Abstract
For patients with metastatic melanoma, immunotherapy agents represent a promising treatment option, and researchers are actively seeking to identify factors that may predict a favorable response in patients. Recent studies have elucidated possible associations between the gut microbiome and the effects of immunotherapy, where variations in the gut microbiome may influence treatment response and frequency of adverse effects. In this clinical review, we describe the current literature related to the gut microbiome in the setting of immunotherapy, and we provide an overview of interventions under investigation that may modulate the gut microbiome. These interventions include fecal microbiota transplantation, probiotics, and dietary modifications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
For patients with metastatic melanoma, current standard treatment options include the following immunotherapy classes: anti-programmed cell death 1 (anti-PD-1), anti-programmed death-ligand 1 (anti-PD-L1) [5], and anti-cytotoxic T-lymphocyte-associated antigen 4 (anti-CTLA-4). |
Recent studies have shown increasing evidence that the gut microbiome may influence the anti-tumor effects of immunotherapy and that modulation of the gut microbiome may enhance or impair patient response to immunotherapy. |
There has been ongoing research evaluating interventions (e.g., fecal microbiota transplantation, probiotics, dietary modifications) to alter the gut microbiota in order to optimize immunotherapy response rates in patients. |
Introduction
The human microbiome plays a critical role in human health and disease and comprises the collection of microorganisms that inhabit the surface of the body's epithelium [1]. The gut microbiome, the largest microbiome in the human body, contains approximately 3 × 1013 bacteria [4]. Variations in the composition of the gut microbiome can influence physiologic functions such as metabolism, inflammation, and innate and acquired immunity [1]. Collectively, the human microbiome may also influence cancer initiation, progression, and treatment response including response to immunotherapy [2].
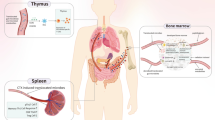
Immunotherapy agents, also referred to as immune checkpoint inhibitors (ICIs) or immune checkpoint blockade therapeutics (ICBTs), treat cancer by reducing inhibition of the body’s immune system. By “lightening up on the brakes,” these agents enable the immune system to better recognize and destroy cancer cells. Immunotherapy has revolutionized the treatment of melanoma and other cancers such as lung cancer, ovarian cancer, renal cancer carcinoma, and Hodgkin’s lymphoma [3, 4]. For patients with metastatic melanoma, promising new agents include monoclonal antibodies against anti-programmed cell death 1 (anti-PD-1) [5], anti-programmed death-ligand 1 (anti-PD-L1) [5], and anti-cytotoxic T-lymphocyte-associated antigen 4 (anti-CTLA-4) [6] (Table 1).
In metastatic melanoma patients, response to immunotherapy has been found to be associated with specific gut flora: patients who respond well to immunotherapy demonstrate different gut flora compared with those who respond poorly [7,8,9,10,11]. In preclinical mouse models of metastatic melanoma, altering the gut microflora has been shown to enhance response to immunotherapy [7,8,9, 12, 13]. The effects of gut microbiome modulation on immunotherapy response have also been demonstrated in human cohort studies [14]. Multiple lines of research are currently exploring how the gut microbiome can be altered to optimize immunotherapy efficacy for various cancers including melanoma.
This clinical review addresses the gut microbiome as it relates to immunotherapy response in melanoma patients and immune-mediated adverse events from immunotherapy. We also provide an overview of interventions that may modulate the gut microbiome and thus affect immunotherapy response. In the current literature, these interventions include fecal microbiota transplantation, antibiotics, probiotics, prebiotics, and dietary modifications. This review is based on published literature and does not contain any new studies with human participants or animals performed by any of the authors.
The Gut Microbiome and Immunotherapy Response in Melanoma
An association between the gut microbiome and immunotherapy responsiveness was first demonstrated in preclinical animal studies. In mouse models, the efficacy of anti-CTLA-4 therapy was found to be directly influenced by gut microbial composition [12]. The presence of certain commensal gut microbes such as Bacteroides fragilis, Bacteroides thetaiotaomicron, Burkholderiales, and Bifidobacterium was shown to be associated with enhanced tumor control [12, 13]. Interestingly, oral administration of Bifidobacterium alone achieved a similar degree of tumor control compared with anti-PD-1 therapy, and combining the two approaches achieved a synergistic anti-tumor effect [13].
