Abstract
Introduction
Dupilumab was initially approved in 2017 as the first biologic therapy for atopic dermatitis (AD). We characterized adults with AD initiating dupilumab in a real-world setting in the USA/Canada.
Methods
PROSE is an ongoing, longitudinal, prospective, observational, multicenter registry of patients with AD initiating dupilumab per country-specific prescribing information. We report baseline data (day of first dupilumab injection) for patients enrolled from April 2018 through July 2019.
Results
Among 315 patients (mean age 42.5 years, 55.2% female), the median AD duration was 17.0 years; 65.4% reported a history of type 2 inflammatory comorbidities (e.g., allergic rhinitis, asthma), and 93.3% reported treatment(s) for AD in the previous year, including topical corticosteroids (90.8%), systemic corticosteroids (36.2%), and nonsteroidal systemic therapies (14.0%). In total, 89.2% had an Overall Disease Severity score of 3 (moderate) or 4 (severe). Other mean disease severity scores included the following: Eczema Area and Severity Index 16.9 (range 0–72), body surface area affected 26.8%, Patient-Oriented Eczema Measure 18.5 (range 0–28), Dermatology Life Quality Index 12.7 (range 0–30), and pruritus Numerical Rating Scale score 6.9 (range 0–10).
Conclusion
Patients initiating dupilumab have longstanding moderate-to-severe AD with significant disease burden and frequent type 2 comorbidities.
ClinicalTrials.gov Identifier
NCT03428646.
Video Abstract (MP4 23,650 kb)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Dupilumab was initially approved in 2017 as the first biologic therapy for atopic dermatitis (AD). |
Patients with AD enrolled in dupilumab clinical trials had considerable disease burden, and this is also true for most patients receiving dupilumab treatment by prescription in the real world. |
We analyzed adults in the PROSE registry study (an ongoing, longitudinal, prospective, observational, multicenter registry of US and Canadian patients with AD initiating dupilumab in a real-world setting) with respect to sociodemographics, history of AD, and other type 2 inflammatory comorbidities, AD treatment history, and disease severity measured by physician assessments and patient-reported outcomes. |
What was learned from the study? |
Real-world patients who initiated dupilumab had variable AD signs, symptoms, quality of life impact, and past/current treatments. |
Physician assessments alone appeared to underestimate disease burden, highlighting the importance of patient-reported outcomes when selecting appropriate treatments for moderate-to-severe disease. |
Digital Features
This article is published with digital features, including a video abstract, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.19535917.
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by pruritus, eczematous lesions, and upregulation of type 2 immune responses [1,2,3]. AD was traditionally thought to start in childhood and improve with age [4, 5]. However, data increasingly suggest that AD often continues into, or can even start during, adulthood [1, 4,5,6]. Recent cross-sectional evidence shows a prevalence of AD of 7.3% (16.5 million cases) among adults in the USA, of which 6.6 million (40%) are moderate to severe in severity [7]. AD can have a profound impact on quality of life (QoL) and has been associated with increased risk of depression and anxiety [7,8,9]. Patients with AD are also at increased risk of other inflammatory diseases driven by type 2 cytokines, e.g., asthma and allergic rhinitis [1, 10].
Dupilumab (Dupixent, Regeneron Pharmaceuticals, Inc., NY)—a fully human VelocImmune-derived [11, 12] monoclonal antibody—blocks the shared receptor alpha component for interleukins 4 and 13, thus inhibiting signaling of both cytokines. Dupilumab clinical trials have shown that these cytokines are key drivers of type 2 inflammation, which play a major role in AD [13,14,15,16,17], asthma [18], chronic rhinosinusitis with nasal polyposis [19, 20], and eosinophilic esophagitis [21]. In the USA and Canada, dupilumab is approved for the treatment of patients aged ≥ 6 years with moderate-to-severe AD not adequately controlled by topical prescription medications (or when these are not advisable) [22, 23]. Dupilumab is also indicated as add-on maintenance treatment for patients aged ≥ 6 years (USA) or ≥ 12 years (Canada) with moderate-to-severe asthma with eosinophilic phenotype, oral corticosteroid-dependent asthma, and adults with inadequately controlled chronic rhinosinusitis with nasal polyposis [22, 23].
