Abstract
Introduction
Moderate to severe atopic dermatitis (AD) is associated with a significant disease burden, impacting sleep, quality of life, and treatment needs. The aim of this study was to characterize disease burden and treatment patterns for adults with moderate to severe AD in three European countries: France, Italy, and the UK.
Methods
This retrospective analysis of adult patients with moderate to severe AD in Europe used medical records and physician/patient survey data collected in August 2019 to April 2020. Demographic and baseline disease characteristics, information on current comorbidities, disease flares, and current and previous treatments were collected by the physician. Patient-perceived burden was assessed using patient-reported outcome (PRO) questionnaires, which were completed on a voluntary basis and included the following instruments: Patient-Oriented Eczema Measure (POEM), Dermatology Life Quality Index (DLQI), EuroQol five-dimensional (EQ-5D), and Work Productivity and Activity Impairment (WPAI). Disease severity was subjectively assessed by physicians and was based on their own definition of the terms mild, moderate, and severe. Data were analyzed descriptively.
Results
The physician-reported sample included 912 patients with moderate to severe disease from France (n = 314), Italy (n = 309), and the UK (n = 289); approximately 30% of patients provided PRO data. Across these countries, 22–41% of patients reported current flares; mean POEM and DLQI scores were 10.6–13.1 and 9.5–11.1, respectively, indicating a high disease burden. However, systemic therapy use was low (e.g., conventional systemics were used by 18–24% of patients). Physician-assessed disease severity did not fully align with EASI scores, indicating that factors in addition to skin signs are impacting AD severity.
Conclusion
Patients with moderate to severe AD report significant disease burden, highlighting unmet treatment needs, particularly with respect to the underuse of systemic treatments despite AD being a systemic disease and the associated disease burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
With new therapies for adult patients with moderate to severe AD in European countries, the need to better understand the burden of disease and real-world treatment patterns for this patient population remains of key importance. |
This country-specific analysis provides insights from a patient–physician survey on patient and disease characteristics, including current flare status, treatment patterns, and comorbidities, and describes PROs in adults with moderate to severe AD. |
What was learned from the study? |
Results of the analysis indicate that adult patients with moderate to severe AD have a significant disease burden and unmet treatment needs, including the under-utilization of systemic treatments, despite AD being a systemic disease. |
Findings of the current analysis are supported by those of previously conducted analyses, including a large European prospective observational study and other retrospective real-world studies in patients with moderate to severe AD. |
Introduction
Atopic dermatitis (AD) is a chronic, relapsing inflammatory disorder characterized by erythematous, pruritic, dry, scaly, and often lichenified skin [1,2,3,4]. It is linked to aberrant immunologic responses [3] and, as such, is associated with common atopic comorbidities, including asthma and allergic rhinitis [5,6,7]. It is also associated with non-atopic comorbidities, such as depression, anxiety, bacterial and viral infections, and obesity [5,6,7].
The onset of AD most commonly occurs in early childhood, with up to 25% of children affected by the condition [2]. As most cases of childhood AD resolve by adulthood, AD is less common in adults than children. However, AD can persist or even start in adulthood, and one in four adults with AD report adult onset [8]. The prevalence of AD in adults has been reported as 4.4% in the European Union (EU), 3.6% in France, 8.1% in Italy, and 2.5% in the UK [9]. Among patients with AD in the EU, the proportion with moderate to severe disease varies from 46% to 66% depending on the patient-reported measurement scale used [Patient Global Assessment (PGA) 46%; Patient-Oriented Eczema Measure (POEM) 53%; Patient-Oriented Scoring of Atopic Dermatitis (PO-SCORAD) 66%] [9]. Severe AD represents a small proportion of the overall AD population (3–13%), regardless of measure or region [9].
According to a US population-based survey, pruritus is the most burdensome symptom of AD across all severities of adult AD, although additional signs, symptoms, and sequelae of scratching become more prominent in severe AD [10]. Other symptoms with an important impact on health-related quality of life (HRQoL) include skin pain and sleep disturbance. In addition, AD of any severity had a limiting effect on lifestyle in over half of patients (51.3%), impacted daily activities in 43.3%, and led to avoidance of social interaction in 39.1% of patients. This negative impact was greater in patients with severe disease than in those with moderate disease. Other studies have also shown that AD is associated with mental health symptoms or conditions, functional impairment, and reduced HRQoL, and negatively impacts on social, work-related, and intimate aspects of life [11,12,13,14,15,16].
