Abstract
Topical formulation and delivery technologies for pharmaceutical application should simultaneously address efficacy, safety and convenience of therapy. This has historically proven to be challenging, since formulation features that drive efficacy often have undesirable consequences for safety and convenience and vice versa. Polyaphron dispersion (PAD) technology is a novel topical formulation and drug delivery system developed with the purpose of preserving these key attributes. PAD formulations are typically oil-in-water dispersions consisting of oil droplets encapsulated in a multi-molecular shell structure. This shell structure protects potentially unstable active molecules solubilized in the oil from hydrolytic degradation. Example data are presented of enhanced drug penetration from PAD formulations, including dermal delivery of calcipotriene, betamethasone dipropionate and tacrolimus as well as ocular delivery of ciclosporin A. Local tolerability is an important safety parameter for topical formulations, where high levels of surfactants can cause skin irritation. In this regard, a key benefit of PAD formulations is the inherent reduced requirement for surfactants to generate stable formulations compared to conventional emulsion systems. Patients with chronic diseases with topical manifestations such as psoriasis or atopic dermatitis have been reported to miss up to 70% of planned topical applications, mainly due to a lack of satisfaction with their therapy. Patients generally prefer light, moisturizing, non-greasy and quickly absorbed vehicles that are simple to use on all body parts. PAD formulations can generally be designed to meet these criteria. In conclusion, PAD technology provides high flexibility in topical drug design and can be applied to several body locations without compromising efficacy, safety or convenience of therapy.
Clinical Trial Register: Clinicaltrials.gov: NCT03802344.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Polyaphron dispersion (PAD) technology is a novel topical formulation and drug delivery system that, in a single product, combines efficacy and safety without compromising convenience of therapy. |
Topical formulation and delivery technologies for pharmaceutical application should simultaneously address efficacy, safety and convenience of therapy. |
Patients with chronic diseases with topical manifestations such as psoriasis or atopic dermatitis have been reported to miss up to 70% of planned topical applications, which can have a significant impact on treatment outcomes. |
A calcipotriene/betamethasone dipropionate cream has been developed using PAD technology, and this has demonstrated attractive skin penetration, efficacy, safety and patient satisfaction data in the treatment of plaque psoriasis in nonclinical and clinical trials. |
Introduction
Topical therapy is a popular treatment modality for many dermatological, ophthalmic and other indications where the target tissue can be reached by topical application without the potential safety concerns associated with the broader and higher drug exposure inherent to systemic therapy. The many and diverse topical drugs offered to physicians and patients have, over the years, demonstrated that a successful topical drug must meet three critical elements: (i) high efficacy, (ii) favourable safety and local tolerability, and (iii) convenience of the formulation in patients’ daily routines [1,2,3,4,5].
Convenience and aesthetic acceptability are particularly relevant to topical application, since greasiness, altered appearance and disrupted daily routines will negatively impact adherence to therapy and consequently real-world efficacy [1]. Certain application areas such as the scalp and face or highly inflamed and sensitive skin may require dosage forms that have differing physical attributes from a formulation designed for more general application. While topical formulations obviously need to optimize delivery of the active ingredients through the skin barrier to the target tissue, it is important that the vehicle formulation does not negatively impact the skin barrier structure and function or contain ingredients that can cause irritation or allergic sensitization [6].
Several drug delivery technologies and topical dosage forms have been developed, each having advantages [7, 8] but unfortunately also often having significant compromises. Among the standard dosage forms, ointments are based on fluid and/or solid oils, commonly white soft petrolatum, often combined with an aggressive solvent such as propylene glycol. Ointments generally offer high diffusion of active ingredients through the skin barrier [9] and immediate hydration by decreasing trans-epidermal water loss [10]. However, even assuming a low frequency of adverse reactions, many patients are averse to ointments on aesthetic grounds because of the difficulty rubbing in the medication and issues with the medication’s greasiness and the medication sticking to clothes [11]. Conventional creams and lotions tend to be more aesthetically pleasing, being easier to rub into the skin, and are less likely to stick to the patients’ clothing, resulting in a patient preference for these dosage forms [11,12,13]. Creams and lotions are usually based on emulsion technology, which employs high levels of surfactants to form physically stable oil-in-water dispersions without visual phase separation of oil and water. The high level of surfactants can lead to skin irritation caused by extraction of lipids and damage to the epidermal barrier function [14]. Furthermore, creams and lotions have traditionally generated products with lower efficacy compared to ointments due to suboptimal delivery of active ingredients through the skin barrier [15].
Challenges to drug safety and tolerability are often linked to the choice of active therapeutic agents, their pharmacology and their strength. Examples of typical application-site adverse reactions are contact dermatitis, folliculitis, skin atrophy or other forms of skin irritation. Alternatively, local tolerability may be compromised in an effort to optimize efficacy by the inclusion of excipients such as solubilizers or penetration enhancers that can, by themselves, cause application site reactions (e.g. propylene glycol).
Consequently, the development of topical therapies should consider the efficacy, safety and convenience of the product with equal importance. There is an unmet need within topical therapies for a vehicle that combines the low irritancy and effective drug delivery of ointments with the aesthetic appeal of light creams and lotions. The objective of this review is to present and discuss the properties and benefits of polyaphron dispersion (PAD) technology as a novel topical formulation and drug delivery system, including its ability to combine efficacy, safety and convenience of treatment.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Physical and Chemical Characteristics of Polyaphron Dispersion Technology
Polyaphrons (also called colloidal liquid aphrons and biliquid foams) have, over time, been used or proposed for diverse industrial applications (for example, in purification, extraction, drilling and waste water treatment [16, 17]) due to their high stability, specific physicochemical properties and ability to flow, but are relatively unknown in medical applications [17].
