Abstract
Introduction
Hypertrophic scarring caused by conventional open thyroidectomy is prevalent among Asians and published trials have proved that silicone occlusive sheeting is a useful treatment for hypertrophic scarring. However, silicone occlusive sheeting does not effectively prevent scar widening. Here, we report elastic silicone occlusive sheeting as a new type of silicone application. In this study, we compared the effects of elastic silicone occlusive sheeting on scar width and appearance after conventional open thyroidectomy with those of silicone occlusive sheeting.
Methods
In this prospective, randomized, assessor-blinded study, a total of 74 patients who underwent conventional open thyroidectomy were recruited to undergo elastic silicone occlusive sheeting and silicone occlusive sheeting on the healed wound. Split scar study and scar quality were assessed on the basis of scar width, Vancouver scar scale, pain/itching visual analogue scale, and patients’ subjective degree of satisfaction with the scar, during the patients’ 6-month review.
Results
A total of 61 patients completed the study. Scar width, Vancouver scar scale score, and patients’ subjective degree of satisfaction indicated that elastic silicone occlusive sheeting was associated with narrower scars and significant improvement in scar appearance. The two methods did not differ significantly with regard to pain/itching visual analogue scale.
Conclusions
Our findings highlight elastic silicone occlusive sheeting as an effective treatment for scarring, resulting in narrower and better scars after conventional open thyroidectomy. The use of elastic silicone occlusive sheeting after conventional open thyroidectomy may minimize the formation of hypertrophic scars in the early postoperative period.
Trial Registration
ChiCTR2100049740.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hypertrophic scarring caused by conventional open thyroidectomy is prevalent and an effective treatment is badly needed. |
Silicone occlusive sheeting is not highly efficient at reducing scar width while various clinical trials have shown that it effectively prevents pathological scarring. |
Elastic silicone occlusive sheeting is a relatively new form of silicone application that combines occlusion and tension offloading but no study has found this combination to be more effective than either strategy alone. |
The study compared the effects of elastic silicone occlusive sheeting versus silicone occlusive sheeting on scar width and appearance after conventional open thyroidectomy. |
What was learned from the study? |
Elastic silicone occlusive sheeting overcomes the shortcomings of the silicone occlusive sheeting, which has limited capacity to reduce scar width. |
Scar width and scar appearance especially in the terms of vascularity and pigmentation are improved by using elastic silicone occlusive sheeting compared with silicone occlusive sheeting. |
Introduction
Since the year 2000, the incidence of thyroid cancer is reported to be rising significantly. Thyroid cancer is mainly treated through conventional open thyroidectomy, which creates a large incision and forms a disfigured scar. Studies indicate that the risk of pathologic scarring is higher in Asian patients than in Caucasians [1, 2].
Pathologic scars include hypertrophic scars, which remain within the boundaries of the original lesion, and keloids, which tend to expand beyond the boundaries of the original lesion. It is widely accepted that the tension acting on the wound edges is a major contributor to the disfiguring caused by scars. Wounds in areas of high tension, such as the manubrium, scapula, and joint, have a higher likelihood of developing wide pathological scars [3]. The neck is an area of frequent movement and high tension, which increase the risk of pathologic scarring. Although a wide range of treatments have been proposed for the prevention and minimization of pathological scarring, treatments capable of reducing tension around the wounds are limited.
Although various randomized clinical trials have shown that silicone occlusive sheeting effectively prevents pathological scarring [4,5,6], it is not highly efficient at reducing scar width. Clinically, tension offloading devices are used to reduce tension around the wound. However, tension offloading devices do not improve scar height, pigmentation, and pliability. To improve scar appearance, anti-scar treatments like silicone gels are often used. Additionally, the use of tension offloading devices is associated with a high rate of skin maceration, which limits wider clinical use of the device. Thus, more effective approaches are needed for the treatment of scar pathogenesis. Elastic silicone occlusive sheeting is a relatively new form of silicone application that combines occlusion and tension offloading. To date, no study has found this combination to be more effective than either strategy alone. Here, we compared the effects of elastic silicone occlusive sheeting versus silicone occlusive sheeting on scar width and appearance after conventional open thyroidectomy.