European guidelines published in 2018 [17, 18] suggested that adults with severe AD whose symptoms are not adequately controlled with topical agents (e.g., emollients, corticosteroids, calcineurin inhibitors) should be considered for treatment with conventional systemic immunosuppressants (e.g., cyclosporine, methotrexate, azathioprine, mycophenolate mofetil), the biologic agent dupilumab, phototherapy, or short-term oral corticosteroids for acute flare management. However, cyclosporine was the only licensed oral medication for AD at the time the guidelines were published; importantly, treatment with cyclosporine should not exceed 2 years because of common side effects such as hypertension and (usually irreversible) nephrotoxicity [17, 18]. Newer treatments for AD include the oral selective Janus kinase (JAK) inhibitors baricitinib, upadacitinib, and abrocitinib, all of which were recently approved in the EU for the treatment of moderate to severe AD in adult patients who are candidates for systemic therapy [19,20,21]. The injectable interleukin-13 inhibitor tralokinumab has also been approved for this indication [22].
With newly emerging therapies and further treatments in development [1, 23, 24], there is a continuous need to better understand the burden of disease and real-world treatment patterns for adults with moderate to severe AD in European countries, particularly the barriers regarding conventional (and on-label) treatments and limitations of their use. Findings from recent analyses of treatment patterns in the UK [25], Europe [26], and the USA [27, 28] suggest a lack of disease control with established therapies and an unmet need for safe and effective targeted agents for long-term disease control [25, 26].
The objective of this study was to characterize the disease burden for adult patients with moderate to severe AD using patient-reported outcomes (PROs) and physician surveys in three European countries: France, Italy, and the UK. This country-specific analysis presents data on patient and disease characteristics, including current flare status, treatment patterns, and comorbidities, and describes PROs in the context of physician-defined disease severity in this patient population.
Methods
Study Design, Data Source, and Study Participants
A retrospective observational study was conducted using medical records and physician and patient survey data from the Adelphi Atopic Dermatitis Disease Specific Programme (DSP). Adelphi DSPs are large, multinational, cross-sectional (point-in-time) surveys that provide current “real-world” data from both patients and physicians at clinical practice sites, including specialty physician practices [29].
The survey collected data from adult patients (aged ≥ 18 years) with physician-diagnosed AD who were either currently experiencing or had a history of moderate to severe disease. Data were also collected from their primary care providers [i.e., general practitioners (GPs)] or specialist (dermatologist, allergist/immunologist) physicians. The survey was conducted in France, Italy, and the UK during the period August 2019 to April 2020. In the UK, recruitment of primary care physicians (PCPs)/GPs included a small proportion [8/62 (13%)] with a self-defined special interest in dermatology, whereas recruitment of PCPs/GPs in France and Italy did not involve/require any special interest. Although data were captured for patients with mild, moderate, and severe disease, the analysis focused on those currently with moderate to severe disease.
Physicians were identified from publicly available lists of healthcare professionals and invited to participate in the DSP. For inclusion in the study, physicians were required to be actively involved in AD drug management and have a minimum monthly workload of five adult patients with moderate to severe AD, including at least one patient with moderate and one with severe AD. Physicians were requested to complete a patient record form (PRF) for each of the next five consecutive eligible patients consulting with AD. PRFs included detailed information related to subjective and objective clinical characteristics and treatment.
All patients for whom a PRF was completed were invited to complete a patient self-completion form (PSC) on a voluntary basis. If they agreed to do so, the PSC was completed using pen and paper after the consultation and independent of the physician. The PSC was linked to the physician-completed PRF and provided patient insights into their disease, including validated PROs.
Determination of Disease Severity
Disease severity was determined according to the clinical judgment of consulting physicians. Specifically, physicians were asked for their overall assessment of the severity of AD for each patient based on their own definition of the terms mild, moderate, and severe.
Study Variables
Demographic and baseline disease characteristics, as well as information related to current comorbidities, were extracted from the PRFs. Comorbidities were split into atopic and non-atopic conditions, and information about them was based on the physician’s knowledge of each patient and their medical records. The PRFs also provided data on disease flares (defined as an acute episode/temporary worsening of symptoms, as per clinical judgment), and on current topical therapy, including topical corticosteroids, topical calcineurin inhibitors, and topical crisaborole, all reported either as monotherapy or in combination. Systemic corticosteroids, conventional systemic therapies (which included cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil but excluded systemic corticosteroids), and dupilumab were reported either as monotherapy or in combination with topical agents.
