Abstract
Introduction
Although pulsed dye laser (PDL) remains the gold standard for the treatment of port-wine stains (PWS), hematoporphyrin monomethyl ether photodynamic therapy (HMME-PDT) is another treatment modality that has been shown to be effective in the treatment of PWS. This study aimed to observe the clinical efficacy and therapeutic response of HMME-PDT in the treatment of pediatric Chinese patients with PWS and to analyze the association between the efficacy of therapy and the dermoscopic features of PWS.
Methods
Pediatric patients with PWS and negative HMME skin test were enrolled between December 2017 and May 2021. Patients received an intravenous injection of 5 mg/kg HMME, and lesions were irradiated with 532-nm LED green light with a power density of 70–80 mW/cm2 for 20–25 min. Digital photographs and dermoscopic images were taken before and after two treatment sessions, and the clinical response was observed. The relationship between the efficacy of HMME-PDT and the dermoscopic features of PWS was retrospectively analyzed.
Results
A total of 216 pediatric patients (1–14 years) were recruited. Sixty-six patients had the pink type, while 150 had the purple type. After two HMME-PDT sessions, 55 patients showed excellent efficacy (25.46%), 77 patients showed good efficacy (35.65%), 69 patients showed fair efficacy (31.94%), and 15 patients showed no improvement (6.95%). Dotted and globular vessels were highly associated with excellent efficacy (41.82%); linear vessels were mainly associated with good efficacy (54.55%); reticular vessels were mainly associated with fair (55.07%) and mixed vessels were mainly associated with no improvement (26.66%).
Conclusion
HMME-PDT is an effective and safe treatment for pediatric patients with PWS. Dotted and globular vessels as well as linear vessels showed better efficacy compared to the other dermoscopic patterns in patients with PWS. Dermoscopy can provide useful clinical information about treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Little is known about the efficacy of HMME-PDT in pediatric patient with PWS |
The main purpose of this study was to evaluate the efficacy of HMME-PDT in pediatric Chinese patients and analyze the relationship between dermoscopic features of PWS and treatment outcome |
What was learned from the study? |
HMME-PDT is an effective and safe treatment modality for pediatric patients with PWS |
Some dermoscopic features were associated with better treatment outcome |
Introduction
Port-wine stains (PWS) are a subtype of low-flow congenital capillary malformations that occur at birth and affect < 1% of children. PWS grow and become darker in color with age. In some cases, they may present with varying degrees of disfigurement as a result of local tissue hypertrophy [1]. The distribution of PWS is usually unilateral and dermatomal; however, midline involvement is also seen [2]. PWS vary in size, location, color and thickness and are mainly classified into pink or red flat, purple flat, or nodular lesions [3]. About 75–85% of these lesions occur on the face and neck, which causes social-psychological problems for patients and their families [4]. In general, PWS have a benign clinical course, with the exception of cases with Sturge-Weber syndrome [1]. To date, PDL remains the gold standard for the treatment of PWS; however, up to 20% of PWS are hardly lightened with PDL [2, 5]. Photodynamic therapy (PDT) is an alternative, promising treatment modality for PWS, which was first applied to treat PWS by Gu Ying et al. in China in 1991 [6]. Several studies have reported the response rate of PDT in different types of PWS and age groups [7,8,9,10]. This therapy is based on a photochemical interaction among the photosensitizer, light and oxygen in the target tissue leading to apoptosis and endothelial destruction [11]. HMME is a new photosensitizer characterized by strong fluorescence and shorter post-treatment photosensitivity compared with first-generation photosensitizers; therefore, it has been the photosensitizer of choice for PDT [7, 12]. Ultrasound imaging has been used to diagnose and evaluate diseases of the skin and its appendages [13]; for instance, Khalaf et al. [14] recently reported that high-frequency ultrasound can evaluate the clinical efficacy of HMME photodynamic therapy. Dermoscopy, on the other hand, is another non-invasive, effective tool that can improve the diagnosis of vascular skin lesions and improve the clinical assessment of PWS by determining the depth of ectasia, which can help predict the outcome of treatment [15,16,17]. Several studies reported the association between dermoscopic features and the efficacy of PDL [18, 19]. In contrast, relatively little is known about the association between dermoscopic features of PWS and the efficacy of HMME-PDT. We therefore evaluated the efficacy of HMME-PDT in the treatment of PWS in pediatric patients and analyzed the correlation between the dermoscopy vascular pattern of PWS lesions and treatment outcome.
