Abstract
Introduction
Polymorphic light eruption (PLE) is the most common idiopathic, acquired photodermatosis. The pathophysiology of PLE is not yet fully understood but seems to involve immunological mechanisms, UVA-induced oxidative stress, and the subsequent elicitation of a cellular stress response affecting keratinocyte gene expression and skin immune function. In the present study, a high broad-spectrum sunscreen medical device (MD), containing a very high protection complex of UVB and UVA filters and ectoin, was investigated for its ability to protect against UVA-induced PLE.
Methods
The study was carried out as a monocentric, double-blinded, randomized, untreated controlled design. The test MD was applied (2 mg/cm2) on one side of the chest according to a randomization list of 15 patients with a typical history of PLE, and the contralateral area remained untreated. After product application, the test areas were exposed daily to increasing doses of UVA radiation (from 40 to 60 J/cm2) until a PLE reaction was detected or for a maximum of five consecutive days. Evaluations of induced PLE included clinical scoring and chromametry for erythema and pigmentation.
Results
Overall, no positive PLE reaction was observed on the side of the chest treated by the test MD, whereas positive PLE reactions were triggered on the untreated side of 13 subjects. Subjective sensations were very rare on the MD-treated side but were numerous and more severe on the untreated side. Chromametry and clinical visual inspection indicated that the skin color was unchanged on the MD-protected side, whereas high increased values of erythema and pigmentation were observed on the untreated chest side.
Conclusion
This MD sunscreen based on a complex of UVA–UVB filters and 1% of ectoin may be effective in preventing UVA-induced PLE. New studies comparing this MD sunscreen versus the same product without ectoin should be conducted.
ClinicalTrials.gov identifier: NCT05320315 (retrospectively registered 09/17/2021).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
PLE is the most common photodermatosis, characterized by abnormal, recurrent, and delayed reaction to sunlight. Patients with PLE experience significant discomfort and loss of quality of life during spring and summer months. |
We assessed the efficacy of a high broad-spectrum sunscreen containing ectoin, a lipid raft stabilizer osmolyte, to prevent UVA-induced PLE. |
What was learned from this study? |
The combination of a very high UVB and UVA protection combined with ectoin provides very effective prevention of UVA-induced PLE. Further studies comparing this MD sunscreen versus the same product without ectoin should be performed. |
Introduction
Polymorphic light eruption (PLE) is the most common photosensitivity disorder in white Caucasians, affecting 11–21% of the population in the Northern Hemisphere, especially affecting more women than men in their second to third decade of life. It seems to be an immunological and genetic-related reaction that causes a skin hypersensitivity reaction, such as eruptions, plaques, bullae, and purpura [1]. Of note, the development of such skin lesions was associated with an increased expression of intercellular adhesion molecule-1 (ICAM-1) in epidermal keratinocytes [2]. PLE lesions occur always after solar or artificial UV-light exposure and affect only the sun-exposed areas, occurring particularly on the V-area of the chest, arms, forearms, legs, and upper part of the back, moreover in the severest forms, also the face. Symptoms always include itching or burning, accompanied with several morphological expressions (i.e., “polymorphous” or “polymorphic”) from erythema to papules, papulovesicles accompanied occasionally by blisters, plaques, sometimes erythema multiforme-like, insect bite-like wheals, and purpura [3]. The clinical manifestations appear within a few hours to days from light exposure, last for a few days, and subside within about a week, while pigmentary sequelae (hyper- or hypopigmentation) may remain. PLE may last for many years for some patients, often recurring annually in the same season, but can improve over time for others, and sometimes even spontaneously remit [4].
Therapy relies mainly on topical or systemic corticosteroids, but also on broad-spectrum sunscreens and antioxidants for prevention. Even using 1 mg/cm2 (less than the guidelines suggest, 2 mg/cm2) of broad-spectrum sunscreens might be beneficial in mild forms [5]. According to the published literature on the PLE, avoidance of UV exposure and the use of high SPF broad-spectrum sunscreens with efficacy against both UVB and UVA can minimize the risk of photosensitivity effects [6, 7]. Previous studies showed that UVA (320–400 nm) radiation is the main triggering factor in PLE [1, 5, 8]. Phototesting may be helpful in confirmation of a photosensitivity disorders, particularly photodermatoses that are immunologically mediated. Once a diagnosis is confirmed, phototherapy can be used in the management of many photodermatoses. Photohardening after photochemotherapy or narrowband UVB may be beneficial in preventing the disorder.
