Abstract
Introduction
Until recently, patients discontinuing first-line (1L) hedgehog inhibitors (HHIs) for basal cell carcinoma (BCC) had few subsequent treatment options. The objective of this study was to describe the treatment journey and prognosis of patients discontinuing 1L HHI for BCC.
Methods
This was a retrospective cohort study of patients with BCC who discontinued 1L HHI treatment in The US Oncology Network between 1 January 2012 and 1 January 2019 (with follow-up until 1 May 2020). Two cohorts were identified: patients who initiated a second-line (2L) treatment (2L initiators), and patients with 1L progression or toxicity without pathology-confirmed complete response who did not initiate 2L treatment (2L non-initiators). Patient demographics, treatment characteristics, and outcomes are reported for each cohort.
Results
Among 115 patients with BCC who received 1L HHI treatment, 63.5% (n = 73/115) discontinued 1L HHIs. Of those, 50.7% (n = 37/73) discontinued because of documented toxicity or progression, without evidence of a complete response. We identified 4 patients who initiated 2L systemic treatment (median age 68.7 years, 100.0% female) and 15 patients who were eligible for the 2L non-initiator cohort (median age 80.2 years, 20.0% female). Median 1L HHI duration was 6.8 months (range 1.9–20.6 months) for the 2L non-initiator cohort and 8.6 months (range 6.8–42.2 months) for 2L initiators. At the end of follow-up, among 2L non-initiators (median follow-up duration 9.7 months), 40.0% were lost to follow-up, 33.3% had died, 20.0% continued observation, and 6.7% transitioned to an academic medical center or hospital; among 2L initiators (median follow-up duration 6.3 months), 50.0% were lost to follow-up, 25.0% had died, and 25.0% continued observation.
Conclusions
Following 1L HHI discontinuation, lack of standardized care and suboptimal outcomes were observed, including limited receipt of 2L treatment. Further studies are necessary to evaluate the impact of newer BCC treatment options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Why carry out this study? |
Until recently, patients discontinuing first-line (1L) hedgehog inhibitors (HHIs) for basal cell carcinoma (BCC) had few subsequent treatment options. |
The objective of this study was to describe the treatment journey and prognosis of patients discontinuing 1L HHI for BCC. |
What was learned from this study? |
Following 1L HHI discontinuation, lack of standardized care and suboptimal outcomes were observed, including limited receipt of 2L treatment. |
Further studies are necessary to evaluate the impact of newer BCC treatment options. |
Digital Features
This article is published with digital features, including an infographic, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.19487429.
Introduction
Basal cell carcinoma (BCC) is the most common cancer in the USA, with an estimated 2 million patients diagnosed annually and an increasing incidence of disease [1, 2]. For most patients diagnosed with BCC, local treatment, including surgical excision, radiotherapy, or superficial therapies, is curative [3]. The prognosis worsens, however, if medical attention is delayed or if BCC recurs after local treatment, in which case patients may present with locally advanced or metastatic BCC [4]. It is estimated that locally advanced BCC occurs in 0.8% of cases, while metastatic BCC occurs in 0.0028% to 0.55% of cases [4, 5].
The approved first-line (1L) treatment for patients with locally advanced or metastatic BCC consists of hedgehog pathway inhibitors (HHIs) [3]. Prior to US Food and Drug Administration (FDA) approval of cemiplimab-rwlc in February 2021, patients who required subsequent treatment or did not tolerate HHIs [3] were limited to noncurative surgery or radiation, along with clinical trial participation [3, 6]. While other studies have evaluated use and outcomes among patients initiating HHIs in the real-world setting [5, 7, 8], to our knowledge, no studies have examined treatment patterns or outcomes following 1L HHI treatment discontinuation for BCC. The aim of this study was to assess the characteristics, treatment patterns, and outcomes of patients in the community oncology setting with BCC who discontinued 1L HHIs.
