Abstract
Introduction
The association between physician-reported and patient-reported outcomes in patients with psoriasis is not adequately explored. Trends in PASI scores across body regions and the descriptive correspondence between physician-reported PASI components and patient-reported Psoriasis Symptom Diary are reported here.
Methods
PURE is a prospective observational study in adult patients from Canada and Latin America with moderate-to-severe chronic plaque psoriasis. The study enrolled 2362 adult patients treated with secukinumab versus other approved therapies (1:1 ratio). The PASI total score, PASI sub-scores for erythema, thickening, and scaling, and PASI scores for each body region were evaluated and further correlated with disease impact using the Psoriasis Symptom Diary.
Results
Secukinumab treatment showed early reduction in the PASI total score (mean ± SD) from 13.3 ± 9.02 at baseline to 2.3 ± 3.99 at 3 months; a similar trend was observed for PASI sub-scores for erythema (4.8 ± 3.21 to 0.9 ± 1.44), thickening (4.3 ± 3.00 to 0.7 ± 1.33) and scaling (4.2 ± 3.04 to 0.7 ± 1.30). The reduction in PASI total and sub-scores were sustained up to 36 months. Psoriasis Symptom Diary component scores related to redness, cracking, and scaling showed a similar reduction from baseline at 3 months that was also sustained up to 36 months. PASI regional scores for each body region showed reduction at 3 months with disease in the lower limbs being more treatment resistant. Safety profile of secukinumab was consistent with its established safety profile without any new or unexpected signals.
Conclusions
Overall, an early and sustained resolution of erythema, thickening, and scaling was observed. Improvements were evident across all body regions, with the most persistent disease seen in the lower limbs. Trends in disease severity, as assessed by physicians using PASI, broadly reflected the trend in the comparable questions of the Psoriasis Symptom Diary assessed by patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Given the impact of psoriasis on the daily activities and psychology of patients, it is important to collect patients’ insights on their disease in clinical trials to better understand whether the changes in the physical presentation of psoriasis symptoms during the treatment course had any impact on health-related quality of life (HRQoL). |
PURE is a real-world registry evaluating secukinumab and other approved therapies (biologic therapy, oral systemic therapy, and phototherapy) for the management of moderate-to-severe plaque psoriasis in Canada and Latin America. |
In this interim analysis, the effectiveness of secukinumab has been evaluated using Psoriasis Area and Severity Index (PASI) total scores, PASI component sub-scores (erythema, thickening, and scaling), and PASI scores for each body region, for the resolution of symptoms of moderate-to-severe plaque psoriasis up to 36 months, in patients from Canada and Latin America. |
Considering the limited evidence to complement the clinical observations with the impact of psoriasis on patients' HRQoL, we also evaluated the trends in the components of Psoriasis Symptom Diary, a patient-reported outcome tool, up to 36 months in the PURE registry in this analysis. |
What was learned from the study? |
An early and sustained improvement in disease severity was observed with secukinumab treatment as demonstrated by the 36-month results. This improvement was also reflected in different body regions (head/neck, trunk, upper limbs, and lower limbs), where the lower limbs required a relatively longer time for the reduction of disease severity than the other body regions. |
The PASI score components (erythema, thickening, and scaling) demonstrated improvements as early as 3 months and were sustained throughout the follow-up period of 36 months. |
Overall, secukinumab treatment showed a positive impact on disease activity and HRQoL as evaluated using PASI and Psoriasis Symptom Diary, respectively. |
Introduction
Psoriasis is a systemic immune-mediated, inflammatory disease involving the skin. In some patients, joint manifestations are also present and further contribute to the disease impact. A typical area affected by psoriasis is characterized by erythema, thickening, and scaling of plaques [1, 2]. Moderate-to-severe plaque psoriasis tends to be accompanied by a profound impact on patients’ health-related quality of life (HRQoL) [1]. Disease severity of psoriasis is assessed using the Psoriasis Area and Severity Index (PASI), a widely employed physician-rendered tool. PASI is a weighted, cumulative, numeric, and validated measure of psoriasis severity and the surface area affected in four constituent body regions (head/neck, trunk, upper limbs, and lower limbs) [3]. The analysis of PASI scores by body regions would allow a comprehensive evaluation of disease severity as well as treatment response, even for difficult to treat localized areas. However, very limited data is available on treatment response corresponding to changes in PASI score across body regions [4, 5]. Given the impact of psoriasis on the daily activities and well-being of patients, it is important to understand the impact of disease severity on patient’s HRQoL. The Psoriasis Symptom Diary was thus designed in accordance with the recommendations from the United States (US) Food and Drug Administration guidelines [6, 7], with the specific aim of generating patient-reported endpoints for moderate-to-severe chronic plaque psoriasis. Such patient-reported outcome (PRO) tools would also be helpful for healthcare professionals to gain an understanding of the disease severity and impact on patients. Moreover, the Psoriasis Symptom Diary is an important validated patient-rendered tool, which can be useful in situations such as the COVID-19 pandemic, when physician–patient interaction can be conducted only virtually through telephone or video conferencing.
