Abstract
Introduction
Atopic dermatitis (AD) is an inflammatory disease causing severe skin itching. Data on patient–physician disconnect on treatment satisfaction in patients with AD in Japan are limited. We investigated patient–physician disconnect on treatment satisfaction in AD and if it influences treatment patterns, clinical characteristics, and patient-reported outcomes (PROs).
Methods
Data were drawn from the Adelphi AD Disease Specific Programme (DSP), a real-world, point-in-time survey of physicians and patients with AD conducted in Japan from April to July 2019. Patients and physicians were grouped according to level of treatment satisfaction (“extremely satisfied” to “extremely dissatisfied”); with any level of dissatisfaction recorded as “less than satisfied.” Data were collected on treatment patterns, clinical characteristics, and PROs including the Dermatology Life Quality Index (DLQI), Patient-Oriented Eczema Measure (POEM), EQ-5D-3L questionnaire, and Work Productivity and Activity Impairment (WPAI) questionnaire.
Results
Data were provided by 184 patients with AD and 56 physicians; 72.8% of patient–physician pairs reported a fair (kappa coefficient: 0.40) level of agreement on treatment satisfaction, 51.6% of patient–physician pairs were both satisfied, and 21.2% were both less than satisfied. Satisfied physicians prescribed a mean 1.2 fewer treatments than dissatisfied physicians (p < 0.05). Cases where both physician and patient were less than satisfied or where patients were less satisfied than their physicians reported the worst PROs, DLQI (both less than satisfied: mean 10.7 versus patient less satisfied than physician: 10.6 versus overall: 7.9), POEM (19.5 versus 17.3 versus 17.0), EQ-5D-3L (0.82 versus 0.81 versus 0.87) (all, p < 0.05). Work impairment was highest when both patient and physician were less than satisfied (p < 0.05). Physicians cited treatment efficacy and patients cited efficacy and usability as main reasons for dissatisfaction.
Conclusion
Overall, 12.0% of patients were less satisfied with their AD treatment than the physician, demonstrating some of the worst PROs, suggesting unmet need that could be improved by better patient–physician communication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There are limited data on the level of patient–physician disconnect on treatment satisfaction in patients with atopic dermatitis (AD) in Japan. |
We investigated patient–physician disconnect on treatment satisfaction in AD and its influence, if any, on physician treatment patterns and patient-reported outcomes (PROs). |
What was learned from the study? |
We found that 12.0% of patients were less satisfied with treatment than their physician and had some of the worst PROs in the study sample. |
Better communication could improve patient–physician alignment on treatment satisfaction and improve PROs for those patients experiencing unmet need. |
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin condition marked by extreme pruritus (itching) and is frequently linked with atopic and nonatopic comorbidities, reflecting the systemic nature of the disease [1]. This condition causes inflammation and disruption of the skin barrier, resulting in adverse effects on patient quality of life (QoL) [2]. Patients with AD often suffer from disturbance of sleep [3] and skin pain [4] due to their condition, as well as commonly experiencing impacts on their social functioning and psychological wellbeing [2].
AD is one of the most prevalent skin conditions in Japan [5], tending to develop in childhood and often resolving itself with age. Despite this, the prevalence of the disease in adolescents (ages 13–17) ranges from 0.2% to 24.6% worldwide [6] and affects 3.3% of adults in Japan [7]. AD has been linked to work and productivity impairment, with one-third of adult patients with AD absent from work due to this condition [7]. This may result in larger-scale socioeconomic strain in countries with high prevalence of AD.
The main aim of treatment is to reduce the number of flare-ups, control flare-ups which occur, and reduce the itch and skin pain associated with AD [8]. Topical corticosteroids and topical calcineurin inhibitors are the current standard therapies recommended by the Japanese AD treatment guidelines for managing inflammation in AD, and topical moisturizers are recommended to alleviate cutaneous barrier disruption [9, 10]. For severe refractory cases, systemic treatment such as oral cyclosporin or ultraviolet irradiation is an option [11]. Dupilumab and baricitinib are approved systemic agents for the treatment of moderate-to-severe AD in Japan and have thus expanded the available treatment options [12, 13].
Patient-reported outcomes (PROs) and physician evaluation are the basis for the assessment of treatment satisfaction and disease progression in AD. It is essential that patient and physician perceptions align in terms of disease activity and treatment satisfaction to optimize the treatment plan and achieve the best possible outcome for the patient [14, 15]. Where there is agreement between patients and physicians, health conditions tend to be more stable [16].
