Abstract
Alopecia areata (AA) represents an underrecognized burden in Latin America (LA), severely impacting quality of life (QoL). This impact is exacerbated by limited access to specialized dermatologic care and therapies for AA within and among nations. Many of the unmet needs for AA globally also exist in LA. The region has geographic, ethnic, cultural, and economic conditions. With new AA medicines targeting immunologic pathways on the horizon, LA must prepare regarding regulatory issues, reimbursement, awareness, and education to give adequate and timely treatment for patients with AA. To address these issues, the Americas Health Foundation convened a panel of six dermatologists from Argentina, Brazil, Colombia, and Mexico who are experts in AA and its comorbidities for a 3-day virtual meeting to discuss AA diagnosis and treatment in LA and create a manuscript offering recommendations to address discussed barriers. This publication examines unmet AA needs in LA, treatment, and innovative therapies and recommends improving AA care. Access constraints to conventional and novel medicines hinder appropriate treatments for patients. Therapy initiation delays can affect QoL, mental health, and disease progression. People with AA face stigmas, discrimination, and misconceptions owing to a lack of disease awareness. With promising new treatments for AA on the horizon, all stakeholders must coordinate efforts to enhance LA’s AA management landscape and improve patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
AA represents an underrecognized burden in Latin America and severely impacts quality of life |
Research on AA in Latin America is lacking |
A panel of Latin American AA professionals assembled to compile this paper outlining the challenges to AA diagnosis and treatment, as well as advice for overcoming those barriers |
Delays in access to diagnosis and treatment harm patients' quality of life, mental health, and increase disease development |
Promising new targeted therapies for AA are available, and all stakeholders must work together to enhance access and availability of prompt diagnosis and treatment |
Introduction
Alopecia areata (AA) is an immune-mediated disease that occurs in genetically predisposed individuals. The immune system attacks the hair follicle (HF), resulting in variable degrees of hair loss [1,2,3,4]. It affects individuals of all ages, sexes, and ethnicities and is characterized by non-scarring alopecic areas that affect small areas or the entire scalp, hairy areas of the body, and nails [5]. Psychoneuroendocrine pathways and environmental variables like viral infections, psychosocial stress, socioeconomic deprivation, and urban life can also contribute to disease development [6].
In line with global trends, AA is not a common disease in Latin America (LA); yet it represents an often underrecognized burden with a high impact on the quality of life (QoL) of affected patients. LA is a remarkably diverse region with varying access to specialized dermatologic care and treatments for AA between and within nations. Many of the unmet needs for AA globally also exist in LA. However, the region has additional unmet needs specific to its unique geographic, ethnic, cultural, and economic circumstances. With promising new AA therapies on the horizon targeting the disease’s immunologic pathways, LA must prepare regarding regulatory issues, reimbursement, awareness, and education to provide adequate and timely treatment for patients with AA. Thus, this manuscript aims to assess the unmet needs of AA in LA, the existing state of treatment in the region, the landscape of novel therapies, and to make recommendations for the region to improve access to AA management.
Materials and Methods
Americas Health Foundation (AHF) assembled a panel of six expert dermatologists on AA from Argentina, Brazil, Colombia, and Mexico. On 6–8 April 2022, they had a 3-day virtual meeting to develop recommendations for overcoming the obstacles to AA diagnosis and treatment in LA. AHF used PubMed, MEDLINE, and EMBASE to identify the experts. Augmenting this search, AHF contacted thought leaders from LA’s medical community to confirm that the list accurately represented the needs. All the experts who attended the meeting are named authors of this manuscript.
AHF developed specific questions to address barriers limiting access to AA diagnosis and treatment in LA and assigned one to each panel member. A written response to each question was drafted by individual panel members on the basis of the literature review and personal expertise. The entire panel reviewed and edited each narrative during the 3-day conference through numerous rounds of discussion until a total agreement was reached. An AHF staff member moderated the discussion. When the panel disagreed, additional discussions were held until everyone agreed on the paper’s content. The recommendations developed were based on the evidence gathered, expert opinion, and personal experience and were approved by the entire panel. After the conference, the final manuscript was distributed by email to the panel for review and approval. The authors retain control over the paper’s content. All images were shared with the informed consent of the patients. This article is based on previously conducted studies and the panel’s personal experience and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Epidemiology
Epidemiologic data on AA, necessary to further understand disease behavior and course, are scarce and often conflicting globally. This issue is more prominent in LA, where the available data stem from very few studies [7,8,9,10,11,12]. AA prevalence is estimated at 0.2–3.8% in Mexico [10]. In Peru, AA prevalence ranges from 0.1–0.2%, accounting for 0.7–3.5% of all dermatology consults in Lima, and 2% of all new cases in dermatology clinics [12]. In Colombia, a prevalence of 0.05% was found in 2018, with a higher proportion in women [13]. Of note, the number of new cases increased during 2017–2019 but declined from 2020 to 2021, likely owing to fewer consults during the COVID-19 pandemic.
In a survey conducted by the Brazilian Society of Dermatology, AA accounted for 1.2% of all dermatologic consultations [8]. In comparison, in a major referral center in Brazil, it accounted for 16.2% of pediatric consultations and 29.4% of first-time visits [8, 10]. This contrast indirectly highlights gaps in knowledge of AA management at the primary care level, as many patients are referred for care at specialized centers.