In addition, as the pathogenesis of PLE seems to involve UVA-induced oxidative stress, and subsequent deregulation of antioxidative immune responses [9], the use of topical antioxidants has been proposed to prevent PLE rashes [10, 11]. Ectoin, (S)-2-methyl-1,4,5,6-tetrahydropyrimidine-4-carboxylic acid, is an innovative multifunctional natural active osmolyte substance that has shown protection in humans against UV-induced Langerhans cell depletion and sunburn cell formation. It is capable of preventing UVA radiation-induced gene expression in keratinocytes, and in theory it could be used to protect human skin against PLE [12]. Also, UVA radiation was previously shown to be able to elicit a stress response in human keratinocytes [13], which is initiated at the level of the cell membrane, where it involves a destabilization of lipid rafts [14], and which, as a consequence, causes an increased expression of keratinocyte ICAM-1. Of note, this UVA-induced stress response can be blocked by stabilizing lipid rafts by treating epidermal keratinocytes with the osmolyte ectoin [15].
The objective of the present study was to assess the photo protective efficacy of a medical device (MD) FOTO ULTRA ISDIN SOLAR ALLERGY FUSION FLUID (ISDIN SA, Barcelona Spain) against UVA-induced PLE. This MD is formulated with a combination of sun filters and 1% of ectoin [16].
Methods
This study was conducted in accordance with the ethical principles originating from the Declaration of Helsinki and its amendments, and the ICH guidelines for Good Clinical Practice (GCP) as currently in force, and in compliance with local regulatory requirements. The protocol was approved by the Ethics Committee of Lyon, France (no. 2020-A01487-32). Informed consent was obtained from all subjects before the initiation of the study. The study was carried out as a monocentric, double-blinded, randomized, untreated controlled intra-individual design on the protective efficacy of a MD against UVA-induced polymorphic light eruption (PLE).
Subjects
Fifteen healthy subjects were recruited for the study. The subjects had a known history of typical PLE on the chest after intense sun exposure and had not had a last PLE outbreak in the past 8 months. The subjects must not have been exposed to a source of ultraviolet rays (sun or artificial) for at least 6 months before the study and had to agree not to expose themselves throughout the study. All randomized women of childbearing potential used an effective contraception method for at least 1 month prior to first visit and throughout the study. The subjects agreed to not apply cosmetic, medical, or aesthetic treatments outside of the study protocol on the chest during the whole study duration.
Materials
A solar simulator was used for irradiation (LOT ORIEL, model 92 292, equipped with a 1600 watt high-pressure xenon-vapor lamp). UVB and lower wavelengths were eliminated using a Schott 360/3 mm filter and a UG11 filter was used to exclude visible and infrared light. Thus, the output beam of the lamp comprised UVA light spectrum between 320 and 400 nm, peaking at 360 nm. The light source intensity was measured using dosimeter UV-meter PMA 2100 (SOLAR LIGHT, USA) as described in COLIPA and/or FDA guidelines.
Study Design
The study consisted of a screening visit followed by six evaluation visits (days 1, 2, 3, 4, 5, and 8) and was performed as follows:
At day 1, the investigator delineated one 10 × 15 cm2 test site on each side of the subject’s chest. Double baseline colorimetric measurements and a standardized photograph of the chest were performed. Then, the test product was applied (2 mg/cm2) on one side of the chest according to a randomization list. The other side remained untreated. Fifteen minutes after test product application, both test sites received a dose of 40 J/cm2 of UVA radiation from a solar simulator. Five to 6 hours after exposure, the investigator performed clinical assessments (erythema, papules, vesicles, pigmentation, and PLE severity) on both test sites and recorded subjective sensations (itching, burning).
From day 2 to 5, the same protocol as day 1 was reproduced, except that the UVA dose was increased after day 2 (50 J/cm2 at day 3 and day 4 and 60 J/cm2 at day 5).
