit. The telehealth and in-person cohorts were compared for the rate of full adherence to apremilast (PDC ≥ 0.80) using logistic regression models, and for the risk of discontinuation (persistence) of apremilast using Cox regression models and Kaplan–Meier analyses. The covariates used in those two models included age, gender, region, physician specialty at index visit, diagnosis of index visit (PsA vs. PsO), any systemic non-biologic use in the baseline (yes vs. no), and any systemic biologic use in the baseline (yes vs. no). A logistic regression model was performed to study the association between type of visit for the initiation and baseline characteristics. In addition to the covariates used in the adherence and persistence models, the independent variables for this model included any baseline telehealth visit before the index telehealth visit. Adjusted odds ratio (OR) and 95% confidence intervals (CI) were reported for the logistic regression model while adjusted hazard ratio (HR) and 95% CI were reported for the Cox regression model. All data transformations and statistical analyses were performed using SAS© version 9.4 (SAS Institute, Cary, NC, USA).
Results
Among the total of 505 patients with PsO or PsA who initiated apremilast between 1 April 2020 and 30 June 2020, 141 patients initiated the drug via a telehealth visit and 364 patients initiated it via an in-person visit. Baseline patient characteristics are shown in Table 1. The mean age for both cohorts was similar (46.8 [telehealth] vs. 48 years [in-person]; p = 0.304). The proportion of females was 61.7% in the telehealth cohort versus 56.3% in the in-person cohort. At the index visit, the telehealth cohort had a lower proportion of patients with a PsO diagnosis compared to the in-person cohort (72.3% vs. 82.4%, respectively) and a higher proportion of patients with a PsA diagnosis (27.7% vs. 17.6%, respectively; p = 0.012). Compared to the in-person cohort, more than twofold as many patients in the telehealth cohort visited a rheumatologist (28.4% vs. 12.1%) on the index visit. Both cohorts had similar comorbidities at baseline. A significantly higher proportion of patients in the telehealth cohort received non-apremilast systemic therapy during the baseline period compared to the in-person cohort (36.2% vs. 22.3%, respectively; p = 0.001). During baseline, higher proportions of patients in the telehealth cohort had systemic non-biologic (18.4% vs. 10.4%, respectively; p = 0.015) as well as systemic biologic (22.7% vs. 13.5%, respectively; p = 0.011) therapy use.
During the 6-month follow-up period, patients in the telehealth cohort had similar mean PDC (SD) as the in-person cohort (0.695 [0.308] vs. 0.728 [0.290]; p = 0.272). The proportion of patients with full adherence (PDC ≥ 0.80) was also similar across both cohorts (49.6% [telehealth] vs. 56% [in-person; p = 0.195). The proportion of patients initiating apremilast via a telehealth visit had similar persistence (without a ≥ 60-day gap) to those initiating in-person (62.4% vs. 66.2%, respectively; p = 0.422). Figure 2 illustrates the days to discontinuation for both cohorts. Mean duration of apremilast continuation without a ≥ 60-day gap was similar in both groups (132.3 [telehealth] vs. 137.9 [in-person] days; p = 0.312). Similar persistence and adherence findings were observed in the pre-pandemic period, from 1 April 2019 to 30 June 2019 (see ESM Table S2; ESM Fig. S1).
A telehealth visit at index was more likely among younger patients (OR 0.98, 95% CI 0.96–1.00; p = 0.025), patients visiting a rheumatologist (OR 2.27, 95% CI 1.10–4.68; p = 0.027), and patients with any baseline telehealth visit compared to their counterparts (OR 1.91, 95% CI 1.20–3.04; p = 0.007) (Table 2).