There is a lack of data on patients receiving dupilumab for AD in a real-world setting. Thus, the PROSE registry will study patients, treatment practices, and dupilumab effectiveness and safety in US and Canadian patients with AD who initiated dupilumab in a real-world setting. We analyzed adults in PROSE with respect to sociodemographics, history of AD and other type 2 inflammatory comorbidities, AD treatment history, and disease severity measured by physician assessments and patient-reported outcomes (PROs).
Methods
Study Design
The PROSE registry (ClinicalTrials.gov Identifier NCT03428646) is an ongoing, longitudinal, prospective, observational study of adolescents and adults with physician-diagnosed AD who initiated dupilumab, prescribed according to country-specific prescribing information in the USA and Canada. AD was diagnosed according to physicians’ clinical judgment in routine practice, as the study protocol did not mandate standardized diagnostic criteria. Consecutive patients with AD at each study site who receive an initial prescription for dupilumab are invited to participate. This interim analysis includes data from adults with a first-ever prescription of dupilumab for AD from 6 April 2018 through 28 July 2019. Appropriately constituted institutional review boards approved the study (Supplementary Table 1), which was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and is consistent with applicable regulatory requirements.
Patients
For this interim analysis, eligible patients were aged ≥ 18 years, initiated dupilumab as standard of care for AD according to country-specific prescribing information [22, 23], were willing and able to comply with study-related activities and understand and complete study-related questionnaires, and provided informed consent. Exclusion criteria included contraindication for dupilumab, any condition that could interfere with the patient’s ability to participate, and prior use of dupilumab within 6 months.
Assessments
Baseline assessments were performed on the day of initial dupilumab administration. Baseline characteristics included sociodemographics, specialty of the prescriber, AD history, history of certain type 2 inflammatory comorbidities, AD treatment history, and AD characteristics.
Physician-rated AD assessments included Eczema Area and Severity Index (EASI; scale 0–72), Overall Disease Severity (ODS) score, and body surface area (BSA) affected by AD (%). For the ODS, the physician gave a rating of 0 (no), 1 (minimal), 2 (mild), 3 (moderate), or 4 (severe disease) to the question: “Taking into account all important aspects characterizing the severity of AD, how would you grade your patient’s AD at this time?”.
The following PROs were collected: Patient-Oriented Eczema Measure (POEM) (scale 0–28), Numerical Rating Scale (NRS) measures of skin symptoms and sleep (scale 0–10), and Dermatology Life Quality Index (DLQI) (scale 0–30) (all with higher scores indicating more severe disease/symptoms); Patient Global Assessment of Atopic Dermatitis (PGAD) and Patient’s overall Assessment of Health State (PAHS) (both scale 1–5, with higher scores indicating less severe disease); Health Care Resource Utilization Questionnaire (HCRUQ; patients were asked “Over the past 3 months, have you been hospitalized, or visited the emergency room or an urgent care center because of your eczema? If yes, what was the reason?”; the number of hospitalization days and the number of urgent care or emergency room visits were also recorded); and Work Productivity and Activity Impairment Questionnaire for Atopic Dermatitis (WPAI-AD; a six-item, validated questionnaire to measure impairments in work and activities over the past 7 days; outcomes are expressed as percentages, with higher numbers indicating greater impairment/less productivity).
Statistical Analysis
An interim analysis dataset composed of all adults who were eligible and consented to participate in the study from 6 April 2018 through 28 July 2019 was used to analyze baseline demographics, disease, and treatment history. For continuous variables, descriptive statistics included means and standard deviations (SDs) or medians with interquartile ranges (IQRs); for categorical or ordinal data, frequencies and percentages were used.
Results
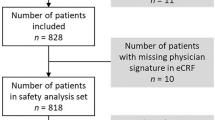
Among 399 patients who received a dupilumab prescription and agreed to participate, 315 (78.9%) initiated treatment with dupilumab and were included in this analysis (280 in the USA and 35 in Canada). The main reasons for exclusion were failure to initiate dupilumab within the protocol-defined 84 days following a prescription (55 patients), consent withdrawn (8 patients), and inclusion criteria not met or exclusion criteria met (6 patients). The median (IQR) time from prescription to treatment initiation was 26 (11–46) days. The delay was mainly due to the need to obtain approval for the prescription from their insurance company and schedule an appointment for administering the injection.