Methods
Study and Patients
Between December 2017 and May 2020, pediatric patients with PWS who had normal renal and hepatic function and no prior treatment with laser, PDT, isotopes, topical or systemic treatment for PWS in the previous 4 weeks were enrolled in this study [20]. Written informed consent was obtained from the patients’ parents or legal guardians before treatment. All included participants had skin type III–IV on the Fitzpatrick Phototype Scale. Patients with known allergy to HMME or its chemical ingredients, scar diathesis and severe hepatic or renal insufficiency were considered ineligible. This study was approved by The Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (015) and was conducted in accordance with the Helsinki Declaration.
Dermoscopy and Clinical Images of PWS Lesions
Patients received two sessions of HMME-PDT, with a 2-month interval. Images were taken before and after each treatment with a digital camera (Canon EOS 700D, Japan), using a fixed light source, position and camera parameters. The dermoscopic images of PWS were obtained before and after each HMME-PDT session using one of the following systems: (1) Nanjing Beining Medical Appliance Co., Ltd; (2) The Design Development Production and Service of Skin and Hair Visualizer BN-PFMF-8001. The dermoscopic images were taken from the most clinically relevant lesion, and in case of multiple facial lesions, the largest lesion was selected. Dermoscopic images were captured from different parts of the treatment area, and the images were evaluated by three blinded dermatologists. The dermoscopic features were divided into (1) vascular morphology with dots or globular vessels, sausage-like vessels, linear vessels, reticular vessels and mixed vessels; (2) nonvascular morphology with white circles and a whitish veil [17].
HMME-PDT Procedure
All patients received HMME-PDT as previously described [20]. Briefly, the dosage of photosensitizer was calculated (5 mg/kg), and the surrounding normal skin was covered with two layers of black fabric. After general anesthesia, patients received a slow injection of hemoporfin (Shanghai Fudan Zhangjiang Bio-Pharmaceutical Co. Ltd., Shanghai, China) via a venous pump for 10 min. The lesions were then irradiated with 532-nm LED green light (Wuhan YaGe LED-3 modified machine, Wuhan YaGe Photoelectric Technology Co., Ltd.) at a power density of 70–80 mW/cm2 for 20–25 min. The irradiation dose and time were selected according to the location and type of PWS.
Post-treatment Care and Follow-Up
Immediately after treatment, a cold ice pack was applied to the treated area. Mild topical corticosteroid cream was precribed for 3–7 days, and parents/guardians were advised to have the children avoid strong light and sun exposure and to use sunscreen for at least 14 days after treatment. Follow-up was performed via an online messaging platform where parents/guardians could report any post-treatment reactions, such as burning sensation, pain, pruritus, numbness, edema, purpura, blistering, crusting, hyperpigmentation and hypopigmentation at the treatment site. Laboratory tests were also performed at baseline and every month for 3 months to monitor adverse events. Patients were scheduled for a general evaluation every 3 months for at least 1 year.
Clinical Efficacy Evaluation
After two treatment sessions, three blinded dermatologists independently reviewed the clinical and dermoscopic images before and after treatment. According to the degree of color blanching from baseline, efficacy was assessed as follows: excellent efficacy: the color had almost or completely faded (≥ 90% improvement); good efficacy: the color had significantly faded (≥ 60% to < 90% improvement); fair: the color had partially faded (≥ 20% to < 60% improvement); no improvement: the color was mostly unchanged (< 20% improvement) [20, 21].
Statistical Analysis
SPSS22.0 statistical software was used for data analysis. The χ2 test and Fisher’s exact test were used to compare response rates between groups. Descriptive statistics were used to analyze the median age and interquartile range of cases. The Mann-Whitney U test was used to compare mean age between groups. P < 0.05 was considered statistically significant.