After adjusting for age, gender, region, physician specialty at index visit, diagnosis of index visit (PsA vs. PsO), any systemic non-biologic use in the baseline, and any systemic biologic use in the baseline, patients initiating apremilast via a telehealth visit had similar risks of discontinuation (HR 1.02, 95% CI 0.79–1.32; p = 0.875] and similar full adherence (OR 0.80, 95% CI 0.52–1.21; p = 0.288) compared to those initiating apremilast in-person (Table 3). Adjusted estimates for adherence were 56.1% for in-person initiators of apremilast and 50.4% for telehealth initiators; patients with a PsO index diagnosis had an adjusted adherence rate of 57.8%, while that of patients with a PsA index diagnosis was 41.3%. Furthermore, older patients (OR 1.03, 95% CI 1.01–1.04; p < 0.001) and those with PsO as the diagnosis at the index visit (OR 0.51, 95% CI 0.29–0.91; p = 0.022) were more likely to be fully adherent than their counterparts.
Discussion
Treatment adherence has been recognized as a key measure of quality, and treatment nonadherence is one of the leading causes of preventable morbidity, mortality, and healthcare expenditure [34, 35]. This study of an adult population diagnosed with PsO or PsA using administrative claims found that patients initiating apremilast via a telehealth visit had similar medication adherence and persistence to those initiating apremilast via an in-person visit. This study identified a number of factors associated with adherence and initiating apremilast via a telehealth visit. Overall, the pre- and post-pandemic cohorts in our analysis had similar medication adherence and persistence.
Telehealth services have expanded over the last 5 years, but the increase in these services significantly increased during the COVID-19 pandemic as in-person medical services for multiple diseases were postponed or cancelled [36, 37]. In addition, patients receiving healthcare via telehealth services maintained or increased medication adherence and increased medication fills compared to those with in-person visits [28, 38,39,40,41,42,43,44]. Our study findings corroborate those from previous studies using telehealth on patients with PsO and PsA [45,46,47,48]. For example, a randomized controlled trial showed similar effectiveness between telehealth and in-person consultation in managing patients with PsO. In another study on PsO during the pandemic, patients preferred telemedicine for safety reasons, convenience, and saving time [49]. These findings suggest telehealth can continue to be used for patients with PsO and patients with PsA even after the pandemic.
We observed higher telehealth utilization in younger patients compared to older ones. One survey of telehealth utilization among rheumatology patients reported less access to phones and cameras was correlated with age, and older patients did not have confidence that their needs could be managed over the phone; younger patients reported conflicts with daily work and appointments as a reason for telehealth use [50]. In our study, patients initiating apremilast via telehealth were more likely to have seen a rheumatologist. This is consistent with a study that reported a sharp increase in telehealth use by rheumatologists [38], and a systematic review showed telehealth visits led to similar disease activity control and patient-reported outcomes as in-person care [51]. Finally, we found patients initiating apremilast via telehealth were more likely to have had a telehealth visit during baseline. A study has shown patients with prior experience with telehealth were more likely to prefer future telehealth visits [52].
Limitations and Bias
Our study has limitations. First, this retrospective observational analysis used administrative claims. These data lack important clinical details and patient perspectives providing information related to disease severity and symptoms. Hence, the study lacked some information to control for potentially confounding variables. However, we have adjusted our modeling analyses for several measurable proxies of disease severity. Second, administrative claims data do not reflect whether medications are taken as prescribed; thus, in studying adherence we can only rely on information regarding medication fills. Third, claims data used for this analysis are generated for reimbursement, not research, and coding errors, misclassification, diagnostic uncertainty, and/or omissions could affect the findings. Nevertheless, health insurance claims data contain a large and valid sample of patient characteristics in a real-world setting. Finally, this study was limited to individuals with commercial and Medicare supplemental insurance coverage and thus may not be generalizable to other populations.
Conclusion
In a patient population with commercial and Medicare supplemental insurance, patients initiating apremilast in the telehealth setting had similar medication adherence and persistence as those initiating in the in-person setting. Telehealth has been recognized by the International Psoriasis Council as a key element in the delivery of dermatological care, and apremilast was deemed a suitable choice for initiation and continuation of PsO care [50]. These real-world data add confidence to this recommendation. Apremilast initiation is a simple process requiring no pre-screening or laboratory monitoring. These findings suggest that patients with PsO and patients with PsA initiating apremilast may be effectively managed via telehealth visits, although future research is needed to assess the impact of additional clinical and treatment factors (such as type of psoriasis and concomitant therapy) on effective management via telehealth.
