Abstract
Introduction
During the SARS-CoV-2 pandemic, personal protective equipment (PPE) became the new social norm for preventing COVID-19, but with an impact on the skin barrier. This study aimed to analyze the factors influencing PPE wearing, following hygiene rules, and effect on facial skin, including onset or exacerbation of dermatoses among healthcare workers (HCW) and non-healthcare workers (N-HCW).
Methods
In 2020, an original survey was carried out among 300 N-HCW and 60 HCW with 60 questions about using PPE and skin lesions experienced before and during the pandemic. Cross-sectional statistical analysis was completed to assess the interplay between environmental factors and maskne occurrence.
Results
The N-HCW group included 74% females and 26% males with an average age 24.67 ± 0.74. Among HCW respondents 91.7% were women and 8.3% were men, with an average age of 30.07 ± 0.36. All participants used PPE. Volunteers for N-HCW mainly chose a disposable (53.3%) and reusable masks (37.3%), while HCW preferred surgical (66.7%) and FFP2/FFP3/N95 masks (30%) and almost never used reusable masks (3.3%). HCW mainly spent 5–8 h with PPE, and N-HCW spent 1–4 h with PPE/day. Respondents with dermatological problems before the pandemic were more aware of the maskne and paid more attention to hygiene with PPE. Significantly, HCW experienced more severe facial skin lesions than N-HCW (p < 0.0001). There was statistical significance in following the basic hygienic rules of wearing PPE between both groups, where HCW practiced them more.
Conclusions
Maskne is a current and urgent problem to be cured. HCW should receive help if they develop maskne, such as limited time spent in PPE and treatment of the results of wearing it, as it is the main trigger of developing maskne. In addition, education about the correct use and choice of PPE should be improved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Maskne is a modern facial skin condition—rediscovered during the COVID-19 pandemic, when social media platforms drew attention to this matter. |
Since healthcare workers (HCW) were the first line of defense in fighting COVID-19, we investigated whether their experience of using personal protective equipment (PPE) was different due to their occupation relative to non-healthcare workers (N-HCW). Prolonged mask use, skin diseases, and reusing masks are triggers of face-mask-induced skin lesions. |
HCW more frequently developed maskne compared to N-HCW. |
Women also more often developed maskne in comparison to men in both groups. |
Introduction
The first case of SARS-CoV-2 infection in Poland was registered on March 4th, 2020, and 16 days after, the epidemic status emerged [1]. However, it was not mandatory, until April 16th, 2020, to wear personal protective equipment (PPE) outside and in public spaces.
By the time this article was written, it was required to cover the mouth and nose area just in closed areas and public transport.
When the pandemic erupted in 2020, what we did know about protecting ourselves from being infected by this virus was keeping distance, staying at home, disinfecting our hands, and wearing a mask or any other type of PPE in public spaces. As the last one mentioned became compulsory in many countries, a new problem occurred—facial skin problems. Most noted was maskne, which is a combination of two words—mask and acne [2]. Also, this term refers to acne mechanica—a type of acne caused by friction, pressure, rubbing, or occlusion of the facial skin in areas covered by PPE [2]. On facial skin, PPE creates a “dead space” between the face and the mask; this space traps sweat, oils, and dead skin cells beneath them that creates an ideal environment in terms of heat, humidity, and nourishment for the growth of bacteria. All these factors contribute to clogging pores and eventually to the development of purulent and seborrheic lesions in the areas covered by PPE. Thus, typical maskne locations are areas covered by PPE such as are chin, nose and areas around it, cheeks, and areas around the mouth [3]. Depending on the type of PPE, the locations may differ. Eventually, the criteria for diagnosing maskne were developed by Teo et al. which are developing acne in 6 weeks from the start of wearing masks or exacerbation of acne in the area covered by masks that is on the mouth, nose, and cheeks—the area named as “the O zone”. To confirm a diagnosis, it is needed to exclude some conditions in the previous patients’ history that may have affected the skin, such as seborrheic dermatitis, rosacea, or perioral inflammation [4].
