Abstract
Background
Narrow-band (NB) UVB has been combined with a number of topical treatments. However, there have been no specific data regarding treatment results of a fixed combination of calcipotriene 50 μg/g plus betamethasone 0.5 mg/g aerosol foam (Cal/BD) combined with NB-UVB phototherapy so far.
Objectives
To assess the efficacy of Cal/BD foam coupled to twice-weekly NB-UVB and whether this combined regimen requires fewer UVB treatments and a lower cumulative UVB dose compared to phototherapy alone.
Methods
This cross-sectional, prospective, parallel-group study enrolled 187 consecutive moderate-to-severe psoriatic patients who were allocated to two groups in a 1:2 ratio. The overall duration of the treatment cycle was 12 weeks. At baseline and after 2, 4, 8 and 12 weeks, we registered the modified (not considering head lesions) PASI, the number of Cal/BD applications, the NRS score for itching and the adverse effects.
Results
The combined regimen was more effective in clearing psoriasis [final mPASI: 2.1 (0; 8.2) versus 4.4 (0; 19.6); p < 0.01] and reducing itching [(final NRS score for itching: 0 (0; 3) versus 1 (0; 4); p < 0.01]. Fewer exposures [12 (4; 20) versus 24 (8; 24); p < 0.01] and a lower cumulative UVB dose [6.1 (5.4; 9.3) J cm−2 versus 13.1 (9.8; 19.7) J cm−2; p < 0.01] were required. A higher number of patients achieved complete clearance [47 (74.6%) versus 58 (46.8%) patients (p < 0.001)]. Both treatments were well tolerated without acute adverse effects.
Conclusion
Cal/BD + NB-UVB is a very effective treatment that produces a rapid improvement in clinical lesions and itching and can be considered a valuable alternative to systemic treatments for psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There are no specific data regarding treatment results of a fixed combination of calcipotriene 50 μg/g plus betamethasone 0.5 mg/g aerosol foam (Cal/BD) combined with NB-UVB phototherapy. |
What did the study ask?/What was the hypothesis of the study? |
The combined regimen was more effective in clearing psoriasis and reducing itching. |
What was learned from the study? |
A higher number of patients achieved complete clearance. |
What has been learned from the study? |
Cal/BD + NB-UVB is a very effective treatment that produces a rapid improvement in clinical lesions and itching and can be considered a valuable alternative to systemic treatments for psoriasis. |
Introduction
Despite recent treatment advances, unmet needs for psoriatic patients still remain, and narrow-band UVB (NB-UVB) phototherapy remains a pillar in the treatment strategy.
However, there is no standard optimal phototherapeutic protocol: efficacy is not only measured with the rate of healed patients, but also through the total number of sessions needed and the cumulative UV doses used.
A possible strategy to achieve these goals is the combination of NB-UVB with systemic treatments, e.g. acitretin, methothrexate and biologics [1, 2]. However, this may be thwarted by contraindications, drug interactions, hazards from systemic toxicity and, aside from acitretin, they can all promote the development of UV-induced skin cancer.
Topical therapies, e.g. emollients, keratolytics, coal tar, anthralin, analogues of vitamin A and vitamin D, calcineurin inhibitors and corticosteroids, do not have these limitations. They are often used to remove scales that can impair UV penetration into the skin, to clear lesions in areas that cannot be exposed to UV, and for rapid itch relief [3]. However, patients’ adherence is often poor if the formulation stains or it is greasy and smelly or if application takes time; even lower adherence is found when the formulation needs frequent applications, especially when the treatment is prolonged and/or large skin areas are treated [2,3,4].
A recently introduced topical treatment, a super-saturated foam containing a fixed combination of calcipotriene 50 μg/g plus betamethasone 0.5 mg/g (Cal/BD) (Enstilar© foam, Leo Pharma SA, Ballerup, DK) was found to be more effective than foams with the same components used separately [5]. Additionally, in direct comparative studies in patients with mild to moderate psoriasis, the foam was seen to be more effective than the Cal/BD gel [6] and the Cal/BD ointment [7].