Results
Patients
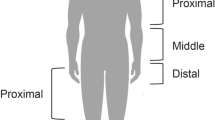
A total of 216 pediatric patients with an average age of 6.97 (1–14) years were included in the study; 54.63% of them were female (118/216). Based on clinical examination of the lesion, PWS were of flat purple and pink type (150 and 66 patients, respectively) (Table 1); 83.33% of the lesions were on the face (180 patients), including 43 on the first branch of the trigeminal nerve (V1), 39 on the second branch (V2), 51 on the third branch (V3) and 47 in the center of the face (upper eyelid, medial side of the cheek, nose, chin and upper cutaneous lip). Twenty-two patients had lesions on the arms or legs, and 14 had lesions on the neck. Most patients had lesions 5–10 cm2 in size (134 patients) (Table 2).
Clinical Efficacy
After two HMME-PDT sessions, 55 showed excellent efficacy (25.46%), 77 showed good efficacy (35.65%), 69 showed fair efficacy (31.94%), and 15 (6.95%) showed no improvement. Purple-type lesions showed better overall efficacy than pink-type lesions (P < 0). There was no significant difference between treatment response and patient sex (P = 0.655) or with age (P = 0.062). However, there was a significant difference between the site of the lesion and efficacy. Lesions on the face and neck responded better than those on the extremities (P < 0). While excellent efficacy was more likely to be observed in PWS on the first branch of the trigeminal nerve (V1: 83.72%), good efficacy was seen more in PWS on the third branch of the trigeminal nerve (V3: 64.70%). Most lesions located on the center of the face showed fair response (74.47%) (Table 2).
Dermoscopic Features
Linear vessels were the most common vascular pattern seen in the PWS lesions [n = 84 (38.89%)], followed by reticular vessels in 79 cases (36.57%), dots or globules vessels in 31 (14.35%), whitish veil in 9 (4.12%), mixed vessels in 7 (3.29%) and white circles vessels in 4 (1.85%), and 0.93% had sausage-like vessels (n = 2) (Table 3).
In the 84 lesions with linear vessels, 17 cases showed excellent efficacy (shown in Fig. 1a), good efficacy in 42 cases, fair efficacy in 22 cases and no improvement in 3 cases (shown in Fig. 1b). Among the 79 lesions with reticular vessels, 14 cases showed excellent efficacy, 21 cases showed good efficacy (shown in Fig. 2a), 38 cases showed fair (shown in Fig. 2b), and 6 cases showed no improvement. Of the 31 lesions with dotted and globular vessels, 23 cases showed excellent efficacy (shown in Fig. 3) and 8 cases showed good efficacy. For the nine lesions with a whitish veil, one case showed excellent efficacy, four showed good efficacy, three showed fair, and one showed no improvement (shown in Fig. 4). Also, one case of the mixed vessels pattern showed good efficacy, two had fair efficacy, and four had no improvement (shown in Fig. 5). Of the lesions with white circles, one showed good efficacy (shown in Fig. 6), whereas three showed fair efficacy. For the remaining two lesions with sausage-like vessels, one case showed fair (shown in Fig. 7) and one showed no improvement (Table 4).
a Linear vessels pattern with excellent treatment efficacy after two sessions of HMME-PDT. a1–a2 Digital photographs; a3–a4 dermoscopic images (pre- and post-treatment). b Linear vessel pattern on patient's arm associated with no improvement in treatment after two sessions of HMME-PDT; b1–b2 digital photographs; b3–b4 dermoscopic images (pre- and post-treatment)
a Reticular vessels pattern with good efficacy after two sessions of HMME-PDT; a1–a2 digital photographs; a3–a4 dermoscopic images (pre- and post-treatment). b Reticular vessel pattern with fair efficacy after two sessions of HMME-PDT; b1–b2 digital photographs; b3–b4 dermoscopic images (pre- and post-treatment)
Post-treatment Side Effects
All patients reported varying degrees of mild edema. Thirty-nine patients had pruritus, pustules and crusts. One patient had scar formation. No other local or systemic side effects were observed.
Discussion
We retrospectively analyzed the efficacy of HMME-PDT in a large group of pediatric patients. The treatment was shown to be an effective and safe modality in children with minimal or no side effects. We observed an overall high excellent and good response rate (25.46% and 35.65%, respectively), consistent with previous studies on the same age group [10, 11, 22]. We did not observe statistical differences between sex groups or age and response to treatment. However, there was a significant difference among lesion site, size and therapeutic response (P = 0). Lesions located on the face and neck appeared to respond better to HMME-PDT than lesions on the extremities. In addition, PWS on the first branch of the trigeminal nerve (V1) were associated with a significantly higher response than lesions located on the second and third branches (V2); these results were similar to those previously reported [8, 23].