The breadth and variety of different types of PPE and the extended use beyond previous standards have led to a spectrum of common dermatologic conditions, not only acne but also contact or irritant dermatitis, pressure-related skin injury, and moisture-associated skin irritation [5]. Maskne was previously seen mostly in athletes who wear special protective face gear and workers who wear helmets, but the SARS-CoV-2 pandemic and obligatory use of PPE spread the disease across the world [6]. Nowadays, due to much time being spent among possibly COVID-positive patients, the health care service workers have worn PPE for a long time and every day at their workplace, making this group more vulnerable to various facial dermatoses, including maskne. This phenomenon was already studied by Kaihui Hu et al. on healthcare workers (HCW) in Hubei province, who demonstrated that regular, long wearing of N95 masks led to developing scars and itch in the area covered by the PPE [7]. Furthermore, Techasatian et al. surveyed both HCW and non-healthcare workers (N-HCW) in Thailand resulting in confirmation of time and material of PPE being the trigger to developing adverse skin reactions, to the disadvantage of HCW, as they are more likely to use N95 masks [8]. Skin diseases are also an essential factor in worsening skin conditions in both HCW and N-HCW equally [9,10,11].
Our research expands these results to European habits of using and wearing PPE by frontline HCW and compares it to N-HCW in the Polish population.
The current study aimed to assess the choice and use of PPE by Polish HCW and N-HCW, comparing their knowledge, hygiene, and sanitary regime during PPE usage and their impact on facial skin, including new onset or exacerbation of existing facial dermatoses. We attempted to evaluate possible triggering or environmental factors influencing people’s behavior on PPE-wearing and facial skin conditions. Additionally, the survey intended to analyze the recognition of the "maskne" issue in both HCW and N-HCW, explore the recognition of that new acne type, and presumably raise the need for education on this issue.
Methods
An original anonymous self-designed online survey was carried out among 60 HCW and 300 N-HCW. A survey contained 60 questions split into sections: general information, dermatological interview, data on personal protective equipment information, and daily hygiene data.
A self-administered questionnaire was made using Google Forms and shared via social media platforms (Facebook, Facebook Medical Groups, Instagram). Data were collected from December 14th, 2020, to April 4th, 2021. Both groups answered a structured questionnaire regarding their choice and usage of PPE, knowledge and attitude regarding sanitary rules, their experience with PPE, especially their impact on facial skin. In addition, they were asked about facial skin lesions experienced before and during the pandemic. The used questionnaire is added to the Supplementary Materials. All the answers were equally crucial to our research, and its result reflects respondents’ personal opinions and assessments. Gained information was thoroughly checked to avoid duplication, misunderstandings, and incorrectness in the result. Uncompleted questionnaires were excluded from our research. The study was approved by the Bioethics Committee of the Medical University of Bialystok (approval no. APK.002.394.2020). All respondents provided informed consent.
Statistical Analysis
All the gathered responses underwent cross-sectional analysis, and non-numerical responses have been ranked based on the available literature data and our former clinical experience. Data characterized with a normal distribution were analyzed using Student's t test, non-parametric data were subjected to Mann–Whitney non-parametric analysis, whereas binary data underwent chi-square testing. Descriptive percentages values were presented as they are.
To assess the correlations between studied parameters Spearman rank test was used. Two-tailed p < 0.05 was considered statistically significant. Computations were performed using GraphPad 8 Prism Software (GraphPad Software, San Diego, CA, USA).