Data on PROs were obtained from the PSCs and included the self-administered measures described below. The POEM questionnaire assesses the frequency of AD symptoms over the past week. The instrument covers seven domains/items (itch, sleep, bleeding, weeping or oozing, cracking, flaking, and dry or rough skin), and total scores range from 0 to 28, with higher scores indicating greater severity [32, 33]. The Dermatology Life Quality Index (DLQI) is a dermatology-specific questionnaire that measures the impact of skin disease on HRQoL. It comprises ten questions relating to daily life in the last week and covers six domains/items (symptoms and feelings, daily activities, leisure, work and school, personal relationships, and treatment). Total scores range from 0 to 30, with higher scores indicating a greater impact on the patient’s life [34, 35]. The three-level EQ-5D is a generic (i.e., non-disease-specific) instrument that provides an assessment of general health/HRQoL [36]. Health utility index scores are generated with country-specific algorithms and range from 0 to 1, with lower scores reflecting poorer HRQoL. The Work Productivity and Activity Impairment (WPAI) questionnaire measures the impact of disease on work productivity and daily activities over the past week. The instrument includes four items (absenteeism, presenteeism, loss of productivity and work, and impact on activities), and the score is expressed as a percentage, with higher scores indicating a greater impact [37].
Data were collected on the percentage of patient body surface area (BSA) affected by AD. Data provided by physicians on the PRFs were used to calculate Eczema Area and Severity Index (EASI) scores [30], which provide an assessment of skin signs and extent of skin involvement. Severity strata for the EASI, as defined by Leshem and colleagues [31], were applied as follows: 0, clear; 0.1–1.0, almost clear; 1.1–7.0, mild; 7.1–21.0, moderate; 21.1–50.0, severe; 50.1–72.0, very severe. Uncontrolled AD was defined as changeable or deteriorating on the basis of physician description of current disease.
Statistical Analyses
Results are presented separately for patients with moderate AD and those with severe disease, and for both groups combined (i.e., moderate to severe disease). Descriptive statistics were provided for demographics and disease characteristics (e.g., time since diagnosis, comorbidities, flare status, treatment, etc.). Continuous variables were described using mean and standard deviation (SD). Categorical variables were reported as the frequency and percentage within each category. Univariate tests were used to compare these variables between patients with moderate versus severe AD, and between patients flaring versus those not flaring (for those with a flare history), i.e., t-test for continuous variables, and Fisher’s exact test for binary categorical variables. p-Values < 0.05 were considered statistically significant.
PROs (POEM, DLQI, EQ-5D, WPAI) were compared between patients with moderate versus severe AD, and between those flaring versus those not flaring, each using inverse probability-weighted regression adjustment, a propensity score type method that adjusts for potential bias due to confounding factors. The moderate versus severe AD comparison was adjusted for age, sex, body mass index (BMI), and Charlson Comorbidity Index. For the flaring versus not flaring comparison, current AD severity was also included as a confounding factor. For each PRO, adjusted means with accompanying standard errors within each group and a p-value comparing the adjusted means were reported. Means and SDs, unadjusted for confounders, were also reported within subgroups but were not compared with statistical tests.
No imputation of missing data was conducted, although PRFs were completed online, which minimized missing data. A comparison of baseline characteristics of patients completing versus those not completing PSC forms was conducted using Fisher’s exact test for categoric and t-test for numeric/continuous variables, with p < 0.05 indicating a statistically significant difference between PSC responders and nonresponders.
Compliance with Ethics Guidelines
The DSP fulfills the definition of a market research survey under the EphRMA Code of Conduct and is therefore conducted to market research, rather than clinical, guidelines. Market research surveys are exempt from requiring institutional review board (IRB) approval; however, the Western IRB (WIRB) conducted a methodological review of the atopic dermatitis DSP and provided an exemption.
The DSP was conducted in compliance with the ICH Declaration of Helsinki. Freely given, specific and informed consent, was obtained from each respondent to take part in the DSP and for the processing of their personal data. All data provided by physicians and patients were anonymized.
Results
Of 1517 patients surveyed across the three countries (data provided by 307 physicians), 605 (40%) had mild disease, 746 (49%) had moderate AD, and 166 (11%) had severe AD on the basis of physician assessment. All patients with mild AD had a history of moderate to severe disease. Therefore, the current analysis included 912 patients who currently had moderate to severe AD on the basis of PRF completion (PRF population): 314 in France, 309 in Italy, and 289 in the UK. In the PRF population, 78–84% of patients had AD of moderate severity and 16–22% had severe disease (Table 1).