Studies in human cohorts have also found that responders (Rs) and non-responders (NRs) to immunotherapy differed in terms of their gut microbiome. For anti-PD-1 therapy, fecal samples from Rs were found to exhibit greater diversity of gut bacteria and higher abundance of certain gut microbes such as Clostridiales, Ruminococcaceae, and Faecalibacterium compared with NRs [7]. Other gut microbes such as Bifidobacterium longum, Collinsella aerofaciens, Enterococcus faecium, and Dorea formicogenerans were also found in greater abundance in Rs compared to NRs [11]. In contrast to Rs, NRs to anti-PD-1 therapy had lower diversity of gut bacteria and higher abundance of the phylum Bacteroidales [7].
For anti-CTLA-4 therapy, the presence of the phylum Firmicutes in the gut microbiota was associated with enhanced immunotherapy response [10]. A clinical study exploring anti-CTLA-4 and anti-PD-1 combination therapy found that the fecal samples of Rs were enriched with specific gut microbes such as Faecalibacterium prausnitznii, Bacteroides thetaiotamicron, and Holdemania filiformis [11]. These above findings may be due to an enhanced immune response against cancer cells, mediated by increased antigen presentation and improved T-cell function [7].
Overall, these studies have identified numerous taxa of gut microbes that may modulate immunotherapy response. The levels of these gut microbes may be therapeutically manipulated to enhance tumor control in melanoma patients receiving immunotherapy. Further studies are needed to understand the mechanisms by which specific gut microbes influence immunotherapy response in melanoma.
Immune-Related Adverse Effects from Immunotherapy
Gut microbiota may modulate not only the effects of immunotherapy on tumor burden but also its immune-related adverse effects (irAEs). These adverse effects from immunotherapy are believed to arise as a result of the loss of T-cell inhibition and reduced self-tolerance and may affect the gut, skin, liver, and the endocrine system [15]. One of the most common adverse effects reported following immunotherapy administration is immunotherapy-induced colitis, which presents as diarrhea and may prompt treatment cessation [15, 16]. Of note, toxicity symptoms are more frequent for patients receiving single-agent anti-CTLA-4 compared to single-agent anti-PD-1 or anti-PD-L1 therapy [9, 17]. Patients receiving combination anti-CTLA-4 with either anti-PD-1 or anti-PD-L1 therapy experience more frequent and more severe irAEs compared to patients receiving monotherapy approaches [18, 19].
Prospective clinical studies in metastatic melanoma patients receiving anti-CTLA-4 therapy have examined the association between treatment-induced colitis and baseline gut microbial composition [10, 20]. Investigators found that overabundance of the Bacteroidetes phylum, especially the Bacteroides genus, at baseline was associated with a reduced risk for colitis [10, 20]. However, these patients were also associated with having a poor response to anti-CTLA-4 therapy [10]. Meanwhile, patients with higher levels of the Faecalibacterium genus (and other genera in the Firmicutes phylum) experienced more frequent colitis symptoms but demonstrated an enhanced response to anti-CTLA-4 therapy [10].
These studies suggest that baseline microbial composition may be an important factor for consideration when predicting patient risks for irAEs. Additionally, there appears to be a correlation between irAEs and response to immunotherapy that may be mediated by the gut microbiome. Further studies are needed to understand the role of different gut microbes in irAEs and their predictive value for imminent gastrointestinal symptoms.
Antibiotic Use and the Gut Microbiome
Since the gut microbiome may affect immunotherapy response in patients, iatrogenic disruptions of gut bacteria including antibiotic use may positively or negatively affect the efficacy of immunotherapy. Broad-spectrum antibiotics may disrupt gut bacteria, decrease levels of proinflammatory cytokines (e.g., IL-6, IFN-γ), and reduce immunotherapy response [16]. Preclinical studies in mouse models have shown that the use of antibiotics can reduce the effectiveness of anti-PD-1 and anti-CTLA-4 therapies [9, 12, 21].