Results
General Data and Pre-pandemic Health Status
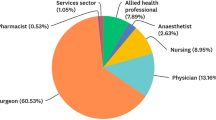
A total of 360 volunteers participated in the survey, 300 N-HCW and 60 HCW. In the group of HCW, 55 (91.7%) were women, and five (8.3%) were men. In the group of N-HCW, 222 (74%) were women, and 78 (26%) were men. The HCW group consisted of neatly selected people. The HCW group consisted of doctors, nurses, paramedics, medical assistants, or orderlies. Data about respondents’ age and occupation were also collected. Among N-HCW, the largest part were people aged 18 to 24, with an average age of 24.67 ± 0.74 years old, while HCW were mostly respondents between 25 and 35 years old, with an average age of 30.07 ± 0.36 years old. Respondents mostly lived in cities occupied by 150,000 to 500,000 citizens. Over half of all respondents (202/360, 56.1%) did not suffer from any dermatological disease. Moreover, 66.9% (241/360) did not visit a dermatologist before the pandemic. Among the people who suffered from dermatosis before the pandemic (HCW 28/60, 46.7%; N-HCW 130/300, 43.3%;), the respondents mainly mentioned acne (HCW 15/28, 53.6%; N-HCW 82/130, 63.1%), atopic dermatitis (HCW 5/28, 17.9%; N-HCW 22/130, 16.9%), seborrheic dermatitis (HCW 7/28, 25%; N-HCW 15/130, 11.5%), rosacea (HCW 1/28, 3.6%; N-HCW 11/130, 8.5%). Respondents were prescribed medications and skin care products according to the treatment regulations for their skin diseases. Patient demographics and characteristics of dermatological help are presented in Table 1.
During the pandemic, 98.3% of HCW (59/60) and 87.3% of N-HCW (262/300) claimed to have facial skin problems, either on the whole face or just around the mouth, nose, and cheeks area. Figures 1, 2, 3, and 4 compare both groups and the severity of their skin disease before and after the pandemic emerged.
Scaled intensity of symptoms on the whole face within a N-HCW group and HCW group before and after the pandemic. Pre-pandemic intensity of facial symptoms in N-HCW was mainly at levels 0 to III, after the pandemic began level IV and level V doubled in percentage of replies, while level III halved. Less visible changes were in the HCW group, where before the pandemic level III and II dominated, and after the pandemic began the level IV increased significantly, and level III decreased by half
Scaled intensity of symptoms on the areas covered by PPE. Before the pandemic began among N-HCW, there was a decreasing trend of appearance of symptoms. When the pandemic began, level IV as well as level V significantly increased, and a decrease occurred at the other levels. Similarly, among HCW, level IV and V significantly increased, level III remained the same, and level 0, I, and II decreased
Topical and systemic treatment was prescribed for lesions that emerged during the pandemic. Gels containing adapalene with benzoyl peroxide, clindamycin, or clindamycin with benzoyl peroxide were mostly used as a topical treatment, with 100% efficiency (9/9), but in 66.7% (6/9), the lesions came back. Oral lymecycline was mostly used as systemic treatment, with 80% efficiency (4/5), but in 75% (3/4), the lesions returned.
Preference and Usage of PPE
The most popular PPE used by our entire study group was a disposable surgical mask, then a reusable mask, and FFP2/FFP3/N95. The most chosen PPEs by HCW and N-HCW are represented in Figure S1 in the Supplementary Materials.
Amid disposable surgical mask users, 46.3% (74/160) of N-HCW and 40% (16/40) of HCW admitted to reusing their masks, 31.9% (51/160) of N-HCW and 35% (14/40) HCW did that occasionally, and only 21.9% (35/160) N-HCW and 25% (10/40) HCW never reused a mask. HCW reused the same mask less frequently than N-HCW (p = ns; p = 0.0437). A percentage distribution of reusing masks by both groups is presented in Figure S2 of the Supplementary Materials.
The majority of those who used the FFP2/FFP3/N95 mask had reused it regularly or seldom.
HCW spent approximately 5–8 h wearing PPE daily while N-HCW mostly spent 1–4 h wearing PPE. The time wearing PPE by HCW was significantly higher than the N-HCW (p = 0.026, p = 0.098, respectively). Symptoms of maskne in HCW and N-HCW were also positively correlated with time spent in PPE (p = 0.0367, p = 0.0026). In both groups, women spent more time wearing PPE each day than men, with significance only in N-HCW group (p = 0.0016). Women also more often developed maskne than men in both groups (p = 0.0001) (Fig. 5).
Almost half of all female respondents, 47.3% (131/277) (HCW: 50.9%, 28/55; N-HCW: 46.4%, 103/222) wore make-up underneath their PPE. The majority of all respondents admitted touching the face covered with PPE (Fig. S3).