Previous research has shown that there is a disconnect in how patients with AD perceive the severity of their symptoms when compared with their physicians, with one study reporting that almost one-third of patients rated symptom severity differently from their physician [17]. Other studies have reported gaps in the communication and understanding of disease burden between patients with AD and their physicians [18], and Okubo et al. reported a difference between patients with AD and physicians in Japan in their preference for a new treatment, with 77% of physicians and just 46% of patients saying they would opt in to new treatment [19].
There is evidence that patient–physician disconnect can affect patients’ willingness to engage with treatment, with Kamei et al. reporting that adherence to medication among patients with AD in Japan was positively correlated with their health literacy and satisfaction with communication with their physician [20]. These findings demonstrate the importance of assessing and quantifying the level of patient and physician disconnect with respect to treatment satisfaction. However, the available research on the disconnect between patients and physicians concerning success of treatment regimens and status of disease in patients with AD in Japan is limited. Therefore, the aim of this study was to investigate the patient and physician disconnect regarding AD treatment satisfaction and to evaluate whether treatment satisfaction gaps are associated with PROs, clinical characteristics, and treatment patterns, with a view to build on the sparse real-world evidence of physician and patient perception gaps in Japan.
Methodology
Study Design
Data were drawn from the Adelphi AD Disease Specific Programme (DSP), a point-in-time survey of physicians and their adult patients with AD in a real-world clinical setting conducted in Japan between April and July 2019. Data were collected through physician- and patient-completed questionnaires designed to gather information on disease impact and treatment satisfaction and included retrospective data captured from each patient’s medical record. A complete description of the survey methodology has been previously published and validated [21, 22].
Participants
To be included in the study, physicians had to be involved in AD management and see a minimum of five patients with moderate-to-severe AD monthly (including at least one patient with moderate and one patient with severe AD). The selected physicians were instructed to complete a physician survey followed by a physician-completed patient record form (PRF) for the next five consecutively consulting adult patients with AD. To meet the inclusion criteria, patients were required to be aged 15 years or older, diagnosed with AD, and either have a history of or be currently experiencing moderate or severe disease.
Physician-Recorded Data
The PRFs included questions on patient demographics: age, sex, body mass index (BMI), and work status; and clinical characteristics: disease duration, physician-reported AD severity (mild, moderate, or severe) at the time of consultation and at initiation of current treatment, and current body surface area (BSA) affected. The data captured also included all the information required to calculate a current score on the Eczema Area and Severity Index (EASI) (range 0–72, higher score indicating greater severity) for each patient, as well as current treatment and physicians’ satisfaction with treatment. The data collected on treatment patterns included the total number of treatments ever prescribed to the patient and the number of times the treatment regimen was switched by the physician.
Treatment satisfaction was assessed on a Likert scale. Physicians were asked how satisfied they were with patients’ current treatment based on current disease control; they could choose from seven options: “extremely satisfied,” “very satisfied,” “satisfied,” “neither satisfied nor dissatisfied,” “dissatisfied,” “very dissatisfied,” “extremely dissatisfied.”
Patient-Reported Data
At the time of consultation, patients for whom physicians completed a record form were invited to complete a patient self-completion (PSC) questionnaire. The PSC included questions about the symptoms that the patient experienced daily, a range of PROs, and their satisfaction with treatment, for which the patients’ responses could be matched with physician-reported treatment satisfaction.
For symptoms of AD including skin itch, sleep disturbance, skin pain, depression, and anxiety, patients were asked to report how often they experienced these symptoms (“all the time,” “regularly,” “sometimes,” “rarely”) and rate how much each symptom bothered them (“not at all,” “a little,” “moderately,” “very,” “extremely”).
Health-related quality of life was assessed using the Dermatology Life Quality Index (DLQI) questionnaire, which covers six domains: symptoms and feelings, daily activities, leisure, work and school, personal relationships, and treatment. The options for the patient’s response to how often they experience certain symptoms/ issues are “not at all,” “a little,” “a lot,” and “very much,” with corresponding scores of 1, 2, and 3; a 0 is allocated to an unanswered (“not relevant”) response. Totals range from less to more important on a scale from 0 to 30 and scores are regarded as clinically relevant if there is a 5-point change from baseline [23].
