Abstract
Introduction
Actinic cheilitis (AC) is the biologic precursor of invasive squamous cell carcinoma (SCC) of the vermilion, and different treatment options have been investigated, but their efficacy is hampered by local inflammation, pain and slow recovery. Daylight photodynamic therapy (dl-PDT) has been demonstrated to represent a valuable treatment option for AC, but its feasibility is limited by weather conditions and latitude.
Methods
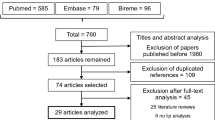
Our study proposed to compare the efficacy and tolerability of conventional photodynamic therapy (c-PDT) and indoor daylight photodynamic therapy (idl-PDT) with a white LED lamp for the treatment of AC. Sixteen patients were enrolled in the study: 8 (50%) treated with c-PDT and 8 (50%) treated with idl-PDT. All patients completed the study protocol.
Results
Both idl-PDT and c-PDT were demonstrated to be highly effective in terms of reduction of the cumulative lesional area and severity of the clinical score. Neither treatment was inferior to the other. The inflammatory reaction and the pain scores were milder with idl-PDT, whereas the cosmetic outcome was not different.
Conclusion
The present findings confirm that idl-PDT can represent a valid therapeutic strategy for AC patients as well, despite the procedural difficulties and the risk of poor tolerability related to the body site.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Actinic cheilitis (AC) represents a therapeutic challenge. |
This study compared two treatments for AC: conventional photodynamic therapy (c-PDT) and indoor-daylight-photodynamic therapy (idl-PDT). |
Photodynamic therapy (PDT) is based on the activation of a photosensitizing drug by irradiation with light to cause a selective cytotoxic damage on the skin. c-PDT is performed with a red light, while idl-PDT with a white LED lamp. |
Our investigation demonstrated that idl-PDT is a valuable alternative to c-PDT in AC treatment with better tolerability and not-inferior efficacy. |
Introduction
Actinic cheilitis (AC) is the biologic precursor of invasive squamous cell carcinoma (SCC) of the vermilion, and its development and progression are related to the progressive accumulation of ultraviolet (UV)-related genotoxic damage [1,2,3,4].
The estimated rate of progression to SCC ranges from 10% to 30% [5], and there are no clinical features that allow for the prediction of which AC will progress. Therefore, treatment of all lesions is recommended regardless of clinical features.
Topical drug treatments containing 5-fluorouracil (FU), imiquimod (IMI), diclofenac (DCF), methyl aminolevulinate (MAL) and aminolevulinic acid (ALA), as well as chemical peels and surgical options, (e.g. dermabrasion, cryotherapy, electrosurgery, Er: YAG laser, CO2 laser, conventional surgical vermilionectomy and Mohs micrographic surgery) have been investigated, with variable treatment results [6,7,8].
Unfortunately, efficacy is hampered by the difficulty in managing treatments in this anatomical area: inflammatory reactions are frequent and severe and the recovery is often slow and painful.
In addition, these treatment options have been investigated in small non-randomized and in a few comparative clinical trials or retrospective studies; thus guidelines for AC treatment are not available so far [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
In comparison with other drug treatments, photodynamic therapy (PDT) with ALA or MAL [11,12,13, 16, 17, 20, 21] has the advantage of being delivered in one or two sessions, thus lowering the duration of the post-intervention inflammatory reaction of the lips that is often difficult to manage by patients. When it is delivered according to the conventional protocol (c-PDT) with red light exposure from a LED lamp after 3 h of application of the sensitizer [10,11,12,13,14, 17, 20, 21, 25], the clearance rates are high [10, 13, 15, 16, 18, 19, 21,22,23] but adverse effects, such as intense pain, stinging and burning sensations are frequent.
Daylight PDT (dl-PDT) has been demonstrated to represent a valuable treatment option with similar efficacy to and less pain and inflammation than c-PDT [9, 15, 19, 22,23,24], although comparative studies are not available so far. In this setting, the MAL or ALA cream is applied without occlusion for 30 min and then the lip is exposed to direct or indirect solar radiation for 2 h [26].
However, the light dose cannot be standardized because it varies with latitude, altitude, season and hour of the day. Moreover, the treatment session cannot take place in the case of dark clouds, rain, strong wind and low (10 °C) or high temperatures, causing the need for patients to be rescheduled with a subsequent appointment [27, 28].