Recently, a pooled analysis of three phase II/III studies [6, 8,9,10] has demonstrated that it is also very effective for the treatment of patients with more severe psoriasis (baseline mPASI > 10), with a good proportion of patients achieving mPASI ≤ 1 (20.2%), ≤ 3 (49.2%) and ≤ 5 (63.7%) after 4 weeks [11]. In a matching-adjusted indirect comparison, it was found to be more effective than a few non-biologic systemic drugs, e.g. apremilast, methotrexate or acitretin, and approximately as effective as fumaric acid esters [12].
However, still better results need to be achieved in light of the treatment goals (e.g. PASI 90 or PASI 100 and/ or PASI < 2, DLQI < 2 or PGA clear or almost clear) that are desirable for moderate and severe psoriasis nowadays [1].
The present cross-sectional clinical trial aimed at comparing the therapeutic results of a 12-week treatment cycle with NB-UVB phototherapy versus a combined regimen with a Cal/BD foam that was applied daily before (2 weeks) and in the early phases (2 weeks) of a NB-UVB phototherapy cycle, followed by twice-weekly use on 2 consecutive days for 10 weeks.
Methods
This was a cross-sectional, comparative, open-label study. We enrolled white subjects of either sex, older than 18 years, with a clinical diagnosis of plaque-type psoriasis and with a modified (excluding head) Psoriasis Area and Severity Index (mPASI) > 7. We have excluded the head from the comparison because the Cal/BD foam was not applied on the face and whole-body phototherapy in a NB-UVB cubicle is not effective for hairy scalp psoriasis [13]. Due to safety recommendations for the use of the Cal/BD foam, only patients with < 30% affected body surface area were treated [12]. The mPASI was assessed at baseline (T0) and after 2 (T1) (only in the patients with the combined protocol), 4 (T2), 8 (T3) and 12 (T4) weeks of treatment.
Exclusion criteria were: coexistent psoriatic arthritis, use of photosensitive or immunosuppressive drugs, pregnancy and breast feeding; additionally, systemic treatments for psoriasis were not allowed in the 2 months before the randomization.
Consecutive patients were assigned at a 2:1 rate to two groups: the first group received phototherapy and the second one a combined treatment with once-daily application of Cal/BD foam before (2 weeks) and in the early phase (2 weeks) of phototherapy, followed by twice-weekly use on 2 consecutive days for 8 weeks. The therapies were interrupted before study completion in the case of complete clearance (mPASI90 and/or mPASI < 3) [1] or no or poor response, i.e. disease worsening or an improvement of lower than mPASI75 and/or if an absolute mPASI > 3 was achieved without further amelioration in the subsequent monthly control. These last patients were switched to a systemic treatment for psoriasis. Patients who, at the end of the 12-week treatment cycle, achieved a mPASI improvement of between 75 and 90% and/or an absolute mPASI > 3 but < 6 were considered partial responders and they were switched to oral apremilast or cyclosporine, or they continued with Cal/BD foam alone, according to the clinician’s evaluation. No maintenance phototherapy was given.
Phototherapy was delivered to both groups according to the same treatment protocol [14]. The initial dose ranged between 0.1 and 0.4 J cm−2 according to skin phototype. Patients were treated twice a week, and UV doses were adjusted at each session according to the erythema response. In short: 10%, 5% or no incremental increase was achieved if, respectively, none, a barely perceptible or a well-defined asymptomatic erythema response at 48 h was seen.
The Cal/BD foam was always applied once daily in the evening. Therefore, on the days on which the phototherapy took place, the foam was applied 6–8 h after the UV exposure.
All enrolled patients were included in the full analysis set.
The primary end-point of the present study was the comparison of improvements in psoriatic lesions at 4, 8 and 12 weeks, together with the study of the rate of patients that achieved complete resolution. Statistical analysis was based on the full analysis set (intention to treat). The tested hypothesis was that the sequential regimen was superior to phototherapy in terms of the decrease in the proportion of patients with mPASI90 or mPASI < 3. The secondary end-points were the comparisons of cumulative NB-UVB doses and number of exposures, the intensity of itching, the incidence of adverse effects and patients’ adherence to the treatment protocol.
The radiation source was a Waldmann 7001 cabinet (Waldmann Lichttechnik, Villingen-Schwenningen, Germany) equipped with 40 Philips TL-01/100 W lamps (Philips Eindhoven, Netherlands) with a peak in emission at 312 ± 2 nm. Irradiance was measured with a portable broadband UV meter (Waldmann) after calibration with a Macam SR 9910 spectroradiometer (Macam Photometrics Ltd, Livingston, Scotland).