In an experimental study, investigators administered broad-spectrum antibiotics to sarcoma mouse models [12]. The tumors continued to progress in the antibiotic-treated mice, but in the control mice with intact gut flora, the tumors were stable [12]. Similarly, in clinical studies, patients who took antibiotics before or shortly after beginning immunotherapy experienced considerably lower survival [9]. These findings suggest that the gut microbiota may be required for the anti-tumor effects of anti-CTLA-4 therapy [12]. A possible direct correlation between antibiotic use and poor immunotherapy response warrants further exploration. Future observational studies may perform longitudinal microbiome analyses in patients receiving immunotherapy before and after antibiotic use [16].
Interventions for Modulating the Gut Microbiome to Enhance Immunotherapy Response
In modulating the gut microbiome, specific interventions may enhance immunotherapy response in metastatic melanoma patients. Current interventions under investigation include fecal microbiota transplantation (FMT), probiotics, prebiotics, and dietary modifications.
Fecal Microbiota Transplantation (FMT)
In FMT, fecal matter is transferred from a donor to a host with therapeutic intent. While the fecal samples predominantly consist of commensal gut bacteria, viruses and fungi can also be administered along with bacteria, though sample reproducibility is challenging [22]. FMT is commonly used to treat recurrent Clostridium difficile infection. Response rates to FMT for C. difficile colitis are thought to differ according to administration routes: administration via colonoscopy or enema demonstrates the highest response rates, followed by administration via nasogastric tube or oral capsules [23]. FMT has also been utilized in bone marrow transplantation (BMT) patients requiring pre-procedure antibiotics. A trial among transplant patients showed that autologous FMT can reconstitute the gut microbiome in patients following BMT [24].
Clinical insights from the use of FMT for C. difficile colitis and BMT may support the use of FMT in the setting of immunotherapy. Currently, experimental studies are seeking to utilize FMT in order to modulate the gut microbiome and improve immunotherapy outcomes [25]. In mice receiving FMT from humans, FMT was found to modulate both the gut microbiome and the tumor microbiome, affecting tumor growth and tumor immune infiltrates [26]. In multiple studies on anti-PD-1 efficacy, mice receiving FMT from Rs to anti-PD-1 therapy showed significantly reduced tumor growth and enhanced treatment efficacy compared to those receiving FMT from NRs [7,8,9]. In a recent clinical trial among patients with metastatic melanoma receiving anti-PD-1 therapy, 3 out of 10 NRs became Rs after FMT from Rs, and no adverse effects were noted [14]. These findings support the possibility that resistance to immunotherapy may be overcome by modulating the gut microbiota [14].
Based on results from various FMT trials, important factors to consider when designing FMT interventions include patient selection, FMT timing/modality, and post-FMT follow-up [17]. There may be additional factors inherent to the donor that may affect FMT efficacy, such as the composition and functional aspects of the transplanted microbiota [22]. The variations in donor FMT specimens may limit the reproducibility and thus scalability of the intervention. Antibiotic ablation prior to FMT may be an important step to allow engraftment of the donor microbiota. Medication and antibiotic use should also be carefully monitored following FMT [17]. These multiple factors for consideration may affect the clinical practicality and feasibility of FMT for cancer patients receiving immunotherapy.
Probiotics
Probiotics are live microorganisms that may confer health benefits to the host by enhancing the gut microbiome [27]. Probiotics may range from simple formulations with monoclonal microbes to complex formulations involving multiple bacterial strains. Probiotics can be taken either as an oral supplement or obtained through fermented foods such as yogurt, kefir, sauerkraut, kombucha, miso, and kimchi [27]. Lactic acid bacilli such as Bifidobacterium and Lactobacillus are single strains of cultured bacteria that are widely commercially available, and they have been well studied in the context of various gastrointestinal disorders [27].