Methods
Study Design and Data Sources
We conducted a retrospective cohort study using The US Oncology Network data between 1 January 2012 and 1 May 2020, and the Limited Access Death Master File (LADMF). The US Oncology Network includes nearly 1400 affiliated community-based physicians operating in over 480 sites of care across the USA, with over 1.2 million patients treated annually [9].
From The US Oncology Network’s electronic health record (EHR) system, iKnowMed (iKM), a platform that captures outpatient practice encounter data, we obtained data on patient demographics; clinical information such as disease diagnosis, diagnosis stages, Eastern Cooperative Oncology Group (ECOG) performance status, and laboratory testing results; and treatment information, such as line of therapy and treatment administration within The US Oncology Network [10, 11]. Structured data fields within the iKM EHR were supplemented by unstructured data collected from chart review to capture information contained in progress notes or scan reports. Electronic chart review data were collected using a secure, web-based electronic case report form by healthcare professionals with oncology experience using standardized abstraction guidelines [12].
The Social Security Administration’s LADMF was an additional source of vitality information [13]. If there was a discrepancy in dates of death between the EHR and LADMF sources, the LADMF date was prioritized unless (1) EHR activity indicated that a patient visit occurred after date of death as documented in the LADMF, or (2) the dates of death between the two sources varied by more than 6 months. In these cases, the date of death recorded in the iKM EHR was used since it encompasses non-official records, including telephone conversations with the patient’s family. Previous research suggests high concordance between death dates captured in the iKM EHR and those sourced from the LADMF, with most death information being sourced from the EHR rather than the LADMF [14].
This study was conducted in accordance with legal and regulatory requirements, as well as with scientific purpose, value, and rigor, and it followed generally accepted research practices. This study was granted an exception and waiver of consent by The US Oncology Inc. Institutional Review Board.
Study Population
The study population consisted of patients who discontinued 1L HHI monotherapy (i.e., vismodegib or sonidegib) for BCC between 1 January 2012 and 1 November 2019, and either initiated second-line (2L) treatment (i.e., 2L initiators) or had documented progression or toxicity to 1L treatment without evidence of pathology-confirmed complete response and did not initiate 2L treatment (i.e., 2L non-initiators).
Eligible patients were required to be ≥ 18 years of age on the index date (as defined below) and to have at least two visits within The US Oncology Network and a recorded diagnosis of BCC prior to or on the index date. Patients were excluded if their EHRs were inaccessible for research purposes or if they received treatment for another primary cancer up to 3 years prior to and including the index date, with the exception of patients with fully resected cutaneous malignancies (e.g., adnexal neoplasms, cutaneous squamous cell carcinoma, cutaneous T-cell and B-cell lymphoma, BCC, or Merkel cell carcinoma).
We first identified the patients meeting these criteria who initiated 2L systemic treatment, and their index date was defined as the date of 2L initiation. Among the remaining patients who might qualify as 2L non-initiators, we sought to exclude patients who were using HHI as neoadjuvant to surgery or radiation. To do this, a data-driven approach was used to determine the index date for the 2L non-initiator cohort based on when patients would be expected to receive potential curative surgery or radiation treatment. The study team reviewed the time between HHI discontinuation and subsequent surgery and radiation therapies among potential 2L non-initiators, as well as the time between HHI discontinuation and 2L initiation among 2L initiators, and then selected 90 days following HHI discontinuation as the index date for 2L non-initiators. Patients who received surgery or radiation in this 90-day period or lacked 90 days of follow-up after 1L discontinuation were excluded from the analysis.
Patients were followed from the index date until initiation of treatment for another primary cancer (with the exception of patients with fully resected cutaneous malignancies), loss to follow-up (defined as the last visit within The US Oncology Network), death, or the end of the study period (1 May 2020), whichever occurred first.