Across the three countries, 45–66% of physicians were GPs or GPs with a special interest in dermatology (UK only), and the remainder were specialists, either dermatologists or allergists. In general, the proportion of specialists was higher for patients with severe than moderate disease, although this varied by country. In France, 77% of patients with severe AD were consulting with a specialist compared with 43% in Italy and 58% in the UK. The number of patients who voluntarily completed PSCs (PSC population) was 261 (29%), including 69 in France (22%), 128 in Italy (41%), and 64 in the UK (22%). In the PSC population, 75–88% of patients had moderate AD and 12–25% had severe disease across countries (Table 2).
Baseline Patient Characteristics
Baseline characteristics of patients currently presenting with moderate to severe AD based on the PRF population are summarized in Table 1. Across the three countries, mean age was 37.0 (SD 15.2) to 38.4 (SD 15.2) years, 50–54% of patients were male, and the mean time since AD diagnosis was 7.0 (SD 9.3) to 13.6 (SD 13.0) years. Current mean EASI scores for patients ranged from 8.1 (SD 5.9) to 11.7 (SD 9.8), with higher EASI scores in patients with severe AD. Current EASI disease severity category was most commonly mild (38–53%) or moderate (38–46%), with severe/very severe disease reported in 4–14% of patients; the remainder were in the clear (2–4%) category. EASI disease severity categories did not consistently match physician-rated disease severity, although no statistical analysis was performed. Baseline characteristics were generally similar between patients who completed PSCs and those who did not, although in all three countries the proportion of white patients was significantly higher (p < 0.05) among PSC responders than among nonresponders, and some country-specific statistically significant differences were also observed (Supplementary Table 1).
Flares
The proportion of patients currently experiencing a flare ranged from 28% to 41% across the three countries (41% in France, 28% in Italy, and 40% in the UK) (Table 1). The range was 25–37% for patients with moderate disease and 41–64% for those with severe AD.
The proportion of patients who experienced a flare in the last 12 months ranged from 58% to 71% across the three countries and was similar for patients with moderate or severe AD.
Current Treatments
Most patients were treated with topical therapies (corticosteroids, calcineurin inhibitors, and/or crisaborole), although the proportion of patients receiving topical treatments varied between countries (80% in France, 61% in Italy, and 84% in the UK) and was higher in patients with moderate disease than in those with severe disease (Fig. 1). The proportion of patients treated with systemic corticosteroids also varied between countries (6% in France, 24% in Italy, and 8% in the UK); these agents were primarily used in combination with topical therapy, and their use was higher in patients with severe AD. Overall, the use of conventional systemic therapies (excluding systemic corticosteroids) ranged from 18% in France and the UK to 24% in Italy. Combination therapy with topical therapy was more common than monotherapy across countries, and the use of conventional systemic therapies was higher in patients with severe AD. In all three countries, the most commonly used conventional systemic agents were cyclosporine and methotrexate (Supplementary Table 2).
Current treatment by atopic dermatitis severity in a France, b Italy, and c the UK. Data derived from patient record forms completed by physicians. Combination treatment indicates in combination with topical therapy. Combo combination treatment, cSys conventional systemic therapy (cyclosporine, methotrexate, azathioprine, mycophenolate mofetil), Mono monotherapy, sCS systemic corticosteroid, Topical topical therapy (topical corticosteroid, topical calcineurin inhibitor, and/or crisaborole)
Comorbidities
Across the three countries, atopic comorbidities were reported in 56–62% of patients (56% in France, 57% in Italy, and 62% in the UK). The most frequently reported atopic comorbidities included asthma (21–37% of patients) and allergic rhinitis (18–29%), followed by urticaria (4–11%) and allergic contact dermatitis (5–10%) (Fig. 2). No atopic comorbidities were reported in 38–44% of patients. In general, patients receiving systemic treatments had more comorbidities than those not receiving such treatments (data not shown).
Non-atopic comorbidities were reported in 44–50% of patients across the three countries (45% in France, 50% in Italy, and 44% in the UK). The most frequently reported non-atopic comorbidities were anxiety (18–26%), depression (7–16%), hypertension (4–15%), diabetes (4–11%), and insomnia (4–8%) (Fig. 2).
Patient-Perceived AD Burden Based on Patient-Reported Outcomes
PRO responses in the PSC population, including results from the POEM, DLQI, EQ-5D, and WPAI instruments, indicated more severe impairment in those with severe AD than in those with moderate disease. PROs also showed greater impairment in patients with severe versus moderate AD when results were adjusted for confounders (Table 2). Across the three countries, mean POEM scores (reflecting the frequency of AD symptoms) ranged from 10.6 (SD 6.3) to 13.1 (SD 6.9). Scores ranged from 10.3 (SD 6.1) to 12.7 (SD 6.9) for patients with moderate AD, and from 12.2 (SD 7.3) to 18.4 (SD 6.1) for those with severe disease. Across countries, the highest mean POEM subscores were for itch (1.9–2.8) and dry/rough skin (2.0–3.0) (Fig. 3).