During the study, patients were allowed to use an emollient cream as needed when they did not apply the Cal/BD foam.
At the monthly medical examinations, patients were asked to assess the severity of itching on a 0–10 numerical rating scale (NRS).
At the end of the treatment cycle, we calculated the number of UV exposures and the cumulative UV dosage.
Throughout the study period, patients were solicited to immediately report any possible adverse event possibly related to Cal/BD foam and/or phototherapy.
The study was conducted in the light of the Declaration of Helsinki and followed a protocol approved by our institutional review board.
All patients received written and verbal information about the clinical trial and signed an informed consent prior to entering the study.
The study was approved by the local ethics committee and registered with the number NP4710.
Statistical Analysis
The IBM Sample Power® software ver. 3.0 and the OpenEpi® software ver. 3.01 were used to calculate the sample size; sampling tests were accepted at the power level 1 − β > = 80%, α = 5%, and two-tailed confidence interval were applied.
The database was formatted through the Microsoft Excel® software and later imported from IBM SPSS® ver. 26.0.1. The use of the Stata® software ver. 15.0 was also considered for any comparisons or implementations of the test output.
Categorical variables are presented as frequencies or percentages and compared with using the chi-square test or Fisher’s exact test, as appropriate. Continuous variables are presented as mean ± SD (in the case of a normal distribution) or median and IQR (in the case of a skewed distribution) and compared using Student’s t test or the Mann–Whitney test. Normality of distributions was assessed using the Kolmogorov–Smirnov test. Differences between two or more groups were evaluated by the Mann–Whitney test or the Kruskal–Wallis test, respectively, and correlations among variables by Pearson’s or Spearman’s rank correlation test.
A two-sided alpha level of 0.05 was used for all tests.
Results
We enrolled 187 consecutive patients who were allocated in a 2:1 ratio to the group treated with NB-UVB phototherapy alone or to the one treated with NB-UVB phototherapy plus Cal/BD.
The main clinical details of the patients enrolled in the two groups are summarized in Table 1. The groups had no statistically significant differences in age, gender, skin phototype, duration of psoriasis and positive family history. At baseline, the median (IQR) mPASI scores of the groups were not different (p = NS): 12 (4; 30.2) in patients treated with NB-UVB alone versus 12.6 (5; 33.2) in patients treated with the combined regimen (Table 1).
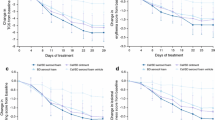
All patients completed the treatment course, and all patients assigned to the combined treatment declared that they fully respected the prescriptive regimen for the application of Cal/BD foam and that the number of days [median (IQR): 5 (0; 8)] throughout the whole treatment cycle on which they did not apply the foam was negligible. Both NB-UVB phototherapy and the combined regimen were effective, with a significant reduction of mPASI at T2 [5.4 (0; 8.6) and 8.5 (0; 30.6), respectively], T3 [2.9 (0; 0.6) and 5.6 (0; 24.0), respectively) and T4 [2.1 (0; 8.2) versus 4.4 (0; 19.6)], in comparison to baseline (always p < 0.001). A box plot of the median (IQR) mPASI at T0, T2, T3 and T4 in the two groups is shown in Fig. 1. In addition, we observed a statistically significant decrease of mPASI after the first 2 weeks (T1) (p < 0.001) of the combined regimen, when patients were treated with the Cal/BD foam only.
Box plot of median (IQR) mPASI at baseline (T0) and after 4 (T2), 8 (T3) and 12 (T4) weeks in the two groups. In both groups, mPASI values at T2, T3 and T4 were always significantly lower (p < 0.001, Mann–Whitney test) in comparison to the baseline mPASI value. The symbol * indicates an outlier, i.e. a data point that is located outside the whiskers of the box
The comparison of the results with the two treatment regimens showed that the decrease of mPASI was always significantly clearer with the combined regimen versus phototherapy alone; this was true at T2 (p < 0.01), T3 (p < 0.01) and also T4 (p < 0.01).
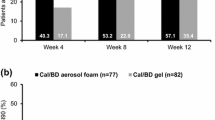
A complete response was seen in 58 (46.8%) patients treated with NB-UVB alone and 47 (74.6%) (p < 0.001) treated with the combined regimen. We also observed that a larger proportion of the patients achieved a quicker complete remission in the group receiving the combined regimen (Fig. 2): these patients showed full resolution as early as 4 (p < 0.05) or 8 (p < 0.01) weeks after the beginning of the treatment (Table 2).