Baseline Sociodemographic Characteristics
The mean (SD) age was 42.5 (17.0) years, and 55.2% were female (Table 1). Most patients had private health insurance or belonged to a health maintenance organization (66.7%); 57.8% had at least a college education; and 60.0% were employed/self-employed (Table 1). Most prescribers (96.5%) were dermatologists and/or allergists (Table 1).
AD History
The median (IQR) age at AD diagnosis was 16.0 (3.0, 44.0) years, and the median (IQR) duration of AD was 17.0 (4.0, 30.0) years (Table 2). Overall, 34.9% of patients had a family history of AD.
History of Type 2 Inflammatory Comorbidities
The majority of patients (65.4%) reported a history of one or more type 2 inflammatory comorbidities, most commonly allergic rhinitis (34.9%) and asthma (29.2%); and 38.7% had ≥ 2 type 2 inflammatory comorbidities (Table 2).
AD Treatment History
All patients reported ever receiving prior AD treatment(s), with 93.3% reporting this during the past year (Table 3). Most patients (92.7%) had ever received topical corticosteroids, and 38.4% had received topical calcineurin inhibitors (Table 3). Overall, 49.5% of patients had ever received systemic AD treatment(s): 41.0% systemic corticosteroids and 16.8% nonsteroidal systemic therapies (e.g., methotrexate, cyclosporine) (Table 3). Phototherapy was reported by 10.2% of patients (Table 3). Treatments during the previous 12 months, along with treatment durations, are detailed in Table 3.
A total of 41.9% of patients were receiving AD medication at baseline: 39.0% topical and 6.0% systemic (Table 3).
Baseline Disease Characteristics and Burden
The most common type 2 inflammatory comorbidities that were active (i.e., symptomatic and/or requiring treatment) at baseline were allergic rhinitis (22.5%), asthma (15.2%), allergic conjunctivitis (9.8%), and food allergies (9.5%) (Table 4). Overall, the population enrolled in PROSE had moderate-to-severe AD, as assessed by physicians and PROs. The mean (SD) EASI was 16.9 (13.4) (i.e., moderate) [24]; 55.9% and 33.3% of patients were suffering from moderate and severe disease, respectively, according to ODS (Table 4).
The mean (SD) POEM score was 18.5 (6.7), consistent with moderate-to-severe disease [25,26,27], and the mean (SD) DLQI was 12.7 (7.5) (i.e., severe effect on QoL) [26, 27] (Table 4). Mean (SD) NRS scores ranged from 6.9 (2.3) for pruritus to 4.6 (3.1) for skin feeling hot.
Four of 227 patients who completed the HCRUQ had been hospitalized for AD [mean (SD) duration: 4.8 (4.4) days] and 26 of 226 patients had visited the emergency room during the previous 3 months for reasons such as eczema flare (n = 26), unbearable itch (n = 22), skin infection (n = 10), or other AD-related reasons (n = 8). From the WPAI-AD, during the previous 7 days, the mean (SD) percent work time missed due to AD was 4.7% (16.9%) (n = 129); AD-related impairment while working was 35.6% (31.7%) (n = 208); overall work impairment due to AD was 34.3% (28.7%) (n = 126); and activity impairment due to AD was 44.1% (32.3%) (n = 220).
Stratification of Baseline ODS by Other Measures
Physician-assessed ODS correlated well with physician-assessed EASI, and patients with moderate disease by ODS had, on average, moderate disease by EASI, etc. (Fig. 1) [24]. However, ODS seemed to underestimate overall AD severity compared with PROs. On average, patients with physician-assessed mild or moderate ODS self-assessed their disease as moderate or severe by POEM and having a moderate-to-severe effect on their QoL by DLQI (Fig. 1) [25,26,27].
Disease characteristics (EASI, POEM, DLQI) by ODS. aEASI scale 0–72, with 0–1 indicating clear/almost clear; 1.1–7, mild; 7.1–21, moderate; 21.1–50, severe; and 50.1–72, very severe [24]. bPOEM scale 0–28, with 0–2 indicating clear/almost clear mild; 0–7 or 3–7, mild; 8–16 or 8–19, moderate; 17–24, 17–28, or 20–28, severe; 25–28, very severe [25,26,27]. cDLQI scale 0–30, with 0–5 indicating mild; 6–10, moderate; 11–30, severe [26, 27]. DLQI Dermatology Life Quality Index, EASI Eczema Area and Severity Index, NA not available, ODS Overall Disease Severity, POEM Patient-Oriented Eczema Measure, PRO patient-reported outcome, SD standard deviation
The correlation between baseline EASI total score and baseline pruritus NRS was low (Pearson correlation coefficient 0.227).