Herein we describe the specific application of polyaphrons dispersed in a polar solvent (usually water) for the formulation and topical delivery of pharmaceutical agents, which is also termed polyaphron dispersion technology or PAD technology. These formulations are typically oil-in-water dispersions with oil droplets in the range 1 to 50 µm. As such, they fall under the International Union of Pure and Applied Chemistry (IUPAC) definition of ‘emulsion’ [18], although they are structurally distinct and offer several advantages compared to conventionally stabilized emulsions.
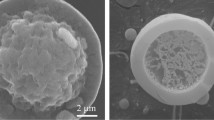
Polyaphron droplets are formed from an inner core of nonpolar solvent (typically a pharmaceutically acceptable oil) that, through the manufacturing process, is encapsulated in an outer shell with a multi-layer structure of surfactants, oil and water that stabilizes and separates the inner core from the continuous disperse phase (typically water). Sebba originally proposed that the shell structure is an organized surfactant bilayer and a so-called soapy shell [19]. However, based on subsequent studies, consensus has evolved that Sebba’s initial model is probably too simplistic and that a multi-molecular or multi-layer structure is an integrated part of the PAD droplet shell [17, 20]. This multi-molecular/layer organization should not be interpreted as uninterrupted static consecutive layers, but rather envisioned as a dynamic nanoscale three-dimensional bicontinuous structure involving surfactants and auxiliary molecules such as bound water and oil (Fig. 1). In specific systems, the thickness of the shell has been estimated to correspond to 80–350 molecules of surfactant or approximately 96–750 nm [21,22,23]. In conventional emulsions, the interfacial film formed between the oil and water is principally one surfactant molecule thick.
a Schematic illustration of a PAD technology formulation of oil-in-water droplets. A multimolecular layer of organized surfactant, oil and water forms a robust three-dimensional bicontinuous structure around the oil droplet. PAD technology formulations are manufactured with a low level of surfactant in the water and oil phases, in contrast to conventional emulsions that require a large excess of surfactant in the water phase to maintain physical stability. b Scanning electron microscope image of a cleaved polyaphron oil droplet. The central, rough, region is oil (olive oil in this example) and the smoother outer shell structure is surfactant, water and oil. c Scanning electron microscope image of a cleaved polyaphron oil droplet. The central oil core (brominated vegetable oil in this case) sublimated off during sample preparation, leaving the outer shell structure of surfactant, water and oil
Pharmaceutical PAD formulations are generally manufactured in a two-step process where the first step is the formation of an oil-in-water PAD with a high oil level of 80 to 90% w/w. In the second step, one or more high-oil-content pre-stabilized PADs are dispersed in an aqueous environment containing a polymeric gellant to obtain a physically stable oil-in-water dispersion (PAD formulation) (Fig. 2). The initial production of a high-oil-level dispersion generates the particular attributes of PAD droplets that are retained even upon dilution. This dilution and subsequent retention of benefits from the concentrated PAD is the principal precept of PAD technology. The two-step approach also permits great formulation flexibility, allowing various functionalities to be built into the final PAD-based formulation, e.g. therapeutic agents with different solubilities or incompatibilities can be fully solubilized in different oils close to their saturation limits for optimal tissue penetration, and a skin barrier or moisturization function can be integrated through correct selection of oils and the addition of natural moisturizing factors. Further, the final oil level can be adjusted in a wide range from eye drops with a very low oil content and light lotions and creams up to intensive creams with a high oil content. The overall droplet size in PAD formulations will depend on the choice of excipients and the applied manufacturing process. The rheology of the final PAD formulation and the prevention of creaming of the oil droplet dispersion is primarily controlled by the aqueous phase polymeric gel, in contrast to conventional emulsion creams that require excess levels of surfactants and the use of less-pleasing solid waxes to maintain physical stability. The polymeric gel can be of the carbomer or natural gum type and will impart a non-Newtonian shear point sufficient to prevent creaming. The rheology can be further customized by the incorporation of additional materials such as polymeric thickeners, usually cellulosic based, such as hypromellose or hydroxyethyl cellulose. The concentration, polymeric molecular weight, and potential synergistic interactions between polymers can allow the formulation of products that, while based on the same oil phase and exhibiting similar release/permeation behaviour, are perceived as light lotions or heavy creams due to differing thixotropic behaviour of the gel phase. Taken together, this means that PAD formulations can be designed to be aesthetically elegant and to target relevant body locations, including the scalp, without sacrificing the efficacy and tolerability of the formulation.
PAD technology formulations are generally manufactured in a two-step process where the first step is the formation of an oil-in-water PAD with a high oil level. In the second step, one or more high-oil-content pre-stabilized PAD premix modules are dispersed in an aqueous phase environment typically containing a polymeric gellant to obtain a physically stable final formulation. The PAD premix modules can be designed to provide different functionalities to the final PAD technology formulation
In addition to the greater aesthetic parameter, the use of an aqueous gel allows for the creation of physically robust creams with improved temperature insensitivity due to fewer potential temperature-induced phase changes. A quality by design (QbD) approach should be employed to ensure consistent and reliable performance of the drug product formulation from physical, chemical and pharmacological perspectives [24]. Some of the critical quality attributes that are typically employed to characterize PAD formulations are viscosity, droplet size, pH, chemical stability, preservation efficacy and skin penetration.