Patient-Oriented Eczema Measure subscores (mean and standard deviation) by atopic dermatitis severity in a France, b Italy, and c the UK. Data derived from patient self-completion forms. Mod/Sev moderate or severe; *indicates that the number of patients was lower for this parameter in some or all countries and/or disease severity categories
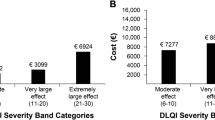
Mean DLQI scores (reflecting the impact of AD on HRQoL) were 10.1 (SD 6.3) in France, 9.5 (SD 5.7) in Italy, and 11.1 (SD 5.6) in the UK. Across countries, scores were 8.5 (SD 5.6) to 10.0 (SD 4.6) in patients with moderate disease and 12.0 (SD 7.1) to 18.9 (SD 6.3) among those with severe disease.
Overall, mean EQ-5D scores ranged from 0.74 to 0.89 in patients with moderate to severe disease, indicating poor HRQoL. Mean EQ-5D scores were 0.74 (SD 0.22) in France, 0.86 (SD 0.12) in Italy, and 0.89 (SD 0.14) in the UK. Across the three countries, scores were 0.77–0.91 for patients with moderate AD and 0.70–0.77 for those with severe disease.
Work productivity and daily activity, as assessed using the WPAI, were also impaired to a greater extent among patients with severe AD than among those with moderate disease (Table 2). Across the three countries, mean overall work impairment due to AD ranged from 20% to 25% [France 24.9% (SD 26.7), Italy 20.2% (SD 19.9), UK 22.1% (SD 21.9)], with a range of 18–21% for patients with moderate disease and 30–46% for those with severe disease. Mean overall activity impairment due to AD in patients with moderate to severe disease ranged from 25% to 33%.
In general, there was a trend toward PROs being more severely impaired in patients who were currently experiencing a flare than in those who were not, although this difference was not consistently significant after adjustment for confounders (Table 3). In all countries, mean POEM and DLQI scores were numerically higher, indicating greater disease burden, and EQ-5D values were lower, indicating poorer HRQoL, for patients experiencing flares versus those not experiencing flares. WPAI percent activity impairment due to AD was also numerically higher in those currently experiencing flares. Although there were no statistically significant between-group differences for any of these parameters in France and the UK, patients in Italy currently experiencing a flare had significantly higher mean adjusted DLQI scores (10.9 versus 7.5; p = 0.0012) and significantly greater percent activity impairment due to AD (43.7 versus 24.1; p = 0.0001) than those not currently experiencing a flare (Table 3).
Discussion
The present analysis characterized a real-world adult population with moderate to severe AD across three European countries (France, Italy, and the UK) in terms of demographic and disease characteristics, flare status, current treatments, comorbidities, and PROs. Across all three countries, 40% of patients currently had physician-rated mild disease, 49% had moderate disease, and 11% had severe disease, which is generally consistent with previously reported data [9, 38]. Overall, results showed that moderate to severe AD has a significant impact on HRQoL, as evidenced by PROs evaluated using the POEM, DLQI, EQ-5D, and WPAI instruments. Although disease burden based on PROs was generally greater among patients with severe than moderate disease, the burden was also substantial in patients with moderate disease. Despite the significant impact of moderate to severe AD on patient symptom burden (POEM assessment) and HRQoL, the use of systemic therapies was low in this patient population.
Interestingly, although the frequency of current flares was higher among patients with severe AD than in those with moderate disease, the frequency of flares during the last 12 months was similar regardless of disease severity. This might reflect the fluctuating nature of the disease and suggests that disease severity may shift across a continuum from moderate to severe.
The use of systemic therapy varied widely across the three countries. The proportion of patients treated with systemic corticosteroids ranged from 6% in France to 24% in Italy, and the use of conventional systemic therapy ranged from 18% in France and the UK to 24% in Italy; both were primarily used in combination regimens. Use of dupilumab, which had been available for at least 6 months in each country at the time of data collection, also ranged widely across countries, from 5% in the UK to 16% in France; it was also most commonly prescribed as combination therapy. Therefore, the study showed low utilization of dupilumab, as might be expected in view of its limited period of availability at the time the survey was conducted, but data also showed low use of conventional systemic treatment regimens, even in patients with severe disease. This suggests not only suboptimal management of adult patients with moderate to severe AD—many of whom have atopic or non-atopic comorbidities—but also unmet treatment needs. In particular, patients with severe disease had a higher disease burden despite the greater use of systemic therapy, highlighting an unmet treatment need at the time of the survey.