The presence of erythema, papules, or vesicles was scored at days 1, 2, 3, 4, and 5 before and 5–6 hours after exposure, and at day 8 using a 5-point grading scale (0, absence; 0.5, doubtful; 1, weak but well defined; 2, moderate; 3, severe). Development and severity of PLE were scored following the scoring system derived from Hadshiew [10] and detailed in Table 1.
UVA exposures were to be stopped on the concerned site if positive PLE reactions were triggered. The UVA exposures continued on the test site presenting no PLE reactions. Safety was assessed by adverse events evaluation from day 1 to 8.
Itching and burning, if any, were evaluated at each time point before and 5–6 hours after exposure and at day 8 on both sides of the chest using a 0–10 numerical rating scale (0, no symptom; 1–3, mild; 4–6, moderate; 7–9, severe; 10, the worst imaginable [17]).
The intensity of the induced pigmentation was assessed by a trained investigator using an internal visual scale [18] ranging from 0 to 9 (including 0.5 for doubtful pigmentation). The assessment is based on the comparison of the pigmentation of the test zone with that of the surrounding unexposed control skin. The different levels are as follows: “no difference,” “doubtful pigmentation,” “very pale brown,” “pale brown,” and “brown” with three grading modulations for the three last levels (e.g., brown−, brown, and brown+).
Erythema and pigmentation were also measured using a CR 400 chromameter (Konica Minolta,Osaka, Japan) in the L*a*b* system (CIE color space). The component L* is related to skin lightness (0, black; 100, white), a* is related to erythema (red color), and b* to the yellow component of the skin color. The ITA° angle, given by the formula: ITA° = (arctan((L* − 50)/b*) × 180)/π is well correlated with skin pigmentation [19].
The test medical device (MD) (FOTO ULTRA ISDIN SOLAR ALLERGY FUSION FLUID) was provided by ISDIN S.A. (Barcelona, Spain). It is a class I medical device commercialized in Europe and elsewhere since 2013. It contains a combination of UVA and UVB filters (octocrylene 8%, titanium dioxide 5%, butyl methoxydibenzoylmethane 3.6%, bis-ethylhexyloxyphenol methoxyphenyl triazine 3%) and 1% of ectoin. This formulation offers a very high photo protection level (sun protection factor, SPF > 100 and UVA protection factor, UVA PF = 40).
To illustrate the effects of the treatment, standardized photographs of the chest were systematically taken at each time point before exposure and at day 8, and in case of PLE positive reactions at 5–6 hours after exposure.
Statistics
Statistical analyses were performed using R software version 4.0.2. The primary endpoint was the cumulative number of subjects who did not develop a positive PLE reaction (cumulated to day 8). The photo-protected treated and the untreated zones were compared using a McNemar test performed at a 5% two-sided significance level.
The PLE severity scores were summarized by treatment at each study visit. Since UVA exposures had to be stopped on the chest site once positive PLE reactions were observed, then the PLE score attributed to this site for the remaining days was the worst PLE score observed for the subject during the whole study. A mixed effect model was applied. The model includes the treatment, the visit, and the interaction treatment × visit as fixed effects and the subject as random effect. For the time taken to develop a PLE reaction, the test MD and the untreated zone were compared using a McNemar test performed at a 5% two-sided significance level.
A sample size calculation indicated that a group of 15 subjects would allow the detection of a significant difference of 11 subjects or more with positive PLE between the photo-protected side and the untreated one with 90% probability and at the α risk of 0.05.
Results
Subjects
Fifteen subjects, 13 women and 2 men, with a mean age of 44 ± 11 years (range 25–57 years) were included in the study. Ten subjects were Fitzpatrick Skin Type III, 4 were Skin Type IV, and 1 was Skin Type I (ITA° range 36–64°). All patients completed the study, but one subject missed the last visit (day 8). There was no major protocol deviation during this study.