Both lipophilic and hydrophilic compounds can be formulated using PAD technology; however, only lipophilic compounds dissolved in the discontinuous oil phase take advantage of the protective properties of the droplet shell structure. Non-lipophilic compounds can be solubilized in the continuous phase, which, in addition to water, can contain high levels of alcohols and glycols for increased solubility of low-solubility compounds. Small molecules within the standard range of molecular weight allowing skin penetration (< 500 Da) are obvious choices for PAD technology [25]; however, larger molecules such as tacrolimus (804 Da) and ciclosporin A (1202 Da) can also be efficiently delivered as exemplified below. Macromolecules, including peptides/proteins and nucleotides, can be formulated in PAD technology. Peptides and proteins have in some systems been shown to associate with the oil–water interface and lead to increased stability or enzymatic activity [26, 27]; however, to the knowledge of the authors, no topical delivery data are currently available for macromolecules.
The formulation and processing flexibility associated with PAD technology enables the decoupling of oil droplet stabilization from the wider rheological system. The defined quality target product profile can thereby be reached more readily. This flexibility is achieved without the significant formulation compromises sometimes required with traditional semi-solid formulation methodologies. Furthermore, the “formulation space” around the preferred formulation can be readily explored and characterized so an optimized product is developed. The physical stability of well-processed PAD formulations is generally high, with very little change in visual appearance and droplet size during long-term storage. Some of the defining features for long-term storage stability are the choice of immiscible continuous and discontinuous solvent phases, the selection of surfactants with a hydrophilic–lipophilic balance matching the solvents, and processing that ensures uniform droplet size and stability of the gelled aqueous phase.
The emulsifying activity of surfactants is an essential component in the formation of stable emulsions. It is well accepted that non-ionic surfactants are less irritating than anionic, cationic or zwitterionic surfactants [14]. Conventional creams and lotions typically contain 2–5% surfactants to maintain physical stability. The level of surfactant shown to cause irritation such as erythema or a measurable change in skin hydration can be as low as 0.5% for anionic surfactants [28] and up to 2% w/w for non-ionic surfactants [14].
A key benefit of PAD formulations is the inherent reduced requirement for surfactants to generate stable dispersions. The highly focused distribution of surfactants in the PAD droplet shell allows the total level of surfactants in a PAD formulation to be from several fold up to 30-fold lower than in conventional emulsion creams and lotions with comparable oil content. The lack of excessive surfactants in PAD formulations reduces the risk of oil-soluble drugs being solubilized into the aqueous phase and possibly exposed to hydrolytic degradation, thereby giving greater chemical stability. It further minimizes wash-out of epidermal lipids, which can lead to disruption of the skin barrier function and skin irritation.
Topical Delivery of Active Compounds
Formulation of oil-soluble therapeutic agents using PAD technology has enabled enhanced penetration to target tissues. This can be attributed to several elements, including (i) the selection of excipients at optimal relative levels that will fully solubilize the drug, (ii) penetration driven by the evaporation of solvent/water upon skin application, leading to drug oversaturation, and (iii) low levels of water-soluble surfactants that may hinder skin penetration by forming bulky micellar structures around drug molecules.
The ability of PAD formulations to deliver calcipotriene (CAL, also known as calcipotriol) and betamethasone dipropionate (BDP) to human skin has been evaluated in Franz cell skin flux studies. Measurement of the cumulative flux of the drug through human epidermis was demonstrated to be significantly higher for CAL/BDP PAD-cream compared to the marketed anhydrous oil-based CAL/BDP topical suspension/gel, both formulations containing the same concentrations of CAL and BDP (Fig. 3a, b). The impact of different choices and levels of oils in PAD formulation variants on the skin flux efficiency of calcipotriene is shown in comparison to a marketed calcipotriene ointment in Fig. 3c. All PAD formulations had a greater skin flux than achieved with calcipotriene ointment. The improved flux for the PAD formulations resulted from a higher overall oil content and specific combinations of oils and penetration-enhancing excipients [29, 30].
Comparisons of Franz cell human skin flux through epidermis: CAL/BDP PAD cream versus CAL/BDP topical suspension (TS)/gel (a, b) and variants of CAL PAD cream regarding the content and type of oils versus CAL ointment (c). Methodology: Human skin was kept frozen until preparation. Subcutaneous fat was removed mechanically, and epidermis was removed from dermis by heat separation and mounted on a Franz cell chamber filled with receptor phase (70% phosphate-buffered saline, pH 7.4, 50 mM; 30% isopropanol). Test products were applied to the skin at 0, 16, 40 and 64 h, similar to the methodology described in Simonsen et al. [62]. An isocratic HPLC method was used for the detection of CAL and BDP in the receptor fluid. Error bars are illustrated at the standard error of the mean. Results of a statistical assessment by Student’s t-test comparing CAL/BDP PAD cream and CAL/BDP TS/gel at 72 h are displayed as *** (for p < 0.001) and **** (for p < 0.0001) [29, 30]
The translation of the enhanced skin flux properties of CAL/BDP PAD-cream to clinical efficacy has been demonstrated in two phase 3 trials evaluating efficacy and safety in the treatment of plaque psoriasis. The pooled phase 3 data demonstrate that a significantly greater proportion of patients achieved treatment success in the physician global assessment (PGA), defined as a minimum improvement of two grades to “clear” or “almost clear” disease. After 8 weeks of treatment, 43.2% of patients in the CAL/BDP PAD-cream group achieved PGA treatment success, compared to 31.9% in the CAL/BDP topical suspension/gel group (p < 0.0001) and 5.2% in the vehicle cream group (p < 0.0001) [31]. In one of the phase 3 trials, patients with body and scalp psoriasis were enrolled. In this trial, the percentage of patients achieving a PGA of “clear” or “almost clear”, representing controlled disease, was 62.2% in the CAL/BDP PAD-cream group compared to 11.4% in the vehicle group (p < 0.0001) (Fig. 4a). Further, 68.3% of patients with scalp psoriasis in the CAL/BDP PAD-cream group compared to 26.1% in the vehicle group achieved controlled disease (a PGA of “clear” or “almost clear”) on the scalp at week 8 (p < 0.0001), with a significant onset of efficacy already after 1 week of treatment (29.5% vs 0.1%; p < 0.0001) (Fig. 4b). This demonstrates that the CAL/BDP PAD cream is suitable for the treatment of psoriasis on both the body and scalp.