Terms of following the hygiene rules while wearing a PPE included: (1) washing and disinfecting hands before and after putting it on – 19.7% N-HCW (59/300) and 23.3% HCW (14/60) did that after each use (p < 0.0001, p < 0.0001, respectively), (2) proper putting on, removing by the bands of PPE (Fig. S4).
Awareness of the Existence of the Term Maskne and the Issue
The overall awareness of the term “maskne” was fairly low. However, the N-HCW group knew the subject significantly better (35.3%, 106/300) than the HCW group (26.7%, 16/60) (p = 0.0022) (Fig. S5).
Symptoms and Factors Related to Wearing PPE
The most common feeling that the respondents had when wearing the masks was increased moisture on the face (HCW 81.7%, 49/60; N-HCW 75%, 225/300), followed by increased warming/redness of the face (HCW 30%, 18/60; N-HCW 35.7%, 107/300) and increased sweating (HCW 36.7%, 22/60; N-HCW 34.3%, 104/300).
In the research, we analyzed many factors that collated with the occurrence of maskne but also triggered the development of face-mask-induced skin lesions. All of them are listed in Table S1 in the Supplementary Materials; a positive R-value means the factor is collated to the occurrence of maskne.
These collected factors and results show that the pandemic times generally did not have a positive influence on facial skin. Maskne symptoms were developed by many in both HCW and N-HCW groups, as it is described below (Fig. 6).
Discussion
The COVID-19 pandemic was not the first one where a maskne problem was recognized. The problem first occurred in 2004 at the time of the SARS outbreak. At that time, it was recognized by Foo et al., who surveyed HCW in Singapore, from which 35.5% reported lesions characteristic of maskne: acne, facial itch, and rash [12]. The first published EBM articles about maskne as a COVID-19 issue were those by Teo WL, where the genesis, pathophysiology, risk factors, and treatments for this disease are discussed, although it was not the first time that the term maskne was used [4, 5]. Social media and culture widely popularized it before thorough research emerged in medical publications.
Due to compulsory and nonstop protection against SARS-CoV-2, HCW became patients themselves in dermatological offices, which is why a comparison of their behavior with the general population was made. Our research contained 60 HCW to 300 N-HCW. To our surprise, almost every questioned HCW (96.7%, 58/60) and 87.3% of N-HCW (262/300) had claimed to have facial skin problems, either on the whole face or just around the mouth, nose, and cheeks area. Moreover, before the pandemic, in both examined groups, the female gender and younger age were predisposed to maskne-like symptoms, such as itch, redness, excessive sweating, and purulent lesions. Similar results were obtained in Thailand, Turkey, Ireland, and Saudi Arabia, where females below 30 were found to be statistically significant to develop acne symptoms due to wearing PPE [8, 10, 13, 14]. Our research showed that in HCW wearing PPE for more than 8 h per day there was a strong correlation with developing maskne, whereas Kiely et al. and Sadia Yaqoob et al. have not found the duration of wearing masks to be statistically significant [11, 13]. However, Aravamuthan et al. and Techasatian et al., based on 215 and 833 respondents, respectively, confirmed that prolonged mask-wearing strongly influences emerging mask-induced acne [8, 15]. Altun et al. also observed that female gender and longer working hours are significant factors for developing maskne [16].
Spigariolo et al. presented diagnostic criteria for maskne based on Teo W-L. researching a recent publication, which are [4, 17]:
-
I.
Appearance of acne after 6 weeks of mask-use or aggravation of pre-existing acne in the mask area
-
II.
Elementary lesions as papules, pustules, and comedones;
-
III.
Localization in the area of mask or O-area;
-
IV.
Temporal relationship with mask use: aggravation/development of acne with prolonged usage (> 4–6 h/day) and improvement when not worn for a long period;
-
V.