Secukinumab is a human monoclonal antibody that selectively neutralizes interleukin-17A (IL-17A), a cornerstone cytokine involved in psoriasis pathogenesis [8,9,10,11,12]. It has shown rapid onset of action and sustained effectiveness with a favorable safety profile in the treatment of moderate-to-severe plaque psoriasis and psoriatic arthritis, in real-world registries such as CorEvitas [13] in North America, BADBIR [14] in the United Kingdom, PROSE [15] in 17 countries across Europe, and PROSPECT [16] in Germany. PURE is a real-world registry evaluating secukinumab and other approved therapies (biologic therapy, oral systemic therapy, and phototherapy) for the management of moderate-to-severe plaque psoriasis in Canada and Latin America [17].
This analysis reports the effectiveness of overall secukinumab treatment in the resolution of moderate-to-severe plaque psoriasis, as well as on the individual components of PASI scores in different body regions over 36 months. This analysis also reports trends in the individual components of the Psoriasis Symptom Diary over a period of 36 months.
Methods
Study Design
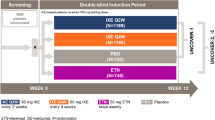
PURE is an observational, prospective, international, two-cohort registry of adult Patients with moderate-to-severe chronic plaqUe psoRiasis in Latin AmErica (Argentina, Brazil, Costa Rica, Guatemala, Mexico, Panama, and the Dominican Republic) and Canada. The registry has been ongoing since 2015, enrolling 2362 adult patients (secukinumab or other treatments in a 1:1 ratio) from 81 community- and hospital-based specialty sites. In this registry, nearly 89.0% of the patients were from Canada. The study includes a 5-year follow-up at completion, with recommended assessments at baseline, 3 and 6 months, and every 6 months thereafter. Changes in treatment can occur independently from the study at the physician’s discretion [15] (Fig. 1).
Inclusion and Exclusion Criteria
Patients (aged ≥ 18 years) who were diagnosed with moderate-to-severe chronic plaque psoriasis by a specialist were included in the study. The clinical decision to start psoriasis treatment (secukinumab, other biologic therapy, oral systemic therapy, or phototherapy) was reached previously and was independent of study enrollment. Treatments were prescribed in accordance with the product monograph per the local standard of care and regional regulatory and/or reimbursement policies. Patients who were unwilling or unable to comply with the study requirements or those involved in a clinical trial of an investigational drug, concurrently or within the last 30 days were excluded from the study.
Baseline Demographics and Disease Characteristics
Demographic characteristics of the patients, including age, sex, ethnicity, body weight, time since diagnosis, previous biologic exposure, and medical history were recorded at enrollment. The medical history was coded by MedDRA version 20.0. Disease severity was assessed using the PASI, Investigator’s Global Assessment (IGA), and body surface area (BSA) measurements, while disease impact was evaluated using the Psoriasis Symptom Diary.
Outcomes Evaluated
Psoriasis Area and Severity Index (PASI)
PASI is routinely used to evaluate psoriasis severity. It is a composite score of average erythema, thickening, and scaling of each affected area, graded as 0–4 for increasing severity, and weighted by the proportion of BSA affected [3, 18, 19]. PASI total score (0–72) is the cumulative score of the PASI regional score weighted by body region (head/neck [10%], upper limbs [20%], trunk [30%], and lower limbs [40%]) [18].