Indoor dl-PDT (idl-PDT) is a new PDT treatment protocol that differs from dl-PDT only because the patient is treated indoors with exposure to an artificial broadband white light source instead of outdoors with natural daylight [26]. The advantages are the delivery of a standard light dose and the avoidance of environmental variability [26, 29,30,31].
The present randomized comparative clinical trial aimed to compare treatment outcomes of c-PDT and idl-PDT with a new polychromatic white light lamp for AC.
Methods
Patients
Inclusion Criteria
The study included males or females 18 years of age or older affected by AC of the lip vermilion confirmed by histology.
Exclusion Criteria
The exclusion criteria were: congenital and acquired photosensitive disorders; immunosuppression due to idiopathic, disease-specific or therapeutic reasons; known allergy to MAL, ALA or excipients of the cream; history of hypersensitivity to nut products or other known protein antigens; participation in other clinical studies either currently or within the last 30 days; local treatment (both medical or surgical) for AC within the last 3 months; pregnant or breast-feeding women; any conditions that may be associated with a risk of poor protocol compliance.
The study was held at the Dermatologic Department of the University of Brescia from January 2019 to March 2021 in accordance with the Declaration of Helsinki and was approved by the Local Ethics Committee (protocol no. 3718). All patients were given verbal and written information on the nature of the study, and they signed an informed consent form before enrolment.
Irradiation Units
Two light sources based on LED technology were used: a lamp (Aktilite CL128, Photocure ASA, Oslo, Norway) with output confined in the red waveband (630 ± 5 nm) and a polychromatic white LED lamp (400–700 nm) (Dermaris, Surgiris, Croix, France).
The emission spectra of the two light sources were measured with a SR 9910 spectroradiometer (Macam Photometrics Ltd, Livingston, UK).
Irradiances at working distances (8 cm for c-PDT and 30 cm for iDL-PDT) were 775 W m−2 for the red lamp and 72.6 W m−2 for the white one.
According to the treatment protocols recommended by the producers, the skin was exposed for 8 min with c-PDT and 120 min with idl-PDT. Therefore, the light doses were 37 J cm−2 for c-PDT and 52.3 J cm−2 for idl-PDT and the effective light doses for PpIX photoactivation were 0.86 Jeff cm−2 with c-PDT and 1.39 Jeff cm−2 with idl-PDT. The effective light dose was calculated with the normalized PpIX absorption spectrum [32], the spectral irradiance of the lamps and treatment time.
Treatment Procedure
At baseline (T0), randomization with a 1:1 allocation ratio to the treatment options was done by phone with a computer-generated list using random permuted blocks of four to ensure concealment of allocation. Patients and treating physicians were not blinded to group assignment.
With both protocols, the treated skin area was prepared with a mildly abrasive pad to remove scales and crusts and to roughen the surface of the AKs before application of a 1-mm-thick layer of cream containing 160 mg MAL g-1 (Metvix; Galderma SA, Lausanne; Switzwerland).
A cotton roll was placed in the internal part of the lower lip to make the vermilion more everted and the treated area more exposed.
The treatment with the white LED lamp was delivered according to the dl-PDT treatment protocol [33]: the treated area was not covered with an occlusive medication and the light exposure began after 30 min and lasted 2 h.
Red LED lamp treatment (c-PDT) was delivered according to the protocol approved by the European Medicines Agency [34]. The skin area was covered with an occlusive and light-shielding dressing (Tegaderm; 3M Italia, Milan, Italy) and an opaque adhesive tape (Hypafix; BSN Medical, Milan, Italy) for 3 h and then irradiated with the red light LED lamp.
A follow-up examination took place after 3 months from the end of treatment (EOT) (T1). Patients with incomplete response underwent a second treatment with the preferred treatment option.
Clinical Assessment
At baseline (T0), two performance indexes on each treated area were separately assessed by two investigators (G.L.R., E.G.P) blinded to treatment assignment: (1) the AC’s cumulative area (cm2) calculated on the basis of analysis (Vectra Viewer software®, Canfield, Fairfield, NJ, USA) of 3D (Vectra H1 camera, Canfield, Fairfield, NJ, USA) and 2D digital pictures (ImageJ, US National Institutes of Health, Bethesda, MD, USA) [35]; (2) the clinical severity score ranging on a scale of 0 to 3 (with higher numbers indicating greater severity) of the following parameters: dyschromia, atrophy, erythema, dryness, scales/hyperkeratosis, crusts, erosions/fissures, and infiltration (maximum total score 24). [19]
Soon after the exposures, patients self-rated pain and/or burning sensation on a standardised 1–10 visual analogue scale (VAS).