Treatment Patterns
Treatment patterns prior to 1L HHI initiation, during HHI treatment, and—for the 2L initiator cohort—following HHI discontinuation, were described. Specifically, prior BCC-related surgery or radiation was captured, along with prior surgery locations (head, trunk, or other locations). Type of HHI monotherapy initiated (i.e., vismodegib or sonidegib), year of HHI initiation, time from initial BCC diagnosis to 1L HHI initiation, and reasons for 1L HHI discontinuation were captured as documented by providers. HHI treatment duration was calculated from the initiation and discontinuation dates. The start date was defined as the first prescription date of HHIs following a diagnosis of BCC or verified date in progress notes if the regimen was initiated offsite. The date of treatment discontinuation was defined as the discontinuation date explicitly documented in physicians’ notes, the date of treatment switch or addition of another anticancer regimen (switching between sonidegib and vismodegib was not considered a switch), or the last prescription date if the treatment occurred ≥ 120 days before the last visit date, whichever was first.
For the 2L initiator cohort, the treatment-free interval was defined as the days between the date of 1L HHI discontinuation and the start of 2L treatment. The types of 2L treatments initiated were also described.
Outcomes
Patient disposition was described at the end of follow-up, and patients were categorized as lost to follow-up, died, transitioned to an academic medical center or hospital, or continued observation. The number of patients who transitioned to hospice, and days from 1L discontinuation to hospice care, were also summarized. For the 2L initiator cohort, treatment status at the end of 2L treatment was categorized as completed planned treatment, died during 2L treatment, ongoing 2L treatment, or discontinued 2L treatment because of progression.
Other Variables
Other data elements assessed on the index date included demographic and clinical characteristics such as age, sex, race, geographic location of practice, ECOG performance status closest to index, locally advanced or metastatic status, and initial tumor sites. Ages > 90 years were collapsed into a single category to conform to Health Insurance Portability and Accountability Act guidelines.
Statistical Analysis
Patients were described in terms of demographic and clinical characteristics, treatment patterns, and outcomes according to whether they were a 2L initiator or 2L non-initiator. Owing to the small sample size, continuous variables were described using medians and ranges (maximum and minimum). Categorical variables were reported using patient counts and percentages, with the denominator being the number of patients with non-missing data. Missing data were not imputed, and the proportion of patients with missing values is reported.
Results
Study Attrition
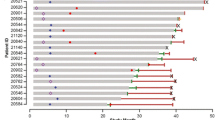
Within The US Oncology Network, 3884 patients were identified with a diagnosis of BCC any time prior to 1 November 2019 based on available structured data (Fig. 1). Among these, 138 patients with BCC treated with HHIs between 1 January 2012 and 1 November 2019 had at least two visits in The US Oncology Network and had data that were accessible for research purposes. A total of 115 (83.3%) received HHIs as 1L systemic BCC therapy. Of these, 73 (63.5%) discontinued 1L HHIs between 1 January 2012 and 1 November 2019, with 33 of 73 (45.2%) discontinuing because of documented toxicity or progression without evidence of a complete response. Four patients who discontinued HHIs initiated 2L systemic treatment. Among the remaining 33 patients potentially eligible as 2L non-initiators, 18 were excluded: one patient received treatment for another primary cancer, 12 did not have ≥ 90 days of follow-up after 1L discontinuation, and 5 received surgery or radiation in the 90-day period following HHI discontinuation. The final study sample consisted of 19 patients: 15 in the 2L non-initiator cohort and 4 in the 2L initiator cohort.
Demographic and Clinical Characteristics
The median age of patients in the 2L non-initiator cohort (n = 15) was 80.2 years (range 46.9–90+ years), with 80.0% (n = 12/15) being male (Table 1). All patients with available race data (n = 11/15) were white. Most patients in this cohort were treated in the Western (53.3%; n = 8/15) or Southern (33.3%; n = 5/15) regions of the USA. Twelve of 15 patients in the 2L non-initiator cohort had documented ECOG performance status: 83.3% (n = 10/12) had a score of 0 or 1, with the remaining 16.7% (n = 2/12) having a score of 2+. Among the 11/15 patients with available information on BCC locally advanced or metastatic disease status, 90.9% (n = 10/11) had locally advanced disease and 9.1% (n = 1/11) had metastatic disease at initial BCC diagnosis.