The number of patients who achieved a partial response after 12 weeks was 36 (29%) with phototherapy and 11 (17.5%) with the combined regimen, and this difference was not significantly different. Twenty-nine of these patients continued the Cal/BD foam therapy only, 7 patients began a treatment cycle with apremilast and 5 patients with cyclosporine.
Patients who prematurely interrupted the treatment because of inefficacy or a flare in the first 12 weeks or had a poor response at the end of the treatment cycle were significantly more frequent in the group treated with phototherapy alone: 30 (24.2%) versus 5 (7.9%) (p < 0.001). These patients were switched to adalimumab (12 patients), secukinumab (5 patients), methotrexate (3 patients), cyclosporine (7 patients) or PUVA therapy (8 patients).
The cumulative median UVB dosages [6.1 (5.4; 9.3) J cm−2 versus 13.1 (9.8; 19.7) J cm−2; p < 0.01] and the median (IQR) total number of exposures [12 (4; 20) versus 24 (8; 24); p < 0.01] were significantly lower in the group treated with the combined regimen therapy than in the group treated with phototherapy alone.
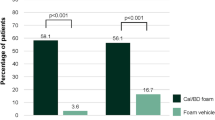
The baseline NRS score for itching was not significantly different between groups [(p = NS)]: 4 (0; 8) in the group treated with phototherapy alone and 4 (0; 8) in the group treated with the combined regimen. With both treatments, itching decreased significantly (always p < 0.01) in comparison to baseline; this happened at all times: at T2 [3 (0; 7)], T3 [2 (0; 4)] and T4 [1 (0; 4)] with phototherapy alone and at T2 [2 (0; 4)], T3 [1 (0; 4)] and T4 [0 (0; 3)] with the combined regimen. In the group treated with the sequential regimen, we also observed a quick improvement in the NRS score for itching; this was already seen at T1: 3 (0; 5) (p < 0.01). The comparison between groups showed that the improvement was superior with the combined regimen at T2 (p < 0.01, T3 (p < 0.01) and T4 (p < 0.01) (Fig. 3).
Nine patients (5 in the group treated only with phototherapy and 4 with the combined regimen) reported a single episode of an excessive phototoxic reaction that was mild and transitory. No patient experienced undesirable effects related to Cal/BD.
Discussion
Under the conditions of the present study, both treatments were significantly effective in comparison to the baseline, but the combined Cal/BD-NBUVB treatment regimen showed superior efficacy in comparison to NB-UVB phototherapy alone, with a higher reduction in the mPASI score and a greater number of complete responders, i.e. patients achieving mPASI90 or mPASI < 3. The improvement was also faster, with better results already seen after 4 and 8 weeks. In addition, the reduction of itching was greater and faster. Finally, the total number of NB-UVB doses and the cumulative number of exposures needed were lower.
The reason for the greater and faster efficacy of the combination regimen remains to be clarified, but a few possible explanations can be taken into account. First of all, Cal/BD can increase the reduction of the overall mPASI because it can improve lesions of skin areas (axillary pillars, natal cleft, groins and the inner part of the thighs) that are normally poorly or not exposed to light due to the three-dimensional conformation of the human body. Additionally, the skin from the knee down is exposed to a lower UV dose because of the uneven emission along the vertical axis of cabinets equipped with fluorescent tubes [15]. Second, Cal/BD can decrease the thickness of the plaques by removing scales and reducing the dermal inflammation, thus facilitating the penetration of NB-UVB into the epidermis and superficial dermis. Finally, calcipotriene, betamethasone dipropionate and phototherapy activate biological mechanisms in immune cells and keratinocytes in different molecular ways, leading to distinct and complementary effects, and they have overlapping and mutually empowering effects [16,17,18,19].
Vitamin D analogues inhibit epidermal hyperproliferation, induce keratinocyte differentiation, restore epidermal barrier function and have immunomodulatory properties that contribute to increasing Tregs, increasing the release of inhibitory cytokines such as interleukin (IL)-10, and reducing Th17 cells [15], whereas corticosteroids act primarily as immunosuppressors, targeting pro-inflammatory cytokines and chemokines, promoting keratinocyte differentiation, and mainly blocking DNA transcription [19].