PLE Reactions
Table 2 displays the cumulative number of subjects who did and did not develop a positive PLE reaction (primary endpoint) over the entire study. This table indicates that no positive PLE reaction was observed on the side protected by the test MD, whereas positive PLE reactions (with a minimum score grade 1) were triggered on the untreated side of 13 subjects. No PLE reaction was triggered on the untreated side for two subjects. Therefore, efficacy of the test MD was highly statistically significant (p < 0.001) in protecting against UVA-induced PLE versus untreated skin.
The cumulative number of subjects with no positive PLE reaction over time is summarized in Fig. 1. This figure indicates that the first PLE triggered was observed on the untreated side at day 2, 6 h after the UVA exposure. The difference between both untreated and protected chest sites became significant (p = 0.013) from day 4 before exposure (only a difference tendency was observed at day 3 + 6 h, p = 0.074).
Regarding the PLE symptoms on the side of the chest protected by the test MD, only two doubtful and one weak erythema, one doubtful papule, and no vesicles score were observed. On the other hand, on the untreated side, most of the worst erythema scores were severe (grade 3, n = 10) or moderate (grade 2, n = 4), and most of the worst papules scores were moderate (grade 2, n = 3) or weak but well defined (grade 1, n = 7). Additionally, one weak but well-defined vesicles score (grade 1) was reported on the untreated side. No severe PLE score was recorded.
The PLE worst severity scores observed during the study are shown in Fig. 2 (percentage rounded values).
Concerning the subjective sensations, only one patient reported moderate burning and itching reactions on the side of the chest protected by the MD, whereas numerous moderate to severe reactions were seen on the untreated side. The worst subjective scores for itching and burning observed during the study are displayed in Fig. 3 (percentage rounded values).
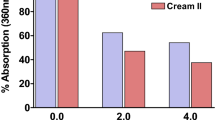
Chromametry measurements indicated that the skin color was unchanged on the side of the chest protected by the test MD, whereas on the untreated chest side increased values of a* (erythema), and ITA (skin color), and decreased values of L* (skin lightness) were observed. Evolution of parameter a* on both sides is shown in Fig. 4a.
a Chromametry parameter a* over time. Error bars represent standard error of mean (SEM). Double stars (**) indicate significant difference (p < 0.001). b Chromametry parameter ITA over time. Error bars represent standard error of mean (SEM). Double stars (**) indicate significant difference (p < 0.001)
The evolution of the colorimetry parameter ITA, expressing skin color, is shown in Fig. 4b. Note, when ITA decreases, skin color intensity increases.
Concerning visual scores of pigmentation, no induced pigmentation was observed on the protected chest side, whereas a clearly visible pigmentation was seen on the untreated side. Visual scores of pigmentation showed a similar evolution as that observed with ITA angle (see Fig. S1 in the electronic supplementary material for details).
Comparison of protected chest side (left) versus unprotected chest side (right) is illustrated for one subject in Fig. 5.
No local safety concerns and no AEs were observed in this study.
Discussion
PLE is the most common photodermatosis, characterized by abnormal, recurrent, and delayed reaction to sunlight. Patients with PLE experience significant discomfort and loss of quality of life during spring and summer months [20, 21]. High levels of anxiety and depression can occur in patients with PLE [22]. Young patients, as well as patients with facial involvement, may need psychological management [23].
In most cases, PLE may be prevented by avoiding sun exposure, wearing protective clothing, and, most importantly, regularly using broad-spectrum sunscreens, in particular during the first exposure of the year. New generation broad-spectrum sunscreens, with high sun protection factors for UVB (SPF), together with longer wavelength UVA protection, have been reported to confer total or partial protection in up to 90% of patients with PLE [24]. Also, topical application of an antioxidant-containing skin care product appears to provide protection against UV-induced development of skin lesions in patients with PLE [25, 26]. Several lines of evidence indicate that reactive oxygen species are involved in the pathogenesis of PLE [10, 27].
Concerning the methodology used in this the study, some specificities can be outlined: (1) the small sample size (n = 15) was previously shown [5, 28] to be enough to detect product activity for UVA-induced PLE owing to the intra-individual design, which increases the power of the test; and (2) the design treated versus untreated, which mimics “real life” conditions, has previously been published [29].