Prospective, vehicle and active-comparator controlled, randomized, phase 3 trial evaluating efficacy in patients with plaque psoriasis at multiple sites in Europe (MC2-01-C7; NCT03802344; N = 490). The design of the trial included a screening and 8-week treatment period. The trial population consisted of male and female patients above the age of 18 years with mild-to-moderate psoriasis according to PGA and with a treatment area of 2–30% of the body (trunk and/or limbs) (CAL/BDP PAD cream N = 213; PAD-cream vehicle N = 68). “Controlled disease” was defined as an improvement from baseline to clear or almost clear disease at the indicated time points. a Controlled disease assessed for the body. b Controlled disease assessed for patients with scalp psoriasis involving a minimum 10% of the scalp (CAL/BDP PAD cream N = 112; PAD-cream vehicle N = 38). Data are shown according to a treatment-policy strategy with multiple imputations, and p values represent a comparison of CAL/BDP PAD cream to vehicle calculated by a logistic regression model using randomized treatment, country and baseline PGA on the body as independent variables. The trial protocol was approved by institutional review boards for each site, and all patients provided written informed consent prior to any trial-related procedures. Detailed efficacy data from phase 3 trials are presented elsewhere [31, 63]
A PAD-technology-formulated cream of tacrolimus has also been formulated and its penetration evaluated in vivo in comparison to a marketed 0.1% tacrolimus ointment [32]. Tacrolimus penetration to epidermis and dermis was measured in skin biopsies taken from minipigs treated twice daily for 4 weeks with 0.03% PAD cream, 0.1% PAD cream and 0.1% tacrolimus ointment, which contains propylene carbonate, an aggressive aqueous solvent permeation enhancer. The highest concentration of tacrolimus was found in epidermis compared to dermis, and the concentration was higher for 0.1% PAD cream than for 0.03% PAD cream in both epidermis and dermis. Application of 0.1% PAD cream resulted in ~ 1.5-fold higher penetration to both epidermis and dermis than achieved with the 0.1% tacrolimus ointment comparator (Fig. 5). All the formulations were well tolerated, with no drug-related or vehicle-related skin reactions observed [33].
Penetration of tacrolimus into minipig epidermis (a) and dermis (b). Test products [tacrolimus PAD cream 0.03%, tacrolimus PAD cream 0.1% and tacrolimus ointment 0.1% comparator (Protopic® 0.1%)] were applied twice daily to eight 2.5 × 2.5 cm application sites on the backs of four male Göttingen minipigs (25 mg product/cm2). Skin biopsies (n = 8 per treatment) for bioanalysis by LC–MS/MS were collected after 28 days of treatment, 4 h after the last dosing. Epidermis was separated from dermis and subcutaneous tissue was removed from the dermis using a scalpel. Stratum corneum and any residual formulation were removed by 40 tape strips before punching the biopsy. Error bars are shown as standard error of the mean. The study was conducted according to Good Laboratory Practice for Medicinal Products as required by the Danish Health and Medicines Authority and in accordance with the OECD Principles of Good Laboratory Practice [33]
The enhanced penetration profile of PAD formulations has further been demonstrated in ocular delivery. Ocular penetration of ciclosporin A (CsA) from a PAD-formulation-based eye drop demonstrated 4.7-fold higher penetration to cornea for 0.06% CsA and 8.3-fold higher for 0.1% CsA compared to a marketed 0.05% CsA, as calculated by AUC 0.5–24 h (Fig. 6) [34].
Pigmented rabbits received a single instillation of 30 µl PAD 0.06% CsA, PAD 0.1% CsA or a marketed 0.05% CsA emulsion (Restasis®) in both eyes. Rabbit corneas were sampled at 0.5, 1, 2, 5, 12 and 24 h after instillation. CsA was extracted and the content was determined by a RRLC-MS/MS method (n = 6 eyes per data point) [34]. All animals were treated according to the European Convention and the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research [64]
Compliance with ethics guidelines was assured in all presented studies; please see the “Acknowledgements” section or figure legends for further details.
Local Tolerability and Safety
Favourable local tolerability and safety are important target features of topical therapies. Exposure of therapeutic agents is typically the main driver of local tolerability and safety outcomes, whereas excipients only occasionally trigger severe local adverse reactions. Some excipients can impair the skin barrier, while other excipients conversely can contribute to improving skin barrier function. Examples of excipients to avoid or minimize in a topical formulation are propylene glycol, benzalkonium chloride and ionic surfactants such as sodium lauryl sulfate [35], whereas excipients to consider to include because of their protective or repairing function are constituents of natural moisturizing factor and moisturizing oils [36].
PAD formulations can readily be developed to support high local tolerability and maintenance of the barrier function. Non-ionic surfactants are included at low levels and are well tolerated. Other excipients can be chosen with high flexibility and even selected to have protective functionality. As an example, a comparative 8-week dermal safety study in minipigs concluded that CAL/BDP PAD cream was well tolerated and a commercial CAL/BDP ointment comparator less well tolerated, with 50% (3 of 6) animals requiring 5 days off-dose during the study due to adverse reactions in the application site area. Similar systemic exposures of the active compounds between test groups were measured in the study (Fig. 7). In human clinical trials, all reported local application-site-related adverse reactions for CAL/BDP PAD cream were below 1%, with the most frequent being application-site pain, irritation, and pruritus, each with a frequency of 0.7% [31].