Exclusion of other dermatoses such as perioral dermatitis, rosacea, seborrheic dermatitis, ICD, and ACD
The present study affirms that those who already suffer from skin illness, especially acne, AD, and rosacea, are more likely to both develop mask-induced acne lesions and progress their illness. Damiani et al. suggested the additional term, which is “mask rosacea” as in his research, patients with rosacea reported the deterioration of their face skin condition, developing especially papulopustular and erythematotelangiectatic lesions [18]. Other dermatoses such as atopic dermatitis, seborrheic dermatitis, and perioral dermatitis also progressed during the pandemic, especially in HCW that were obliged to wear masks for a very long time each day, as reported by the German study conducted by Niesert et al. [9]. Therefore, maskne can coexist with other dermatological diseases, and should be differentiated from other dermatoses, though symptoms, pathophysiology, and treatment may be similar to acne vulgaris [16, 19]. This aspect should be undoubtedly investigated, and more research is required to give patients proper care. HCW and N-HCW reported that their skin condition and illnesses, especially acne, were aggravated during the pandemic. Although in our research, the frequency of maskne symptoms suggested by Spigariolo et al. and Rudd et al. was higher in HCW than in N-HCW [17, 20].
This is confirmed in a recent publication of Niesert et al., where the advantage of HCW developing mask-related acne was statistically significant [9]. Previous studies do not recognize a statistical significance between occupation and developing maskne [7, 10, 18]. Case reports of patients with mask-related acne and adverse reactions prone to mask-wearing cover both groups, and the duration of wearing face-masks and skin illnesses prior to the pandemic were the component that triggered the occurrence of maskne [11, 18, 21, 22].
As the results of our research show, nodular and purulent lesions were the most reported by both groups—HCW and N-HCW during the time of obligatory coverage of the mouth and nose in public spaces. This was noticed by Han et al. in similar research, which states that both groups were diagnosed with a relapse or first attack of acne, though significantly more of their patients were provided healthcare [21]. It can be stated that patients who suffer from acne are the most vulnerable to developing maskne, which our results confirm. Techasatian et al. found the same dependence among the Thai population, where 54.5% of participants reported lesions in the O-zone area, among which 39.9% reported developing acne [8]. Our respondents pointed out increased moisture on the face as the most disturbing factor while wearing a mask (80% HCW and 75.7% N-HCW), which directly correlates with maskne pathophysiology theory [5]. Similar results were obtained by Bakhsh et al., where respondents complained of high humidity, sweating, and oily skin. This recent article also points out that those who suffered acne before the pandemic had relapsed their skin disease. Increased moisture triggers Cutibacterium acnes to multiply and the development of inflammation [5, 8]. They also noticed, what our report acknowledges that using surgical and N95 masks increase the risk of developing acne [12, 14]. Unfortunately, the vast majority of our respondents used surgical masks, although the CDC does not recommend wearing N95 respirators and surgical masks for N-HCW [23].
Surgical masks are made of three layers of non-woven polymer fabric; the most common material is polypropylene. N95 masks are produced from similar polymeric textures. Although polypropylene seems to be a thoroughly investigated component, incidents of developing skin diseases while having direct contact with this material have been occurring [24]. Case reports of contact allergic reactions and flares of rosacea or acne in both medical and non-medical users of these masks were, and still are, highly described. Monica Corazza et al. describe a case report on severe contact urticaria mimicking allergic contact dermatitis due to a surgical mask being worn during the COVID-19 pandemic [25]. Kaihui Hu et al. analyzed the HCW group, and the three most reported skin reactions were nasal bridge scars, facial itching, and skin damage [7]. Our study repeats these symptoms, as both HCW and N-HCW pointed out the loss of skin integrity, itch, and excessive dryness as their problems in the mouth, nose, and cheeks area and disturbing features of wearing a mask or face shield. The authors also suggested wearing a surgical mask underneath the N95 mask to prevent scar formation [7]. According to our research, the use of surgical masks may even worsen already-existing skin problems. Double layering might make an even more humid environment inside the mask, which according to Teo W., is crucial in forming lesions of maskne [5]. Pain was also observed as one of the disturbing features of HCW in our research. The problem of painful scars, aching, and local swelling was widely described in Ünver et al.'s publication, where nurses directly pointed out their problems and issues while wearing PPE [26]. There was no correlation between maskne-like symptoms and the type of PPE used prior to the pandemic, so Spigariolo et al. do not recommend any specific type of PPE since masks must be chosen relative to the personal risk of exposure [17]. On the contrary, Bakhsh et al. observed such a correlation in their analysis, where those wearing surgical masks were more prone to developing maskne [14]. Szepietowski et al. have not seen statistical significance in wearing a surgical mask or respirators, and neither does our study, although there is a slight advantage of disposable masks over N95 masks in developing itch (HCW 58.3%, 7/12, 41.7%, 5/12; N-HCW 56.3%, 18/32, 6.3%, 2/32, respectively). The authors also marked facial dermatoses as an important factor in developing itch while wearing PPE, which we also have observed in those suffering from acne and atopic dermatitis [27]. Overall, 13.3% of HCW and 10.7% of N-HCW developed itch in the mouth, nose, and cheeks area during the pandemic due to wearing masks in our research.