AD severity was measured with the Patient-Oriented Eczema Measure (POEM), a validated, patient-derived measure scored on a scale from 0 to 28, which assesses the patient’s experience of seven domains over the last week: itch, sleep, bleeding, weeping or oozing, cracking, flaking, and dry skin. A lower score indicates a better result in the POEM outcome measure [24].
The patient’s ability to work and perform regular activities was measured using the Work Productivity and Activity Impairment (WPAI) questionnaire. The WPAI is composed of six questions designed to determine employment status, AD-related work absences, absences for other reasons, how AD affects work productivity, hours worked, and how AD affects activities outside of work. The recall period is defined as the 7 days preceding the date on which the questionnaire was completed, excluding the day on which the questionnaire was completed. Four parameters are used to score the answers from the questionnaire: percentage of absenteeism, percentage of presenteeism, the percentage of total work impairment (derived from combining absenteeism and presenteeism), and percentage of impairment during out-of-work activities [25].
Overall QoL was assessed with the EQ-5D-3L questionnaire and analogue scale. The EQ-5D-3L is comprised of two components: a 0–100 mm visual analogue scale that rates the patient’s health and a descriptive system which is composed of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), that are ranked in three levels by the patient: “no problems,” “some problems,” and “extreme problems” [26]. The Japan-specific tariff was applied to EQ-5D-3L scores. The population norms for EQ-5D-3L in Japan in 2016 were reported as 0.957 in males and 0.933 in females aged 30–39 years [27].
Ethics
The DSP fulfills the definition of a market research survey under the European Pharmaceutical Market Research Association (EphMRA) Code of Conduct and is therefore conducted to market research, rather than clinical guidelines [28]. Market research surveys are exempt from requiring Institutional Review Board (IRB) approval; however, the Western IRB (WIRB) conducted a methodological review of the atopic dermatitis DSP and provided an exemption (institution protocol reference AG-8382).
The DSP was conducted in compliance with the Declaration of Helsinki. Freely given, specific, and informed consent was obtained from each respondent to take part in the DSP and for the processing of their personal data. All data provided by physicians and patients were anonymized.
Statistical Analysis
In analyses where we were interested in patient and physician alignment on treatment satisfaction, we combined their responses and compared groups where physicians and patients were in agreement (both satisfied and both dissatisfied) with groups where patients were either less or more satisfied with treatment than their physician.
In analyses that included the status of the patient’s AD we combined patients that physicians reported as improving and stable to form the “controlled” group and combined patients reported to be changeable, deteriorating slowly, and deteriorating rapidly to form the “uncontrolled” group.
Numerical variables were described using number (n), mean, and standard deviation (SD); categorical variables were described using n and percentages (%). Comparisons in descriptive analyses were made using T-tests and analysis of variance for numeric variables, and chi-squared tests for categorical variables. Kappa analysis was used to analyze the level of agreement between patient and physician satisfaction with treatment. Kappa statistics are measured on a scale ranging from 0.00 to 1.00, with levels of agreement categorized as follows: below 0.00 (poor), 0.00–0.20 (slight), 0.21–0.40 (fair), 0.41–0.60 (moderate), 0.61–0.80 (substantial), and 0.81–1.00 (almost perfect) [29].
In addition to the above, for analyses such as physician satisfaction with treatment, clinical characteristics and number of treatment lines, analysis groups were based on physician level of satisfaction regardless of patient satisfaction. Similarly, analyses of PROs, patient symptom burden, and patient treatment satisfaction were based on patient level of satisfaction.
Results
In total, 56 dermatologists provided data on 265 patients. Of those patients, 184 completed a PSC and were currently receiving prescribed treatment. Patients in this sample had been diagnosed for a mean of 11.6 years, were 38.5 years of age on average, and 57.1% were male.
We found that overall, a total of 72.8% of patients reported a fair level of agreement (kappa coefficient: 0.40) with their physician on assessment of treatment satisfaction, with 51.6% of these patients and physician pairs reporting they were both satisfied with treatment and 21.2% of pairs reporting they were both less than satisfied with treatment (Table 1).
Patient Demographics and Clinical Characteristics
Table 2 presents results from patient and physician pairs in four groups based on their agreement or lack of agreement on their satisfaction with treatment.