Pictures of minipigs from a dermal toxicity study taken after 4 weeks of once-daily application of CAL/BDP PAD cream (left) and a marketed CAL/BDP ointment (Daivobet®, right). The dermal toxicity study was part of nonclinical requirements in support of regulatory submissions. The study was conducted according to Good Laboratory Practice for Medicinal Products as required by the Danish Health and Medicines Authority and in accordance with the OECD Principles of Good Laboratory Practice [65]
Aesthetic Elegance and Satisfaction with Treatment
Recent guidelines for the topical treatment of psoriasis issued in both the United States and Europe recommend that clinicians consider patient preference when selecting the most appropriate vehicle for topical therapy [37,38,39]. Different vehicles may have different clinical advantages depending on, for instance, body location, hair density, and personal preference, which are important factors to take into account to ensure patient adherence to treatment.
It has previously been reported that up to 73% of psoriasis patients do not comply with their current treatment and that aesthetic acceptability, efficacy and safety are very important aspects of successful topical treatment of psoriasis [2, 13]. Qualitative and quantitative research has confirmed that efficacy, safety and formulation attributes are the most important parameters for both the choice of and adherence to any topical therapy intended for repeated long-term treatment of psoriasis [40]. When presented with the profile of CAL/BDP PAD cream, and having had the opportunity to test the PAD-cream vehicle, patients interviewed in-person (n = 11) rated the “the overall reaction to the product” a score of 6.3 and the “likelihood of requesting the product” a score of 6.8 on a scale of 1 (extremely unlikely) to 7 (extremely likely). Patients interviewed by telephone (n = 15) and by a web-based questionnaire (n = 113) without physical testing of the product had a slightly lower rating of the likelihood of requesting the product (5.6 and 5.5, respectively), indicating that patients may generally expect topical therapies to be burdensome and that there is a potential to exceed such expectations by using novel topical vehicles.
Generally, there is a need for validated tools to evaluate patients’ acceptance of topical therapy vehicles [41]. A psoriasis treatment convenience scale (PTCS) has been validated, consisting of five questions addressing ease of application, greasiness, moisturization and impact on the daily routine plus an overarching question regarding the patient’s overall satisfaction with the treatment [42]. Other examples of similar questionnaires are the Vehicle Preference Measure [43], the Topical Therapy Adherence Questionnaire (TTAQ) [44] and the Topical Product Usability Questionnaire (TPUQ) [45]. These instruments can be used to directly compare the acceptability of vehicles, as exemplified by the superiority of psoriasis treatment convenience in favour of CAL/BDP PAD cream versus CAL/BDP suspension/gel [31] and an overall preference for suspension/gel over CAL/BDP foam identified using TPUQ [45]. However, even though gross differences in patients’ acceptance of topical therapy vehicles can be evaluated by direct comparison, personal preferences can vary and should be considered by physicians [46].
Discussion
Many topical delivery technologies and formulations have, even in recent years, almost exclusively focused on drug delivery and the efficacy of the therapeutic agent. Indeed, efficacy is a critical component of regulatory approval, detailing to medical communities and market access. Several examples have demonstrated that innovative topical delivery vehicles for specific therapeutic agents can attain significantly differentiated clinical and patient-reported outcomes compared to more traditional formulations [15]. However, it is also well accepted that patients’ real-world overall treatment satisfaction with topical products is much more complex than just pure efficacy. Studies have demonstrated that product efficacy, safety and convenience all play a key role in ensuring the highest possible adherence to therapy by patients [1,2,3,4, 47]. Patients with psoriasis and atopic dermatitis have been reported to miss up to around 70% of planned topical applications when the treatment period extends to several weeks, leading to suboptimal treatment outcomes, reduced quality of life and increased healthcare costs [1, 13, 48, 49]. Patients generally prefer light, moisturizing, non-greasy and quickly absorbed vehicles for reasons of ease of application and aesthetic acceptability [50]. Patient preference may further be affected by dermatologic condition, age and race [45, 50, 51].
As described in the previous sections, PAD technology has enabled the clinical development of topical formulations characterized by a combination of high drug penetration and efficacy, favourable safety and convenient application for the patient. High penetration of CAL and BDP has also been achieved by an alternative pressurized paraffin-based anhydrous aerosol foam formulation in which the two drug compounds are solubilized in a supersaturated form [52]. While this formulation has demonstrated high clinical efficacy [53], it lacks the treatment satisfaction associated with CAL/BDP PAD cream, including parameters concerning ease of application and greasiness [54].
During the last 20 years, tacrolimus ointment has been widely used as an efficacious treatment of atopic dermatitis and related indications, although patient acceptability of the formulation has been rated low [55]. A cream emulsion formulation of tacrolimus has been under development as an alternative to the marketed tacrolimus ointment [56]. Tacrolimus cream variants demonstrated the same or higher penetration through rat skin compared to ointment; however, storage stability data was questionable and clinical development was never completed [56].