Change history
23 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s13555-023-00984-2
References
Langley RGB, Krueger GG, Griffiths CEM. Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005;64(Suppl 2):ii18–23.
Gladman DD, Antoni C, Mease P, Clegg DO, Nash P. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(Suppl 2):ii14–7.
Brockbank J, Gladman D. Diagnosis and management of psoriatic arthritis. Drugs. 2002;62(17):2447–57.
Pilon D, Teeple A, Zhdanava M, et al. The economic burden of psoriasis with high comorbidity among privately insured patients in the United States. J Med Econ. 2019;22(2):196–203.
Vanderpuye-Orgle J, Zhao Y, Lu J, et al. Evaluating the economic burden of psoriasis in the United States. J Am Acad Dermatol. 2015;72(6):961-967.e5.
Ogdie A, Hwang M, Veeranki P, et al. Health care utilization and costs associated with functional status in patients with psoriatic arthritis. J Manag Care Spec Pharm. 2022;28(9):997–1007.
Stewart TJ, Tong W, Whitfeld MJ. The associations between psychological stress and psoriasis: a systematic review. Int J Dermatol. 2018;57(11):1275–82.
Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y. The psychosocial burden of psoriasis. Am J Clin Dermatol. 2005;6(6):383–92.
Armstrong AW, Schupp C, Wu J, Bebo B. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003–2011. PLoS One. 2012;7(12):e52935.
Gudu T, Kiltz U, de Wit M, Kvien TK, Gossec L. Mapping the effect of psoriatic arthritis using the international classification of functioning, disability and health. J Rheumatol. 2017;44(2):193–200.
Feldman SR, Zhao Y, Shi L, Tran MH, Lu J. Economic and comorbidity burden among moderate-to-severe psoriasis patients with comorbid psoriatic arthritis. Arthritis Care Res (Hoboken). 2015;67(5):708–17.
Singh JA, Guyatt G, Ogdie A, et al. 2018 American College of Rheumatology/National Psoriasis Foundation Guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol. 2019;71(1):5–32.
American Academy of Dermatology Association. Psoriasis clinical guideline. 2023. https://www.aad.org/member/clinical-quality/guidelines/psoriasis. Accessed 6 Dec 2022.
Ogdie A, Coates LC, Gladman DD. Treatment guidelines in psoriatic arthritis. Rheumatology. 2020;59(Supplement_1):i37–46.
Feldman SR, Goffe B, Rice G, et al. The challenge of managing psoriasis: unmet medical needs and stakeholder perspectives. Am Health Drug Benefits. 2016;9(9):504–13.
Menter A, Gottlieb A, Feldman SR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58(5):826–50.
Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135(12):2955–63.
Higa S, Devine B, Patel V, Baradaran S, Wang D, Bansal A. Psoriasis treatment patterns: a retrospective claims study. Curr Med Res Opin. 2019;35(10):1727–33.
Xu Y, Sudharshan L, Hsu M-A, et al. Patient preferences associated with therapies for psoriatic arthritis: a conjoint analysis. Am Health Drug Benefits. 2018;11(8):408–17.
Lin NY, Ramsey RR, Miller JL, et al. Telehealth delivery of adherence and medication management system improves outcomes in inner-city children with asthma. Pediatr Pulmonol. 2020;55(4):858–65.
Parikh R, TouVelle MN, Wang H, Zallek SN. Sleep telemedicine: patient satisfaction and treatment adherence. Telemed e-Health. 2011;17(8):609–14.
Schulze LN, Stentzel U, Leipert J, et al. Improving medication adherence with telemedicine for adults with severe mental illness. Psychiatr Serv. 2019;70(3):225–8.
Pouls BPH, Vriezekolk JE, Bekker CL, et al. Effect of interactive ehealth interventions on improving medication adherence in adults with long-term medication: systematic review. J Med Internet Res. 2021;23(1):e18901.
Headley M. Managing medication adherence during COVID-19. Patient Safety Quality Healthcare. 2020. https://www.psqh.com/analysis/managing-medication-adherence-during-covid-19/. Accessed 25 Nov 2022.