Methods
Elastic Silicone Occlusive Sheeting and Comparator
The elastic silicone occlusive sheeting has an elastic backing layer on one side and a silicone gel structure on the other. Its underlying principle is based on stress and strain, ensuring enough elasticity and resilience to reduce tension around the wound. Elastic silicone occlusive sheeting has very high elastic and resilient forces. The elastic silicone occlusive sheeting used in this study was 0.9 mm thick, 60 mm wide, and 80 mm long (Fig. 1). The sheeting was stretched before use and then applied around the scar areas in order to occlude them and offload tension around them. This strategy can be applied on necks, arms, legs, and trunks. Because adhesion is limited, elastic silicone occlusive sheeting can maintain a length of 80–93 mm on the skin after being stretched. Silicone occlusive sheeting, a self-adhesive silicone patch (0.3 mm thick, Fig. 2), was used as a comparator. The elastic silicone occlusive sheeting stretches easily (tensile modulus of elasticity 0.45 N/mm2, Fig. 3). It also has very good resilience that can generate a tensile elasticity of up to 3.95 N when placed on the skin while stretched to 93 mm. Comparatively, the silicone occlusive sheeting is hard to stretch. However, when stretched, it can reach a tensile modulus of elasticity of 0.64 N/mm2. Additionally, its resilience declines, which limits its ability to reduce tension around the healed wound. In conclusion, although the tensile modulus of elasticity of the elastic silicone occlusive sheeting is lower than that of the silicone occlusive sheeting, its resilience is better than that of silicone occlusive sheeting, which enables elastic silicone occlusive sheeting to reduce skin tension around the healed incision.
The elastic silicone occlusive sheeting. A An illustration of an elastic layer on the upper side and a silicone gel structure on the inferior side of the elastic silicone occlusive sheeting used as the experimental group. B The actual shape of the elastic silicone occlusive sheeting. The thickness, width, and length are 0.9 mm, 60 mm and 80 mm, respectively. The elastic silicone occlusive sheeting C before and D after stretching. Elastic silicone occlusive sheeting E before and F after application on the skin
The silicone occlusive sheeting. A The actual shape of the silicone occlusive sheeting used as the control with a thickness of 0.3 mm. B An illustration of the silicone occlusive sheeting before stretching. C The silicone occlusive sheeting after stretching. Silicone occlusive sheeting D before and E after application on the skin
Study Design and Ethical Approval
This single-center, prospective, randomized, assessor-blinded, and split scar trial was conducted at the Department of Breast Surgery. Patients were continuously enrolled from August to October 2021. Ethical approval for the study was granted by the Ethics Committee of the First Affiliated Hospital of Army Medical University, PLA, before the study started. All patients gave written informed consent, and the study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Identification of Patients
Inclusion criteria were (a) patients with a healed wound on the neck following conventional open thyroidectomy, (b) patients aged at least 18 years old, (c) patients able to give informed consent, and (d) a healed wound length of at least 4 cm.
Exclusion criteria were (a) intellectually challenged patients, (b) patients unable to understand written and oral Chinese, (c) patients who were unwilling or unable to return for follow-up, (d) pregnant women, (e) known history of allergy to the silicone occlusive sheeting, (f) patients with healed wounds with lengths of less than 4 cm, and (g) patients with other anti-scar treatment.
Patient Sample Size
Scar widths were used as the primary outcome measures for power analysis. A priori power analysis indicated that the study would need to enroll 74 patients in order to detect a difference of 0.7 mm, assuming α = 0.05, a power of 90, a standard deviation of 1.67, and a 20% patient dropout rate [7].
Randomization
After patient enrollment, the wound was divided in half. The left (superior) half and right (inferior) half of the wound were labeled A and B, respectively. Treatment method was assigned using a random integer generator [8], which generated zeroes and ones, which represented left/superior and right/inferior, respectively. If side A was designated for treatment using silicone occlusive sheeting, side B received elastic silicone occlusive sheeting (Fig. 4).