Psoriasis Symptom Diary
The Psoriasis Symptom Diary is a 16-item psoriasis-specific PRO tool that subjectively assess the severity of key signs and symptoms of plaque psoriasis (including alterations in skin color, severity of scaling, pain, cracking, burning, stinging, and itching) and how each component affects the daily activities/psychology of patients [7]. Factors evaluated for disease burden from a patient’s perspective included (i) hiding the affected skin; being bothered by (ii) scaling, (iii) pain, (iv) cracking, (v) burning, (vi) stinging, and (vii) itching; (viii) avoiding activities with other people; and (ix) embarrassment.
Data Evaluation
In this study, the mean (standard deviation [SD]) scores for the PASI (total PASI and regional PASI) and Psoriasis Symptom Diary components were evaluated at months 3, 6, 12, 18, 24, 30, and 36. Safety was assessed by the incidence of adverse events (AEs) and serious AEs (SAEs). AEs were assessed using a hierarchical list of medication exposures, (in descending order of priority: secukinumab, other biologics followed by non-biologics) and were attributed to the medication exposure closest to the top of the hierarchy. The number of patients (N) receiving secukinumab treatment who reached a specific time point at which the PASI and Psoriasis Symptom Diary scores were calculated in this analysis.
Statistical Analysis
All data analyses were performed using statistical software (SAS version 9.4, SAS Institute, Cary, NC, USA). Quantitative parameters were summarized as the number of available data, mean ± SD, median, minimum, and maximum values, and 95% confidence interval (95% CI) for the mean. Categorical variables were summarized as the number and proportion of participants belonging to each category. Testing for statistical significance was not performed. The analysis population included participants derived from study treatment cohort 1 (initiated with secukinumab) and study treatment cohort 2 (initiated with other therapies). Analysis timepoints for the outcome measures such as PASI, IGA, and Psoriasis Symptom Diary, were adjusted by the start date of secukinumab for cohort 2 participants. Total PASI score was calculated using the validated PASI scoring system. PASI regional score was calculated on a 100% scale, ranging from 0 to 72. The percentage of BSA was considered.
Ethical Consideration
All patients provided informed consent to participate in the PURE study. The PURE study design was reviewed by the ethics committees or institutional review boards and was conducted in accordance with the principles of the Declaration of Helsinki.
Results
Baseline Demographics and Disease Characteristics
As of January 24, 2020, 848 patients were initiated on secukinumab as per the physician’s decision. At baseline, the overall mean (± SD) age of patients enrolled in the registry was 49.7 (13.83) years (Table 1). At baseline, the mean (± SD) total PASI score was 13.3 (9.02; N = 840) and the mean affected BSA was 17.0% (15.75; N = 839) (Table 1). The detailed medical history of the patients enrolled in the study is presented in Table 2.
Effectiveness of Secukinumab
Total PASI Scores
The baseline total PASI score (mean [± SD; N]: 13.3 [9.02; 840]) showed an early decrease at 3 months (2.3 [3.99; 732]) and remained consistently low up to 36 months (1.6 [2.26; 73]; Fig. 2). The mean (± SD) percentage of BSA affected by psoriasis was 17.0% (15.75) at baseline, which reduced to 2.7% (6.02) at 3 months and 1.6% (3.29) at 18 months, with the reductions being sustained up to 36 months (1.2% [2.26]; Fig. 3). The baseline mean (± SD; N) PASI scores for erythema, thickening, and scaling were 4.8 (3.21; 836), 4.3 (3.00; 836), and 4.2 (3.04; 835), respectively. Early reductions from baseline in the mean (± SD; N) PASI scores for erythema, thickening, and scaling was observed at 3 months (0.9 [1.44; 730], 0.7 [1.33; 730], and 0.7 [1.30; 730], respectively), with sustained responses up to 36 months (0.5 [0.77; 72], 0.5 [0.77; 72], and 0.5 [0.76; 72], respectively; Fig. 4).