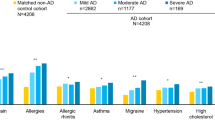
There was a trend that patients who were less satisfied than their physician had experienced AD for longer than patients in the other groups (mean 23.3 years); however, this was not statistically significant. We found differences in distribution of patients with mild, moderate, and severe AD across the satisfaction groups (p < 0.05). Where both the patient and physician were satisfied, patients were more likely to have milder (p < 0.05) and more often controlled disease (p < 0.05) than where both patient and physician were less than satisfied. There was a significant difference between groups in the proportion of patients experiencing a flare-up at the time of data collection. Overall, where patients and physicians were both dissatisfied, 35.9% of these patients were experiencing a flare-up at the time of data collection, 25.0% for patients who were more satisfied than the physician, 13.6% for patients who were less satisfied than the physician, and 9.5% when both were satisfied (p < 0.05). Overall, patients experienced a mean of 4.0 symptoms during acute episodes per year, however, this was considerably higher where both physician and patient were less than satisfied [mean (SD) per year: 6.7 (6.0)]. Similarly, EASI scores were also significantly different between groups (p < 0.05). Higher EASI scores were recorded where both patient and physician were less than satisfied (mean 14.7) and where the patient was less than satisfied but the physician was satisfied (mean 11.7).
Table 3 shows that physician satisfaction is closely associated with observable clinical characteristics and disease status. For patients where the physician was satisfied (n = 117 patients), a higher proportion of these patients had mild (p < 0.05) and controlled disease (p < 0.05), and fewer flare-ups (p < 0.05). Similarly, these patients were reported to have lower mean BSA, EASI score, and number of flare-ups over the last 12 months (all, p < 0.05).
Key reasons for physician dissatisfaction with treatment were centered around ineffectiveness, with lack of control of pruritus, lack of overall efficacy, and persistent symptoms being the most cited reasons for dissatisfaction (Fig. 1).
Treatment Patterns
Patients whose physicians were less than satisfied had received a greater number of treatments in total than patients whose physicians were satisfied with treatment (p < 0.05, Fig. 2).
Similarly, in cases where the physician was less than satisfied with treatment, patients had their treatment switched more often, with more of these patients receiving a greater number of 2–3+ treatment regimens over the course of their disease (p < 0.05, Fig. 3).
Patient-Reported Outcomes
Lower mean DLQI scores (better QoL) were reported in the groups where the patient was satisfied, regardless of physician satisfaction. Where patients were less than satisfied, the mean DLQI score was similar to cases where both the patient and their physician were less than satisfied (Fig. 4a). In the case of the POEM, which measures symptoms, the highest scores (worst QoL) were reported by the groups with any dissatisfied participant (either patient or physician) (Fig. 4b), whereas EQ-5D-3L scores followed a similar pattern to the DLQI, with the groups where the patient was satisfied recording the highest mean scores (indicating better QoL) and those where the patient was less than satisfied recording the lowest mean scores (Fig. 4c).
a Patient-reported Dermatology Life Quality Index (DLQI), b Patient-Oriented Eczema Measure (POEM) and c EQ-5D-3L by level of agreement with physician on treatment satisfaction. DLQI Dermatology Life Quality Index, POEM Patient-Oriented Eczema Measure. EQ-5D-3L scores based on Japan-specific tariff. Lower EQ-5D-3L and higher DLQI scores indicate more impaired quality of life. Higher POEM scores indicate more severe atopic dermatitis. §Analysis of variance
Overall, we found work productivity impairment was highest where both patients and physicians were less than satisfied with treatment, with these patients reporting higher activity impairment (49.5%) than when both patient and physician were satisfied (25.9%) (Table 4).
Table 5 presents the patient-reported burden as high across all patient groups, but highest where the patient was less satisfied than the physician and where both the physician and patient were less than satisfied. Sleep disruption and skin pain were worse when there was any treatment dissatisfaction irrespective of whether it was physician dissatisfaction, patient dissatisfaction, or both (p < 0.05 and p < 0.05, respectively, across the four groups).
Among the patients who reported being dissatisfied with treatment, the most common reasons for dissatisfaction differed to those reported by physicians and concerned both usability and efficacy, with 29.5% citing that it left a greasy layer on their skin and 24.6% stating that it had not improved their condition the way they had hoped and it was inconvenient/messy to use. (Fig. 5).
Discussion
Our research among Japanese dermatologists and their adult patients with AD showed a disconnect between physician and patient satisfaction with treatment for over a quarter of patients (27.2%). The resulting kappa value of 0.40 indicates only a fair level of agreement between physicians and their patients. Compared with similar research in the USA and Europe, the level of agreement was slightly lower (USA 0.53; Europe 0.54) (data on file, Adelphi Real World). Other published research on psoriasis found a similar value (kappa, 0.37) to that observed in the current study [30].