The ability of psoriasis patients to adhere to twice-daily therapy of tacrolimus ointment and salicylic acid gel for 8 weeks has been studied by the use of electronic monitoring caps on the topical medication bottles. Based on the electronic monitoring log, adherence to therapy declined to 51% after 8 weeks, whereas the patients reported their adherence as 90% in their own log [57]. Analysis of efficacy in this trial showed that the adherence rate was a significant predictor of improvement. A 10% decrease in treatment adherence was associated with a loss of efficacy of 1 point on a 0–9 point scale, corresponding to an almost 20% reduction in efficacy improvement from baseline [58], illustrating the importance of treatment adherence for overall real-world efficacy. A study of 102 psoriasis patients concluded that adherence was significantly higher for patients applying gels and creams than for those using ointments whenever the body area affected was extensive, while the opposite was found when the affected area was small [13]. This is further substantiated by a 52-week, prospective, observational trial in psoriasis patients in which CAL/BDP suspension/gel was associated with higher treatment convenience, adherence, and overall satisfaction ratings than CAL/BDP ointment, resulting in a relatively high real-world efficacy of the suspension/gel formulation relative to the ointment. This was in contrast to lower efficacy levels of the suspension/gel versus the ointment when determined in a controlled clinical setting in which patient compliance was assured [59, 60].
While topical drug efficacy and safety should always be considered in the choice of topical therapies, the general recommendation is to keep the treatment regimen as simple as possible, i.e. applicable to all relevant disease severities and body locations, to take into account patient preferences in the treatment decision-making process, and to provide educational support to increase the ability of patients to control their own therapy [46, 61]. Topical PAD formulations have the potential to address some of these challenges as they have great flexibility in topical drug design.
Conclusions
Patients with chronic diseases with topical manifestations have been reported to miss a significant fraction of the prescribed applications, mainly due to a lack of satisfaction with the therapy. PAD technology is a novel formulation and drug delivery system that provides great flexibility in topical drug design. PAD formulations can, in a single product, be designed to be applicable to several body locations without compromising efficacy, safety and convenience of therapy. Improving adherence to treatment for patients may ultimately result in better treatment outcomes in real-world clinical practice.
References
Bewley A, Page B. Maximizing patient adherence for optimal outcomes in psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 4):9–14.
Fouere S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(Suppl 3):2–6.
Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006;55(4):607–13.
van de Kerkhof PC, Steegers-Theunissen RP, Kuipers MV. Evaluation of topical drug treatment in psoriasis. Dermatology. 1998;197(1):31–6.
Mohammed YH, Moghimi HR, Yousef SA, Chandrasekaran NC, Bibi CR, Sukumar SC, et al. (2017) Efficacy, safety and targets in topical and transdermal active and excipient delivery. In: Dragicevic NI, Maibach H, editors., et al., Percutaneous penetration enhancers drug penetration into/through the skin: methodology and general considerations. Heidelberg: Springer; 2017. p. 369–91.
Lemery E, Briançon S, Chevalier Y, Oddos T, Gohier A, Boyron O, et al. Surfactants have multi-fold effects on skin barrier function. Eur J Dermatol. 2015;25(5):424–35.
Mayba JN, Gooderham MJ. A guide to topical vehicle formulations. J Cutan Med Surg. 2018;22(2):207–12.
Benson HAE, Grice JE, Mohammed Y, Namjoshi S, Roberts MS. Topical and transdermal drug delivery: from simple potions to smart technologies. Curr Drug Deliv. 2019;16(5):444–60.
Cevc G, Mazgareanu S, Rother M, Vierl U. Occlusion effect on transcutaneous NSAID delivery from conventional and carrier-based formulations. Int J Pharm. 2008;359(1–2):190–7.
Hashim PW, Chen T, Hebert AA, Kircik LH. Topical treatment for the management of atopic dermatitis. J Drugs Dermatol. 2019;18(s2):s112–6.
Puig L, Carrascosa JM, Belinchon I, Fernandez-Redondo V, Carretero G, Ruiz-Carrascosa JC, et al. Adherence and patient satisfaction with topical treatment in psoriasis, and the use, and organoleptic properties of such treatments: a Delphi study with an expert panel and members of the Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Actas Dermo-Sifiliograf. 2013;104(6):488–96.
Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4(4):221–4.
Teixeira A, Teixeira M, Almeida V, Gaio R, Torres T, Magina S, et al. Does the vehicle matter? Real-world evidence on adherence to topical treatment in psoriasis. Pharmaceutics. 2021;13(10):1539.
Fujimura T, Shimotoyodome Y, Nishijima T, Sugata K, Taguchi H, Moriwaki S. Changes in hydration of the stratum corneum are the most suitable indicator to evaluate the irritation of surfactants on the skin. Skin Res Technol. 2017;23(1):97–103.
Iversen L, Dauden E, Segaert S, Freeman K, Magina S, Rigopoulos D, et al. Reformulations of well-known active ingredients in the topical treatment of psoriasis vulgaris can improve clinical outcomes for patients. J Eur Acad Dermatol Venereol. 2017;31(8):1271–84.
Molaei A, Waters KE. Aphron applications—a review of recent and current research. Adv Colloid Interface Sci. 2015;216:36–54.
Ward K, Taylor A, Mohammed A, Stuckey DC. Current applications of colloidal liquid aphrons: predispersed solvent extraction, enzyme immobilization and drug delivery. Adv Colloid Interface Sci. 2020;275: 102079.
McNaught AD, Wilkinson A. Compendium of chemical terminology. Hoboken: Blackwell Science; 1997. p. 464.
Sebba F. Foams and biliquid foams, aphrons. New York: Wiley; 1987.
Yan Y-l, Zhang N-S, Qu C-T, Liu L. Microstructure of colloidal liquid aphrons (CLAs) by freeze fracture transmission electron microscopy (FF-TEM). Colloids Surf A Physicochem Eng Asp. 2005;264(1):139–46.