The estimated global incidence of AA varies between 0.57% and 3.8%, with a lifetime risk of 2.8% [14,15,16]. In the United Kingdom, the average prevalence is 0.58% in adults and higher in the Asian population compared with the white population [17]. In the USA, the cumulative lifetime incidence is 2%, with 0.1–0.2% prevalence in the general population [15, 18]. The First National Health and Nutrition Examination Survey, conducted from 1971 to 1974, identified AA prevalence in the USA as 1–2 in 1000 people [18]. This study remains relevant because it is the largest, and more recent studies corroborate its results [19]. Two recent studies in Greece and Japan estimated the prevalence of AA at 1.27% and 2.45%, respectively. Cumulative AA incidence has been found to increase almost linearly with age [14, 20, 21].
In the USA, the prevalence of severe and very severe forms of AA, such as alopecia totalis (AT), alopecia ophiasis (AO), and alopecia universalis (AU) is low: 0.08%, 0.02%, and 0.03%, respectively. Some studies have found a higher prevalence of AA in Black populations than in white or Asian, both in general and severe subtypes [22, 23]. This finding may be relevant in LA owing to the substantial Black ancestry of the region’s population. However, US population-based studies that included Hispanic/Latino populations found no differences in odds ratio compared with white populations.
Burden of Disease and Comorbidities
Despite its autoimmune component and substantial impact on QoL, payers, physicians, and the general population sometimes consider AA a cosmetic concern [24]. AA is associated with a negative impact on QoL, affecting patients personally, socially, financially, and physically. Over time, cumulative disability may perpetuate poor self-esteem, social disconnection, negative coping strategies, and failure to achieve full-life potential [24]. The uncertainty, social stigma, and misconceptions surrounding AA also contribute to the burden of the disease. A Brazilian study evaluated QoL in patients with AA using the Short-Form Health Survey and found an impact on psychological, emotional, and social aspects [25]. A Colombian multicentric survey used the validated Skindex-29 evaluated QoL and included 11 patients with AA. The presence of any dermatological lesion led to some degree of alteration in QoL and high emotional impact was reported.[26].
In addition, AA is associated with various comorbidities. Among these are psychiatric conditions found in 65–74% of people with AA, the most common being depression (38%) and generalized anxiety disorder (39–62%), approximately eightfold higher than in the general population [14]. A Mexican study found QoL disturbance in 77.6% of adults, 65.9% had signs of depression or anxiety, and 12.8% were at risk of death by suicide. A total of 76.7% of children had QoL disturbance, and 6.3% showed signs of depression [27, 28]. A Chilean study found the following comorbidities in patients with AA: depression (15%), allergic rhinitis (11%), anxiety (6.5%), hypothyroidism (3.9%), and vitiligo (2.6%) [7].
Pathophysiology
AA results from complex interactions of genetic factors, immune system dysregulation, neuroendocrine pathways, and environmental factors.
Genetic Factors
Susceptibility to AA is related to multiple genes involved in immune response, including CTLA4, IL2RA, IL2, IL21, NOTCH4, MICA, EOS, HLA, IKZF4, IL17A/IL17RA, peroxiredoxin 5, syntaxin 17, HLA, and ULBP [4, 29, 30]. ULBP gene mutations are strongly associated with AA but no other autoimmune diseases; this gene encodes the activating ligands of the receptor associated with NKG2D [27, 29,30,31,32]. Specific human leukocyte antigen (HLA) alleles such as DQB1*03 and DRB1*1104 are susceptibility markers for AA development [29]. HLA-DR11 and HLA-DQ7 alleles are associated with AU or AT [33].
Loss of Immune Privilege and Autoimmunity
The HF is a site of immune privilege (IP), a state of tolerance to antigen introduction. Loss of IP in anagen is a critical step in the immunopathology of AA. IP is characterized by reduced expression of major histocompatibility complex (MHC) class I /II and β2-microglobulin; increased production of immunosuppressive molecules such as transforming growth factor-beta 2 (TGF-β2), migration inhibition factor, insulin-like growth factor 1, α-melanocyte-stimulating hormone (MSH), indoleamine 2, 3-dioxygenase and cortisol, impaired antigen-presenting cells, and an extracellular matrix barrier that prevents the entry of CD8+ lymphocytes and natural killer (NK) cells [1, 4, 29, 34]. The cause of IP loss is unknown; however, it is believed to be secondary to skin microtrauma, infectious or emotional stress, bacterial superantigens, mast cell degranulation, or increased perifollicular secretion of interferon gamma (IFN-γ) [4].
Autoimmunity associated with AA is due to the ectopic expression of MHC I molecules in the bulge during anagen, leading to the autoantigen recognition by CD8+ T cells and subsequent naive T-cell activation and differentiation into Th1, Th2, Th17, or TReg cells [4, 30, 34, 35]. Although a specific autoantigen in AA has not been identified, melanocyte-derived proteins have been proposed. Peptides derived from Gp100, and the melanoma antigen recognized by T lymphocytes stand out.
In acute phases, there is a predominantly peribulbar and a lesser intrafollicular inflammatory infiltrate in anagen HFs, composed of CD8+ (20–40%), CD4+ (60–80%) T lymphocytes, and NK cells, which impact matrix cell proliferation, causing the loss of IP and accumulation of autoreactive T cells that induce telogen prematurely [1, 4, 29, 32, 34]. Further, increased ectopic expression of MHC I and II lead to increased IFN-γ, perpetuating autoreactivity [30]. The inflammatory infiltrate decreases in chronic phases, and there is a miniaturization of the HF [4, 30]. Inflammatory infiltrate generally spares the HF stem cell reservoir, so alopecia is usually reversible [36].