After 3 months (T1), the same two investigators (G.L.R., E.G.P.) who were blinded to treatment assignment evaluated the clinical response and calculated AC’s cumulative area and severity score. Dermoscopic investigation was performed as a confirmation at both timepoints.
The percentage of reduction of AC’s area from baseline was assessed: patients with reduction > 65% were considered complete responders.
Cosmetic outcome was assessed by a distinct investigator (MTR) who was blinded at the initial treatment allocation. It was graded into one of four categories: excellent (no or mild redness or change in skin pigmentation), good (moderate redness or change in skin pigmentation), fair (slight-to-moderate scarring, atrophy or induration) and poor (extensive scarring, atrophy or induration) [36].
Statistical Analysis
Statistical analysis was carried out using the SPSS (version 25.0; IBM SPSS, Armonk, NY, USA) software program.
Normal distribution of collected data was analysed by the Kolmogorov–Smirnov test.
Categorical variables were summarized by using percentages and continuous variables by calculating medians and range (minimum and maximum values).
Continuous variables were compared by using the Wilcoxon test.
Chi-square test was used for percentages comparison.
To compare the efficacy of the two treatments, a non-inferiority margin of 15% was set.
Linear regression was used to identify any patients’ clinical and demographic characteristics as possible predictive factors of treatment response.
All results were considered statistically significant at the p ≤ 0.05 level.
Results
Sixteen patients were enrolled in the study: 8 (50%) treated with c-PDT and 8 (50%) treated with idl-PDT. All patients completed the study protocol. The main clinical details are presented in Table 1.
The Kolmogorov–Smirnov test showed that the population was not normally distributed (p < 0.05).
The median (range) individual cumulative area of treated AC was 3.21 (3.11–3.90) cm2 with c-PDT and 3.18 (3.10–3.91) cm2 with idl-PDT (p = 0.71) (Fig. 1a). The median individual severity score was 7.5 (6–9) cm2 with c-PDT and 6.5 (5–8) cm2 with idl-PDT (p = 0.05), (Fig. 1b).
The total AC area and the severity score reduced significantly after both idl-PDT (p < 0.0001 and p = 0.02, respectively) and c-PDT (p < 0.0001 and p = 0.01, respectively) (Fig. 2).
To compare the efficacy of the two treatment modalities, the variations (ΔT0 − T1) of AC area and severity score were assessed. No significant differences were found (p = 0.96 each; Figs. 3a, b, 4)
Difference of ratios of responder patients who achieved a reduction in AC cumulative area of at least 65% (100% with idl-PDT and 87% with c-PDT) was non-inferior to 95% [Confidence Interval (CI) from −19 to −6], far below the pre-defined non-inferiority margin of 15%.
c-PDT was more painful [VAS: 4 (0–10) with c-PDT versus 0 (0–1) with idl-PDT (p < 0.0001)].
Patients did not report any other local or systemic adverse event after the two procedures.
The cosmetic outcome was not different at a statistical level of significance (p = 0.16). It was rated as excellent in five (62.5%) patients treated with idl-PDT and in two (25%) patients treated with c-PDT; good in two (25%) patients treated with idl-PDT and in three (37.5%) patients treated with c-PDT; fair in one patient treated with idl-PDT (12.5%) and three patients treated with c-PDT (37.5%).
The analysis of patients’ clinical and demographic characteristics (age, sex and clinical score at baseline) by linear regression as possible predictive factors of treatment response showed no influence on AC area reduction or clinical score reduction after each treatment (p > 0.05 for each variable analysed).
Discussion
This was the first randomized comparative non-inferiority clinical study of c-PDT with a red LED lamp versus idl-PDT with a polychromatic white LED lamp for AC, and we found that both idl-PDT and c-PDT were highly effective as measured by the reductions of the cumulative lesional area and the severity of the clinical score and that neither treatment was inferior.
The inflammatory reaction and pain scores were milder with idl-PDT, whereas the cosmetic outcome was not different.