Regional PASI Scores
Disease extent was more pronounced in the upper and lower limbs than in the head/neck and trunk as evidenced by higher PASI regional scores and a larger affected BSA at baseline. A faster reduction in disease activity was observed in the head/neck and trunk, while a relatively slower reduction in disease activity was seen in the limbs, as evidenced by the affected BSA, especially in the lower limbs, at 18, 24, and 36 months (Fig. 5). All body regions demonstrated an improvement in the PASI regional score as early as 3 months, which was sustained up to 18 and 36 months (Fig. 5). The improvement in the PASI regional score was consistent across the erythema, thickening, and scaling subscales. The proportion of patients with very severe erythema, thickening, and scaling reached 0% at 36 months, except for scaling in the lower limbs, which was 1.4% (Table 3). The proportion of patients with severity rated as “none” was consistently higher at 36 months than at baseline for all body regions (Table 3).
Total IGA Scores
A higher proportion of patients achieved clear/almost clear skin at 3 months (66.6%; N = 734), which was sustained at 18 months (65.4%; N = 329), 24 months (66.0%; N = 235), and 36 months (61.4%; N = 75) than at baseline (1.8%; N = 841). Hence, the proportion of patients reporting clear/almost clear skin increased at 3 months and was sustained up to 36 months (Fig. 6).
Psoriasis Symptom Diary Scores
Patient-reported mean scores for the Psoriasis Symptom Diary components for disease severity showed an early reduction from baseline scores, as early as at 3 months, in noticeable skin color, severity of scaling, pain, cracking, burning, stinging, and itching with secukinumab treatment (Fig. 7a), which were sustained up to 36 months (Fig. 7a). A similar trend in the Psoriasis Symptom Diary components for disease burden were also observed; an early reduction, as early as 3 months, from baseline scores, which was sustained up to 36 months (Fig. 7b).
Long-Term Safety of Secukinumab
Of the 848 patients exposed to secukinumab, 605 (71.3%) reported an AE. Infections and infestations (34.8%) were the most commonly affected system organ class AEs, followed by musculoskeletal and connective tissue disorders (15.1%), general disorders and administration-site conditions (12.9%), and gastrointestinal disorders (12.1%; Table 4). Twelve (1.4%) patients had injection site reaction-related AEs. AEs leading to treatment discontinuation occurred in 120 (14.2%) patients. SAEs were reported in 67 (7.9%) patients, of which 48 (5.7%) patients had SAEs that led to hospitalization or prolonged hospitalization and 9 (1.1%) patients discontinued treatment due to SAEs. Deaths were reported in four patients (bone marrow cancer [n = 1], cardiac arrest [n = 1], subarachnoid hemorrhage [n = 1], and mesenteric ischemia [n = 1]), which were judged not being related to study treatment by the investigator. No new safety signals were reported during the 36-month observation period.
Discussion
Secukinumab has shown consistent efficacy and safety in clinical trials and real-world studies [9, 14, 15]. Here, we have reported its effectiveness as assessed objectively by a treating physician with the aid of routinely used psoriasis assessment tools as well as subjectively through PROs in patients with moderate-to-severe plaque psoriasis.
In this PURE registry analysis, patients treated with secukinumab experienced early benefits, as early as 3 months, which were sustained up to 36 months. These trends were observed for both total and regional PASI scores. The mean PASI regional scores showed an early improvement at 3 months from baseline across the body regions following secukinumab treatment that was sustained up to 36 months. A similar trend in early and sustained benefits was observed even when the total PASI scores were qualitatively categorized into scores for erythema, thickening, and scaling, confirming the effectiveness of secukinumab in reducing the overall disease severity as well as disease severity across body regions and component symptoms.