Treatment algorithm. A The elastic silicone occlusive sheeting and the silicone occlusive sheeting have a width of 60 mm and length of 80 mm. B Illustration of stretching the elastic silicone occlusive sheeting and the silicone occlusive sheeting before use. C The elastic silicone occlusive sheeting and the silicone occlusive sheeting were applied when the wound had healed and the scab of the wound had completely peeled off. D The wound was divided in half. If one side was designated for treatment using silicone occlusive sheeting, the other side received elastic silicone occlusive sheeting. E After 6 months, scar width, the Vancouver scar scale, the pain/itching visual analogue scale, and patients’ subjective degree of satisfaction were measured
Usage Procedure
The elastic silicone occlusive sheeting and the silicone occlusive sheeting were applied when the scab of the wound had completely peeled off. To ensure offloading around the wound, both the elastic silicone occlusive sheeting in the intervention group and the silicone occlusive sheeting in the control group were stretched before application, and used for almost 5 months after application. In week 1, the sheetings were applied for 8–12 h each day. From week 2 onward, they were applied for 24 h a day.
Clinical Assessments
The primary outcome measure of scar appearance was scar width. The secondary outcomes of scar appearance included the Vancouver scar scale, the pain/itching visual analogue scale, and patients’ subjective degree of satisfaction with the scar. Patients were evaluated 6 months after surgery, with an acceptable window for follow-up of 2 weeks before or after the assessment period.
Scar Width
A Vernier caliper was used to measure scar widths 1.5 cm from the midline on each side.
Vancouver Scar Scale
The Vancouver scar scale, a validated scar evaluation tool, was used as secondary outcome measure for power analysis. The Vancouver scar scale is based on four scar criteria (vascularity, pigmentation, height, and pliability; Table 1). Standardized digital images were taken with a labeled standard scale (centimeters and millimeters) next to each scar. Two blinded plastic surgeons, who were not involved in the intervention, evaluated the scar using the same scale for scar vascularity, pigmentation, thickness, and pliability [9].
Visual Analogue Scale
At the same time, the pain/itching visual analogue scale was used to assess pain and pruritus intensity [10, 11]. The pain/itching visual analogue scale score is based on a 10-cm line representing the patient’s intensity of pain and itching (“no pain/itching”, score = 0 and “worst imaginable pain/itching”, score = 10 [10-cm scale]). The pain/inching visual analogue scale was self-completed by the patient. To this end, the patient was asked to place a line perpendicular to the visual analogue scale at the point that represented their pain/inching intensity.
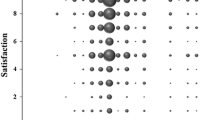
Patients’ Subjective Degree of Satisfaction with the Scar and Side Effects
Patients were surveyed about their overall degree of satisfaction using the following response choices in a grading scale: grade 1(very dissatisfied), grade 2 (not satisfied), grade 3 (moderately satisfied), grade 4 (satisfied), grade 5 (very satisfied). Patients also reported any side effects of treatment, including allergy, erythema, and infection.
Statistical Analysis
Scar widths, the Vancouver scar scale, the pain/itching visual analogue scale, and patients’ subjective degree of satisfaction with the scar are presented as mean ± SD. Differences between the groups for the parameters, scar width, Vancouver scar scale, the pain/itching visual analogue scale, and patients’ subjective degree of satisfaction with the scar were statistically compared using paired t tests. Statistical analysis was done using SPSS version 26 (IBM). P ≤ 0.05 indicated statistical significance.
Results
Patient Demographics
A total of 95 patients were screened and 74 of these were enrolled into the study. Of the 21 patients who were not enrolled, one did not meet inclusion criteria, while 20 declined to participate (7 were not concerned about the scar and 13 were unwilling to attend follow-up appointments) in the study. Of the 74 enrolled patients, 61 returned for their 6-month follow-up scar assessment (Fig. 5). The patients’ ages ranged from 21 to 52 years (mean age 40.5 years). Of the participants, 54 were women (88.5%) and 7 were men (11.5%) (Table 2).
Objective Assessment of the Scar Based on Scar Width
At the 6-month follow-up, mean scar width (our primary outcome measure) on the silicone occlusive sheeting side was significantly wider than the scar width on the elastic silicone occlusive sheeting side (1.02 mm versus 0.47 mm, respectively, P < 0.01, Table 3).