The substantial proportion of patients with uncontrolled AD, either changeable or deteriorating, also highlights unmet treatment needs. Overall, for patients with moderate to severe disease, AD was uncontrolled in 36–59% of patients and deteriorating in 10–29% across countries. As might be expected, the rate of uncontrolled AD was higher among patients with severe AD than in those with moderate disease.
In the current study, disease severity was subjectively assessed by physicians and did not fully match EASI severity categories. This suggests that overall skin signs alone do not capture the full extent of disease severity for the patient in terms of symptom burden, HRQoL, and impact on their ability to undertake work and daily activities. Body location in particular can impact disease burden, especially if more visible areas such as the face or hands are affected [39]. Therefore, we hypothesize that the poor alignment between disease severity and EASI is due to physicians taking additional factors into consideration, including body location and patient-reported impact on daily life, such as symptoms, HRQoL, and work ability.
In the current analysis, both atopic and non-atopic comorbidities were common, which is consistent with previous data [5]. Across the three countries, atopic comorbidities were reported in 56–62% of patients, and non-atopic comorbidities were reported in up to half of patients, with anxiety and depression consistently seen across countries. In general, the likelihood of having a comorbidity increased with the use of systemic treatments, which might be expected since use of systemic treatments is likely to reflect patients with more severe disease. Similar to our findings, the EUROSTAD prospective observational study recently reported a high level of comorbidities, AD burden, and impact on work and daily activities [26].
Although other recent real-world retrospective analyses [25, 27, 28] and a review of AD [40] also highlighted unmet treatment needs in this patient population, a unique and important strength of the current analysis is that both physician- and patient-reported outcomes were derived from the same patients. Another strength of the study is the use of the Adelphi DSP data source, a large international database that captures real-world country-specific information on disease characteristics and management, PROs, and HRQoL. The DSP also provides a tool to analyze unmet therapeutic needs. Additional methodological strengths include the enrollment of a sample of patients and use of standardized data collection tools across countries to facilitate between-country comparisons. The physician sample was generally representative of “real-world” clinical practice, with minimal exclusion criteria governing their selection.
The study has several inherent limitations. Assessment of AD severity and disease flare by physicians was subjective rather than based on a formalized diagnostic checklist and therefore may have varied between physicians and possibly countries. Approximately 50% of physicians were GPs, who may not have been experienced in providing the information (percentage of BSA affected in each body region) required to calculate the EASI score. This could have contributed to the finding that physician-assessed disease severity did not fully align with EASI scores and may have impacted treatment patterns, such as the proportion of patients receiving systemic therapy. Similarly, documentation of comorbidities was based on physicians’ knowledge and not standardized, potentially contributing to the variation in comorbidities across countries.
The nonrandomized study design, which included the next five consulting patients who were eligible for inclusion, provided a cross-section of patients presenting to a physician but may have resulted in over-representation of patients who consult more frequently or were currently experiencing a flare. Physician and patient participation in the study was also likely influenced by willingness to participate in the research and practical considerations of geographic location. The cross-sectional design of the study precluded demonstration of cause and effect, although this was not the primary purpose of the analysis. In addition, the point-in-time assessment does not reflect the whole concept of disease severity, which may encompass disease and treatment history as well as other factors. Since the completion of PSCs was voluntary, results for PROs and PROs by flare status were derived from a smaller sample (~ 30% of patients) than those for baseline characteristics, current flare status and history, current treatment, and comorbidities. However, comparison of patient demographic and disease characteristics for patients who did and who did not provide PRO data showed no consistent differences across countries, and the propensity score analysis accommodated some of these. In addition, for some baseline demographic and disease characteristic parameters and PROs, data were missing for some patients; therefore, results were not consistently available for all patients across countries for every outcome. Another limitation of the study was that it was conducted prior to the approval of JAK inhibitors and tralokinumab, and it is unclear how the availability of these agents would affect treatment patterns. Finally, the quality of data depended to a large extent on the accurate reporting of information by physicians and patients, which may be subject to recall bias.
Conclusions
This analysis demonstrates the high burden of AD in adults with moderate to severe disease, as assessed through flare status, treatment patterns, comorbidities, and PROs. Patients with severe disease show higher rates of current flares and uncontrolled disease than those with moderate AD. Physicians appear to consider factors in addition to skin signs in their assessment of AD severity. These findings highlight the unmet treatment needs of patients with moderate to severe AD, particularly with respect to the underuse of systemic treatments, despite AD being a systemic disease and causing a significant disease burden as shown in this analysis.