The severity and incidence of psoriasis across body regions have a profound negative impact on patients. Facial and scalp psoriasis is known to have a greater impact on patient’s HRQoL because of their high visibility [20, 21]. The response to psoriasis treatment varies according to its incidence in different body regions [20, 22]. In this PURE registry analysis, a rapid reduction in disease activity was seen in the head/neck and trunk, unlike in the limbs, which were more affected at baseline and needed a relatively longer time for reduction in disease activity. These findings are consistent with the post hoc results from the pooled analysis of two phase 3 clinical trials (CLEAR and CLARITY), where the time to achieve complete skin clearance was shorter for the head/neck (mean PASI score at week 52: 1.0; week 16: 1.0; baseline: 17.1) and trunk (mean PASI score at week 52: 0.8; week 16: 0.9; baseline: 19.5) than for the upper limbs (mean PASI score at week 52: 1.6; week 16: 1.4; baseline: 19.9) and lower limbs (mean PASI score at week 52: 2.0; week 16: 2.0; baseline: 24.0), indicating that the limbs were the most difficult-to-treat regions [23]. This trend of faster reduction in disease activity for the head/neck and trunk versus limbs is also observed with other IL-17A inhibitors and tumor necrosis factor-alpha inhibitors [5, 24].
In this PURE registry analysis, the benefits across body regions were also reflected by the reduced disease severity across all PASI components. The early decrease in PASI total and component scores was supported by a higher proportion of patients achieving clear or almost clear skin, as assessed using the IGA, from baseline to 3 months. Hence, across different measures of physician-reported scores, secukinumab treatment showed a reduction in disease severity.
There is limited evidence that complements the clinical observations with PROs in patients with moderate-to-severe plaque psoriasis. In this analysis, patient perspectives based on their responses to key questions related to the noticeable color of skin, cracking, and scaling (components of the Psoriasis Symptom Diary) were descriptively correlated with erythema, thickening, and scaling (components of PASI, physicians’ perspectives) respectively. A reduced negative impact of moderate-to-severe psoriasis symptoms was observed on patient’s HRQoL, as reflected by the scores obtained from the Psoriasis Symptom Diary questionnaire. This study provides a qualitative demonstration of the trends in disease severity with secukinumab treatment, which are reflected in patient responses and independently provides complementary insights using physician- and patient-reported outcomes. In the previously published reports, secukinumab-treated patients from two pivotal phase 3 clinical trials (ERASURE and FIXTURE), who had completed the Psoriasis Symptom Diary at baseline and week 12, reported rapid improvement in three key patient-reported symptoms [25, 26]. The long-term safety profile of secukinumab as observed in this analysis was consistent with its established safety profile; no new or unexpected signals were reported.
This PURE registry analysis provides insights into the real-world effectiveness of secukinumab, from both physician and patient perspectives; however, as with other observational studies, there are certain limitations. Data must be interpreted with caution, as the analysis was descriptive in nature and the number of patients who reached the 36-month follow-up visit was small. It is noteworthy that the number of patients at any specific time point represents those who reached a milestone during their follow-up and does not represent a linear loss to follow-up.
Conclusions
The 36-month results from the PURE registry showed an early and sustained improvement in disease severity following secukinumab treatment. The effectiveness trend was observed in all body regions, albeit with important differences in the pattern of effectiveness in the lower limbs. Patient perspectives as observed in the outcomes from Psoriasis Symptom Diary demonstrated a reduced impact of disease severity and improved HRQoL, which was consistent with physician perspectives in patients with moderate-to-severe plaque psoriasis in Canada and Latin America.
References
Langley RG, Krueger GG, Griffiths CE. Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005;64:18–23.
Kim WB, Jerome D, Yeung J. Diagnosis and management of psoriasis. Can Fam Physician. 2017;63:278–85.
Fink C, Alt C, Uhlmann L, Klose C, Enk A, Haenssle HA. Intra- and interobserver variability of image-based PASI assessments in 120 patients suffering from plaque-type psoriasis. J Eur Acad Dermatol Venereol. 2018;32:1314–9.
Touw CR, Hakkaart-Van Roijen L, Verboom P, Paul C, Rutten FF, et al. Quality of life and clinical outcome in psoriasis patients using intermittent cyclosporin. Br J Dermatol. 2001;144:967–72.
Armstrong AW, Villanueva Quintero DG, Echeverría CM, Gu Y, Karunaratne M, Reyes SO. Body region involvement and quality of life in psoriasis: analysis of a randomized controlled trial of Adalimumab. Am J Clin Dermatol. 2016;17:691–9.