Subjective Assessment of the Scar Using the Vancouver Scar Scale
The results of the secondary outcome measure, Vancouver scar scale score, are shown in Table 4. The Vancouver scar scale scores of the elastic silicone occlusive sheeting side were significantly better than those of the silicone occlusive sheeting side (mean 3.93 versus 4.49) at the 6-month follow-up (lower scores indicate better outcomes, P < 0.01). Subcategory outcomes from the Vancouver scar scale score, such as scar vascularity, pigmentation, height, and pliability, are shown in Table 4. Pigmentation (P < 0.01) and vascularity (P < 0.01) scores for these scar characteristics were significantly different between the two sides, all favoring the better appearance of the elastic silicone occlusive sheeting side (Fig. 6). Moreover, the mean height score from the Vancouver scar scale was 0.98 for the elastic silicone occlusive sheeting side and 1.0 for the silicone occlusive sheeting side. Mean pliability score from Vancouver scar scale was 1.02 for the elastic silicone occlusive sheeting side and 1.03 for the silicone occlusive sheeting side. Scar height (P = 0.321) and pliability (P = 0.321) did not differ significantly between the two sides.
Subjective Assessment of the Scar Using the Pain/Itching Visual Analogue Scale
The pain/itching visual analogue scale scores at 6-month follow-up are shown in Table 5. The mean pain visual analogue scale score was 0.77 for the silicone occlusive sheeting side and 0.82 for the elastic silicone occlusive sheeting side. Visual analogue scale score for pain on the silicone occlusive sheeting side did not differ significantly from that of the elastic silicone occlusive sheeting side (P = 0.083). Moreover, the mean itching visual analogue scale score was 0.31 on the silicone occlusive sheeting side versus 0.36 on the elastic silicone occlusive sheeting side. Pruritus visual analogue scale scores did not differ significantly between the two sides (P = 0.083).
Subjective Assessment of the Scar Using Patients’ Subjective Degree of Satisfaction
From the patients’ perspective, the average degree of satisfaction with the scar was 4.25 in the elastic silicone occlusive sheeting group and 3.79 in the silicone occlusive sheeting group. There was significant statistical difference (P < 0.01). The results are outlined in Table 6.
Side Effects
Both the elastic silicone occlusive sheeting and silicone occlusive sheeting were not associated with any side effects in the 61 patients.
Discussion
Hypertrophic or keloid scarring after conventional open thyroidectomy is a ubiquitous but challenging phenomenon. Concerns over hypertrophic scarring in the neck area are a major psychological obstacle for patients considering whether to undergo conventional open thyroidectomy. Although methods like laparoscopic thyroidectomy minimize postoperative scarring, their surgical indications are limited. Thus, effective strategies for improving scar appearance are urgently needed.
Multiple factors contribute to undesirable scars, including the patient’s ethnic background, the anatomical location of the incision, local mechanical tension, surgical technique, and postoperative infections [12]. The neck is prone to pathologic scarring because of its frequent movement and local high tension. Moreover, tension acting on the neck is a major cause of scar disfigurement. Here, we describe a relatively new silicone-based strategy that combines occlusion and a tension offloading device. Using scar width, the Vancouver scar scale, the pain/itching visual analogue scale, and patients’ subjective degree of satisfaction analyses, we show that elastic silicone occlusive sheeting can narrow the scar and improve scar appearance following conventional open thyroidectomy. Elastic silicone occlusive sheeting and silicone occlusive sheeting differed significantly with regard to scar width and Vancouver scar scale scores. Scar width on the elastic silicone occlusive sheeting side was narrower when compared with that of the silicone occlusive sheeting. The mean Vancouver scar scale score of the elastic silicone occlusive sheeting was lower than that of the silicone occlusive sheeting. Additionally, scar vascularity, pigmentation, height, pliability, and Vancouver scar score of the elastic silicone occlusive sheeting were improved whereas there was no statistical difference of the pliability and height, probably because the size of patients was not enough and the minimum score of scar height in the Vancouver scar scale was 1 representing 2 mm height which cannot reflect the true differences.