Discussion
This analysis of the sociodemographic and AD characteristics of adults receiving a first prescription for commercially available dupilumab at selected sites in the USA and Canada shows a considerable reduction in the disease burden, with prevalent AD signs, itch, and impacted QoL despite treatment with topical and/or systemic therapies.
Patients enrolled in PROSE had a longstanding history of AD, with a median of 17.0 years since diagnosis. Two-thirds of patients had private health insurance/health maintenance organization coverage, over half had a college education, and 60.0% were employed, showing a good representation of a real-world population.
Almost two-thirds of the patients had a history of type 2 inflammatory comorbidities, and more than half of these had two or more type 2 inflammatory comorbidities. Nearly all patients had received AD treatment(s) in the previous year, with nearly half of them having received systemic treatment. Most patients had moderate or severe AD on the day of first dupilumab injection per physician assessment (EASI and ODS), but the mean patient-reported severity was generally in the severe range, as was the mean impact on QoL. Of note, we piloted the use of ODS, which is a basic questionnaire not previously used in studies. ODS prompts the investigator to provide a physician global assessment, considering “all important aspects” that characterize AD severity. ODS was included on an exploratory basis as an alternative to the Investigator Global Assessment (IGA), which has been widely used in clinical trials to assess AD severity but is limited to acute features of lesion severity (erythema and induration/papulation) and does not take into account other important elements of AD severity, such as affected BSA, itch, sleep loss, QoL, frequency and duration of AD exacerbations, and treatment response [28]. While ODS does not specifically evaluate individual elements of disease severity (e.g., AD lesion extent and severity, patient complaints, frequency and severity of exacerbations, response to treatment, etc.), we hoped that, as a physician global assessment tool, ODS would better characterize AD severity by opening up the assessment to “all important aspects” of the patient’s AD.
The baseline characteristics of adults in the current US dupilumab registry can be compared with those of patients from two published observational studies. The Japanese ADDRESS-J AD registry included adults with moderate-to-severe AD (IGA 3 or 4; scale 0–4), none of whom received dupilumab [29]. The TREatment of ATopic eczema, the Netherlands (TREAT NL) dupilumab registry included adult AD patients who started dupilumab in routine clinical care, which is available in the Netherlands after patients receive ≥ 4 months of treatment with at least one conventional systemic therapy at an adequate dose [30]. Patients in PROSE had less severe AD than those in ADDRESS-J or TREAT NL when assessed by EASI, but more severe AD than those in ADDRESS-J and less severe AD than those in TREAT NL when assessed by POEM or DLQI [29, 30]. The lower disease burden in PROSE compared with TREAT NL (in which all patients received dupilumab) may be due to the more stringent inclusion criterion in TREAT NL and/or the different health care systems in the USA and the Netherlands.
In TREAT NL [30], all patients had received systemic treatments (as per the national criteria in the Netherlands), mainly cyclosporine (89.1%), corticosteroids (61.5%), and methotrexate (46.6%) [30], while 44.8% of patients in PROSE reported systemic AD treatment in the previous year. In ADDRESS-J [29], topical treatments were widely reported as the most recent treatment before baseline (86.7%), while only 39.0% of patients in PROSE reported using a topical treatment at baseline. Another difference in the treatment patterns in the three registries is that, in PROSE and ADDRESS-J [29], very few patients had undergone phototherapy, while 75.1% of patients had undergone previous phototherapy in TREAT NL [30]. This could be due to different treatment availabilities and/or preferences in the USA, Japan, and the Netherlands, or could be related to the differences in the disease severity. Treatment differences aside, results from all three registries show that despite treatment with topical therapies, systemic therapies, and phototherapy, disease severity remained high, showing an unmet need for these patients with AD.
In PROSE, we found good agreement between physician-reported measures but poor correlations between these and PROs. Similar findings were reported in ADDRESS-J [29], showing that physicians can underestimate the impact of AD. Clearly, the different assessment tools each capture distinct features of AD, i.e., itch, lesional symptoms, QoL, etc. Hence, multiple tools are required to sufficiently characterize disease severity.