Lebwohl M, Swensen AR, Nyirady J, Kim E, Gwaltney CJ, Strober BE. The psoriasis symptom diary: development and content validity of a novel patient-reported outcome instrument. Int J Dermatol. 2014;53:714–22.
Strober B, Zhao Y, Tran MH, Gnanasakthy A, Nyirady J, Papavassilis C, et al. Psychometric validation of the psoriasis symptom diary using phase III study data from patients with chronic plaque psoriasis. Int J Dermatol. 2016;55:e147–55.
Papp KA, Langley RG, Sigurgeirsson B, Abe M, Baker DR, Konno P, et al. Efficacy and safety of secukinumab in the treatment of moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled phase II dose-ranging study. Br J Dermatol. 2013;168:412–21.
Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis-results of two phase 3 trials. N Engl J Med. 2014;371:326–38.
Paul C, Lacour J-P, Tedremets L, Kreutzer K, Jazayeri S, Adams S, et al. Efficacy, safety and usability of secukinumab administration by autoinjector/pen in psoriasis: a randomized, controlled trial (JUNCTURE). J Eur Acad Dermatol Venereol. 2015;29:1082–90.
Armstrong AW, Vender R, Kircik L. Secukinumab in the treatment of palmoplantar, nail, scalp, and pustular psoriasis. J Clin Aesthet Dermatol. 2016;9:S12–6.
McInnes IB, Mease PJ, Kirkham B, Kavanaugh A, Ritchlin CT, Rahman P, et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386:1137–46.
Strober BE, Germino R, Guana A, Greenberg JD, Litman HJ, Guo N, et al. US real-world effectiveness of secukinumab for the treatment of psoriasis: 6-month analysis from the Corrona Psoriasis Registry. J Dermatolog Treat. 2020;31:333–41.
Yiu ZZN, Mason KJ, Hampton PJ, Reynolds NJ, Smith CH, Lunt M, et al. Drug survival of adalimumab, ustekinumab and secukinumab in patients with psoriasis: a prospective cohort study from the British Association of Dermatologists Biologics and Immunomodulators Register (BADBIR). Br J Dermatol. 2020;183:294–302.
Augustin M, Dauden E, Mrowietz U, Konstantinou MP, Gerdes S, Kingo K, et al. Secukinumab treatment leads to normalization of quality of life and disease symptoms in psoriasis patients with or without prior systemic psoriasis therapy: the PROSE study results. J Eur Acad Dermatol Venereol. 2021;35:431–40.
Thaçi D, Körber A, von Kiedrowski R, Bachhuber T, Melzer N, Kasparek T, et al. Secukinumab is effective in treatment of moderate-to-severe plaque psoriasis: real-life effectiveness and safety from the PROSPECT study. J Eur Acad Dermatol Venereol. 2020;34:310–8.
Papp KA, Gooderham M, Beecker J, Lynde CW, Delorme I, Dei-Cas I, et al. Rationale, objectives and design of PURE, a prospective registry of patients with moderate to severe chronic plaque psoriasis in Canada and Latin America. BMC Dermatol. 2019;19:9.
Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Ann Rheum Dis. 2005;64:65–73.
Fadzil MH, Ihtatho D, Affandi AM, Hussein SH. Area assessment of psoriasis lesions for PASI scoring. J Med Eng Technol. 2009;33:426–36.
van de Kerkhof PC, Murphy GM, Austad J, Ljungberg A, Cambazard F, Duvold LB. Psoriasis of the face and flexures. J Dermatolog Treat. 2007;18:351–60.
Kragballe K, Menter A, Lebwohl M, Tebbey PW, van de Kerkhof PC. Long-term management of scalp psoriasis: perspectives from the International Psoriasis Council. J Dermatolog Treat. 2013;24:188–92.
Wozel G. Psoriasis treatment in difficult locations: scalp, nails, and intertriginous areas. Clin Dermatol. 2008;26:448–59.