The different kinetics of photochemical and photobiological reactions in keratinocytes can explain these differences. During idl-PDT, skin is irradiated with a low irradiance of white light for a long time, thus inflammation is mild because the low amount of porphyrins that is synthesized by cells after the initial 30 min of application and additional porphyrins that are synthesized during the 2 h of incubation are progressively photobleached; meanwhile, in c-PDT, a large amount of accumulated porphyrin during the 3 h of occlusive medication is abruptly photosensitized in 8 min [29]. Furthermore, unlike white light, red light allows a better activation of porphyrins that are in the deeper level of the epidermis. These photobiological differences strongly influenced the intensity of pain and inflammatory skin reactions but not the efficacy in the treatment of a superficial lesion such as AC.
A total of 17 uncontrolled pilot studies with c-PDT (5 with MAL [12, 16,17,18, 20], 5 with ALA-conventional PDT [10, 13, 14, 21, 25] and another with methyl aminoxo pentanoate [11]) and outdoor dl-PDT (6 with MAL [9, 15, 18, 19, 22,23,24]) for the treatment of AC were previously reported, and their main results are summarized in Table 2. Efficacy ranged from 62.7% [17] to 100% [9, 10, 12, 15] of patients with complete remission, and a good or excellent cosmetic outcome ranging from 33% [11] to 100% [10, 16] of treated patients, and differences cannot be apparently explained on the basis of the sensitizer (MAL or ALA), treatment modality (idl-PDT or c-PDT), number of sessions (ranging from one to six), interval between session (1 or 2 weeks), and location of AC (upper or lower lip) (Table 2).
Tolerability was low with dl-PDT and strong with c-PDT, although broad differences were found between studies that used the same treatment modality.
An additional three studies compared the effectiveness, safety and tolerability of c-PDT with excimer-dye laser [25], long-pulsed pulsed dye laser (LP PDL) (595 nm) [37] and erbium:yttrium-aluminium-garnet ablative fractional laser [38] as the light source [25, 37, 38]. All studies reported successful results, but the advantages, if any, of red LED light remain to be established. In an uncontrolled study, sequential treatment with c-PDT and IMI 5% cream was successful in 80% of patients after 1 year [39] but it also increased the degree and duration of inflammation, pain and discomfort for the patient.
The efficacy and safety of idl-PDT with different light sources were previously investigated in patients with actinic keratosis of the face and scalp.
A retrospective non-randomized and non-controlled study paired illumination sources mimicking the green and red components of daylight installed on the ceiling of a treatment room (Indoorlux System, Swiss Red Ag, Murten, Switzerland) [31]. The treatment was conducted in 32 patients affected by superficial (Olsen grade I–II) actinic keratosis using a nanoemulsion‐based gel formulation containing 10% ALA hydrochloride. The complete lesion clearance rate at 3 months follow-up was 93%, and the mean VAS score after 30 min 0.1 ± 0.4 [31].
In a following randomized comparative study [40], a single session of idl-MAL-PDT with four xenon H4 light bulbs (DBU Dansk Biludstyr A/S, Aarhus, Denmark) with a colour temperature of 6000 K was better tolerated than c-MAL-PDT, but was found to be less effective: 51.5% versus 62.7% of CR of superficial (Olsen I and II) actinic keratosis.
In a randomized trial [41] comparing the efficacy and safety of outdoor dl-MAL-PDT and idl-PDT with an operating-room LED light source with a white output for the treatment of actinic keratosis regardless of their clinical thickness, no significant difference of efficacy with the two treatments at 1-, 3- and 6-month follow-up examinations was found. The median number and percentage reductions in AKs per field were 52.3% for dl-PDT and 58% for idl-PDT at 3 months (p = 0.29). Pain and inflammatory reactions were mild with both treatments, without significant differences.
A recent randomized split-face controlled study from our department has compared the effectiveness, tolerability and patient preference of c-PDT and idl-PDT with a white LED lamp (Dermaris, Surgiris, Croix, France) for grade I–II AKs of the face and scalp [26]. The study showed the lack of inferiority and the better tolerability of idl-PDT compared with c-PDT, with the former being found to be the preferred treatment for patients.
The present trial investigated the treatment of AC according to the same protocol that was used for the treatment of actinic keratosis [26].
The present findings confirm that idl-PDT can represent a valid therapeutic strategy for AC patients as well, despite the procedural difficulties and the risk of poor tolerability related to the body site.
However, this study presents some limitations. First, it was blinded only for the investigator, who assessed treatment results, and not for patients and other physicians. Second, the follow-up was rather short term, and therefore we could not evaluate late relapses and whether they effectively reduce or eliminate the risk of progression towards invasive SCC. Third, we have compared results obtained with a single treatment cycle. However, we can hypothesize a better result with two sessions, as was demonstrated with both c-PDT and DL-PDT of actinic keratosis [34, 42]. Lastly, the sample size of the study is limited to only 16 patients, which is to be considered preliminary for future studies on wider cases.