Amiri MC, Woodburn ET. A method for the characterisation of colloidal gas aphron dispersions. Chem Eng Res Des. 1990;68:154–60.
Bredwell MD, Worden RM. Mass-transfer properties of microbubbles. 1. Experimental studies. Biotechnol Progr. 1998;14(1):31–8.
Jauregi P, Mitchell GR, Varley J. Colloidal gas aphrons (CGA): dispersion and structural features. AIChE J. 2000;46(1):24–36.
Namjoshi S, Dabbaghi M, Roberts MS, Grice JE, Mohammed Y. Quality by design: development of the quality target product profile (QTPP) for semisolid topical products. Pharmaceutics. 2020;12(3):287.
Bos J, Meinardi MM. The 500 dalton rule for the skin penetration of chemical compounds and drugs. Exp Dermatol. 2000;9(3):165–9.
Lye GJ, Stuckey DC. Structure and stability of colloidal liquid aphrons. Colloids Surf A Physiochem Eng Asp. 2016;131(1–3):119–36.
Ward K, Cortés JGC, Stuckey DA-O. Alginate as a support ligand for enhanced colloidal liquid aphron immobilization of proteins and drug delivery. Biotechnol Bioeng. 2018;116(12):3168–78.
Wilhelm KP, Surber C, Maibach HI. Effect of sodium lauryl sulfate-induced skin irritation on in vivo percutaneous penetration of four drugs. J Invest Dermatol. 1991;97(5):927–32.
MC2 Therapeutics. Diffusion 85 comparison of MC2-01 cream formulations: distribution of actives, reduced number of PADs. Hørsholm: MC2 Therapeutics; 2017.
MC2 Therapeutics. MC2 therapeutics skin flux study 92. Hørsholm: MC2 Therapeutics; 2016.
Pinter A, Green LJ, Selmer J, Praestegaard M, Gold LS, Augustin M, et al. A pooled analysis of randomized, controlled, phase 3 trials investigating the efficacy and safety of a novel, fixed dose calcipotriene and betamethasone dipropionate cream for the topical treatment of plaque psoriasis. J Eur Acad Dermatol Venereol JEADV. 2022;36(2):228–36.
Protopic ointment. European public assessment report - product information. European Medicines Agency. 2022.
CiToxLab. Topical tacrolimus cream—a 4-week local skin tolerance study in minipigs (study ID: 77536; MC2-11-PC01). Évreux: CiToxLab; 2020.
Praestegaard M, Steele F, Gomez F. Pharmacokinetic characterization of a novel ocular formulation of ciclosporin. Investig Ophthalmol Visual Sci. 2016;57(12):5388.
EC. Annex to the European Commission guideline on ‘Excipients in the labelling and package leaflet of medicinal products for human use’ (SANTE-2017-11668). Brussels: EC; 2019.
Lebwohl M, Herrmann LG. Impaired skin barrier function in dermatologic disease and repair with moisturization. Cutis. 2005;76(6 Suppl):7–12.
Elmets CA, Korman NJ, Prater EF, Wong EB, Rupani RN, Kivelevitch D, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2020;84(2):432–70.
Maul JT, Anzengruber F, Conrad C, Cozzio A, Häusermann P, Jalili A, et al. Topical treatment of Psoriasis vulgaris: the Swiss Treatment Pathway. Dermatology. 2021;237(2):166–78.
Körber A, Wilsmann-Theis D, Augustin M, von Kiedrowski R, Mrowietz U, Rosenbach T, et al. Topische Therapie bei Psoriasis vulgaris—ein Behandlungspfad. J Dtsch Dermatol Ges. 2019;17(Suppl 4):3–14.
Triangle Insights Group. Primary and secondary qualitative and quantitative research of positioning of MC2-01 PAD-cream for psoriasis. Durham: Triangle Insights Group; 2017.
Kornmehl H, Callis Duffin K, Salame N, Perez-Chada LM, Singh S, Garg A, et al. Examination of treatment satisfaction instruments in psoriasis: 2017 results from the Psoriasis Working Group of the International Dermatology Outcome Measures (IDEOM). Dermatology. 2021;237(2):151–7.
Feldman SR, Præstegaard M, Andreasen AH, Selmer J, Holm-Larsen T. Validation of the self-reported psoriasis treatment convenience scale (PTCS). Dermatol Ther (Heidelb). 2021;11(6):2077–88.
Housman TS, Mellen BG, Rapp SR, Fleischer AB Jr, Feldman SR. Patients with psoriasis prefer solution and foam vehicles: a quantitative assessment of vehicle preference. Cutis. 2002;70(6):327–32.
Zschocke I, Mrowietz U, Lotzin A, Karakasili E, Reich K. Assessing adherence factors in patients under topical treatment: development of the Topical Therapy Adherence Questionnaire (TTAQ). Arch Dermatol Res. 2014;306(3):287–97.
Hong CH, Papp KA, Lophaven KW, Skallerup P, Philipp S. Patients with psoriasis have different preferences for topical therapy, highlighting the importance of individualized treatment approaches: randomized phase IIIb PSO-INSIGHTFUL study. J Eur Acad Dermatol Venereol. 2017;31(11):1876–83.
Augustin M, Holland B, Dartsch D, Langenbruch A, Radtke MA. Adherence in the treatment of psoriasis: a systematic review. Dermatology. 2011;222(4):363–74.
Hoelker S, Ninosu N, Buettner S, Peitsch WK, Schaarschmidt ML. Patient preferences for topical psoriasis treatments: a discrete choice experiment. J Dermatolog Treat. 2022;33(5):2595–604.