For the 2L initiator cohort (n = 4), the median age of patients was 68.7 years (range 48.4–71.1 years) and all (n = 4/4) were female (Table 1). Most patients in the 2L initiator cohort were white (75.0%; n = 3/4) and treated in the Southern (75.0%; n = 3/4) region of the USA. Among patients with documented ECOG performance status (n = 3/4), all had a score of 1. Among the 3 of 4 patients with available information on locally advanced or metastatic BCC, 66.7% (n = 2/3) had metastatic disease and 33.3% (n = 1/3) had locally advanced disease at initial BCC diagnosis.
Treatment History
All patients in both cohorts received 1L vismodegib monotherapy (Table 2).
The median time from initial BCC diagnosis to 1L HHI treatment among the 2L non-initiator cohort (n = 15) was 2.1 months (range 0.0–80.5 months), and the median 1L HHI treatment duration was 6.8 months (range 1.9–20.6 months). Sixty percent of patients (n = 9/15) initiated 1L treatment between 2012 and July 2015 (prior to FDA approval of sonidegib), while the remaining 40% (n = 6/15) initiated treatment after July 2015 (Table 2). Most patients (93.3%; n = 14/15) discontinued 1L HHI treatment because of toxicity, with one patient of 15 (6.7%) discontinuing because of progression.
The median time from initial diagnosis to 1L treatment among the 2L initiator cohort (n = 4/4) was 3.5 months (range 0.0–77.1 months), and the median 1L treatment duration was 8.6 months (range 6.8–42.2 months). Half the patients in the 2L initiator cohort (n = 2/4) initiated 1L HHI treatment between 2012 and July 2015 (prior to FDA approval of sonidegib), while the remaining patients initiated HHI treatment after July 2015 (Table 2). All patients in the 2L initiator cohort (n = 4/4) discontinued 1L treatment because of progression.
Outcomes
The median duration of follow-up was 9.7 months (range 3.2–42.2 months) for patients in the 2L non-initiator cohort (n = 15/15) and 6.3 months (range 0.7–61.1 months) for patients in the 2L initiator cohort (n = 4/4) (Table 3).
The median time between 1L discontinuation and 2L initiation was 75 days (range 2–130 days) among patients in the 2L initiator cohort. Among the 4 patients in the 2L initiator cohort, one received carboplatin and paclitaxel (25.0%; n = 1/4), one received cemiplimab (25.0%; n = 1/4), one received nivolumab (25.0%; n = 1/4), and one received pembrolizumab (25.0%; n = 1/4).
At the end of the study follow-up period, among the 2L non-initiator cohort (n = 15), 40.0% of patients (n = 6/15) were lost to follow-up, 33.3% (n = 5/15) died, 20.0% (n = 3/15) were under continued observation, and 6.7% (n = 1/15) had transitioned out of The US Oncology Network to an academic medical center or hospital outside this system (Table 3). Three of the 15 patients in the 2L non-initiator cohort had documentation of receiving a care, with a median time of 20.0 months (range 13.7–22.1 months) from 1L discontinuation.
Among the 2L initiator cohort (n = 4/4), status of 2L treatment at the end of follow-up was as follows: one patient had completed planned treatment (n = 1/4; 25.0%), one was still on treatment (n = 1/4; 25.0%), one died during 2L treatment (n = 1/4; 25.0%), and one discontinued 2L treatment because of progression (n = 1/4; 25.0%). At the end of the study period, among the 2L initiator cohort (n = 4/4), two patients (n = 2/4; 50.0%) were lost to follow-up, one (n = 1/4; 25.0%) died, and one (n = 1/4; 25.0%) had continued observation (Table 3). None of the patients in the 2L initiator cohort had documentation of hospice care.
Discussion
The results of this study describe the patient characteristics, treatment patterns, and clinical outcomes of patients with BCC who discontinued 1L HHI treatment in the community oncology setting. In a small cohort of patients with BCC discontinuing 1L HHIs, we found that approximately half discontinued because of documented disease progression or toxicity. We observed that few of these patients initiated another line of treatment and that most patients were either lost to follow-up or had died without initiating subsequent systemic treatments.