For patients who were more satisfied with their treatment than the physician, this may be because this group included a higher proportion of patients with moderate or severe disease at the time of data collection who may have lower expectations for their treatment goals than their physician. Similarly, it is possible that these patients, while remaining moderate/ severe, could still have seen some improvement from treatment, and may view any improvement as a good thing, even if it is not large, particularly if the improvement occurs in very visible areas such as the head or face, or if they have had their condition a long time and have seen no improvement until recently.
Patients who were less satisfied with their treatment than their physician tended to have worse PROs than patients who were satisfied. This suggests that the physician may be unaware of the patient’s unmet need and that physicians and patients may have different treatment goals. One possible solution to this is for physicians to use PRO instruments to help them understand patient burden and which symptoms are the most bothersome; however, one study found these were seldom used to assess the impact of AD on the patient’s daily life [17]. This is further complicated by the fact that psychocultural–social tendencies in Japanese culture may mean that patients are less forthcoming when describing their symptoms and needs to their physician [31]. Similarly, in the past physicians have not always disclosed the full extent of a patient’s condition to them [32]. Although communication has improved extensively since Asai’s paper, our results suggest that there is still a need to improve communication between patient and physician.
It should be noted that the POEM behaved slightly differently to both DLQI and EQ-5D-3L in that for the POEM, worse scores were associated with physician dissatisfaction. One possible explanation for this is that the POEM focuses more on symptoms rather than feelings and health status. Another study based on data from the USA reported that patients valued skin-related QoL outcomes when rating the severity of their AD, whereas physicians focused on sleep disturbance [17].
Physicians who were less than satisfied with treatment had prescribed a greater number of different treatments and switched patients’ treatment regimens a greater number of times, indicating that when physicians were dissatisfied, they took steps to improve the treatment for the patient, whereas when the physician was satisfied, they switched treatments less frequently and patients were prescribed fewer different treatments overall. However, despite the physician prescribing different treatments for these patients, a subset of them remained less than satisfied, indicating that there is an unmet need in these patients.
Reported reasons for dissatisfaction with treatment differed among physicians and patients. While both indicated a lack of efficacy as a key reason for dissatisfaction, more than a quarter of patients stated they did not like that the treatment left a greasy layer on their skin. This suggests some misalignment between patients and physicians on the most important attributes for successful treatment; namely, that patients were more concerned with usability than physicians.
Limitations
Several limitations should be considered in the evaluation of our findings. Patients included in this survey may not reflect the general population with AD as we were more likely to pick up patients consulting more frequently and therefore who may be more severely affected by AD than those who do not consult their physician as frequently. Similarly, while minimal inclusion criteria governed the selection of the participating physicians, participation is influenced by willingness to complete the surveys. Patients provided data on a voluntary basis, and might therefore be assumed to be more engaged; however, this would not necessarily be reflected in their level of satisfaction with treatment. As a result of the voluntary questionnaire completion and the fact that we observed high levels of agreement in the sample, some groups analyzed had small patient numbers. The point-in-time design of this study prevents any conclusions about causal relationships; however, identification of significant associations was possible. Physician-assessed severity was based on physician clinical and professional judgement. With regards to patient satisfaction expectations, these are subjective and may differ on a patient-by-patient basis; for example, it is possible that some patients adjust to a new normal, that is, a life with the condition rather than a life without it, and therefore their expectations may become lower over time. Where a patient may have once hoped for total elimination of symptoms, they may later hope for just “manageable” symptoms.
Conclusions
While the majority of physicians and patients were in agreement over treatment satisfaction, for more than a quarter of patients this was not the case. In addition, while worse outcomes were seen in those patients where both the physician and patient were less than satisfied with control on current treatment, patients who were less satisfied with their treatment than their physician tended to have worse PROs than patients who were satisfied. For these patients, better communication between physician and patient may improve this disconnect, and physicians could also use PROs to help understand patient burden. All this combined will allow physicians to recognize what is important to a patient and potentially improve clinical outcomes. These findings should be reevaluated following the introduction of new treatment options for AD since this survey was conducted.