AA onset is associated with the increased secretion of IFN induced by CD8+ NKG2D+ T cells (necessary and sufficient for disease development) that generate the loss of IP in the HF [4, 37, 38]. The activation of Th1 cells and secreted cytokines cause positive feedback that perpetuates the Th1 response and activates tumor necrosis factor (TNF) and IL-1α, and IL-1β that inhibit HF proliferation [30, 34]. Additionally, the loss of IP causes follicular epithelial cells to produce IL-15, which leads to positive and persistent feedback on the cytotoxic activity of NK cells and CD8+ T lymphocytes that produce IFN-γ [4, 29, 39] IL-15 activates the Janus kinase (JAK)-signal transducer and activator of transcription (STAT) signaling pathway [4, 29, 34, 39].
There is a positive correlation between IL-17 serum levels and the severity and duration of hair loss in AA [34]. Likewise, although some studies show an increase in Th2 cells that produce several interleukins, the role of humoral immunity has not been studied in AA [30, 34, 38]. What is clear is that there is dysregulation in the Th1, Th2, and Th17 pathways. The presence of proinflammatory serum markers such as IL-2 or TNF in patients with AA suggests that the disease is a systemic disorder not limited to HF [30, 34, 38].
Neuroendocrine Pathways
Approximately 23% of patients with AA have experienced an emotional event or crisis before disease onset [1, 32]. Neuropeptides produced by cutaneous nerves, such as substance P (SP), the peptide related to the calcitonin gene (PRCG), and the vasoactive intestinal peptide (VIP) modulate skin inflammation. Substance P mediated stress-induced hair growth inhibition in mice. PRCG induces mastocyte degranulation and liberation of TNF-α and IL-10, which may decrease antigenic presentation by inhibiting CD86 expression on Langerhans cells (LC) [40]. Additionally, expression of VIP receptors 1 and 2 is downregulated in the bulbs of patients with AA compared with controls. Still, their ligands are typical in nerve fibers, suggesting altered signaling mediated by VIP receptors [29, 37]. Of note, patients with AA have higher corticotropin-releasing hormone and α-MSH levels in the epidermis, HF, and sebaceous glands, indicating local hormonal–neurogenic system activated by higher cortisol levels after stressful events [30].
Environmental Factors
Several lifestyle and environmental factors are associated with a higher risk of AA. Autoimmune diseases, vaccines, and viral infections (SARS-COV-2, Epstein Barr virus, Hepatitis B and C viruses) have been identified as AA triggers in genetically predisposed individuals [41]. Additionally, smoking, alcohol consumption, sleep disturbances, obesity, and medications, including some biologics, immune checkpoint inhibitor anti-PDL1, anticonvulsants, and abacavir, among others, have also been associated with triggering AA [1].
Diagnosis
AA diagnosis is primarily based on clinical history and physical examination [35]. The most common AA presentation consists of one or several auto-resolutive alopecic areas with normal or slightly erythematous skin, follicular openings, and without scarring [29]. However, multiple coalescent areas are present in some cases and may progress to diffuse scalp or body involvement. The scalp is involved in almost all AA cases, most commonly affecting the occipital area [42]. Clinical forms of AA are described in Box 3. Nail involvement can occur in 10.5–38% of cases, with a spectrum of findings from subtle nail plate pitting to total nail dystrophy [43,44,45]. These findings are more frequently associated with severe AA and are a poor prognostic factor (see images 1, 2, and 3). Dermoscopy may provide a valuable tool to rule out differential diagnosis and a minority of patients may benefit from a histopathological analysis [29, 35, 46]. An important differential diagnosis in LA is syphilis and traction alopecia because of their high prevalence [47, 48]. See Table 1.
AA severity is defined by clinical involvement and impact on QoL. Although several clinical evaluation tools exist, the Severity Alopecia Tool (SALT), a scale used to quantify AA severity based on the percentage of affected scalp, is the most frequently employed in clinical trials [49]. SALT calculates severity by dividing the scalp into four sections (back 24%, top 40%, both sides 18% each). A SALT score of ≥ 50% indicates severe AA [49, 50]. The AA investigator global assessment (AA-IGA) can provide clinically relevant evaluations of severity and treatment response. This score also defines severe AA as a percentage of hair loss ≥ 50% and considers eyebrows, eyelashes, and nails [8, 51].
Although these scales are quick and easy-to-use instruments, in this panel’s experience, AA severity is not routinely assessed by most dermatologists in clinical practice in LA. Nevertheless, their application allows an objective assessment of AA progression, determining the necessity for systemic treatment and evaluating clinical response. No published consensus exists on the optimal strategy for assessing AA’s QoL and psychosocial effects. Currently, no QoL assessment tools tailored to AA and validated for LA languages are currently available. Nonetheless, in this panel’s experience, the Dermatology Life Quality Index (DLQI) is the most used in LA.
The Brazilian AA consensus proposes evaluating severity with the following scale: mild AA: 20% or less scalp hair loss; moderate AA 21–49% scalp hair loss; and severe AA 50–100% scalp hair loss [52]. A mild or moderate severity rating increases to the next level if any of the following are present: negative impact on psychosocial functioning, noticeable involvement of eyebrows or eyelashes, inadequate response after 6 months of treatment, diffuse (multifocal) positive hair pull test consistent with rapidly progressive AA [52]. Implementing this severity scale could provide substantial benefits for treatment decisions and disease monitoring.