References
Lee DE, Clark AK, Tran KA, et al. New and emerging targeted systemic therapies: a new era for atopic dermatitis. J Dermatol Treat. 2018;29(4):364–74.
Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70(2):338–51.
Akdis CA, Akdis M, Bieber T, et al. European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. J Allergy Clin Immunol. 2006;118(1):152–69.
Bieber T. Atopic dermatitis. N Engl J Med. 2008;358(14):1483–94.
Silverberg JI. Comorbidities and the impact of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;123(2):144–51.
Silverberg JI. Atopic dermatitis in adults. Med Clin N Am. 2020;104(1):157–76.
Brunner PM, Silverberg JI, Guttman-Yassky E, et al. Increasing comorbidities suggest that atopic dermatitis is a systemic disorder. J Invest Dermatol. 2017;137:18–25.
Lee HH, Patel KR, Singam V, et al. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis. J Am Acad Dermatol. 2019;80(6):1526-1532.e7.
Barbarot S, Auziere S, Gadkari A, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy. 2018;73(6):1284–93.
Silverberg JI, Gelfand JM, Margolis DJ, et al. Patient burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol. 2018;121(3):340–7.
Chiesa Fuxench ZC, Block JK, Boguniewicz M, et al. Atopic dermatitis in America study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol. 2019;139(3):583–90.
Simpson EL, Bieber T, Eckert L, et al. Patient burden of moderate to severe atopic dermatitis (AD): insights from a phase 2b clinical trial of dupilumab in adults. J Am Acad Dermatol. 2016;74(3):491–8.
Eckert L, Gupta S, Amand C, et al. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77(2):274–279.e3.
Patel KR, Immaneni S, Singam V, et al. Association between atopic dermatitis, depression, and suicidal ideation: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:402–10.
Ring J, Zink A, Arents BWM, et al. Atopic eczema: burden of disease and individual suffering—results from a large EU study in adults. J Eur Acad Dermatol Venereol. 2019;33(7):1331–40.
Ludwig CM, Fernandez JM, Hsiao JL, et al. The interplay of atopic dermatitis and sexual health. Dermatitis. 2020;31(5):303–8.
Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32(5):657–82 (Erratum in: J Eur Acad Dermatol Venereol. 2019;33(7):1436).
Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol. 2018;32(6):850–78.
European Medicines Agency. Baricitinib (Olumiant®) summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/olumiant-epar-product-information_en.pdf. Accessed 21 Nov 2020.
European Medicines Agency. Upadacitinib (Rinvoq®) summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/rinvoq-epar-product-information_en.pdf. Accessed 13 Oct 2021.
European Medicines Agency. Abrocitinib (Cibinqo®) summary of product characteristics. https://www.ema.europa.eu/en/medicines/human/EPAR/cibinqo. Accessed 25 Jan 2022.
European Medicines Agency. Tralokinumab (Adtralza®) summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/adtralza-epar-product-information_en.pdf. Accessed 25 Jan 2022.
Nusbaum KB, Nguyen CM, Fleischer AB Jr. Emerging systemic therapies for atopic dermatitis: biologics. J Dermatolog Treat. 2022;33(3):1269–73.
Damsky W, King BA. JAK inhibitors in dermatology: the promise of a new drug class. J Am Acad Dermatol. 2017;76(4):736–44.
Eckert L, Amand C, Gadkari A, et al. Treatment patterns in UK adult patients with atopic dermatitis treated with systemic immunosuppressants: data from The Health Improvement Network (THIN). J Dermatol Treat. 2020;31(8):815–20.
De Bruin-Weller M, Pink AE, Patrizi A, et al. Disease burden and treatment history among adults with atopic dermatitis receiving systemic therapy: baseline characteristics of participants on the EUROSTAD prospective observational study. J Dermatol Treat. 2021;32(2):164–73.
Armstrong AW, Huang A, Wang L, et al. Real-world utilization patterns of systemic immunosuppressants among US adult patients with atopic dermatitis. PLoS ONE. 2019;14(1):e0210517.
Wei W, Ghorayeb E, Andria M, et al. A real-world study evaluating adeQUacy of Existing Systemic Treatments for patients with moderate-to-severe Atopic Dermatitis (QUEST-AD): baseline treatment patterns and unmet needs assessment. Ann Allergy Asthma Immunol. 2019;123(4):381-388.e2.
Anderson P, Benford M, Harris N, et al. Real-world physician and patient behaviour across countries: disease-specific programmes—a means to understand. Curr Med Res Opin. 2008;24(11):3063–72.