The highly significant differences of scar width between the elastic silicone occlusive sheeting-treated portions and the silicone occlusive sheeting-treated portions are supported by basic science research on mechanotransduction and fibrosis [13,14,15]. Continuous muscular relaxation induced by elastic silicone occlusive sheeting could reduce movement and tension around a healing wound. This tension relief may help prevent scar widening, hypertrophy, and hyperpigmentation. Moreover, skin stretching around the wound by elastic silicone occlusive sheeting did not increase the incidence of skin maceration, which happens when using a tension offloading device.
Various randomized clinical studies have shown that silicone has a positive effect on the healing process of hypertrophic scars. Silicone has been used in various forms, including gel, gel sheets, spray, cream compounds, and silicone oil with or without additives [16, 17]. Studies indicate silicone gel sheeting may exert therapeutic effects via hydration and occlusion [18, 19]. Thus, we hypothesize that improvements in scar appearance result from the better hydration offered by elastic silicone occlusive sheeting, which is thicker than silicone occlusive sheeting. However, the excessive hydration may increase the incidence of skin maceration. Here, we did not observe increased risk of maceration which means the hydration level of elastic silicone occlusive sheeting is appropriate. Additionally, the pain/itching Vancouver scar scale scores did not differ significantly between the two interventions, which increased patients’ compliance.
To our knowledge, this is the first attempt to combine silicone with a tension offloading device. This new form of silicone sheeting overcomes the shortcomings of the silicone occlusive sheeting, which has limited capacity to reduce scar width, as well as the shortcomings of the tension offloading device, which is characterized by a high incidence of skin maceration, and does not improve scar height, pigmentation, and pliability.
The strengths of our study include its split scar comparison, randomized design, blinded evaluation, and use of an objective evaluation index and validated scar outcome instrument. Using the same patient as control allowed direct comparison of scar morphology, and enabled matching of the control and intervention groups by age, sex, anatomic location, variation in individual healing, and variable susceptibilities to scar formation. Thus, this strategy avoids the common confounding factors and biases encountered during patient selection.
It is worth mentioning that the final endpoint for this study was 6 months. This time point was chosen on the basis of our understanding of how scars change over time. We reasoned that 6 months met the criteria for the minimum acceptable time at which scar analysis should be performed, which is consistent with other studies [20, 21].
The limitation of this study is that the anatomical location is limited to the neck. The variety of anatomical locations could also have influenced tension offloading.
The strategy described here is applicable for patients undergoing conventional open thyroidectomy. To our knowledge, this strategy of elastic silicone occlusive sheeting is the first to combine the merits of silicone with a tension offloading device. The highly statistically significant differences including scar width, the Vancouver scar scale, and patients’ subjective degree of satisfaction with the scar between the elastic silicone occlusive sheeting-treated scars and the silicone occlusive sheeting-treated scars strongly indicate that the observed differences are real and not attributable to chance.
Conclusion
These results have important implications in conventional open thyroidectomy. Although it is hard to accurately estimate the number of patients that are unhappy with scars worldwide, the efficacy of the strategy described here suggests that elastic silicone occlusive sheeting can address an important unmet need and offer an alternative option to surgeons and patients undertaking scar management.
References
Miranda-Filho A, Lortet-Tieulent J, Bray F, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 2021;9(4):225–34.
Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet. 2016;388(10061):2783–95.
Butzelaar L, Ulrich MMW, Mink van der Molen AB, et al. Currently known risk factors for hypertrophic skin scarring: a review. J Plast Reconstr Aesthet Surg. 2016;69(2):163–9.
Mukherjee T, Chopra S, Aggarwal A, et al. Surgical scar revision using silicone gel sheet as an adjunct. Natl J Maxillofac Surg. 2021;12(1):36–41.
Wang F, Li X, Wang X, et al. Efficacy of topical silicone gel in scar management: a systematic review and meta-analysis of randomised controlled trials. Int Wound J. 2020;17(3):765–73.
O’Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;9:CD003826.
Niessen FB, Spauwen PH, Robinson PH, et al. The use of silicone occlusive sheeting (Sil-K) and silicone occlusive gel (Epiderm) in the prevention of hypertrophic scar formation. Plast Reconstr Surg. 1998;102(6):1962–72.