The real-world patients in PROSE are somewhat different from the patients in pivotal phase 3 dupilumab AD studies [31]. PROSE patients were more likely to be female (55% versus 37–46% across arms in SOLO 1 and 2, CHRONOS, and CAFÉ) and had lower physician-assessed AD severity (median affected BSA: 19% versus 51–59%; EASI: 14 versus 29–32) but similar PROs (median POEM: 19 versus 19–22; DLQI: 12 versus 13–15) [31]. This in part reflects the strict entry criteria for the phase 3 trials, which mandated a baseline EASI ≥ 16 (SOLO 1 and 2 [32], CHRONOS [13]) or ≥ 20 (CAFÉ [15]), and an IGA score ≥ 3. Further, there were no eligibility restrictions within PROSE concerning concomitant AD treatments at baseline or any other point, whereas the phase 3 studies required washout for topical and systemic AD medications before initiating dupilumab [13, 15, 32].
Strengths and Limitations
In this registry of real-world patients who initiated dupilumab, the collection of comprehensive baseline data on the day of the first dupilumab administration allowed for a thorough characterization of patient sociodemographics, AD history, AD treatment history, associated type 2 comorbidities, and AD severity variables, including physician-assessed AD signs and PROs (AD symptoms and QoL measures). Post-baseline assessments in future analyses will allow for the longitudinal observation of the real-world effectiveness of dupilumab. The study will also capture safety information and health care utilization data. Furthermore, since the study did not mandate standardized diagnostic criteria, patient selection was based entirely on routine diagnostic practice by participating physicians, favoring the generalizability of these observations to “real-world” populations.
However, this study also has some limitations. Certain aspects of the study design could have formed a cohort of patients that may not be generalizable to the wider patient population. For example, the requirements for monthly PRO assessments might have garnered a more disciplined or self-motivated patient type. Further, investigative sites were not chosen to ensure representative sampling of US and Canadian patients with AD. Also, as only sites in the USA and Canada were included, the worldwide generalizability of the results is limited. Lastly, some data were missing.
Conclusions
Patients enrolled in PROSE and initiating dupilumab in the real world have longstanding moderate-to-severe AD, with significant and variable disease burden based on AD signs, symptoms, and QoL, and with frequent type 2 comorbidities. Physician assessments alone appeared to underestimate the burden of disease, highlighting the importance of PROs when selecting appropriate treatments for moderate-to-severe AD.
Change history
10 July 2022
A peer-reviewed video abstract was retrospectively added to this publication.
References
Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–22.
Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis. J Allergy Clin Immunol. 2012;130(6):1344–54.
Boguniewicz M, Alexis AF, Beck LA, et al. Expert perspectives on management of moderate-to-severe atopic dermatitis: a multidisciplinary consensus addressing current and emerging therapies. J Allergy Clin Immunol Pract. 2017;5(6):1519–31.
Abuabara K, Yu AM, Okhovat JP, Allen IE, Langan SM. The prevalence of atopic dermatitis beyond childhood: a systematic review and meta-analysis of longitudinal studies. Allergy. 2018;73(3):696–704.
Chan AR, Sandhu VK, Drucker AM, Fleming P, Lynde CW. Adult-onset atopic dermatitis: presentations and progress. J Cutan Med Surg. 2020;24(3):267–72.
Garmhausen D, Hagemann T, Bieber T, et al. Characterization of different courses of atopic dermatitis in adolescent and adult patients. Allergy. 2013;68(4):498–506.
Chiesa Fuxench ZC, Block JK, Boguniewicz M, et al. Atopic dermatitis in America study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol. 2019;139(3):583–90.
Birdi G, Cooke R, Knibb RC. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int J Dermatol. 2020;59(4):e75-91.
Eckert L, Gupta S, Amand C, Gadkari A, Mahajan P, Gelfand JM. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77(2):274-9.e273.
Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–60.
Macdonald LE, Karow M, Stevens S, et al. Precise and in situ genetic humanization of 6 Mb of mouse immunoglobulin genes. Proc Natl Acad Sci USA. 2014;111(14):5147–52.