Studies investigating probiotic use in colorectal cancer patients found that probiotics increase butyrate-producing bacteria, especially Faecalibacterium and Clostridiales, in mucosal and fecal samples [28]. Furthermore, bacteria associated with colorectal cancer such as Fusobacterium and Peptostreptococcus are reported to be reduced in the stool samples of patients receiving probiotics [28]. Patients with colon cancer receiving 5-fluorouracil (5-FU) have also been found to experience decreased diarrheal symptoms when co-administered Lactobacillus rhamnosus [29].
In melanoma mouse models treated with immunotherapy, Lactobacillus was shown to be depleted in mice exhibiting symptoms of colitis [30]. When Lactobacillus reuteri was administered to the mice, toxicity symptoms were alleviated without impacting treatment efficacy [30]. Administration of Bifidobacterium in melanoma mouse models was also found to improve the anti-tumor effects of immunotherapy [13]. Other studies in mice with melanoma suggest that the specific bacteria that are enriched in Rs, such as Bacteroidetes thetaiotaomicron and Faecalibacterium prausnitzii, may be used in precision probiotic treatments to enhance the efficacy of immunotherapy [11].
Orally administered single-strain probiotics have demonstrated an improved anti-cancer response in mice receiving immunotherapy, and these results supports further investigation into its potential use in cancer patients [13]. However, bacterial colonization of the gut using probiotics in humans, who exhibit more diverse gut microbiomes, is much more challenging than that for mice [31]. While probiotic formulations are generally well tolerated by patients, safety remains an important factor for consideration given reports of bacterial translocation, in which organisms from the gut enter the bloodstream [32]. This adverse effect has been described in critically ill patients receiving commercially available probiotics [32].
Furthermore, when multi-strain probiotics were used to recolonize the gut microbiome following antibiotic use, the gut microbiome exhibited reduced diversity compared to the spontaneous recovery approach, highlighting the need for personalized probiotic formulations [31, 33]. Preliminary results from clinical studies in patients with melanoma also suggest that probiotics may negatively affect the gut microbiome [34]. Due to our knowledge limitations, off-trial probiotic use in the setting of immunotherapy is discouraged at this time.
Dietary Modifications and Prebiotics
Both dietary changes and prebiotics can significantly influence the gut microbiome and these modalities may be used as an intervention in individuals with more subtle microbiota disruptions [35]. For cancer patients, changes in the diet may significantly affect cancer biomarkers such as those for cellular proliferation [35, 36]. Yet, these potentially beneficial effects are just as rapidly reversible, and consistency with a specific diet is challenging for patients.
A preliminary study in melanoma patients has elucidated correlations between diet and treatment response [34]. In addition to overall diet quality, whole grains were found to be positively correlated with a composition of gut bacteria predictive of response to systemic therapy [34]. Conversely, added sugars and processed meats were negatively correlated with treatment response [34].
While probiotics consist of live microorganisms, prebiotics are nutrients such as resistant fibers that enrich the gut flora, and they are also being studied in the context of the gut microbiome and cancer. For instance, administration of inulin, a plant polysaccharide, can stimulate the growth of species that have been correlated with an increased response to immunotherapy, namely Faecalibacterium and Bifidobacterium [37]. Supplementation with both inulin and fructo-oligosaccharide may lead to enrichment of beneficial bacteria such as Lactobacillus and Bifidobacterium [37]. Patients with melanoma who consumed a high-fiber diet were more likely to respond to anti-PD-1 therapy compared to those who consumed a low-fiber diet [34].
Dietary modifications and prebiotics have been shown to significantly influence the levels of beneficial gut microbiome, and ongoing clinical studies in the setting of immunotherapy will further elucidate their potential use for melanoma patients.
Final Thoughts
The human microbiome impacts many aspects of cancer care, such as cancer prevention, development, treatment, and management, though the specific mechanisms remain unclear [2]. The gut microbiome may be important in terms of immune regulation and immunotherapy response in cancer patients. Preclinical animal models and clinical patient cohorts have shown that the gut microbiome may modulate response to immunotherapy in patients with metastatic melanoma. Through various intervention strategies, the microbiome may be potentially manipulated by clinicians to benefit melanoma patients receiving immunotherapy and improve their odds of treatment response.