The anti-psoriatic activity of phototherapy is mediated by a number of immune mechanisms, including suppression of the Th1/Th17 inflammatory axis, reduction of Langerhans cells, increasing circulating and dermal Tregs [16] and up-regulation of the Th2 pathway [20].
Phototherapy also has a strong effect on keratinocytes, inducing apoptosis, cell-cycle arrest and cell differentiation [20].
The earlier and more intense effects of the combined protocol in relieving itching seem to demonstrate that the activities of calcipotriene, betamethasone [21] and phototherapy [22] on itch pathways are additional and therefore do not hinder each other.
Adherence to the treatment schedule can be a challenge when choosing a combination regimen that requires greater patient commitment and usability. In our study, however, adherence was very good, with no patients dropping out and a negligible number of skipped treatments. This positive finding could be related to a combination of factors [3, 23]: in particular, at the beginning of the treatment, the schedule was agreed with the patient, and the short-term and predetermined duration of the application of the foam (daily for 4 weeks and then twice weekly for 8 weeks) was greatly appreciated, as was the rapidity and the degree of improvement of both clinical manifestations and itching. Other important factors in the improvement of compliance were the pleasantness and the tolerability of the formulation of the Cal/BD foam [6, 10].
Under the conditions of the present treatment protocol, the combination with Cal/BD foam was well tolerated without significant acute adverse effects. However, the major concern with NB-UVB is long-term adverse effects, and in particular skin photoageing and carcinogenesis, although the magnitude of this risk, if any, has not been demonstrated so far. However, the Cal/BD combination does not seem to enhance this risk because it has no carcinogenic [24] or photocarcinogenic [25] activities. Indeed, we can hypothesize that the combined protocol could reduce these theoretical risks, because the therapeutic result was achieved with a lower NB-UVB cumulative dose and fewer exposures.
The application of an adjunctive therapy with Cal/BD foam according to the therapeutic regimen that we have used (once-daily Cal/BD foam for 4 weeks, followed by twice-weekly use on consecutive days for 12 weeks) is not new in dermatology, since it was already known to be successful in patients with inadequate response to biologics [26].
In a previous pilot study of 7 patients, the twice-daily application of a Cal/BD ointment plus UVB phototherapy was highly effective [27]. However, it was not a comparative study with UVB alone. In addition, we emphasize that the Cal/BD ointment is less effective than the Cal/BD foam [7, 28], and it has several other disadvantages for the patients, e.g. two applications per day of an ointment is time consuming, and the greasy formulation is often unacceptable [7, 28].
In several other previous studies, the combination of a cream or an ointment containing calcipotriene alone with NB-UVB phototherapy has been investigated. A few studies reported a faster and more complete clinical response, as well as a UVB-sparing effect. However, a few other studies have not found significant differences, or have only found a numerical advantage in terms of the efficacy rate (e.g. PASI score for lesion clearance, etc.) [2].
A main limitation of the present and all previous studies of combination protocols of NB-UVB and topical vitamin D derivatives with or without topical corticosteroids is the short duration of the protocol and follow-up, and therefore it remains unknown if they can be useful for maintenance of remission in patients with moderate to severe psoriasis vulgaris.
Conclusions
The combined Cal/BD-NBUVB therapy could represent an innovative treatment strategy that can clear or almost clear the majority of the lesions in patients with moderate to severe psoriasis vulgaris. Efficacy was superior to NB-UVB phototherapy alone, and the treatment protocol was well tolerated with very good adherence by patients. Given that the efficacy was very high, with 74.6% of patients achieving a complete remission (mPASI90 or absolute mPASI < 3), this simple treatment regimen could represent a valuable alternative to systemic therapies for patients who have contraindications to, are intolerant of, or were resistant to biologics and other disease-modifying antirheumatic drugs. Finally, this treatment protocol could also be useful for improving treatment results of phototherapy of vitiligo, as was suggested by a small recent comparative study in which the combination of topical Cal, topical BD and NB-UVB phototherapy was significantly more effective than NB-UVB phototherapy alone [29].
References
Nast A, Spuls PI, van der Kraaij G, et al. European S3-Guideline on the systemic treatment of psoriasis vulgaris—update apremilast and secukinumab—EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol JEADV. 2017;31:1951–63.