Prognosis and Course
The disease course of AA is unpredictable. Patients with AA maintain the possibility for hair regrowth for many years and possibly for life. However, if left untreated, AA may reduce the number and reserve of HF, rendering the condition irreversible. Approximately 5% of AA cases will develop into AT or AU [6]. The belief that these individuals will lose the ability to regrow hair likely stems from the ineffectiveness of conventional treatments [29]. Negative predictors for hair restoration are outlined in Box 4 [14, 35].
AA Treatment
Despite great improvements in understanding pathophysiology and therapy targets for AA, no treatments have been licensed by regulatory agencies in LA, and few elsewhere. Since reviews have failed to identify a therapy supported by robust evidence, treatments are based on expert opinion or consensus [2]. This might soon change, given several ongoing clinical trials evaluating different therapies, including biologics and small molecules [52, 54,55,56,57].
AA treatment is based on disease severity and extension, patient age, comorbidities, and patient expectations, among other variables. Some patients will have spontaneous hair regrowth without treatment. An international AA treatment consensus reported 68% agreement on intralesional corticoids, 43% for topical treatments (topical corticoids 63%, calcineurin inhibitors 60%, contact immunotherapy 33%), and 36% for systemic therapies [2]. However, more evaluation of the efficacy of these treatments is required to foster evidence-based treatment decisions. These decisions, including when to scale therapy up or down, should be based on disease severity and control and monitored throughout the disease course.
Explaining the nature and progression, the treatment’s efficacy, and side effects, and establishing reasonable treatment expectations with patients, is an often overlooked but crucial part of management. Moreover, it is critical to clarify that, to date, no treatment has altered the long-term disease course. Consequently, the need for maintenance treatment remains to be determined. AA treatments, mechanisms of action, and their availability and accessibility in LA can be found in Table 2.
New Treatment Advances
New targeted therapies are expected to provide more effective and safer options than conventional treatment, especially for severe to very severe AA.
The JAK-STAT pathway in AA involves JAK1, JAK2, JAK3, and TYK2. After JAK phosphorylation, the STATs are translocated to the nucleus, where they bind DNA and trigger targeted gene transcription. This pathway is essential for maintaining innate and adaptive immunity. In AA, it has been determined that it functions as a downstream effector of the IFN-γ and IFN-γc cytokine receptors, yet other mechanisms may also be involved. Therefore, JAK-STAT inhibition disrupts the positive feedback loop between the follicular cell and cytotoxic CD8+ NKG2D+ T cells. Animal studies have shown that the inhibition of the JAK-STAT pathway promotes hair growth by stimulating HF stem cells and an anti-quiescence signal during telogen, hence expediting reentry into anagen. JAK inhibitors also prevent the development of inflammatory Th17 cells and Th1 and Th2 differentiation [29].
TEC family (tyrosine kinase expressed in hepatocellular carcinoma) members ITK, RLK, and TEC have been identified as key components of T-cell-receptor signaling. TEC kinases contribute to T-cell-receptor-driven actin reorganization and cell polarization, which are required for productive T-cell activation. They are important mediators of pathways that control the differentiation of CD4+ T-helper cells [69, 70]. Additionally, TEC is expressed in mast cells and regulates their activation [71].
Tofacitinib citrate was the first JAK inhibitor successfully used to treat AA [72,73,74]. Since then, other specific JAK inhibitors have been developed for AA treatment, including oral baricitinib (JAK1-2), oral ritlecitinib (JAK3/TEC), oral and topical ruxolitinib (JAK1-2), CTP-543 (JAK1-2), and oral brepocitinib (TYK2/JAK1), all of which have shown promising results [73, 75]. Other drugs being evaluated for AA are dupilumab (Anti-IL-4Rα, targeting IL4 and 13), abatacept (CTLA-4), and aprelimast [55, 56].
Access to AA Treatment in LA
Access to dermatologists is limited in LA and often entails lengthy waits. Specialists are mostly concentrated in major metropolitan regions. This impacts timely and accurate diagnosis and treatment initiation. In resource-limited settings such as LA, access to dermatologic treatment depends on medication cost, physician knowledge, cultural and socioeconomic variables, and disease awareness [76]. While most AA treatments are available throughout the region, even some conventional treatments like systemic corticosteroids are not accessible through public healthcare. So even when the drug is available, there is a lack of approvals and consequent coverage/reimbursement in many LA countries because most AA treatments are used “off label.” To access basic treatment, patients often must incur out-of-pocket expenses, an option that is not feasible for all. Because of this, patients in LA often do not have adequate responses to AA therapy because they have not had access to appropriate treatment. Sometimes, this leads to irreversible HF damage and cumulative effects on QoL.
As mentioned previously, only a small proportion of patients may develop severe to very severe AA, necessitating expensive systemic treatment [6]. However, delivering targeted treatment to the appropriate patients, particularly those with severe or refractive disease, must be a priority since it can result in significant benefits for the patient, society, and healthcare systems [77, 78]. This benefit is currently not possible in most LA countries because treatments for moderate to severe AA, such as JAK inhibitors, topical immunotherapy, and biologics, are not routinely reimbursed by public healthcare systems. Patients must either incur substantial out-of-pocket expenses or seek access through legislative intervention. For mild AA cases, topical and intralesional corticosteroids provide an adequate response. However, currently accessible therapies for moderate to severe AA, mainly systemic corticosteroids and conventional immunomodulators, do not offer a safe and efficacious long-term therapy alternative. Consequently, access to novel treatment options is required.