In the present study, the MD included a very high protection UV filters complex, and ectoin was investigated for its ability to protect against UVA-induced PLE. The results indicated that no PLE reaction was triggered on the side protected by the MD, whereas positive PLE reactions were observed on the untreated side of 13 out of 15 subjects (87%). No PLE reaction was triggered on the untreated side of two subjects. This percentage is quite good for photoprovocative test results. Guarrera [30] reported that the positivity of photoprovocative tests range from 47% up to 90%. The discrepancy may depend on the numbers of variables, such as the different light sources, the number of UV exposures or different UV light doses, the size of the irradiated skin area (exposed or not exposed, previously affected by lesions or not), and the season in which the phototest is done. In our study, the difference between both untreated and protected areas was highly significant (p < 0.001). Subjective sensations were very rare on the side protected by the MD and remain mild to moderate, while they were numerous and moderate to severe on the untreated side.
No severe PLE reactions were observed in this study as is usually observed in studies where PLE are experimentally provoked and the PLE reactions are triggered generally after 3–4 days of UVA exposure [8, 29].
Another interesting point is that colorimetry measurements and clinical visual inspection indicated that the skin color was unchanged on the side of the chest protected by the MD, whereas high increased values of a* (erythema) and decreased ITA (increase of skin color) were observed on the untreated chest side.
UVA rays are known to induce skin pigmentation [29]. UVA-induced changes in color begin with an immediate darkening of the skin due to photo-oxidation of preexisting melanin. The dark-blue color is called immediate pigment darkening (IPD). This pigment fades rapidly (within 2 h) after UVA exposure, but a residual pigmentation called persistent pigment darkening (PPD) is observed and may remain detectable for many weeks depending on UVA dose and skin type. This neo-melanization is owing to an increased synthesis of melanin caused by intense UVA exposure. In our study, absence of erythema and pigmentation induction implies that the tested MD offers a complete protection against PLE triggering effect of UVA in all subjects.
The MD tested in this study combines two protection approaches: (1) a complex of UVA–UVB filters that reduce the quantity of UV radiation entering into the skin, and (2) the incorporation of ectoin, an osmolyte that inhibits UVA-induced stress responses. The weakness of this study is that this design does not allow the estimation of the relative contribution of ectoin versus UV filters in the prevention of PLE induced by UVA. To demonstrate any advantage that ectoin may provide, studies comparing MD product versus nonprotected, MD product versus only the product without ectoin, and eventually MD product versus ectoin alone should be conducted.
Conclusions
In conclusion, this MD sunscreen, based on a complex of UVA–UVB filters and 1% of ectoin, may be effective in preventing UVA-induced PLE, but new studies comparing this MD sunscreen versus the same product without ectoin should be conducted.
References
Gruber-Wackernagel A, Byrne SN, Wolf P. Polymorphous light eruption: clinical aspects and pathogenesis. Dermatol Clin. 2014;32:315–34.
Stephansson E, Ros AM. Expression of intercellular adhesion molecule-1 (ICAM-1) and OKM5 in UVA- and UVB-induced lesions in patients with lupus erythematosus and polymorphous light eruption. Arch Dermatol Res. 1993;285(6):328–33. https://doi.org/10.1007/BF00371832.
Hölzle E, Plewig G, von Kries R, et al. Polymorphous light eruption. J Invest Dermatol. 1987;88(3 Suppl):32s–8s.
Hasan T, Ranki A, Jansen CT, et al. Disease associations in polymorphous light eruption. A long-term follow-up study of 94 patients. Arch Dermatol. 1998;134:1081–5.
Bissonnette R, Nigen S, Bolduc C. Influence of the quantity of sunscreen applied on the ability to protect against ultraviolet-induced polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2012;28:240–3.
Gozali MV, Zhou B, Luo D. Update on treatment of photodermatosis. Dermatol Online J. 2016;22:2.
Schleyer V, Weber O, Yazdi A, Benedix F, Dietz K, Röcken M, Berneburg M. Prevention of polymorphic light eruption with a sunscreen of very high protection level against UVB and UVA radiation under standardized photodiagnostic conditions. Acta Derm Venereol. 2008;88(6):555–60.