References
Simpson EL, Paller AS, Siegfried EC, Boguniewicz M, Sher L, Gooderham MJ, Beck LA, Guttman-Yassky E, Pariser D, Blauvelt A, et al. Efficacy and safety of dupilumab in adolescents with uncontrolled moderate to severe atopic dermatitis: a phase 3 randomized clinical trial. JAMA Dermatol. 2020;156(1):44–56.
Na CH, Chung J, Simpson EL. Quality of life and disease impact of atopic dermatitis and psoriasis on children and their families. Child (Basel). 2019;6(12):133.
Barbeau M, Lalonde H. Burden of atopic dermatitis in Canada. Int J Dermatol. 2006;45(1):31–6.
Vakharia PP, Chopra R, Sacotte R, Patel KR, Singam V, Patel N, Immaneni S, White T, Kantor R, Hsu DY et al. Burden of skin pain in atopic dermatitis. Ann Allergy Asthma Immunol. 2017;119(6):548–552 e543.
Furue M, Chiba T, Takeuchi S. Current status of atopic dermatitis in Japan. Asia Pac Allergy. 2011;1(2):64–72.
Tanaka A, Morioke S, Ohya Y, Shimojo N, Takahashi M, Tanaka M, Takahagi S, Kan T, Iwamoto K, Saito R, et al. Comparison of the time course of atopic dermatitis from birth to 19 years old among generations of patients in Japan. J Dermatol. 2021;48(10):1602–6.
Muto T, Hsieh SD, Sakurai Y, Yoshinaga H, Suto H, Okumura K, Ogawa H. Prevalence of atopic dermatitis in Japanese adults. Br J Dermatol. 2003;148(1):117–21.
Ring J, Alomar A, Bieber T, Deleuran M, Fink-Wagner A, Gelmetti C, Gieler U, Lipozencic J, Luger T, Oranje AP, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) Part I. J Eur Acad Dermatol Venereol. 2012;26(8):1045–60.
Saeki H, Nakahara T, Tanaka A, Kabashima K, Sugaya M, Murota H, Ebihara T, Kataoka Y, Aihara M, Etoh T, et al. Clinical practice guidelines for the management of atopic dermatitis 2016. J Dermatol. 2016;43(10):1117–45.
Katayama I, Aihara M, Ohya Y, Saeki H, Shimojo N, Shoji S, Taniguchi M, Yamada H. Japanese guidelines for atopic dermatitis 2017. Allergol Int. 2017;66(2):230–47.
Sidbury R, Davis DM, Cohen DE, Cordoro KM, Berger TG, Bergman JN, Chamlin SL, Cooper KD, Feldman SR, Hanifin JM et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71(2):327–349
Kamei K, Saeki H, Tsuchiya T, Hirose T, Campos-Alberto E, Matsumoto F, Yoshii N, Imafuku S. Real-world treatment patterns of patients with atopic dermatitis in Japan: analysis of the JMDC claims database. J Cutane Immunology and Allergy. 2021;4(5):109–19.
Silverberg JI, Simpson EL, Wollenberg A, Bissonnette R, Kabashima K, DeLozier AM, Sun L, Cardillo T, Nunes FP, Reich K. Long-term efficacy of baricitinib in adults with moderate to severe atopic dermatitis who were treatment responders or partial responders: an extension study of 2 randomized clinical trials. JAMA Dermatol. 2021;157(6):691–9.
Furst DE, Tran M, Sullivan E, Pike J, Piercy J, Herrera V, Palmer JB. Misalignment between physicians and patient satisfaction with psoriatic arthritis disease control. Clin Rheumatol. 2017;36(9):2045–54.
Dunn A, Litrivis E. Aligning patient preferences and patient care at the end of life. J Gen Intern Med. 2011;26(7):681–2.
Kuluski K, Gill A, Naganathan G, Upshur R, Jaakkimainen RL, Wodchis WP. A qualitative descriptive study on the alignment of care goals between older persons with multi-morbidities, their family physicians and informal caregivers. BMC Fam Pract. 2013;14:133–133.
Wei W, Anderson P, Gadkari A, Blackburn S, Moon R, Piercy J, Shinde S, Gomez J, Ghorayeb E. Discordance between physician- and patient-reported disease severity in adults with atopic dermatitis: a US cross-sectional survey. Am J Clin Dermatol. 2017;18(6):825–35.