Conclusion
There are unmet needs in LA’s AA management continuum, including a lack of local data to understand the epidemiology, burden, and disease behavior. While AA has a low prevalence, it poses a substantial burden on QoL and can be financially straining for patients with the disease. In LA, access barriers to conventional and novel treatments hinder patients’ ability to receive opportune and appropriate treatment. These delays in treatment initiation can lead to sustained impacts on patients’ QoL, mental health, and potentially irreversible disease progression. A lack of disease awareness among the general population has resulted in stigmas, discrimination, and misconceptions surrounding patients with AA.
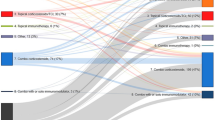
On the other hand, inadequate education on the correct AA treatment and diagnosis at the primary care level and even among specialists further contributes to suboptimal care. This insufficient knowledge may be in part due to the infrequent use of clinimetric scales in clinical practice to assess disease severity and QoL impact, as well as the lack of clinical practice guidelines for AA in most LA countries, resulting in unstandardized diagnostic criteria, workups, control evaluations, and treatment decisions. Additionally, AA must be recognized by both payers and healthcare providers as an autoimmune disease that is not limited to hair loss and requires specialized multidisciplinary care led by a dermatologist focused on disease and comorbidity control and psychosocial support. The unmet needs of AA in LA are summarized in Fig. 1.
With promising new treatment options for AA on the horizon, now is the time to act and improve the AA landscape in LA. To overcome the barriers that AA presents in the region and improve patient outcomes, concerted efforts are necessary by all stakeholders. With this in mind, the authors propose the following recommendations:
Recommendations
-
1.
Generate local data on AA epidemiology; burden of disease; genetic, demographic, and environmental factors; disease course and prognosis; treatment outcomes; pharmacoeconomic analyses (Academia, medical societies, government).
-
2.
Develop national clinical practice guidelines for AA tailored to each country’s unique context to promote standardized, evidence-based decisions that incorporate all relevant stakeholder perspectives, including medical societies, patient advocacy groups, government institutions, and payers. If this is not possible in the short to medium term, each country’s leading medical societies should reach a consensus on which guidelines physicians should adopt (Medical societies, academy, ministries of health).
-
3.
Increase access to AA treatment, both conventional and novel, in both public and private healthcare systems by:
-
a.
Governments, medical societies, and patient organizations: breach inequity gaps in access to specialized care by developing and strengthening collaborative networks within and among LA countries.
-
b.
Regulatory agencies: improve local approval times for treatments once they are approved by international agencies such as the Food and Drug Administration or European Medicines Agency.
-
c.
The pharmaceutical industry: seek regulatory approval for AA treatments, even in “small” markets in benefit of the patient.
-
d.
Government and payers: ensure widespread coverage and reimbursement of basic and advanced AA treatments and explore the potential cost–benefit of providing targeted therapy to patients with moderate–severe AA.
-
a.
-
4.
Increase physician education about AA:
-
a.
Primary care level: basic diagnosis and treatment, appropriate referral situations.
-
b.
Dermatologist: pathophysiology, triggers, comorbidities, signs of activity, prognosis factors, and novel treatments, including biologics, JAK inhibitors, and other small molecules.
-
c.
Other specialists: because AA is often associated with comorbidities, specialists such as endocrinologists, psychologists and psychiatrists, infectious disease specialists, rheumatologists, pediatricians, and internal medicine physicians should be aware of the disease. (Medical societies, healthcare institutions, medical community)
-
a.
-
5.
Ensure comprehensive care with a multidisciplinary approach for AA management, including psychosocial support, individualized strategies for comorbidity management, and using clinimetric scales for disease severity and QoL evaluation for all AA patients at diagnosis and continuously throughout the disease course. (Dermatologists or treating physician)
-
6.
Physicians must provide patients and their families with education on the unpredictable course of AA, its relationship with psychosocial factors, effectiveness, and adverse effects of treatments, and establish reasonable outcome expectations. Creating dedicated AA patient organizations or support groups could improve the emotional burden of the disease [77, 78]. (Dermatologists)
-
7.
Create public awareness campaigns about AA for the public to dispel misconceptions, stigmas, and discrimination surrounding the disease and educate policymakers on the importance of timely and adequate treatment. (Medical societies, industry, governments, PO)
References
Minokawa Y, Sawada Y, Nakamura M. Lifestyle factors involved in the pathogenesis of alopecia areata. Int J Mol Sci. 2022;23(3):1.
Meah N, Wall D, York K, Bhoyrul B, Bokhari L, Sigall DA, et al. The alopecia areata consensus of experts (ACE) study: results of an international expert opinion on treatments for alopecia areata. J Am Acad Dermatol. 2020;83(1):123–30.
Islam N, Leung PS, Huntley AC, Gershwin ME. The autoimmune basis of alopecia areata: a comprehensive review. Autoimmun Rev. 2015;14(2):81–9.
Anzai A, Wang EHC, Lee EY, Aoki V, Christiano AM. Pathomechanisms of immune-mediated alopecia. Int Immunol. 2019;31(7):439–47.