Many of our female respondents admitted to wearing makeup underneath masks. Statistical analysis showed the correlation between developing maskne-like lesions and makeup. Many products used for makeup are known to be comedogenic, especially the ones containing oils, and they trigger developing acne symptoms, named acne cosmetica [28]. Humidity and warmth underneath masks, as mentioned before, are the leading cause of mask-induced acne, but additionally, there is a chance of developing both types of acne—acne mechanica and cosmetologica—at the same time, which is why it is important to remember this aspect while providing a differential diagnosis and exact treatment [4, 17].
The questionnaire also obtained questions about seeking professional help and receiving treatment for both groups’ skin problems. According to the results, in the aspect of maskne, N-HCW rarely used dermatological help and HCW even less, even though they were already under the care of dermatologists, as they were suffering from other dermatoses before the pandemic began. On the contrary, N-HCW were more familiar with the term “maskne” itself than those who worked at the COVID-19 frontline. The obtained result is confirmed in Rudd et al.'s publication, where it is stated that social media played a great part in popularizing the term “maskne” during the pandemic [20]. The pandemic limited the availability of health care, so the low percentage of those who went to dermatologists is not surprising, i.e., in Italy, there was an approximately 80–90% reduction in doctors’ appointments. However convenient the situation was for dermatologists, as they easily converted to telemedicine, they were still experiencing difficulties correctly diagnosing and treating their patients [28, 29]. Referring to the results, the majority of those who suffered from maskne received any treatment. They mainly were prescribed typical topical treatment: monotherapy or combinations of antibiotics, benzoyl peroxide, and retinoids. Our study showed a high risk of relapse of lesions, even when a proper skincare regime and treatment were delivered. There might be many causes of inefficiency of treatment process, i.e., lack of knowledge about proper skincare regime and hygiene of wearing PPE. The present study shows that HCW put more attention into both mentioned before than N-HCW. HCW are significantly more aware of sanitary endangerment of improper usage and hygiene of masks than N-HCW. German research on a similar subject confirms all the above stated—HCW in their study also significantly took preventive measures in the crucial areas of developing maskne [9]. Nevertheless, it is highly needed to spread the knowledge about the proper usage of masks in the N-HCW, as only a small group knows its benefits and consequences.
This study is limited by its online method of surveying, as it was based on the personal perspective of respondents. As authors of this research, we could not check the actual condition of the respondents’ facial skin. Most respondents were women, who were more likely to participate in online surveys on dermatological and beauty topics. It is required to study the influence of particular types of face masks on developing skin lesions in both groups to identify which used materials may induce mask-related acne or, on the contrary, benefit those suffering from dermatoses. Further investigations are needed to improve the treatment guidelines targeted on maskne and a patient’s needs, namely personalized medicine. It is important to acknowledge both needs of a HCW and a regular patient.