Conclusions
The present investigation demonstrated that idl-PDT is a valuable alternative to c-PDT in AC treatment, with better tolerability and lack of inferior efficacy. In addition, it seems to present practical advantages in comparison with outdoor dl-PDT because the spectrum and light dose are fixed and reproducible and it is always feasible and programmable regardless of weather and environmental problems.
References
de Visscher JG, van der Waal I. Etiology of cancer of the lip. A review. Int J Oral Maxillofac Surg. 1998;27(3):199–203.
Markopoulos A, Albanidou-Farmaki E, Kayavis I. Actinic cheilitis: clinical and pathologic characteristics in 65 cases. Oral Dis. 2004;10(4):212–6.
Vieira RA, Minicucci EM, Marques ME, Marques SA. Actinic cheilitis and squamous cell carcinoma of the lip: clinical, histopathological and immunogenetic aspects. An Bras Dermatol. 2012;87(1):105–14.
Jadotte YT, Schwartz RA. Solar cheilosis: an ominous precursor: part I. Diagnostic insights. J Am Acad Dermatol. 2012;66(2):173–84. quiz 185–6.
Lopes ML, Silva Júnior FL, Lima KC, Oliveira PT, Silveira ÉJ. Clinicopathological profile and management of 161 cases of actinic cheilitis. An Bras Dermatol. 2015;90(4):505–12.
Varela-Centelles P, Seoane-Romero J, García-Pola MJ, Leira-Feijoo Y, Seoane-Romero JM. Therapeutic approaches for actinic cheilitis: therapeutic efficacy and malignant transformation after treatment. Int J Oral Maxillofac Surg. 2020;49(10):1343–50.
Salgueiro AP, de Jesus LH, de Souza IF, Rados PV, Visioli F. Treatment of actinic cheilitis: a systematic review. Clin Oral Investig. 2019;23(5):2041–53.
Lai M, Pampena R, Cornacchia L, Pellacani G, Peris K, Longo C. Treatments of actinic cheilitis: a systematic review of the literature. J Am Acad Dermatol. 2020;83(3):876–87.
Stender IM, Wulf HC. Photodynamic therapy with 5-aminolevulinic acid in the treatment of actinic cheilitis. Br J Dermatol. 1996;135(3):454–6.
Hauschild A, Lischner S, Lange-Asschenfeldt B, Egberts F. Treatment of actinic cheilitis using photodynamic therapy with methyl aminolevulinate: report of three cases. Dermatol Surg. 2005;31(10):1344–7. discussion 1348.
Berking C, Herzinger T, Flaig MJ, Brenner M, Borelli C, Degitz K. The efficacy of photodynamic therapy in actinic cheilitis of the lower lip: a prospective study of 15 patients. Dermatol Surg. 2007;33(7):825–30.
Rossi R, Assad GB, Buggiani G, Lotti T. Photodynamic therapy: treatment of choice for actinic cheilitis? Dermatol Ther. 2008;21(5):412–5.
Sotiriou E, Apalla Z, Koussidou-Erremonti T, Ioannides D. Actinic cheilitis treated with one cycle of 5-aminolaevulinic acid-based photodynamic therapy: report of 10 cases. Br J Dermatol. 2008;159(1):261–2.
Sotiriou E, Apalla Z, Chovarda E, Panagiotidou D, Ioannides D. Photodynamic therapy with 5-aminolevulinic acid in actinic cheilitis: an 18-month clinical and histological follow-up. J Eur Acad Dermatol Venereol. 2010;24(8):916–20.
Levi A, Wulf HC, Enk CD. Two cases of actinic cheilitis responsive to daylight-activated photodynamic therapy (DA-PDT). Photodermatol Photoimmunol Photomed. 2013;29(5):268–71.
Fai D, Romano I, Cassano N, Vena GA. Methyl-aminolevulinate photodynamic therapy for the treatment of actinic cheilitis: a retrospective evaluation of 29 patients. G Ital Dermatol Venereol. 2012;147(1):99–101 (PMID: 22370573).