In our study, we generally observed minimal or no post-treatment reactions, as most patients experienced pain, pruritus and edema of varying degrees that resolved with general management. Of the 39 patients who experienced crust formation, only 1 healed with a scar. Fortunately, we did not observe post-treatment hypo- or hyperpigmentation.
Currently, the dermoscopic features of PWS include: mixed vessels, blobs and rings, sausage-like vessels, dots or globules vessels, curved vessels, short clubbed vessels, linear vessels, whitish veil, reticular vessels, white circles and thin long parallel vessels [17]. Seven dermoscopic features were noted in our study. Linear vessels were the most frequently observed dermoscopic feature, followed by reticular vessels, dots or globules vessels, whitish veil, mixed vessels and sausage-like vessels.
The dermoscopic features of dot or globule vessels (also known as type I) represent vertical capillaries located superficially in the papillary dermis and are associated with a strong response to laser treatment compared with other patterns [15, 24, 25]. In our study, most dots or globule vessels were seen in the facial lesion and were associated with high excellent and good response. Similar results have been reported in previous studies [26, 27].
The sausage-like vessels are considered to be superficially located vessels similar to those of dots or globules and response well to laser treatment [28]; however, this pattern was observed in only two cases and was associated with fair or no improvement.
Linear and reticular vessels (also known as type II) were the most common vascular pattern found in our study. Although they are considered deeply located vessels and more difficult to treat than those of dot or globules pattern [18], interestingly, they were associated with excellent and good response in the current study. Furthermore, fair response (≥ 20% to < 60% improvement) was also common in these two vascular patterns. Contrarily, these two patterns showed lower response rates to HMME-PDT in previous reports [26, 27]. However, this could be due to the small number of patients in other dermoscopic patterns. We also hypothesize that the vessels of younger patients are more superficial and more easily destroyed, especially since most patients with linear vessels (39 of 84) were young children aged 1–3 years. It is therefore recommended that treatment be started at an early age.
Mixed vessels (also known as type III) are associated with poor response to laser treatment compared with the above patterns [25, 29]. This pattern was observed in only seven patients in our study, five of whom had pink type and had fair or no response to treatment.
White circles and whitish veils are nonvascular dermoscopic features observed in our study. Whitish veil was observed in nine patients with purple type and white circles in four patients, three of whom had pink type. Although these patterns usually predict poor response to laser treatment [19], notably, both patterns showed good and fair response, and one case with a whitish veil showed excellent response to HMME-PDT. We observed a significant difference in the treatment outcome between the different patterns of dermoscopic features of PWS with P = 0.000 (Table 4); however, this might be due to the small sample size in some dermoscopic patterns.
Our study has some notable limitations. One is that the dermoscopic images in our study were taken from the most clinically relevant lesion, which could lead to possible dermoscopic misclassification, especially because a single lesion may sometimes have different dermoscopic features. In addition, this is a retrospective study that lacks objective assessment tools, which is the main limitation of our study. Therefore, the use of objective instruments such as the chromameter is needed in future prospective studies with larger sample sizes.
Conclusion
Notwithstanding its limitations, our study suggests that HMME-PDT is a safe and effective treatment for PWS in pediatric patients and provided further evidence that dermoscopy is no longer exclusively used for malignant skin tumors but is also of great benefit in benign and inflammatory pathologies. In addition, dermoscopy can be used as a monitoring tool for dermatologic treatments, especially physical-type treatments. However, it should be evaluated with multivariate analysis, as other factors such as lesion location and thickness could also influence therapeutic outcomes. HMME-PDT showed an overall good to fair response in all dermoscopic patterns observed in our study. In addition, V1 involvement and dermoscopic pattern of dots or globules are indicators of favorable treatment outcome.
References
Mahady K, Thust S, Berkeley R, et al. Vascular anomalies of the head and neck in children. Quant Imaging Med Surg. 2015;5(6):886–97.
Jasim ZF, Handley JM. Treatment of pulsed dye laser-resistant port wine stain birthmarks. J Am Acad Dermatol. 2007;57(4):677–82.