Murphy AJ, Macdonald LE, Stevens S, et al. Mice with megabase humanization of their immunoglobulin genes generate antibodies as efficiently as normal mice. Proc Natl Acad Sci USA. 2014;111(14):5153–8.
Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389(10086):2287–303.
Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375(24):2335–48.
de Bruin-Weller M, Thaci D, Smith CH, et al. Dupilumab with concomitant topical corticosteroid treatment in adults with atopic dermatitis with an inadequate response or intolerance to ciclosporin A or when this treatment is medically inadvisable: a placebo-controlled, randomized phase III clinical trial (LIBERTY AD CAFE). Br J Dermatol. 2018;178(5):1083–101.
Simpson EL, Paller AS, Siegfried EC, et al. Efficacy and safety of dupilumab in adolescents with uncontrolled moderate to severe atopic dermatitis: a phase 3 randomized clinical trial. JAMA Dermatol. 2020;156(1):44–56.
Paller AS, Siegfried EC, Thaçi D, et al. Efficacy and safety of dupilumab with concomitant topical corticosteroids in children 6 to 11 years old with severe atopic dermatitis: a randomized, double-blinded, placebo-controlled phase 3 trial. J Am Acad Dermatol. 2020;83(5):1282–93.
Xiong XF, Zhu M, Wu HX, Fan LL, Cheng DY. Efficacy and safety of dupilumab for the treatment of uncontrolled asthma: a meta-analysis of randomized clinical trials. Respir Res. 2019;20(1):108.
Bachert C, Mannent L, Naclerio RM, et al. Effect of subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis: a randomized clinical trial. JAMA. 2016;315(5):469–79.
Bachert C, Han JK, Desrosiers M, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet. 2019;394(10209):1638–50.
Hirano I, Dellon ES, Hamilton JD, et al. Efficacy of dupilumab in a phase 2 randomized trial of adults with active eosinophilic esophagitis. Gastroenterology. 2020;158(1):111-22.e10.
DUPIXENT (dupilumab). Highlights of prescribing information. United States Food and Drug Administration. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761055s031lbl.pdf. Accessed 27 Jan 2022.
Dupixent® product monograph. Sanofi-aventis Canada Inc. 2021. https://pdf.hres.ca/dpd_pm/00062540.PDF. Accessed 27 Jan 2022.
Leshem YA, Hajar T, Hanifin JM, Simpson EL. What the Eczema Area and Severity Index score tells us about the severity of atopic dermatitis: an interpretability study. Br J Dermatol. 2015;172(5):1353–7.
Charman CR, Venn AJ, Ravenscroft JC, Williams HC. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br J Dermatol. 2013;169(6):1326–32.
Silverberg JI, Gelfand JM, Margolis DJ, et al. Severity strata for POEM, PO-SCORAD, and DLQI in US adults with atopic dermatitis. Ann Allergy Asthma Immunol. 2018;121(4):464-8.e3.
Vakharia PP, Chopra R, Sacotte R, et al. Severity strata for five patient-reported outcomes in adults with atopic dermatitis. Br J Dermatol. 2018;178(4):925–30.
Silverberg JI, Simpson EL, Ardeleanu M, et al. Dupilumab provides important clinical benefits to patients with atopic dermatitis who do not achieve clear or almost clear skin according to the Investigator’s Global Assessment: a pooled analysis of data from two phase III trials. Br J Dermatol. 2019;181(1):80–7.
Katoh N, Saeki H, Kataoka Y, et al. Atopic dermatitis disease registry in Japanese adult patients with moderate to severe atopic dermatitis (ADDRESS-J): baseline characteristics, treatment history and disease burden. J Dermatol. 2019;46(4):290–300.
Bosma AL, de Wijs LEM, Hof MH, et al. Long-term effectiveness and safety of treatment with dupilumab in patients with atopic dermatitis: results of the TREAT NL (TREatment of ATopic eczema, the Netherlands) registry. J Am Acad Dermatol. 2020;83(5):1375–84.
Silverberg JI, Simpson EL, Guttman-Yassky E, et al. Dupilumab significantly modulates pain and discomfort in patients with atopic dermatitis: a post hoc analysis of 5 randomized clinical trials. Dermatitis. 2021;32(1S):S81–91.