Sobie EA. An introduction to MATLAB. Sci Signal. 2011;4(191):tr7.
Chan KY, Lau CL, Adeeb SM, et al. A randomized, placebo-controlled, double-blind, prospective clinical trial of silicone gel in prevention of hypertrophic scar development in median sternotomy wound. Plast Reconstr Surg. 2005;116(4):1013–20.
Chiarotto A, Maxwell LJ, Ostelo RW, et al. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. 2019;20(3):245–63.
Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–52.
Dadaci M, Yildirim MEC, İnce B. Effects of botulinum toxin on improving facial surgical scars: a prospective, split-scar, double-blind, randomized controlled trial. Plast Reconstr Surg. 2019;143(1):237e-e238.
He J, Fang B, Shan S, et al. Mechanical stretch promotes hypertrophic scar formation through mechanically activated cation channel Piezo1. Cell Death Dis. 2021;12(3):226.
Duscher D, Maan ZN, Wong VW, et al. Mechanotransduction and fibrosis. J Biomech. 2014;47(9):1997–2005.
Hsu C-K, Lin H-H, Harn HIC, et al. Mechanical forces in skin disorders. J Dermatol Sci. 2018;90(3):232–40.
Moortgat P, Meirte J, Maertens K, et al. Can a cohesive silicone bandage outperform an adhesive silicone gel sheet in the treatment of scars? A randomized comparative trial. Plast Reconstr Surg. 2019;143(3):902–11.
Palmieri B, Gozzi G, Palmieri G. Vitamin E added silicone gel sheets for treatment of hypertrophic scars and keloids. Int J Dermatol. 1995;34(7):506–9.
Mustoe TA. Evolution of silicone therapy and mechanism of action in scar management. Aesthetic Plast Surg. 2008;32(1):82–92.
Garner WL. Epidermal regulation of dermal fibroblast activity. Plast Reconstr Surg. 1998;102(1):135–9.
Bush J, Duncan JAL, Bond JS, et al. Scar-improving efficacy of avotermin administered into the wound margins of skin incisions as evaluated by a randomized, double-blind, placebo-controlled, phase II clinical trial. Plast Reconstr Surg. 2010;126(5):1604–15.
Lim AF, Weintraub J, Kaplan EN, et al. The embrace device significantly decreases scarring following scar revision surgery in a randomized controlled trial. Plast Reconstr Surg. 2014;133(2):398–405.
Acknowledgements
The authors thank all the study participants for their involvement in the study and Henan Huibo Medical Co., Ltd, China for offering the silicone occlusive sheeting and the elastic silicone occlusive sheeting in this research.
Funding
This study was funded by Nature Science Foundation of China (No. 81873936), Clinical Technology Innovation Cultivation Project of Army Medical University (CX2019JS102) and Military Medical Science and Technology Youth Training Program (21QNPY026). These sponsors are funding the journal’s Rapid Service Fee.
Authorship
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Min Jiang, Jiaping Zhang and Yi Zhang designed the study; Min Jiang, Yi Zhang and Qiang Xiang enrolled the patients; Qilin Luo and Fengxia Wen performed the follow-up; Min Jiang, Xupin Jiang, Jie Liu, Chao Wu and Ze Zhang analyzed the data; Jiaping Zhang supervised the experiments; Min Jiang and Jiaping Zhang wrote the manuscript.
Disclosures
Min Jiang, Yi Zhang, Qiang Xiang, Qilin Luo, Fengxia Wen, Xupin Jiang, Jie Liu, Ze Zhang, Chao Wu and Jiaping Zhang have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the Ethics Committee of the First Affiliated Hospital of Army Medical University, PLA. It was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All patients gave written informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jiang, M., Zhang, Y., Xiang, Q. et al. Elastic Silicone Occlusive Sheeting Versus Silicone Occlusive Sheeting in the Treatment of Scars: A Randomized Controlled Trial. Dermatol Ther (Heidelb) 12, 1809–1821 (2022). https://doi.org/10.1007/s13555-022-00763-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00763-5