Conclusions
The COVID-19 pandemic has affected every field of the health care system and dermatology was no different. Our study showed that maskne is a problem mainly for those who have already suffered from skin conditions, and both HCW and N-HCW can be affected. PPE is a trigger, an inducer of already-existing dermatoses because they cause the aggravation of disease symptoms, thus making it more challenging to treat. It does not say that those who have never been dermatological patients are not at risk of developing maskne, but the effect of wearing PPE on them is still minor. Maskne-enhancing factors include female gender, the total time spent in PPE, having chronic dermatological diseases, applying makeup, and lack of knowledge about the proper use of PPE. Regrettably, few people sought help from a specialist during the pandemic. Despite the advanced technology and social media reach, the term maskne was spread in a harmful way, sharing much fake news and disinformation, so the awareness of proper EBM research is needed to be improved. As HCW are more aware of the consequences of incorrect usage of PPE, they should be role models to others and spread their experiences to benefit us all. Ignorance, panic, and a decline in self-esteem can lead people to abandon wearing PPE, which may spread the SARS-CoV-2 virus further and, therefore, raise the number of infected.
References
Gujski M, Raciborski F, Jankowski M, Nowicka PM, Rakocy K, Pinkas J. Epidemiological analysis of the first 1389 cases of COVID-19 in Poland: a preliminary report. Med Sci Monit. 2020. https://doi.org/10.12659/MSM.924702.
Mazhar M, Simpson M, Marathe K. Inner thigh friction as a cause of acne mechanica. Pediatr Dermatol. 2019. https://doi.org/10.1111/pde.13817.
Soundarya S, Sundaramoorthy S. Unmasking the mask: COVID-19 manifestations of PPE kits. Our Dermatol Online. 2020;11:e186–e186.
Teo W-L. Diagnostic and management considerations for “maskne” in the era of COVID-19. J Am Acad Dermatol. 2021;84:520–1.
Teo W-L. The “Maskne” microbiome—pathophysiology and therapeutics. Int J Dermatology. 2021;60:799–809.
Tan KT, Greaves MW. N95 acne. Int J Dermatol. 2004;43:522–3.
Hu K, Fan J, Li X, Gou X, Li X, Zhou X. The adverse skin reactions of health care workers using personal protective equipment for COVID-19. Medicine. 2020;99: e20603.
Techasatian L, Lebsing S, Uppala R, et al. The effects of the face mask on the skin underneath: a prospective survey during the COVID-19 pandemic. J Prim Care Community Health. 2020;11:215013272096616.
Niesert A-C, Oppel EM, Nellessen T, Frey S, Clanner-Engelshofen BM, Wollenberg A, French LE, Reinholz M. “Face mask dermatitis” due to compulsory facial masks during the SARS-CoV-2 pandemic: data from 550 health care and non-health care workers in Germany. Eur J Dermatol. 2021;31:199–204.
Altun E, Topaloglu Demir F. Occupational facial dermatoses related to mask use in healthcare professionals. J Cosmetic Dermatol. 2021;21(6):2535–41.
Yaqoob S, Saleem A, Jarullah FA, Asif A, Essar MY, Emad S. Association of acne with face mask in healthcare workers amidst the COVID-19 outbreak in Karachi, Pakistan. CCID. 2021;14:1427–33.
Foo CCI, Goon ATJ, Leow Y-H, Goh C-L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome? A descriptive study in Singapore. Contact Dermatitis. 2006;55:291–4.
Kiely LF, O’Connor C, O’Briain G, O’Briain C, Gallagher J, Bourke JF. Maskne prevalence and associated factors in Irish healthcare workers during the COVID-19 pandemic. Acad Dermatol Venereol. 2022. https://doi.org/10.1111/jdv.18054.
Bakhsh RA, Saddeeg SY, Basaqr KM, Alshammrani BM, Zimmo BS. Prevalence and associated factors of mask-induced acne (maskne) in the general population of Jeddah during the COVID-19 pandemic. In: Cureus. 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9333340/
Aravamuthan R, Arumugam S. Clinico-epidemiological study of mask induced acne due to increased mask use among health care workers during COVID pandemic in a tertiary care institute. Int J Res Dermatol. 2020;7:48.