Hordinsky MK. Overview of alopecia areata. J Investig Dermatol Symp Proc. 2013;16(1):S13–5.
Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton LJ 3rd. Incidence of alopecia areata in Olmsted County, Minnesota, 1975 through 1989. Mayo Clin Proc. 1995;70(7):628–33.
Zegpi MS, del Reeves P, Cardoso IK, Gustavo CD. Study of patients diagnosed with alopecia areata, and treated at the Dermatological Service of the Diagnostic Center at Universidad Catolica de Chile. Rev Chil Dermatol. 2006;22(1):6.
Ramos PM, Anzai A, Duque-Estrada B, Melo DF, Sternberg F, Santos LDN, et al. Consensus on the treatment of alopecia areata—Brazilian Society of Dermatology. An Bras Dermatol. 2020;95(Suppl 1):39–52.
Olguin-Garcia M, Del Campo M, Guez-Acar M, Peralta-Pedrero M. Factores psicoligicos asociados con la alopecia areata. Dermatol Rev Mex. 2013;57:6.
Miotto IZ, Bessa VR, Vasconcelos LBA, Samorano LP, Rivitti-Machado MC, Oliveira ZNP. Pediatric dermatoses pattern at a Brazilian reference center. J Pediatr (Rio J). 2021;97(2):211–8.
Bertanha F, Nelumba EJ, Freiberg AK, Samorano LP, Festa CN. Profile of patients admitted to a triage dermatology clinic at a tertiary hospital in São Paulo. Brazil An Bras Dermatol. 2016;91(3):318–25.
Naccha E. Alopecia areata e incremento de la prevalencia de desórdenes psiquiátricos. Int Dermatol. 1995;33:1.
Fernández-Ávila DG, Anzóla LPC, Cardona LPG. Prevalencia de las enfermedades dermatológicas en Colombia: alopecia areata una aproximación con los datos del ministerio de salud y protección social. Poster presented at XXXII Congreso Colombiano de Dermatologia. 2018.
Villasante Fricke AC, Miteva M. Epidemiology and burden of alopecia areata: a systematic review. Clin Cosmet Investig Dermatol. 2015;8:397–403.
Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990–2009. J Invest Dermatol. 2014;134(4):1141–2.
Lee HH, Gwillim E, Patel KR, Hua T, Rastogi S, Ibler E, et al. Epidemiology of alopecia areata, ophiasis, totalis, and universalis: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82(3):675–82.
Harries M, Macbeth AE, Holmes S, Chiu WS, Gallardo WR, Nijher M, et al. The epidemiology of alopecia areata: a population-based cohort study in UK primary care. Br J Dermatol. 2022;186(2):257–65.
Safavi K. Prevalence of alopecia areata in the First National Health and Nutrition Examination Survey. Arch Dermatol. 1992;128(5):702.
Benigno M, Anastassopoulos KP, Mostaghimi A, Udall M, Daniel SR, Cappelleri JC, et al. A large cross-sectional survey study of the prevalence of alopecia areata in the United States. Clin Cosmet Investig Dermatol. 2020;13:259–66.
Kyriakis KP, Paltatzidou K, Kosma E, Sofouri E, Tadros A, Rachioti E. Alopecia areata prevalence by gender and age. J Eur Acad Dermatol Venereol. 2009;23(5):572–3.
Furue M, Yamazaki S, Jimbow K, Tsuchida T, Amagai M, Tanaka T, et al. Prevalence of dermatological disorders in Japan: a nationwide, cross-sectional, seasonal, multicenter, hospital-based study. J Dermatol. 2011;38(4):310–20.
Thompson JM, Park MK, Qureshi AA, Cho E. Race and alopecia areata amongst US women. J Investig Dermatol Symp Proc. 2018;19(1):S47-s50.
Lee H, Jung SJ, Patel AB, Thompson JM, Qureshi A, Cho E. Racial characteristics of alopecia areata in the United States. J Am Acad Dermatol. 2020;83(4):1064–70.
Burns LJ, Mesinkovska N, Kranz D, Ellison A, Senna MM. Cumulative life course impairment of alopecia areata. Int J Trichology. 2020;12(5):197–204.
de Hollanda TR, Sodré CT, Brasil MA, Ramos ESM. Quality of life in alopecia areata: a case-control study. Int J Trichology. 2014;6(1):8–12.
Sanclemente G, Burgos C, Nova J, Hernández F, González C, Reyes MI, et al. The impact of skin diseases on quality of life: a multicenter study. Actas Dermo-Sifiliográficas (English Edition). 2017;108(3):244–52.
Vélez-Muñiz RDC, Peralta-Pedrero ML, Jurado-Santa Cruz F, Morales-Sánchez MA. Psychological profile and quality of life of patients with alopecia areata. Skin Appendage Disord. 2019;5(5):293–8.
Majid I, Keen A. Management of alopecia areata: an update. Br J Med Practicion. 2012;5(3).
Pratt CH, King LE Jr, Messenger AG, Christiano AM, Sundberg JP. Alopecia areata. Nat Rev Dis Primers. 2017;3:17011.
Ito T. Recent advances in the pathogenesis of autoimmune hair loss disease alopecia areata. Clin Dev Immunol. 2013;2013: 348546.
Tosti A, Bellavista S, Iorizzo M. Alopecia areata: a long term follow-up study of 191 patients. J Am Acad Dermatol. 2006;55(3):438–41.