Bagel J, Gold LS. Combining topical psoriasis treatment to enhance systemic and phototherapy: a review of the literature. J Drugs Dermatol. 2017;16(12):1209–22.
Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;86(3 Suppl):5–32.
Svendsen MT, Jeyabalan J, Andersen KE, Andersen F, Johannessen H. Worldwide utilization of topical remedies in treatment of psoriasis: a systematic review. J Dermatolog Treat. 2017;28(5):374–83.
Lebwohl M, Tyring S, Bukhalo M, et al. Fixed combination aerosol foam calcipotriene 0.005% (Cal) plus betamethasone dipropionate 0.064% (BD) is more efficacious than Cal or BD aerosol foam alone for psoriasis vulgaris: a randomized, double-blind, multicenter, three-arm, phase 2 study. J Clin Aesthet Dermatol. 2016;9(2):34–41.
Paul C, Stein Gold L, Cambazard F, et al. Calcipotriol plus betamethasone dipropionate aerosol foam provides superior efficacy vs. gel in patients with psoriasis vulgaris: randomized, controlled PSO-ABLE study. J Eur Acad Dermatol Venereol. 2017;31(1):119–26.
Koo J, Tyring S, Werschler WP, et al. Superior efficacy of calcipotriene and betamethasone dipropionate aerosol foam versus ointment in patients with psoriasis vulgaris—a randomized phase II study. J Dermatol Treat. 2016;27(2):120–7.
Leonardi C, Bagel J, Yamauchi P, et al. Efficacy and safety of calcipotriene plus betamethasone dipropionate aerosol foam in patients with psoriasis vulgaris—a randomized phase III study (PSO-FAST). J Drugs Dermatol. 2015;14(12):1468–77.
Leonardi C, Bagel J, Yamauchi P, et al. The aerosol foam formulation of the fixed combination calcipotriene plus betamethasone dipropionate improves the health-related quality of life in patients with psoriasis vulgaris: results from the randomized PSO-FAST study. J Drugs Dermatol. 2016;15(8):981–7.
Thaçi D, Ortonne JP, Chimenti S, et al. A phase IIIb, multicentre, randomized, double-blind, vehicle-controlled study of the efficacy and safety of adalimumab with and without calcipotriol/betamethasone topical treatment in patients with moderate to severe psoriasis: the BELIEVE study. Br J Dermatol. 2010;163(2):402–11.
Pink AE, Jalili A, Berg P, et al. Rapid onset of action of calcipotriol/betamethasone dipropionate cutaneous foam in psoriasis, even in patients with more severe disease. J Eur Acad Dermatol Venereol. 2019;33(6):1116–23.
Bewley AP, Shear NH, Calzavara-Pinton PG, Hansen JB, Nyeland ME, Signorovitch J. Calcipotriol plus betamethasone dipropionate aerosol foam vs. apremilast, methotrexate, acitretin or fumaric acid esters for the treatment of plaque psoriasis: a matching-adjusted indirect comparison. J Eur Acad Dermatol Venereol. 2019;33(6):1107–15.
Paul C, Leonardi C, Menter A, Reich K, et al. Calcipotriol plus betamethasone dipropionate aerosol foam in patients with moderate-to-severe psoriasis: sub-group analysis of the PSO-ABLE study. Am J Clin Dermatol. 2017;18(3):405–11. https://doi.org/10.1007/s40257-017-0258-0.
Wainwright NJ, Dawe RS, Ferguson J. Narrowband ultraviolet B (TL-01) phototherapy for psoriasis: which incremental regimen? Br J Dermatol. 1998;139(3):410–4.
Calzavara-Pinton PG. Efficacy and safety of stand-up irradiation cubicles with UVA metal-halide lamps (and a new filter) or UVA fluorescent lamps for photochemotherapy of psoriasis. Dermatology. 1997;195(3):243–7.
Kotb IS, Lewis BJ, Barker RN, Ormerod AD. Differential effects of phototherapy, adalimumab and betamethasone-calcipotriol on effector and regulatory T cells in psoriasis. Br J Dermatol. 2018;179(1):127–35.
Kubin ME, Kokkonen N, Palatsi R, et al. Clinical efficiency of topical calcipotriol/betamethasone treatment in psoriasis relies on suppression of the inflammatory TNFα - IL-23 - IL-17 axis. Acta Derm Venereol. 2017;97(4):449–55.