Altun E, Topaloglu Demir F. Occupational facial dermatoses related to mask use in healthcare professionals. J Cosmetic Dermatol. 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8662203/. Accessed 4 Aug 2022
Giacalone S, Minuti A, Spigariolo CB, Passoni E, Nazzaro G. Facial dermatoses in the general population due to wearing of personal protective masks during the COVID-19 pandemic: first observations after lockdown. Clin Exp Dermatol. 2021;46(2):368–9.
Damiani G, Gironi LC, Grada A, Kridin K, Finelli R, Buja A, Bragazzi NL, Pigatto PDM, Savoia P. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): Multi-center, real-life, telemedical, and observational prospective study. Dermatol Ther. 2021. https://doi.org/10.1111/dth.14848.
Kaul S, Kaur I, Jakhar D. Facial mask-related acne and acneiform eruption during the coronavirus disease 2019 pandemic: a case series. J Clin Aesthet Dermatol. 2021;14:32–4.
Rudd E, Walsh S. Mask related acne (“maskne”) and other facial dermatoses. BMJ. 2021. https://doi.org/10.1136/bmj.n1304.
Han C, Shi J, Chen Y, Zhang Z. Increased flare of acne caused by long‐time mask wearing during COVID‐19 pandemic among general population. Dermatol Ther. 2020;33(4):e13704. https://doi.org/10.1111/dth.13704
Chiriac AE, Wollina U, Azoicai D. Flare-up of rosacea due to face mask in healthcare workers during COVID-19. Maedica. 2020;15(3):416–7.
CDC. Masks and respirators. In: Centers for disease control and prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed 27 May 2022.
Chua MH, Cheng W, Goh SS, et al. Face masks in the new COVID-19 normal: materials, testing, and perspectives. Research. 2020;2020:1–40.
Corazza M, Bencivelli D, Zedde P, Monti A, Zampino MR, Borghi A. Severe contact urticaria, mimicking allergic contact dermatitis, due to a surgical mask worn during the COVID-19 pandemic. Contact Dermatitis. 2021;84:466–7.
Ünver S, Yildirim M, Cansu Yeni Ğün S. Personal protective equipment related skin changes among nurses working in pandemic intensive care unit: a qualitative study. J Tissue Viability. 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8785367/.
Szepietowski J, Matusiak Ł, Szepietowska M, Krajewski P, Białynicki-Birula R. Face mask-induced itch: a self-questionnaire study of 2,315 responders during the COVID-19 pandemic. Acta Derm Venereol. 2020;100: adv00152.
Gisondi P, Piaserico S, Conti A, Naldi L. Dermatologists and SARS-CoV-2: the impact of the pandemic on daily practice. J Eur Acad Dermatol Venereol. 2020;34:1196–201.
Stewart CR, Lipner SR. Clinical practice during the COVID-19 pandemic: a cross-sectional survey of attending dermatologists. Dermatol Ther. 2020. https://doi.org/10.1111/dth.14484.
Acknowledgements
Funding
This research and the journal’s Rapid Service Fee was funded by the Medical University of Bialystok, Poland, grant number SUB/1/DN/22/001/1149.
Author Contributions
Conceptualization: I.U.M., G.K., A.B.; Formal analysis: I.U.M., G.K., T.W.K. Software: T.W.K.; Investigation: I.U.M., G.K., A.B.; Writing—original draft preparation: I.U.M., G.K. Visualization: I.U.M., G.K., A.B., T.W.K.; Writing— review and editing: A.B., T.W.K.; Supervision: A.B., T.W.K., I.F.; Project administration: I.F.; All authors have read and agreed to the published version of the manuscript.
Disclosures
Izabela U. Malczynska, Gabriela Krych, Anna Baran, Tomasz W. Kaminski, and Iwona Flisiak declare no conflicts of interest.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the Medical University of Bialystok (approval no. APK.002.394.2020, dated 26 Nov 2020). Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Malczynska, I.U., Krych, G., Baran, A. et al. Maskne—Dermatosis of a Pandemic. A Survey on the Impact of PPE on Facial Skin Among HCW and N-HCW in Poland. Dermatol Ther (Heidelb) 12, 2297–2308 (2022). https://doi.org/10.1007/s13555-022-00796-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00796-w