Juárez-Rendón KJ, Rivera Sánchez G, Reyes-López M, García-Ortiz JE, Bocanegra-García V, Guardiola-Avila I, et al. Alopecia areata. Current situation and perspectives. Arch Argent Pediatr. 2017;115(6):e404–e11.
Colombe BW, Price VH, Khoury EL, Garovoy MR, Lou CD. HLA class II antigen associations help to define two types of alopecia areata. J Am Acad Dermatol. 1995;33(5 Pt 1):757–64.
Waśkiel-Burnat A, Kołodziejak M, Sikora M, Stochmal A, Rakowska A, Olszewska M, et al. Therapeutic management in paediatric alopecia areata: a systematic review. J Eur Acad Dermatol Venereol. 2021;35(6):1299–308.
Sterkens A, Lambert J, Bervoets A. Alopecia areata: a review on diagnosis, immunological etiopathogenesis and treatment options. Clin Exp Med. 2021;21(2):215–30.
Olayinka J, Richmond J. Immunopathogenesis of alopecia areata. Curr Res Immunol. 2021;2.
Zhou C, Li X, Wang C, Zhang J. Alopecia areata: an update on etiopathogenesis, diagnosis, and management. Clin Rev Allergy Immunol. 2021;61(3):403–23.
Suchonwanit P, Kositkuljorn C, Pomsoong C. Alopecia areata: an autoimmune disease of multiple players. Immunotargets Ther. 2021;10:299–312.
Olayinka JJT, Richmond JM. Immunopathogenesis of alopecia areata. Curr Res Immunol. 2021;2:4.
Echavarria C, Velasquez M. Aspectos clínicos e inmunopatogénicos de la alopecia areata. Rev Argent Dermatol [online]. 2019;100(2):9.
FIvenson D. COVID-19: association with rapidly progressive forms of alopecia areata. Int J Dermatol. 2021;60(1):127.
Okhovat JP, Marks DH, Manatis-Lornell A, Hagigeorges D, Locascio JJ, Senna MM. Association between alopecia areata, anxiety, and depression: a systematic review and meta-analysis. J Am Acad Dermatol. 2019.
Tan E, Tay YK, Goh CL, Chin GY. The pattern and profile of alopecia areata in Singapore—a study of 219 Asians. Int J Dermatol. 2002;41(11):748–53.
Sharma VK, Dawn G, Kumar B. Profile of alopecia areata in Northern India. Int J Dermatol. 1996;35(1):22–7.
Muller SA, Winkelmann RK. Alopecia areata. An Evaluation of 736 patients. Arch Dermatol. 1963;88:290–7.
Doche I, Hordinsky M. Alopecia areata. In: Doche I, Damasco P, Martins G, editors. Fundamentals of hair and scalp dermoscopy. New Delhi: Jaypee Brothers Medical Publishers; 2018.
Billero V, Miteva M. Traction alopecia: the root of the problem. Clin Cosmet Investig Dermatol. 2018;11:149–59.
Sistema Integrado de Información de la Protección Social [Internet]. SISPRO. Available from: https://www.sispro.gov.co/Pages/Home.aspx.
Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, et al. Alopecia areata investigational assessment guidelines—part II. National Alopecia Areata Foundation. J Am Acad Dermatol. 2004;51(3):440–7.
Olsen E, Hordinsky M, McDonald-Hull S, Price V, Roberts J, Shapiro J, et al. Alopecia areata investigational assessment guidelines. National Alopecia Areata Foundation. J Am Acad Dermatol. 1999;40(2 Pt 1):242–6.
Wyrwich KW, Kitchen H, Knight S, Aldhouse NVJ, Macey J, Nunes FP, et al. The Alopecia Areata Investigator Global Assessment scale: a measure for evaluating clinically meaningful success in clinical trials. Br J Dermatol. 2020;183(4):702–9.
King BA, Mesinkovska NA, Craiglow B, Kindred C, Ko J, McMichael A, et al. Development of the alopecia areata scale for clinical use: results of an academic–industry collaborative effort. J Am Acad Dermatol. 2022;86(2):359–64.
Finner AM. Alopecia areata: clinical presentation, diagnosis, and unusual cases. Dermatol Ther. 2011;24(3):348–54.
Ramírez-Marín HA, Tosti A. Evaluating the therapeutic potential of ritlecitinib for the treatment of alopecia areata. Drug Des Devel Ther. 2022;16:363–74.
Pourang A, Mesinkovska NA. New and emerging therapies for alopecia areata. Drugs. 2020;80(7):635–46.
Mikhaylov D, Glickman JW, Del Duca E, Nia J, Hashim P, Singer GK, et al. A phase 2a randomized vehicle-controlled multi-center study of the safety and efficacy of delgocitinib in subjects with moderate-to-severe alopecia areata. Arch Dermatol Res. 2022.
King B, Ohyama M, Kwon O, Zlotogorski A, Ko J, Mesinkovska NA, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386(18):1687–99.
Freire PCB, Riera R, Martimbianco ALC, Petri V, Atallah AN. Minoxidil for patchy alopecia areata: systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33(9):1792–9.
Gordon PM, Aldrige RD, McVittie E, Hunter JA. Topical diphencyprone for alopecia areata: evaluation of 48 cases after 30 months’ follow-up. Br J Dermatol. 1996;134(5):869–71.