Alpalhão M, Duarte J, Diogo R, Vandemeulebroecke M, Ortmann CE, Kasparek T, et al. Lower limbs are the most difficult-to-treat body region of patients with psoriasis: pooled analysis of CLEAR and CLARITY studies of secukinumab versus ustekinumab by body region. BioDrugs. 2022;36:781–9.
Blauvelt A, Muram TM, See K, Mallinckrodt CH, Crowley JJ, van de Kerkhof P. Improvements in psoriasis within different body regions vary over time following treatment with ixekizumab. J Dermatolog Treat. 2018;29:220–9.
Strober B, Sigurgeirsson B, Popp G, Sinclair R, Krell J, Stonkus S, et al. Secukinumab improves patient-reported psoriasis symptoms of itching, pain, and scaling: results of two phase 3, randomized, placebo-controlled clinical trials. Int J Dermatol. 2016;55:401–7.
Strober B, Sigurgeirsson B, Popp G, Sinclair R, Krell J, Stonkus S, et al. Secukinumab provides clearer skin and better control on patient-reported psoriasis symptoms of itching, pain, and scaling than placebo and etanercept. J Psoriasis Psoriatic Arthritis. 2016;1:167–74.
Acknowledgements
The authors thank the study participants and site staff.
Funding
This study was funded by Novartis Pharmaceuticals AG and led by Novartis Pharmaceuticals Canada. The journal’s Rapid Service Fee was sponsored by Novartis Pharmaceuticals Canada.
Medical Writing, Editorial, and Other Assistance
We thank Syreon Corporation, Canada, for providing operational management/data management and statistical analysis services/other, which was paid for by Novartis Pharmaceuticals Canada. The authors thank Lipi Sarkar, Amrita Dubey, Ashwini Kumar K M, and Jitendriya Mishra (Novartis Healthcare Pvt. Ltd., Hyderabad) for providing medical writing support, which was funded by Novartis Pharmaceuticals AG, in accordance with the Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Melinda Gooderham and Kim A. Papp contributed to study concept and design. Material preparation and data collection were performed by all the authors. Data analysis was performed by Syreon Corporation, Canada. All authors provided critical feedback on the manuscript, approved the final manuscript for submission and are accountable for the accuracy and integrity of the manuscript.
Prior Presentation
This analysis was partially presented in part at the 30th European Academy of Dermatology and Venereology Virtual Congress (29 September 2021–2 October 2021).
Disclosures
Melinda Gooderham serves as a speaker, an investigator or an advisory board member for AbbVie, Amgen, Akros, Arcutis, Arena, Aslan, AnaptysBio, Aristea, Bausch, Boehringer Ingelheim, BMS, Celgene, Coherus, Dermira, Dermavant, Eli Lilly, Galderma, GSK, Incyte, Janssen, Kyowa Kirin, LEO Pharma, MedImmune, Merck, Meiji, Moonlake, Nimbus, Novartis, Pfizer, Regeneron, Sanofi Genzyme, Sun Pharmaceuticals, Takeda, and UCB. Kim A. Papp serves as a consultant for AbbVie, Akros, Amgen, Arcutis, Atellas, Avillion, Bausch Health/Valeant, Baxalta, Boehringer Ingelheim, Can-Fite Biopharma, Celgene, Coherus, Dermavant, Dermira, Dow Pharma, Eli Lilly and Company, Evelo, Galapagos, Galderma, Genentech, Incyte, Janssen, Kyowa Hakko Kirin, Leo Pharma A/S, Merck (MSD), Merck Serono, Novartis, Pfizer, PRCL Research, Regeneron, Roche, Sanofi-Aventis/Genzyme, Takeda, and UCB; received research grants from Anacor, Gilead, GSK, MedImmune, Moberg Pharma, and Sun Pharmaceuticals; is a scientific officer for Akros, Anacor, Arcutis, Dice Pharmaceuticals, and Kyowa Hakko Kirin; is a consultant for Dice Pharmaceuticals, Meiji Seika Pharma, and Mitsubishi Pharma; is a speaker, received honoraria and participated in steering committees and advisory boards for AbbVie, Amgen, Bausch Health/Valeant, Celgene, Eli Lilly and Company, Janssen, Merck (MSD), Novartis, Pfizer and Sanofi-Aventis/Genzyme. Charles Lynde serves as a speaker or consultant or advisor