Keijsers RR, Joosten I, Hendriks AG, Koenen HJ, van Erp PE, van de Kerkhof PC. Balance of Treg versus T-effector cells during systemic treatment with adalimumab and topical treatment with calcipotriol-betamethasone dipropionate ointment. Exp Dermatol. 2015;24(1):65–7.
Segaert S, Ropke M. The biological rationale for use of vitamin D analogs in combination with corticosteroids for the topical treatment of plaque psoriasis. J Drugs Dermatol. 2013;12(8):e129–37.
Yu Z, Wolf P. How it works: the immunology underlying phototherapy. Dermatol Clin. 2020;38(1):37–53.
Jalili A, Lebwohl M, Stein Gold L, et al. Itch relief in patients with psoriasis: effectiveness of calcipotriol plus betamethasone dipropionate foam. J Eur Acad Dermatol Venereol. 2019;33(4):709–17.
Théréné C, Brenaut E, Barnetche T, Misery L. Efficacy of systemic treatments of psoriasis on pruritus: a systemic literature review and meta-analysis. J Invest Dermatol. 2018;138(1):38–45.
Hong CH, Papp KA, Lophaven KW, Skallerup P, Philipp S. Patients with psoriasis have different preferences for topical therapy, highlighting the importance of individualized treatment approaches: randomized phase IIIb PSO-INSIGHTFUL study. J Eur Acad Dermatol Venereol. 2017;31(11):1876–83.
Drugs.com. Enstilar. https://www.drugs.com/pro/enstilar.html. Accessed May 26, 2020.
Lerche CM, Philipsen PA, Poulsen T, Wulf HC. Topical hydrocortisone, clobetasol propionate, and calcipotriol do not increase photocarcinogenesis induced by simulated solar irradiation in hairless mice. Exp Dermatol. 2010;19(11):973–9.
Bagel J, Zapata J, Nelson E. A prospective, open-label study evaluating adjunctive calcipotriene 0.005%/betamethasone dipropionate 0.064% foam in psoriasis patients with inadequate response to biologic therapy. J Drugs Dermatol. 2018;17(8):845–50.
Rogers C. Calcipotriol (Dovobet) ointment in combination with UVB therapy for psoriasis treatment. Dermatol Nurs. 2006;18(3):258–61.
Amat-Samaranch V, Puig L. Safety of calcipotriene and betamethasone dipropionate foam for the treatment of psoriasis. Expert Opin Drug Saf. 2020;19(4):423–32.
Akdeniz N, Yavuz IH, Bilgili SG, Yavuz GO, Calka O. Comparison of efficacy of narrow band UVB therapies with UVB alone, in combination with calcipotriol, and with betamethasone and calcipotriol in vitiligo. J Dermatol Treat. 2014;25(3):196–9.
Acknowledgements
Funding
No funding for the study and publication was requested and received.
Authorship
All named authors (Gaetano Licata, Mariachiara Arisi, Marina Venturini, Mariateresa Rossi, Cesare Tomasi, Irene Calzavara-Pinton, Piergiacomo Calzavara-Pinton) contributed equally to study conception and design, material preparation, data collection and analysis, and to writing and editing the manuscript. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed equally to the concept and design, statistical analysis and the drafting of the manuscript.
Disclosures
Piergiacomo Calzavara-Pinton was a consultant for Sanofi, Abbvie, Jannsen, Leo, Galderma, Novartis and Cantabria; Marina Venturini was a consultant for Novartis, UCB and AbbVie; Mariateresa Rossi was a consultant for Sanofi; Gaetano Licata, Mariachiara Arisi, Cesare Tomasi and Irene Calzavara-Pinton declare that they have no competing interests.
Compliance with Ethics Guidelines
The study was approved by the local ethics committee of the ASST-Spedali Civili di Brescia and registered with the number NP4710. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. The patients in this manuscript gave their written informed consent to participate and for the publication of their case details.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Licata, G., Arisi, M., Venturini, M. et al. Pretreatment with an Aerosol Foam Containing Calcipotriene and Betamethasone Strongly Improves the Efficacy of Narrow-Band UVB Phototherapy. Dermatol Ther (Heidelb) 12, 2161–2171 (2022). https://doi.org/10.1007/s13555-022-00792-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00792-0