Esen Salman K, Kıvanç Altunay İ, Salman A. The efficacy and safety of targeted narrowband UVB therapy: a retrospective cohort study. Turk J Med Sci. 2019;49(2):595–603.
Lee JH, Eun SH, Kim SH, Ju HJ, Kim GM, Bae JM. Excimer laser/light treatment of alopecia areata: a systematic review and meta-analyses. Photodermatol Photoimmunol Photomed. 2020;36(6):460–9.
Sharma VK, Gupta S. Twice weekly 5 mg dexamethasone oral pulse in the treatment of extensive alopecia areata. J Dermatol. 1999;26(9):562–5.
Hammerschmidt M, Mulinari BF. Efficacy and safety of methotrexate in alopecia areata. An Bras Dermatol. 2014;89(5):729–34.
Husein-ElAhmed H, Steinhoff M. Efficacy and predictive factors of cyclosporine A in alopecia areata: a systematic review with meta-analysis. J Dermatolog Treat. 2022;33(3):1643–51.
Farshi S, Mansouri P, Safar F, Khiabanloo SR. Could azathioprine be considered as a therapeutic alternative in the treatment of alopecia areata? A pilot study. Int J Dermatol. 2010;49(10):1188–93.
Verstovsek S, Passamonti F, Rambaldi A, Barosi G, Rosen PJ, Rumi E, et al. A phase 2 study of ruxolitinib, an oral JAK1 and JAK2 Inhibitor, in patients with advanced polycythemia vera who are refractory or intolerant to hydroxyurea. Cancer. 2014;120(4):513–20.
Guttman-Yassky E, Renert-Yuval Y, Bares J, Chima M, Hawkes JE, Gilleaudeau P, et al. Phase 2a randomized clinical trial of dupilumab (anti-IL-4Rα) for alopecia areata patients. Allergy. 2022;77(3):897–906.
Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33(5):850–6.
Schwartzberg PL, Finkelstein LD, Readinger JA. TEC-family kinases: regulators of T-helper-cell differentiation. Nat Rev Immunol. 2005;5(4):284–95.
Berg LJ, Finkelstein LD, Lucas JA, Schwartzberg PL. Tec family kinases in T lymphocyte development and function. Annu Rev Immunol. 2005;23:549–600.
Ellmeier W, Abramova A, Schebesta A. Tec family kinases: regulation of FcεRI-mediated mast-cell activation. Febs J. 2011;278(12):1990–2000.
Morales-Miranda AY, Bueno-Arias GM, Aguirre-Félix ÓG, Tovar-Franco R. Tofacitinib as a treatment of alopecia areata in adolescents. Bol Med Hosp Infant Mex. 2019;76(4):182–7.
Liu LY, Craiglow BG, Dai F, King BA. Tofacitinib for the treatment of severe alopecia areata and variants: a study of 90 patients. J Am Acad Dermatol. 2017;76(1):22–8.
Craiglow BG, King BA. Killing two birds with one stone: oral tofacitinib reverses alopecia universalis in a patient with plaque psoriasis. J Invest Dermatol. 2014;134(12):2988–90.
Guttman-Yassky E, Pavel AB, Diaz A, Zhang N, Del Duca E, Estrada Y, et al. Ritlecitinib and brepocitinib demonstrate significant improvement in scalp alopecia areata biomarkers. J Allergy Clin Immunol. 2022;149(4):1318–28.
Seth D, Cheldize K, Brown D, Freeman EF. Global burden of skin disease: inequities and innovations. Curr Dermatol Rep. 2017;6(3):204–10.
National Alopecia Areata Foundation (Available from: https://www.naaf.org/).
Alopecia UK (cited 2022 August 28). Available from: https://www.alopecia.org.uk/.
Acknowledgements
Funding
The organization, design, and implementation of the consensus conference were carried out by the AHF, a 501(c)3 nonprofit organization dedicated to improving healthcare throughout the Latin American Region and all efforts relating to the conference and publication, including the Rapid Service Fee were funded by an unrestricted grant from Pfizer Foundation.
Editing Assistance
The authors would like to thank Thais Vidal, BA, for their assistance in language-editing the manuscript.
Author Contributions
MMVL. Writing-original draft, investigation, formal analysis, validation. NH. Writing-original draft, investigation, formal analysis, validation. AMJ. Writing-review and editing, project administration. ALC. Writing-original draft, investigation, formal analysis, validation. PCL. Writing-original draft, investigation, formal analysis, validation. MMSdO. Writing-original draft, investigation, formal analysis, validation. MMTB. Writing-original draft, investigation, formal analysis, validation. MRR. Writing-review and editing, visualization, conceptualization, methodology, project administration. MCR. Writing-original draft, Investigation, formal analysis, validation.
Disclosures
Margarita M. Velásquez-Lopera, Natalia Hernández, Angela Marie Jansen, Angela Londoño García, Paula Carolina Luna, María del Mar Saez-de-Ocariz, María Margarita Tamayo-Buendía, Mariana Rico Restrepo, and Maria Cecilia Riviti declare that they have no competing interests.
Compliance with Ethics Guidelines
All images were shared with the informed consent of the patients. This article is based on previously conducted studies and the panel’s personal experience and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Velásquez-Lopera, M.M., Hernández, N., Jansen, A.M. et al. Alopecia Areata in Latin America: Where are We and Where are We Going?. Dermatol Ther (Heidelb) 13, 95–114 (2023). https://doi.org/10.1007/s13555-022-00845-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00845-4