or investigator or received honoraria from AbbVie, Altius, Amgen, Aralez, Arcutis, Bausch Health, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Cipher, Dermavant, Devonian, Eli Lilly, Fresnius Kabi, Galderma, GSK, Innovaderm, Intega Skin, Janssen, Kyowa Kirin, La Roche Posay, LEO Pharma, L'Oreal, Medexus, MedX, Merck, Novartis, P&G, Pediapharm, Pfizer, Regeneron, Roche, Sanofi Genzyme, Sandoz, Sentrex, TEVA, Tribute, UCB, Valeant, Viatris, Volo Health. Isabelle Delorme serves as a speaker or consultant, or received honoraria from AbbVie, Bausch Health, Amgen, Eli Lilly, Novartis, and Janssen. Jennifer Beecker serves as a consultant for AbbVie, Amgen, Arcutis, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, Leo Pharma, Novartis, Sun Pharma, and UCB; is a speaker for AbbVie, Amgen, Arcutis, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, Leo Pharma, Novartis, Sun Pharma, and UCB; and received research grants from AbbVie, Amgen, Janssen, Leo Pharma, Novartis. Lorne Albrecht serves as a speaker or consultant or advisor or investigator or received honoraria/grants from AbbVie; Amgen; Arcutis; Bausch Health; Bristol-Myers-Squibb; Celgene; Eli Lilly; Galderma; Janssen; LEO Pharma; Novartis; Pfizer; Sanofi; UCB. Ignacio Dei-Cas serves as an advisor for AbbVie and Janssen; is a speaker for Novartis, AbbVie and Janssen; and received grants from Janssen. Danielle Brassard is an investigator for AbbVie, Novartis, Reistone, Bausch Health, Leo Pharma; is a speaker for Galderma, Actelion, Janssen, AbbVie, Pfizer, Novartis, Bausch Health, Sanofi, Leo pharma; serves as an advisor for Celgene, Bausch Health, Novartis, Amgen, AbbVie, Pfizer. Vimal H. Prajapati is an investigator for AbbVie, Amgen, Arcutis, Arena, Asana, Bausch Health, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Concert, Dermavant, Dermira, Eli Lilly, Galderma, Incyte, Janssen, LEO Pharma, Nimbus Lakshmi, Novartis, Pfizer, Regeneron, Reistone, Sanofi Genzyme, UCB Pharma, and Valeant; has served as a consultant, advisor and/or speaker for AbbVie, Actelion, Amgen, Aralez, Arcutis, Aspen, Bausch Health, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Cipher, Eli Lilly, Galderma, GlaxoSmithKline, Homeocan, Incyte, Janssen, LEO Pharma, L’Oreal, Medexus, Novartis, Pediapharm, Pfizer, Sanofi Genzyme, Sun Pharma, Tribute, UCB Pharma, and Valeant; received grants from AbbVie, Bausch Health, Celgene, Janssen, LEO Pharma, Novartis, and Sanofi Genzyme. Antonio Vieira is a full-time employee at Novartis Pharmaceuticals Canada Inc. and Lenka Rihakova was a full-time employee at Novartis Pharmaceuticals Canada Inc. until final draft of this manuscript.
Compliance with Ethics Guidelines
All patients provided informed consent to participate in the study. The study design was reviewed and approved by the ethics committees or institutional review boards, and the study was conducted in accordance with the principle of the Declaration of Helsinki (Table S1, see Electronic Supplementary Material).
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available. Novartis is committed to sharing with qualified external researchers access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved on the basis of scientific merit. All data provided are de-identified/anonymized to respect the privacy of patients who have participated in the trial in line with applicable laws and regulations. The data may be requested from the corresponding author of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gooderham, M., Papp, K.A., Lynde, C. et al. Sustained Effectiveness of Secukinumab Across Different Body Regions in Patients with Moderate-to-Severe Plaque Psoriasis from the PURE Registry. Dermatol Ther (Heidelb) 13, 535–553 (2023). https://doi.org/10.1007/s13555-022-00870-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00870-3