Kim J, Combs K, Downs J, Tillman F III. Medication adherence: the elephant in the room. US Pharm. 2018;43(1):30–4.
Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–62.
Efe C, Simşek C, Batıbay E, Calışkan AR, Wahlin S. Feasibility of telehealth in the management of autoimmune hepatitis before and during the COVID-19 pandemic. Expert Rev Gastroenterol Hepatol. 2020;14(12):1215–9.
Lippincott CK, Perry A, Munk E, Maltas G, Shah M. Tuberculosis treatment adherence in the era of COVID-19. BMC Infect Dis. 2022;22(1):800.
Heidbrede T, Mevius A, Kessel S, Wilke T, Maywald U, Thiem A. Real-world systemic treatment of patients with psoriasis: a retrospective study based on German claims data. J Deutsche Dermatol Gesell. 2023;21(6):611-9. https://doi.org/10.1111/ddg.15030.
Merola JF, Tian H, Patil D, et al. Incidence and prevalence of psoriatic arthritis in patients with psoriasis stratified by psoriasis disease severity: retrospective analysis of an electronic health records database in the United States. J Am Acad Dermatol. 2022;86(4):748–57.
Wu JJ, Pelletier C, Ung B, Tian M. Real-world treatment patterns and healthcare costs among biologic-naive patients initiating apremilast or biologics for the treatment of psoriasis. J Med Econ. 2019;22(4):365–71.
Wu JJ, Pelletier C, Ung B, Tian M. Treatment patterns and healthcare costs among biologic-naive patients initiating apremilast or biologics for the treatment of psoriatic arthritis: results from a US claims analysis. Curr Med Res Opin. 2020;36(1):169–76.
Nau D. Proportion of Days Covered (PDC) as a Preferred Method of Measuring Medication Adherence. Pharmacy Quality Alliance, Springfield. http://www.pqaaliance.org/files/PDCvsMPRfinal.pdf. Accessed 3 Jan 2023.
Chaudri NA. Adherence to long-term therapies evidence for action. Ann Saudi Med. 2004;24(3):221–2.
Optum, Inc. Medication adherence: Rx for success. 2012. https://www.optum.com/content/dam/optum3/optum/en/resources/white-papers/MedicationAdherence_WhitePaper.pdf. Accessed 1 Feb 2023.
Ibis World. Telehealth services in the US—market Ssze 2005–2029. 2023. https://www.ibisworld.com/industry-statistics/market-size/telehealth-services-united-states/. Accessed 1 Feb 2023.
Grand View Research. Telehealth market size, share & trends analysis report by product type (software, services), by delivery mode (cloud-based, web-based), by end-use (payers, patients), by disease area, by region, and segment forecasts, 2023-2030. https://www.grandviewresearch.com/industry-analysis/telehealth-market-report. Accessed 1 Feb 2023.
Kwok TSH, Kuriya B, King LK, et al. Changes in service delivery and access to rheumatologists before and during the COVID-19 pandemic in a Canadian universal healthcare setting. J Rheumatol. 2022. https://doi.org/10.3899/jrheum.220658.
Vicente MA, Fernández C, Guilabert M, et al. Patient engagement using telemedicine in primary care during COVID-19 pandemic: a trial study. Int J Environ Res Public Health. 2022;19(22):14682.
Edwards AM, Petitt JC, Kumar S, Levin JB, Sajatovic M. Pre COVID-19 pandemic use of telemedicine for adherence promotion in patients with psychotic disorders: a literature review. Patient Prefer Adherence. 2022;16:2559–65.
Bruns BE, Lorenzo-Castro SA, Hale GM. Controlling blood pressure during a pandemic: the impact of telepharmacy for primary care patients. J Pharm Pract. 2022. https://doi.org/10.1177/08971900221136629.
Kim HJ, Tomaszewski M, Zhao B, et al. Impact of telehealth on medication adherence in chronic gastrointestinal diseases. J Can Assoc Gastroenterol. 2022;5(5):203–7.