Yuan K-H, et al. Photodynamic therapy in treatment of port wine stain birthmarks—recent progress. Photodiagn Photodyn Ther. 2009;6(3–4):189–94.
Schiffner R, Brunnberg S, Hohenleutner U, et al. Willingness to pay and time trade-off: useful utility indicators for the assessment of quality of life and patient satisfaction in patients with port wine stains. Br J Dermatol. 2002;146:440–7.
Stier MF, et al. Laser treatment of pediatric vascular lesions: port wine stains and hemangiomas. J Am Acad Dermatol. 2008;58(2):261–85.
Gu Y, Li J, Guo Z. Photodynamic therapy in treatment of PWS. Beijing Med J. 1991;13(5):317.
Ma G, Han Y, Ying H, Zhang X, Yu W, Zhu J, Cen Q, Chen H, Jin Y, Lin X. Comparison of two generation photosensitizers of PsD-007 and hematoporphyrin monomethyl ether photodynamic therapy for treatment of port-wine stain: a retrospective study. Photobiomodul Photomed Laser Surg. 2019;37(6):376–80.
Han Y, Ying H, Zhang X, Yu W, Cen Q, Chen X, Qiu Y, Chen H, Jin Y, Ma G, Lin X. Retrospective study of photodynamic therapy for pulsed dye laser-resistant port-wine stains. J Dermatol. 2020;47(4):348–55.
Gu Y, Huang N, Liang J, Pan YM, Liu FG. Clinical study of 1949 cases of port wine stains treated with vascular photodynamic therapy (Gu’s PDT). Ann Dermatol Venereol. 2007;134:241–4.
Zhang B, Zhang T, Huang Z, Li Q, Yuan KH, Hu ZQ. Comparison of pulsed dye laser (PDL) and photodynamic therapy (PDT) for treatment of facial port-wine stain (PWS) birthmarks in pediatric patients. Photodiagn Photodyn Ther. 2014;11(4):491–7.
Li-qiang G, Hua W, Si-li N, Chun-hua T. A clinical study of HMME-PDT therapy in Chinese pediatric patients with port-wine stain. Photodiagn Photodyn Ther. 2018;23:102–5.
Reddy K, Brightman L, Geronemus R. Laser treatment of port-wine stains. Clin Cosmet Investig Dermatol. 2015;8:27–33.
Shi W, Wang J, Lin Y, et al. Treatment of port-wine stains with pulsed dye laser: a retrospective study of 848 cases in Shandong Province, People’s Republic of China. Drug Des Dev Ther. 2014;8:2531–8.
Khalaf AT, Sun Y, Wang F, Sheng M, Li Y, Liu X. Photodynamic therapy using HMME for port-wine stains: clinical effectiveness and sonographic appearance. Biomed Res Int. 2020;2020:6030581.
Vázquez-López F, et al. The hand-held dermatoscope improves the clinical evaluation of port-wine stains. J Am Acad Dermatol. 2003;48(6):984–5.
Chuh A, et al. Does dermatoscopy facilitate the detection and diagnosis of vascular skin lesions? A case-control study. J R Coll Physicians Edinb. 2018;48(3):210–6.
Huang Y, Yang J, Li Z, Zhang L, Sun L, Bi M, Wang L. Dermoscopic features of port-wine stains: a study of 264 cases. Australas J Dermatol. 2021;62:e201–6.
Eubanks LE, McBurney E. Videomicroscopy of port-wine stains: correlation of location and depth of lesion. J Am Acad Dermatol. 2001;44(6):948–51.
Shirakawa M, Ozawa T, Wakami S, et al. Utility of dermoscopy before and after laser irradiation in port wine stains. Ann Dermatol Clin. 2012;24(1):7–10.
Zhang XY, Al-Odaini N, Fan RG, Xiong HD, Huang JC, Dai HM, Zhou YH, Huang XY, Wen SJ. The efficacy of hematoporphyrin monomethyl ether photodynamic therapy in adult patients with port-wine stains: a retrospective study. Dermatol Ther. 2022;12:861–9.
Zhao Y, Tu P, Zhou G, et al. Hemoporfin photodynamic therapy for portwine stain: a randomized controlled trial. PLoS One. 2016;11(5):0156219.