Schaefer H, Moyal D, Fourtanier A. State of the art sunscreens for prevention of photodermatoses. J Dermatol Sci. 2000;23(1):S62–74.
Ahmed RS, Suke SG, Seth V, Jain A, Bhattacharya SN, Banerjee BD. Impact of oral vitamin E supplementation on oxidative stress & lipid peroxidation in patients with polymorphous light eruption. Indian J Med Res. 2006;2016:8.
Hadshiew IM, Treder-Conrad CV, Bülow R, Klette E, Mann T, Stäb F, et al. Polymorphous light eruption (PLE) and a new potent antioxidant and UVA-protective formulation as prophylaxis. Photodermatol Photoimmunol Photomed. 2004;20(4):200–4.
Rippke F, Wendt G, Bohnsack K, Dörschner A, Stäb F, Hölzle E, et al. Results of photoprovocation and field studies on the efficacy of a novel topically applied antioxidant in polymorphous light eruption. J Dermatol Treat. 2001;12(1):3–8.
Buenger J, Driller H. Ectoin: an effective natural substance to prevent UVA-induced premature photoaging. Skin Pharmacol Physio. 2004;17:232–7.
Grether-Beck S, Bonizzi G, Schmitt-Brenden H, Felsner I, Timmer A, Sies H, Johnson JP, Piette J, Krutmann J. Non-enzymatic triggering of the ceramide signalling cascade by solar UVA radiation. EMBO J. 2000;19(21):5793–800. https://doi.org/10.1093/emboj/19.21.5793.
Grether-Beck S, Salahshour-Fard M, Timmer A, Brenden H, Felsner I, Walli R, Füllekrug J, Krutmann J. Ceramide and raft signaling are linked with each other in UVA radiation-induced gene expression. Oncogene. 2008;27(35):4768–78. https://doi.org/10.1038/onc.2008.116.
Grether-Beck S, Timmer A, Felsner I, Brenden H, Brammertz D, Krutmann J. Ultraviolet A-induced signaling involves a ceramide-mediated autocrine loop leading to ceramide de novo synthesis. J Invest Dermatol. 2005;125(3):545–53. https://doi.org/10.1111/j.0022-202X.2005.23782.x.
Bünger J, Degwert J, Driller H. The protective function of compatible solute ectoin on the skin, skin cells and its biomolecules with respect to UV-radiation, immunosuppression and membrane damage. IFSCC-Magazine. 2001;4:2.
Phan NQ, Blome C, Fritz F, et al. Assessment of pruritus intensity: prospective study on validity and reliability of the visual analogue scale, numerical rating scale and verbal rating scale in 471 patients with chronic pruritus. Acta Derm Venereol. 2012;92(5):502–7. https://doi.org/10.2340/00015555-1246.
Duteil L, Esdaile J, Maubert Y, Cathelineau AC, Bouloc A, Queille-Roussel C, Passeron T. A method to assess the protective efficacy of sunscreens against visible light-induced pigmentation. Photodermatol Photoimmunol Photomed. 2017;33(5):260–6. https://doi.org/10.1111/phpp.12325.
Chardon A, Crétois I, Hourseau C. Skin colour typology and suntanning pathways. Int J Cosm Scien. 1991;125:191–208.
Ling TC, Richards HL, Jansen AS, et al. Seasonal and latitudinal impact of polymorphic light eruption on quality of life. J Invest Dermatol. 2006;126(7):1648–51. https://doi.org/10.1038/sj.jid.5700306.
Richards HL, Ling TC, Evangelou G. Psychologic distress in polymorphous light eruption and its relationship to patients’ beliefs about their condition. J Am Acad Dermatol. 2007;56(3):426–31. https://doi.org/10.1016/j.jaad.2006.10.035.
Richards HL, Ling TC, Evangelou G. Evidence of high levels of anxiety and depression in polymorphic light eruption and their association with clinical and demographic variables. Br J Dermatol. 2008;159(2):439–44.
Rizwan M, Haylett AK, Richards HL. Impact of photosensitivity disorders on the life quality of children. Photodermol Photoimmunol Photomed. 2012;28(6):290–2.