Devaux S, Castela A, Archier E, Gallini A, Joly P, Misery L, et al. Adherence to topical treatment in psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(Suppl 3):61–7.
Tier HL, Balogh EA, Bashyam AM, Fleischer AB Jr, Spergel JM, Masicampo EJ, et al. Tolerability of and adherence to topical treatments in atopic dermatitis: a narrative review. Dermatol Ther (Heidelb). 2021;11(2):415–31.
Eastman WJ, Malahias S, Delconte J, DiBenedetti D. Assessing attributes of topical vehicles for the treatment of acne, atopic dermatitis, and plaque psoriasis. Cutis. 2014;94(1):46–53.
Figenshau K, Kimmis BD, Reicherter P. Variations in preference for topical vehicles among demographic groups. Cutis. 2020;106(1):40–3.
Lind M, Nielsen KT, Schefe LH, Nørremark K, Eriksson AH, Norsgaard H, et al. Supersaturation of calcipotriene and betamethasone dipropionate in a novel aerosol foam formulation for topical treatment of psoriasis provides enhanced bioavailability of the active ingredients. Dermatol Ther (Heidelb). 2016;6(3):413–25.
Menter A, Gold LS, Koo J, Villumsen J, Rosen M, Lebwohl M. Fixed-combination calcipotriene plus betamethasone dipropionate aerosol foam is well tolerated in patients with Psoriasis vulgaris: pooled data from three randomized controlled studies. Skinmed. 2017;15(2):119–24.
Reich A, Selmer J, Galván J, Trebbien P, Pi-Blanque A, Danø A, et al. Efficacy, quality of life, and treatment satisfaction: an indirect comparison of calcipotriol/betamethasone dipropionate cream versus foam for treatment of psoriasis. Curr Med Res Opin. 2022;38(9):1521–9.
Kempers S, Boguniewicz M, Carter E, Jarratt M, Pariser D, Stewart D, et al. A randomized investigator-blinded study comparing pimecrolimus cream 1% with tacrolimus ointment 0.03% in the treatment of pediatric patients with moderate atopic dermatitis. J Am Acad Dermatol. 2004;51(4):515–25.
Yamanaka M, Yokota S, Iwao Y, Noguchi S, Itai S. Development and evaluation of a tacrolimus cream formulation using a binary solvent system. Int J Pharm. 2014;464(1–2):19–26.
Carroll CL, Feldman SR, Camacho FT, Manuel JC, Balkrishnan R. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51(2):212–6.
Carroll C, Feldman S, Camacho FT, Balkrishnan R. Better medication adherence results in greater improvement in severity of psoriasis. Br J Dermatol. 2004;151(4):895–7.
Lambert J, Hol CW, Vink J. Real-life effectiveness of once-daily calcipotriol and betamethasone dipropionate gel vs. ointment formulations in Psoriasis vulgaris: final analysis of the 52-week PRO-long study. J Eur Acad Dermatol Venereol. 2015;29(12):2349–55.
Queille-Roussel C, Hoffmann V, Ganslandt C, Hansen KK. Comparison of the antipsoriatic effect and tolerability of calcipotriol-containing products in the treatment of Psoriasis vulgaris using a modified psoriasis plaque test. Clin Drug Investig. 2012;32(9):613–9.
Tan X, Feldman SR, Chang J, Balkrishnan R. Topical drug delivery systems in dermatology: a review of patient adherence issues. Expert Opin Drug Deliv. 2012;9(10):1263–71.
Simonsen L, Hoy G, Didriksen E, Persson J, Melchior N, Hansen J. Development of a new formulation combining calcipotriol and betamethasone dipropionate in an ointment vehicle. Drug Dev Ind Pharm. 2004;30(10):1095–102.
Stein Gold L, Green LJ, Dhawan S, Vestbjerg B, Praestegaard M, Selmer J. A phase 3, randomized trial demonstrating the improved efficacy and patient acceptability of fixed dose calcipotriene and betamethasone dipropionate cream. J Drugs Dermatol. 2021;20(4):420–5.
Iris Pharma. Study report: pilot ocular pharmacokinetic study of PAD formulations following a single topical ocular administration in pigmented rabbit (study ID: M59K24412). La Gaude: France; 2013.
CiToxLab. Study report: calcipotriene/betametasone cream: a 8-week toxicity study in minipigs (study ID 76232; MC2-01-PC02). Évreux: CiToxLab; 2015.
Acknowledgements
Funding
Presented data are derived from studies funded by MC2 Therapeutics, Hørsholm, Denmark. MC2 Therapeutics is funding the journal’s Rapid Service Fee.
Author Contributions
All authors have contributed to the drafting of the manuscript. MP has contributed to all presented studies; FS has contributed to the development of PAD technology and studies presented in Figs. 3 and 6; NC has contributed to the development of PAD technology and the study presented in Fig. 5.
Prior Presentation
Phase 3 clinical trial data concerning the efficacy of CAL/BDP PAD cream on the scalp have been presented on a poster at Winter Clinical (Hawaii, US, 2022). Ocular penetration data of ciclosporin A have been presented on a poster at the Association for Research in Vision and Ophthalmology Annual Meeting (Seattle, US, 2016).
Disclosures
Morten Praestegaard, Fraser Steele and Nigel Crutchley are employees of MC2 Therapeutics.
Compliance to Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Praestegaard, M., Steele, F. & Crutchley, N. Polyaphron Dispersion Technology, A Novel Topical Formulation and Delivery System Combining Drug Penetration, Local Tolerability and Convenience of Application. Dermatol Ther (Heidelb) 12, 2217–2231 (2022). https://doi.org/10.1007/s13555-022-00794-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00794-y