Yuan KH, Li Q, Yu WL, Zeng D, Zhang C, Huang Z. Comparison of photodynamic therapy and pulsed dye laser in patients with port wine stain birthmarks: a retrospective analysis. Photodiagn Photodyn Ther. 2008;5:50–7.
Sadeghinia A, Moghaddas S, Tavakolpour S, Teimourpour A, Danespazhooh M, Mahmoudi H. Treatment of port wine stains with 595-nm pulsed dye laser in 27 pediatric patients: a prospective study in the Iranian population. J Cosmet Laser Ther. 2019;21(7–8):373–7.
Procaccini EM, Argenziano G, Staibano S, et al. Epiluminescence microscopy for port-wine stains: pretreatment evaluation. Dermatology. 2001;203:329–32.
Bencini PL, Cazzaniga S, Galimberti MG, et al. Variables affecting clinical response to treatment of facial port-wine stains by flash lamp-pumped pulsed dye laser: the importance of looking beyond the skin. Lasers Med Sci. 2014;29:1365–70.
Huang Y, Yang J, Sun L, Zhang L, Bi M. Efficacy of influential factors in hemoporfin-mediated photodynamic therapy for facial port-wine stains. J Dermatol. 2021;48(11):1700–8.
Li Y, Wang X, Liu Y, Tao J. Dermoscopy predicts outcome in hemoporfin-mediated photodynamic therapy of port-wine stains: a prospective observational study. J Am Acad Dermatol. 2020;83(6):1765–7.
Kwiek B, Rożalski M, Sieczych J, Paluch Ł, Kowalewski C, Ambroziak M. Predictive value of dermoscopy for the treatment of port-wine stains with large spot 532 nm laser. Lasers Surg Med. 2019;51:569–83.
Wang X, Suo H, Gao Y, Du H, Fu Y, Sha S, Liu Y, Su X, An X, Guo X, Li Y, Tao J. Correlation between the hemoporfin-mediated photodynamic treatment response and the dermoscopy vascular pattern in patients with a port-wine stain: a prospective study. J Eur Acad Dermatol Venereol. 2020;34(12):2795–801.
Acknowledgements
The authors thank the patients and their families for allowing us to use their photographs. We thank the entire staff of the operation room of the Department of Dermatology and Venereology of the First Affiliated Hospital of Guangxi Medical University for their invaluable assistance during the procedures.
Funding
This study was supported by grants from the Health Commission of Guangxi Autonomous Region of China (Z20201258 and 2020GXNSFAA297150). This work was also supported by grants from the Natural Science Foundation of Guangxi Province of China (2020GXNSFGA238001) and The First Affiliated Hospital of Guangxi Medical University Provincial and Ministerial Key Laboratory Cultivation Project: Guangxi Key Laboratory of Tropical Fungi and Mycosis Research (no. YYZS2020006). The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have provided final approval of the version to be published.
Authors Contributions
Xin-yu Zhang, Cun-wei Cao and Si-jian Wen designed the study. Xin-yu Zhang, Najwa Al-Odaini, Wen-jun Zheng, Run-ge Fan, Hong-di Xiong, Jia-can Huang, Hong-mei Dai, Yan-hua Zhou, Xiu-yin Huang and Si-jian Wen participated in the treatment process and procedures. Xin-yu Zhang, Najwa Al-Odaini, Cun-wei Cao and Si-jian Wen drafted and wrote the manuscript. All authors have provided final approval of the manuscript.
Disclosures
Xin-yu Zhang, Najwa Al-Odaini, Wen-jun Zheng, Run-ge Fan, Hong-di Xiong, Jia-can Huang, Hong-mei Dai, Yan-hua Zhou, Xiu-yin Huang, Cun-wei Cao and Si-jian Wen declare no conflict of interest.
Compliance with Ethics Guidelines
This study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University, approval number (015). This study was performed in accordance with the Helsinki Declaration. Written informed consent was obtained from the patients' parents or legal guardians before treatment and informed consent was obtained for the possible publication of their digital photographs.
Data Availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, Xy., Al-Odaini, N., Zheng, Wj. et al. The Relationship Between the Effectiveness of HMME-PDT and the Dermoscopic Features of Port-wine Stains in Chinese Pediatric Patients: A Retrospective Study. Dermatol Ther (Heidelb) 12, 1671–1683 (2022). https://doi.org/10.1007/s13555-022-00757-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00757-3