Allas S, Lui H, Moyal D, Bissonnette R. Comparison of the ability of 2 sunscreens to protect against polymorphous light eruption induced by a UV-A/UV-B metal halide lamp. Arch Dermatol. 1999;135(11):1421–2. https://doi.org/10.1001/archderm.135.11.1421.
Jeanmougin M, Peyron JL, Thomas P. Polymorphic light eruption: prophylaxis using a topical combination of antioxidants and UVA protection formulation. Ann Dermatol Venereol. 2006;133(5 Pt 1):425–8. https://doi.org/10.1016/s0151-9638(06)70932-2.
Rippke F, Wendt G, Bohnsack K, et al. Results of photoprovocation and field studies on the efficacy of a novel topically applied antioxidant in polymorphous light eruption. J Dermatolog Treat. 2001;12(1):3–8. https://doi.org/10.1080/095466301750163491.
Hadshiew I, Stäb F, Untiedt S, Bohnsack K, et al. Effects of topically applied antioxidants in experimentally provoked polymorphous light eruption. Dermatology. 1997;195(4):362–8. https://doi.org/10.1159/000245989.
Schleyer V, Weber O, Yazdi A, et al. Prevention of polymorphic light eruption with a sunscreen of very high protection level against UVB and UVA radiation under standardized photodiagnostic conditions. Acta Derm Venereol. 2008;88(6):555–60. https://doi.org/10.2340/00015555-0509.
Fourtanier A, Moyal D, Seité S. Sunscreens containing the broad-spectrum UVA absorber, Mexoryl SX, prevent the cutaneous detrimental effects of UV exposure: a review of clinical study results. Photodermatol Photoimmunol Photomed. 2008;24(4):164–74. https://doi.org/10.1111/j.1600-0781.2008.00365.x.
Guarrera M. Polymorphous light eruption. Adv Exp Med Biol. 2017;996:61–70. https://doi.org/10.1007/978-3-319-56017-5_6.
Galinski EA. Compatible solutes of halophilic eubacteria: molecular principles, water-solute interaction, stress protection. Experienta. 1993;49:487–96.
Botta C, Di Giorgio C, Sabatier AS, et al. Genotoxicity of visible light (400–800 nm) and photoprotection assessment of ectoin, L-ergothioneine and mannitol and four sunscreens. J Photochem Photobiol B. 2008;91(1):24–34. https://doi.org/10.1016/j.jphotobiol.2008.01.008.
Bownik A, Stępniewska Z. Ectoine as a promising protective agent in humans and animals. Arh Hig Rada Toksikol. 2016;67(4):260–5. https://doi.org/10.1515/aiht-2016-67-2837.
Acknowledgements
We would like to thank Jane Murray and Yves Maubert for technical assistance and also Anne-Claire Cathelineau for the statistical analyses. We are very grateful to our volunteers who agreed to take part in this study.
Funding
Sponsorship for this study and the journal’s Rapid Service Fee was provided by ISDIN SA (Barcelona, Spain).
Authorship
All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by L. Duteil, C. Queille-Roussel and C. Granger. The first draft of the manuscript was written by L. Duteil and all named authors commented on previous versions of the manuscript. All named authors read and approved the final manuscript.
Disclosures
Sonia Aladren, Xavier Bustos and Carles Turllas are ISDIN’s employees, Corinne Granger was employed by ISDIN when designing, running the clinical study and analysing the data. Jean Krutmann and Thierry Passeron are paid consultants by ISDIN. Catherine Queille-Roussel was the clinical investigator of the study and Luc Duteil was the CPCAD study manager.
Compliance with Ethics Guidelines
The Ethics Committee of Lyon, France approved the study, under the project reference N° 2020-A01487-32. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments, and all subjects provided informed consent to participate.
Data Availability
The datasets generated during and analyzed and/or during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Duteil, L., Queille-Roussel, C., Aladren, S. et al. Prevention of Polymorphic Light Eruption Afforded by a Very High Broad-Spectrum Protection Sunscreen Containing Ectoin. Dermatol Ther (Heidelb) 12, 1603–1613 (2022). https://doi.org/10.1007/s13555-022-00755-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00755-5