Calzavara-Pinton PG, Rossi MT, Sala R; Italian Group For Photodynamic Therapy. A retrospective analysis of real-life practice of off-label photodynamic therapy using methyl aminolevulinate (MAL-PDT) in 20 Italian dermatology departments. Part 2: oncologic and infectious indications. Photochem Photobiol Sci. 2013;12(1):158–65.
Suárez-Pérez JA, López-Navarro N, Herrera-Acosta E, Aguilera J, Gallego E, Bosch R, Herrera E. Treatment of actinic cheilitis with methyl aminolevulinate photodynamic therapy and light fractionation: a prospective study of 10 patients. Eur J Dermatol. 2015;25(6):623–4.
Fai D, Romanello E, Brumana MB, Fai C, Vena GA, Cassano N, Piaserico S. Daylight photodynamic therapy with methyl-aminolevulinate for the treatment of actinic cheilitis. Dermatol Ther. 2015;28(6):355–68.
Chaves YN, Torezan LA, Lourenço SV, Neto CF. Evaluation of the efficacy of photodynamic therapy for the treatment of actinic cheilitis. Photodermatol Photoimmunol Photomed. 2017;33(1):14–21.
Radakovic S, Tanew A. 5-aminolaevulinic acid patch-photodynamic therapy in the treatment of actinic cheilitis. Photodermatol Photoimmunol Photomed. 2017;33(6):306–10.
Levi A, Hodak E, Enk CD, Snast I, Slodownik D, Lapidoth M. Daylight photodynamic therapy for the treatment of actinic cheilitis. Photodermatol Photoimmunol Photomed. 2019;35(1):11–6.
Andreadis D, Pavlou A, Vakirlis E, Anagnostou E, Vrani F, Poulopoulos A, Kolokotronis A, Ioannidis D, Sotiriou E. Daylight photodynamic therapy for the management of actinic cheilitis. Arch Dermatol Res. 2020;312(10):731–737
Martín-Carrasco P, Sendín-Martín M, Domínguez-Cruz JJ, Bernabeu-Wittel J. Actinic cheilitis treated with daylight photodynamic therapy. Actas Dermosifiliogr (Engl Ed). 2020;111(10):883–885. English, Spanish.
Kodama M, Watanabe D, Akita Y, Tamada Y, Matsumoto Y. Photodynamic therapy for the treatment of actinic cheilitis. Photodermatol Photoimmunol Photomed. 2007;23(5):209–10.
Arisi M, Rossi MT, Spiazzi L, Guasco Pisani E, Venturuzzo A, Rovati C, Tomasi C, Venturini M, Calzavara-Pinton PG. A randomized split-face clinical trial of conventional vs indoor-daylight photodynamic therapy for the treatment of multiple actinic keratosis of the face and scalp and photoaging. J Dermatolog Treat. 2021;28:1–7.
Morton CA, Wulf HC, Szeimies RM, Gilaberte Y, Basset-Seguin N, Sotiriou E, Piaserico S, Hunger RE, Baharlou S, Sidoroff A, Braathen LR. Practical approach to the use of daylight photodynamic therapy with topical methyl aminolevulinate for actinic keratosis: a European consensus. J Eur Acad Dermatol Venereol. 2015;29(9):1718–23.
Wiegell SR, Fabricius S, Heydenreich J, Enk CD, Rosso S, Bäumler W, Baldursson BT, Wulf HC. Weather conditions and daylight-mediated photodynamic therapy: protoporphyrin IX-weighted daylight doses measured in six geographical locations. Br J Dermatol. 2013;168(1):186–91.
Lerche CM, Heerfordt IM, Heydenreich J, Wulf HC. Alternatives to outdoor daylight illumination for photodynamic therapy-use of greenhouses and artificial light sources. Int J Mol Sci. 2016;17(3):309.
Mordon S, Vignion-Dewalle AS, Thecua E, Vicentini C, Maire C, Deleporte P, Baert G, Lecomte F, Mortier L. Can daylight-PDT be performed indoor? G Ital Dermatol Venereol. 2018;153(6):811–6.
Kellner C, Bauriedl S, Hollstein S, Reinhold U. Simulated-daylight photodynamic therapy with BF-200 aminolaevulinic acid for actinic keratosis: assessment of the efficacy and tolerability in a retrospective study. Br J Dermatol. 2015;172(4):1146–8.
Prahl S. Protoporphyrin IX diemthyl ester. 2014. [Cited 2021 November 22]. Available at: http://omlc.ogi.edu/spectra/PhotochemCAD/html/149.html.