As a proven method to alter the gut microbiota, FMT is currently being investigated in clinical trials in the setting of immunotherapy with the goal of augmenting treatment response and/or alleviating treatment-induced toxicity [17]. However, scaling and dissemination of FMT as a therapeutic intervention is challenging given inherent variation in donor FMT specimens across time. Other intervention modalities under investigation include the use of antibiotics, probiotics, prebiotics, and dietary changes. Each of these strategies vary in their cost and accessibility and bear important safety concerns to consider. Compared to FMT, interventions such as dietary changes and prebiotics may be more practical and feasible for patients receiving immunotherapy, though evidence of their effectiveness for patients with melanoma is still limited.
Clinical trials with integrated specimen collection will provide valuable information to help improve each of these approaches and advance our knowledge. By better understanding the interactions between the gut microbiome and the immune system, we may improve upon our abilities to alter the gut microbiome to optimize the efficacy of immunotherapy for cancer patients.
References
Li W, Deng Y, Chu Q, Zhang P. Gut microbiome and cancer immunotherapy. Cancer Lett. 2019;447:41–7.
Xavier JB, Young VB, Skufca J, Ginty F, Testerman T, Pearson AT, et al. The cancer microbiome: distinguishing direct and indirect effects requires a systemic view. Trends Cancer. 2020;6:192–204.
Thompson JA. New NCCN guidelines: recognition and management of immunotherapy-related toxicity. J Natl Compr Canc Netw. 2018;16:594–6.
Kennedy LB, Salama AKS. A review of cancer immunotherapy toxicity. CA Cancer J Clin. 2020;70:86–104.
Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561.
Seidel JA, Otsuka A, Kabashima K. Anti-PD-1 and anti-CTLA-4 therapies in cancer: mechanisms of action, efficacy, and limitations. Front Oncol. 2018;8:86.
Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018;359:97–103.
Matson V, Fessler J, Bao R, Chongsuwat T, Zha Y, Alegre ML, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science. 2018;359:104–8.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–7.
Chaput N, Lepage P, Coutzac C, Soularue E, Le Roux K, Monot C, et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann Oncol. 2017;28:1368–79.
Frankel AE, Coughlin LA, Kim J, Froehlich TW, Xie Y, Frenkel EP, et al. Metagenomic shotgun sequencing and unbiased metabolomic profiling identify specific human gut microbiota and metabolites associated with immune checkpoint therapy efficacy in melanoma patients. Neoplasia. 2017;19:848–55.
Vétizou M, Pitt JM, Daillère R, Lepage P, Waldschmitt N, Flament C, et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015;350:1079–84.
Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015;350:1084–9.
Baruch EN, Youngster I, Ben-Betzalel G, Ortenberg R, Lahat A, Katz L, et al. Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science. 2021;371:602–9.
Spain L, Diem S, Larkin J. Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev. 2016;44:51–60.
Halsey T, Ologun G, Wargo J, Jenq RR. Uncovering the role of the gut microbiota in immune checkpoint blockade therapy: a mini-review. Semin Hematol. 2020;57:13–8.
McQuade JL, Ologun GO, Arora R, Wargo JA. Gut microbiome modulation via fecal microbiota transplant to augment immunotherapy in patients with melanoma or other cancers. Curr Oncol Rep. 2020;22:74.
Blank CU, Rozeman EA, Fanchi LF, Sikorska K, van de Wiel B, Kvistborg P, et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat Med. 2018;24:1655–61.
Zimmer L, Livingstone E, Hassel JC, Fluck M, Eigentler T, Loquai C, et al. Adjuvant nivolumab plus ipilimumab or nivolumab monotherapy versus placebo in patients with resected stage IV melanoma with no evidence of disease (IMMUNED): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;395:1558–68.
Dubin K, Callahan MK, Ren B, Khanin R, Viale A, Ling L, et al. Intestinal microbiome analyses identify melanoma patients at risk for checkpoint-blockade-induced colitis. Nat Commun. 2016;7:10391.
Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell. 2018;33:570–80.