Chopra R, Silverberg JI. Assessing the severity of atopic dermatitis in clinical trials and practice. Clin Dermatol. 2018;36:606–15.
Leshem YA, Hajar T, Hanifin JM, et al. What the Eczema Area and Severity Index score tells us about the severity of atopic dermatitis: an interpretability study. Br J Dermatol. 2015;172(5):1353–7.
Charman CR, Venn AJ, Williams HC. The patient-oriented eczema measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140(12):1513–9 (Erratum in: Arch Dermatol. 2005;141(3):381).
Charman CR, Venn AJ, Ravenscroft JC, et al. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br J Dermatol. 2013;169(6):1326–32.
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Basra MK, Fenech R, Gatt RM, et al. The Dermatology Life Quality Index 1994–2007: a comprehensive review of validation data and clinical results. Br J Dermatol. 2008;159:997–1035.
EuroQol Research Foundation. EQ-5D-5L user guide. September 2019. https://euroqol.org/publications/user-guides. Accessed 21 Nov 2020.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65.
Carmo M, Andrade S, Mendes-Bastos P. Patients under atopic dermatitis treatment in Portugal: results from a physicians’ survey. Poster PSS11 presented at: ISPOR Europe 2018; 2018 Nov 10–14; Barcelona.
Lio PA, Wollenberg A, Thyssen JP, et al. Impact of atopic dermatitis lesion location on quality of life in adult patients in a real-world study. J Drugs Dermatol. 2020;19(10):943–8.
Cork MJ, Danby SG, Ogg GS. Atopic dermatitis epidemiology and unmet need in the United Kingdom. J Dermatol Treat. 2020;31(8):801–9.
Acknowledgments
The authors would like to acknowledge James Piercy, Laure Manuel, Jenny Austin, and Gary Milligan (Adelphi Real World, Bollington, Macclesfield, Cheshire, UK) for their contributions in data extraction, analysis, and related activities.
Funding
This work was supported by Eli Lilly and Company. The journal’s Rapid Service Fee was funded by Eli Lilly and Company.
Medical writing and editorial assistance
The authors would like to acknowledge Greg Plosker and Dr Sue Chambers (Rx Communications, Mold, UK) for medical writing assistance with the preparation of this manuscript, funded by Eli Lilly and Company.
Author contributions
Catherine Reed and Peter Anderson contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Peter Anderson (Adelphi Real World). All authors were involved in interpretation of data for the work. The first draft of the manuscript was written by Catherine Reed, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
C. Elise Kleyn has served as an advisory board member and/or consultant and received honoraria/research grants or participated in clinical trials for AbbVie, Almirall, Amgen, Celgene, Eli Lilly, Janssen, Leo Pharma, La Roche-Posay, Novartis, Pfizer, and UCB. Sébastien Barbarot is an investigator or speaker for AbbVie, Almirall, Chiesi, Eli Lilly, Janssen, Leo Pharma, Novartis, Pfizer, Sanofi Genzyme and UCB-Pharma. Catherine Reed, Serena Losi, Lill-Brith von Arx, Camille Robert, and Susanne Grond are employees of Eli Lilly and Company. Peter Anderson is an employee of Adelphi Real World. Antonio Costanzo served as advisory board member and consultant, and has received fees and speaker's honoraria from or has participated in clinical trials for AbbVie, Almirall, Biogen, Leo Pharma, Eli Lilly, Janssen, Novartis, Pfizer, Sanofi Genzyme, and UCB-Pharma.
Compliance with ethics guidelines
The DSP fulfils the definition of a market research survey under the EphRMA Code of Conduct and is therefore conducted to market research, rather than clinical, guidelines. Market research surveys are exempt from requiring Institutional Review Board (IRB) approval; however, the Western IRB (WIRB) conducted a methodological review of the atopic dermatitis DSP and provided an exemption. The DSP was conducted in compliance with the ICH Declaration of Helsinki. Freely given, specific and informed consent, was obtained from each respondent to take part in the DSP and for the processing of their personal data. All data provided by physicians and patients were anonymized.
Data availability
The dataset supporting the conclusions of this article are included within the article (and its additional files).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kleyn, C.E., Barbarot, S., Reed, C. et al. Burden of Moderate to Severe Atopic Dermatitis in Adults from France, Italy, and the UK: Patient-Reported Outcomes and Treatment Patterns. Dermatol Ther (Heidelb) 12, 1947–1965 (2022). https://doi.org/10.1007/s13555-022-00777-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00777-z