Wiegell SR, Haedersdal M, Eriksen P, Wulf HC. Photodynamic therapy of actinic keratoses with 8% and 16% methyl aminolaevulinate and home-based daylight exposure: a double-blinded randomized clinical trial. Br J Dermatol. 2009;160(6):1308–14.
Galderma Metvix 160mg/g cream: Summary of product characteristics (https://www.medicines.org.uk/emc/medicine/11913). (last Access 10 Dec 2021)
Arisi M, Zane C, Polonioli M, Tomasi C, Moggio E, Cozzi C, Soglia S, Caravello S, Calzavara-Pinton I, Venturini M, Rossi MT, Calzavara-Pinton PG. Effects of MAL-PDT, ingenol mebutate and diclofenac plus hyaluronate gel monitored by high-frequency ultrasound and digital dermoscopy in actinic keratosis—a randomized trial. J Eur Acad Dermatol Venereol. 2020;34(6):1225–32.
Babilas P, Kohl E, Maisch T, Bäcker H, Gross B, Branzan AL, Bäumler W, Landthaler M, Karrer S, Szeimies RM. In vitro and in vivo comparison of two different light sources for topical photodynamic therapy. Br J Dermatol. 2006;154(4):712–8.
Alexiades-Armenakas MR, Geronemus RG. Laser-mediated photodynamic therapy of actinic cheilitis. J Drugs Dermatol. 2004;3(5):548–51.
Choi SH, Kim KH, Song KH. Efficacy of ablative fractional laser-assisted photodynamic therapy for the treatment of actinic cheilitis: 12-month follow-up results of a prospective, randomized, comparative trial. Br J Dermatol. 2015;173(1):184–91.
Sotiriou E, Lallas A, Goussi C, Apalla Z, Trigoni A, Chovarda E, Ioannides D. Sequential use of photodynamic therapy and imiquimod 5% cream for the treatment of actinic cheilitis: a 12-month follow-up study. Br J Dermatol. 2011;165(4):888–92.
Wiegell SR, Heydenreich J, Fabricius S, Wulf HC. Continuous ultra-low-intensity artificial daylight is not as effective as red LED light in photodynamic therapy of multiple actinic keratoses. Photodermatol Photoimmunol Photomed. 2011;27(6):280–5.
O’Gorman SM, Clowry J, Manley M, McCavana J, Gray L, Kavanagh A, Lally A, Collins P. Artificial white light vs daylight photodynamic therapy for actinic keratoses: a randomized clinical trial. JAMA Dermatol. 2016;152(6):638–44.
Vegter S, Tolley K. A network meta-analysis of the relative efficacy of treatments for actinic keratosis of the face or scalp in Europe. PLoS One. 2014;9(6): e96829.
Acknowledgements
The first author thanks all the nursing staff of the dermatology department for their valuable help in daily clinical practice.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Mariachiara Arisi, Piergiacomo Calzavara-Pinton, Marina Venturini and Mariateresa Rossi contributed to design the study protocol. Benedetta Galli collected the data and edited the photographic part. Luigi Spiazzi and Cesare Tomasi participated in the physical and statistical analysis of the data respectively. Mariachiara Arisi, Edoardo Guasco Pisani, Giuseppe La Rosa and Sara Rovaris recruited the patients and collected all the data. Mariachiara Arisi and Piergiacomo Calzavara-Pinton wrote the article and Gaetano Licata revised the article.
Disclosures
Mariachiara Arisi, Benedetta Galli, Edoardo Guasco Pisani, Giuseppe La Rosa, Gaetano Licata, Sara Rovaris, Cesare Tomasi, Mariateresa Rossi, Marina Venturini, Luigi Spiazzi and PierGiacomo Calzavara-Pinton have nothing to disclose.
Compliance with Ethics Guidelines
The study was held at the Dermatologic Department of the University of Brescia from January 2019 to March 2021 in accordance with the Declaration of Helsinki and it was approved by the Local Ethic Committee (Protocol Number 3718). All patients were given verbal and written information on the nature of the study, and they signed an informed consent form before enrolment.
Data Availability
The datasets generated or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arisi, M., Galli, B., Pisani, E.G. et al. Randomized Clinical Trial of Conventional versus Indoor Daylight Photodynamic Therapy for Treatment of Actinic Cheilitis. Dermatol Ther (Heidelb) 12, 2049–2061 (2022). https://doi.org/10.1007/s13555-022-00783-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00783-1