Nakahara T, Fujita H, Arima K, Taguchi Y, Motoyama S, Furue M. Perception gap between patients and physicians regarding disease burden and treatment satisfaction in atopic dermatitis: findings from an on-line survey. Jpn J Dermatol. 2018;128(13):2843–55.
Okubo Y, Ho K-A, Fifer S, Fujita H, Oki Y, Taguchi Y. Patient and physician preferences for atopic dermatitis injection treatments in Japan. J Dermatol Treat. 2020;31(8):821–30.
Kamei K, Hirose T, Yoshii N, Tanaka A. Burden of illness, medication adherence, and unmet medical needs in Japanese patients with atopic dermatitis: a retrospective analysis of a cross-sectional questionnaire survey. J Dermatol. 2021;48(10):1491–8.
Anderson P, Benford M, Harris N, Karavali M, Piercy J. Real-world physician and patient behaviour across countries: disease-specific programmes—a means to understand. Curr Med Res Opin. 2008;24(11):3063–72.
Babineaux SM, Curtis B, Holbrook T, Milligan G, Piercy J. Evidence for validity of a national physician and patient-reported, cross-sectional survey in China and UK: the Disease Specific Programme. BMJ Open. 2016;6(8): e010352.
Finlay AY, Khan GK. Dermatology life quality index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Charman CR, Venn AJ, Williams HC. The patient-oriented eczema measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140(12):1513–9.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65.
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Shiroiwa T, Fukuda T, Ikeda S, Igarashi A, Noto S, Saito S, Shimozuma K. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. 2016;25(3):707–19.
Code of Conduct [https://www.ephmra.org/standards/code-of-conduct/]
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Griffiths CEM, Augustin M, Naldi L, Romiti R, Guevara-Sangines E, Howe T, Pietri G, Gilloteau I, Richardson C, Tian H, et al. Patient-dermatologist agreement in psoriasis severity, symptoms and satisfaction: results from a real-world multinational survey. J Eur Acad Dermatol Venereol. 2018;32(9):1523–9.
Asai A, Okita T, Bito S. Discussions on present Japanese psychocultural-social tendencies as obstacles to clinical shared decision-making in Japan. Asian Bioeth Rev. 2022;14(2):133–50.
Asai A. Should physicians tell patients the truth? West J Med. 1995;163(1):36–9.
Acknowledgements
Funding
Data collection was undertaken by Adelphi Real World as part of an independent survey, entitled the Adelphi AD DSP. The analysis described here used data from the Adelphi AD DSP and was funded by Eli Lilly and Company. Eli Lilly and Company is one of multiple subscribers to the DSP. Eli Lilly and Company did not influence the original survey through either contribution to the design of questionnaires or data collection. The Rapid Service Fee was also funded by Eli Lilly and Company.
Author Contributions
PA, JP, and JA participated in the conception and design of the study; JA, EQ and VAD analyzed and interpreted the data, and CW, TA, CR, JA, JP, PA, and VD participated in manuscript writing and revision of drafts. All authors have reviewed the manuscript; given final approval of the version and agree to be accountable for all aspects of the work and will resolve any questions related to the accuracy or integrity of the work.
Disclosures
PA, JP, JA, EQ and VAD are full-time employees of Adelphi Real World and have no conflict of interest. CW and TA are full-time employees of Eli Lilly Japan K.K. CR is a full-time employee of Eli Lilly and company. CW, TA, and CR are minor shareholders of Eli Lilly and Company. TA is also a minor shareholder of Chugai Pharmaceutical Co., Ltd.
Compliance with Ethics Guidelines
The DSP methodology fits the definition of a market research survey under the EphMRA Code of Conduct [28], therefore this work received a waiver from the Western IRB (institution protocol reference AG-8382). Using a check box, patients provided informed consent for use of their anonymized and aggregated data for research and publication in scientific journals. The study was conducted in compliance with the Declaration of Helsinki.
Data Availability
All data, i.e. methodology, materials, data and data analysis, that support the findings of this survey are the intellectual property of Adelphi Real World. All requests for access should be addressed directly to Peter Anderson at peter.anderson@adelphigroup.com. Peter Anderson is an employee of Adelphi Real World.
Prior Presentation
This data has not been previously presented.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, C., Aranishi, T., Reed, C. et al. Impact of Patient and Physician Disconnect on Satisfaction with Treatment for Atopic Dermatitis in Japan. Dermatol Ther (Heidelb) 13, 505–522 (2023). https://doi.org/10.1007/s13555-022-00866-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00866-z