Thaçi D, Simpson EL, Deleuran M, et al. Efficacy and safety of dupilumab monotherapy in adults with moderate-to-severe atopic dermatitis: a pooled analysis of two phase 3 randomized trials (LIBERTY AD SOLO 1 and LIBERTY AD SOLO 2). J Dermatol Sci. 2019;94(2):266–75.
Acknowledgements
Funding
This research was sponsored by Sanofi and Regeneron Pharmaceuticals, Inc. The journal’s Rapid Service Fee was sponsored by Sanofi and Regeneron Pharmaceuticals, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
Concept and design: JC, ZC, AK, and MA. All named authors contributed to data analyses and interpretation, drafting, and revising the manuscript.
Medical writing, editorial, and other assistance
Medical writing and editorial assistance was provided by Yunyu Huang, PhD, of Excerpta Medica, and was funded by Sanofi and Regeneron Pharmaceuticals, Inc., according to the Good Publication Practice guideline.
Disclosures
Jerry Bagel received research funds payable to the Psoriasis Treatment Center of New Jersey from AbbVie, Amgen, Arcutis Biotherapeutics, Boehringer Ingelheim, Bristol Myers Squibb, Corrona, Dermavant, Dermira/UCB, Eli Lilly, Glenmark, Janssen Biotech, Kadmon, LEO Pharma, Lycera, Menlo Therapeutics, Novartis, Pfizer, Regeneron Pharmaceuticals, Sun Pharma, Taro Pharmaceutical Industries Ltd, and Valeant Pharmaceuticals; consultant fees from AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Janssen Biotech, Novartis, Sun Pharma, and Valeant Pharmaceuticals; and fees for speaking from AbbVie, Bristol Myers Squibb, Eli Lilly, Janssen Biotech, and Novartis. Tien Q. Nguyen is an investigator, consultant, and/or speaker for AbbVie, Almirall, Amgen, Biogen, Bristol Myers Squibb, Corrona, GlaxoSmithKline, Janssen, Eli Lilly, Merck, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi, Sun Pharma, UCB. Hermenio Lima has participated on advisory board as consultant and clinical trials for Regeneron Pharmaceuticals, Inc. and Sanofi. Neal Jain is a consultant/speaker and has received honorarium/research funding from Amgen, AstraZeneca, Lilly, Merck, Novartis, Optinose, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi Genzyme. David M. Pariser is an investigator for Abbott Laboratories, Amgen, Bausch Health, Bickel Biotechnology, Bristol Myers Squibb, Eli Lilly, LEO Pharma, Novartis, Novo Nordisk, Ortho Dermatologics, Peplin, Pfizer, Photocure, Promius Pharma, Regeneron Pharmaceuticals, Inc., Stiefel; consultant for Bausch Health, Bickel Biotechnology, Biofrontera, Bristol Myers Squibb, Dermira, DUSA Pharmaceuticals, LEO Pharma, Novartis, Promius Pharma, Regeneron Pharmaceuticals, Inc., TheraVida; advisory board member of Pfizer. Sylvia Hsu has been an investigator for Amgen, Bristol Myers Squibb, Novartis; member of advisory boards for Janssen, Lilly, Ortho Dermatologics. Gil Yosipovitch conducted clinical trials or received honoraria for serving as a member of the scientific advisory board and consultant for Bellus Health, Eli Lilly, Galderma, LEO Pharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi, Trevi Therapeutics; received research funds from Kiniksa Pharmaceuticals, LEO Pharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi. Haixin Zhang, Jingdong Chao, Shikha Bansal, Andrew Korotzer, Zhen Chen and Marius Ardeleanu are employees and shareholders of Regeneron Pharmaceuticals, Inc. Daniel Richman is an employee and shareholder of Sanofi.
Compliance with ethics guidelines
Appropriately constituted Institutional Review Boards approved the study (Supplementary Table 1), which was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and is consistent with applicable regulatory requirements. All patients provided informed consent to participate in the study.
Data Availability
The datasets generated and analyzed during the current study are not publicly available because the registry study is still ongoing and the current analysis is interim.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bagel, J., Nguyen, T.Q., Lima, H. et al. Baseline Demographics and Severity and Burden of Atopic Dermatitis in Adult Patients Initiating Dupilumab Treatment in a Real-World Registry (PROSE). Dermatol Ther (Heidelb) 12, 1417–1430 (2022). https://doi.org/10.1007/s13555-022-00742-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00742-w