Cvietusa PJ, Goodrich GK, Steiner JF, et al. Transition to virtual asthma care during the COVID-19 pandemic: an observational study. J Allergy Clin Immunol. 2022;10(6):1569–76.
Woodhouse AG, Orvin C, Rich C, Crosby J, Keedy CA. Diabetes outcomes before and during telehealth advancements surrounding COVID-19. J Am Pharm Assoc. 2022;62(1):214–7.
Balato N, Megna M, Di Costanzo L, Balato A, Ayala F. Educational and motivational support service: a pilot study for mobile-phone-based interventions in patients with psoriasis: telepsoriasis services. Br J Dermatol. 2013;168(1):201–5.
Koller S, Hofmann-Wellenhof R, Hayn D, et al. Teledermatological monitoring of psoriasis patients on biologic therapy. Acta Derm Venerol. 2011;91(6):680–5.
Armstrong AW, Chambers CJ, Maverakis E, et al. Effectiveness of online vs. in-person care for adults with psoriasis: a randomized clinical trial. JAMA Netw Open. 2018;1(6): e183062.
Chevallard M, Belloli L, Ughi N, et al. Use of telemedicine during the COVID-19 pandemic in patients with inflammatory arthritis: a retrospective study on feasibility and impact on patient-reported outcomes in a real-life setting. Rheumatol Int. 2021;41(7):1253–61.
Gisondi P, Bellinato F, Piaserico S, Di Leo S, Cazzaniga S, Naldi L. Preference for telemedicine vs. in-person visit among patients with psoriasis receiving biological drugs. Dermatol Ther (Heidelb). 2021;11(4):1333–43.
Kong SS, Otalora Rojas LA, Ashour A, Robinson M, Hosterman T, Bhanusali N. Ability and willingness to utilize telemedicine among rheumatology patients—a cross-sectional survey. Clin Rheumatol. 2021;40(12):5087–93.
Jackson LE, Edgil TA, Hill B, et al. Telemedicine in rheumatology care: a systematic review. Semin Arthritis Rheum. 2022;56: 152045.
Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post–COVID-19 pandemic health care. JAMA Netw Open. 2021;4(12): e2136405.
El Komy MHM, Chiricozzi A, van de Kerkhof P, et al. Telemedicine and psoriasis: a review based on statements of the telemedicine working group of the international psoriasis council. JEADV Clin Practice. 2023;2(1):19–31.
Acknowledgements
Funding
This study and any fees related to publication were funded by Amgen, Inc.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Myriam Cordey, Ashis Das, Eunice Chang, and Caleb Paydar. The first draft of the manuscript was written by Ashis Das; all authors commented on previous versions of the final manuscript. All authors read and approved the final manuscript.
Prior Presentation
Data in this article were presented at the 31st European Academy of Dermatology and Venereology (EADV) Congress; 7–10 September 2022; Milan, Italy.
Disclosures
AD, EC, MB, and CP are employees of PHAR, who were paid by Amgen to conduct this study. PHAR also reports other financial relationships with BioMarin Pharmaceuticals, Bristol-Myers Squibb, Celgene, Dompe, Genentech, Gilead, Mirum Pharmaceuticals, Novartis, Otsuka, Prothena, Regeneron, Sanofi, and Takeda Pharmaceuticals outside the submitted work. KO and MC are employees of and own stock in Amgen.
Compliance with Ethics Guidelines
Institutional Review Board approval to conduct this study was not necessary, as this study used de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data. In order to access the claims data used in this study, a license between PHAR and the data vendor was required as noted in the current data availability statement. PHAR was only able to access the data from the data vendor after signing a licensed agreement with the data vendor.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as they were licensed by PHAR for use in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised: Error in article title corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Das, A.K., Chang, E., Paydar, C. et al. Apremilast Adherence and Persistence in Patients with Psoriasis and Psoriatic Arthritis in the Telehealth Setting Versus the In-person Setting During the COVID-19 Pandemic. Dermatol Ther (Heidelb) 13, 1973–1984 (2023). https://doi.org/10.1007/s13555-023-00967-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-00967-3