Wargo JA. Modulating gut microbes. Science. 2020;369:1302–3.
Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis. 2011;53:994–1002.
Taur Y, Coyte K, Schluter J, Robilotti E, Figueroa C, Gjonbalaj M, et al. Reconstitution of the gut microbiota of antibiotic-treated patients by autologous fecal microbiota transplant. Sci Transl Med 2018;10: eaap9489.
Borody TJ, Warren EF, Leis SM, Surace R, Ashman O, Siarakas S. Bacteriotherapy using fecal flora: toying with human motions. J Clin Gastroenterol. 2004;38:475–83.
Riquelme E, Zhang Y, Zhang L, Montiel M, Zoltan M, Dong W, et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell. 2019;178:795-806.e12.
McQuade JL, Daniel CR, Helmink BA, Wargo JA. Modulating the microbiome to improve therapeutic response in cancer. Lancet Oncol. 2019;20:e77–91.
Hibberd AA, Lyra A, Ouwehand AC, Rolny P, Lindegren H, Cedgård L, et al. Intestinal microbiota is altered in patients with colon cancer and modified by probiotic intervention. BMJ Open Gastroenterol. 2017;4: e000145.
Osterlund P, Ruotsalainen T, Korpela R, Saxelin M, Ollus A, Valta P, et al. Lactobacillus supplementation for diarrhoea related to chemotherapy of colorectal cancer: a randomised study. Br J Cancer. 2007;97:1028–34.
Wang T, Zheng N, Luo Q, Jiang L, He B, Yuan X, et al. Probiotics Lactobacillus reuteri abrogates immune checkpoint blockade-associated colitis by inhibiting group 3 innate lymphoid cells. Front Immunol. 2019;10:1235.
Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell. 2018;174:1388-405.e21.
Yelin I, Flett KB, Merakou C, Mehrotra P, Stam J, Snesrud E, et al. Genomic and epidemiological evidence of bacterial transmission from probiotic capsule to blood in ICU patients. Nat Med. 2019;25:1728–32.
Suez J, Zmora N, Zilberman-Schapira G, Mor U, Dori-Bachash M, Bashiardes S, et al. Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell. 2018;174(1406–23): e16.
Spencer CN, Gopalakrishnan V, McQuade J, Andrews MC, Helmink B, Khan MW, et al. The gut microbiome (GM) and immunotherapy response are influenced by host lifestyle factors. In: Proc American Association for Cancer Research Annual Meeting 2019; 2019 Mar 29–Apr 3; Atlanta, GA, USA.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–63.
Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359:1151–6.
Saedisomeolia A, Wood LG, Garg ML, Gibson PG, Wark PA. Anti-inflammatory effects of long-chain n-3 PUFA in rhinovirus-infected cultured airway epithelial cells. Br J Nutr. 2009;101:533–40.
Acknowledgements
Funding support
Tiffaney Tran is supported by a Melanoma Research Foundation grant. Russell Witt is supported by a National Institutes of Health T32 grant (CA 009599) and an MD Anderson Cancer Center support grant (P30 CA016672). Kelly C. Nelson is supported by philanthropic contributions of the Lyda Hill Foundation to the MD Anderson Cancer Center Moon Shots Program™. No sponsorship was received for this study or the publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
Kelly C. Nelson and Maleka Najmi contributed to the study conceptualization and design and performed the literature search. An initial evidence review was performed by Maleka Najmi. The first draft of the manuscript was written by Maleka Najmi, and all authors commented on previous versions of the manuscript. All authors reviewed and approved the final manuscript.
Disclosures
Maleka Najmi, Tiffaney Tran, Russell Witt, and Kelly Nelson have no conflicts of interest to disclose.
Compliance with Ethics Guidelines
This review is based on published literature and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Najmi, M., Tran, T., Witt, R.G. et al. Modulation of the Gut Microbiome to Enhance Immunotherapy Response in Metastatic Melanoma Patients: A Clinical Review. Dermatol Ther (Heidelb) 12, 2489–2497 (2022). https://doi.org/10.1007/s13555-022-00810-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00810-1