Few studies have described characteristics and outcomes of real-world patients with locally advanced or metastatic BCC [5, 7, 8]. Goldenberg et al. (2016) performed a retrospective cohort study using insurance claims data from October 2011 to September 2012 to estimate the incidence and prevalence of BCC in the USA [5]. In this study, the mean age of patients with incident locally advanced BCC (n = 261) was 72.2 years [standard deviation (SD) 13.7] and 53.3% were male, and the mean age of patients with incident metastatic BCC (n = 7) was 71.3 years (SD 14.9) and 85.7% were male. The mean ages of patients with incident locally advanced and metastatic BCC from the Goldberg study were similar to the median age of 2L initiators in our study (69 years), but considerably younger than the median age of 80 years observed among the 2L non-initiator cohort. The fact that patients who were not subsequently treated were older than the 2L initiators may be due to patient or physician decisions regarding benefit and risk assessments of further BCC treatment due to factors such as advanced age, frailty, and willingness or ability to travel for treatment.
Cozzani et al. (2020) examined real-world use of vismodegib among patients with locally advanced or metastatic BCC who were ineligible for curative surgery or radiotherapy in Argentina [7]. All patients initiated vismodegib, and 90% of patients had locally advanced disease, similar to our study in which all patients were treated with vismodegib and 78.5% of 2L initiators and 2L non-initiators with available data (n = 11/14) had locally advanced disease at initial BCC diagnosis. In the Cozzani study, the cohort had a median age of 73 years and 66.2% were male; in comparison, we observed a median age of 80 years and 80% male in our 2L non-initiator cohort, and a median age of 69 years and 0% male in our 2L initiator cohort.
In our study, all patients received 1L vismodegib monotherapy, even though nearly half initiated HHI treatment after the FDA approval of sonidegib in July 2015 [15]. Similar use of vismodegib was reported in an analysis of MarketScan Commercial and Medicare Supplemental claims data from 2013 to 2018. Among the 469 patients with BCC initiating an HHI, 99.2% received vismodegib. It is hypothesized that the higher use of vismodegib observed in these real-world studies may be due to the earlier approval of vismodegib and better recognition among patients and providers compared with sonidegib.
The median duration of 1L HHI treatment among patients discontinuing HHIs was 7 months among the 2L non-initiator cohort and 9 months among the 2L initiator cohort, shorter than the 10–12-month average treatment duration reported from the pivotal trials [16, 17]. Duration of treatment in this study, however, was similar to the estimated median duration of 8.6 months reported in the STEVIE trial of vismodegib among patients (n = 1215) with locally advanced or metastatic BCC [18]. A retrospective cohort study of patients with locally advanced BCC (n = 48) or metastatic BCC (n = 11) initiating vismodegib in the Netherlands also found that the median treatment duration was 6.4 months (range 1.4–38.5 months) among those with locally advanced BCC and 7.5 months (range 1.6–18.5 months) among those with metastatic BCC [8]. Although we estimated average treatment duration only among patients discontinuing HHI treatment because of toxicity and progression rather than complete response, our findings add to the accumulating evidence that persistence on HHI treatment in the real world is likely considerably shorter than in the trials.
In our study, we also found that the most common reason for HHI 1L treatment discontinuation was toxicity. Clinical trials have reported tolerability issues with HHIs, and both reactive interruption (discontinuing HHI treatment for 8 weeks when adverse reactions occur [16, 17, 19]) and preventive interruption (prospectively alternating between HHI treatment for 8 or 12 weeks, with scheduled 8-week interruptions having been investigated as treatment strategies to improve HHI tolerability) [19,20,21,22]. By the time of the primary analysis data cutoff date of STEVIE (with a median follow-up of 17.9 months for efficacy analysis), 88% (n = 1068/1215) of patients had discontinued vismodegib. Reasons for discontinuation included adverse events (32.7%), disease progression (17.7%), patient request or physician decision (17.7%), death or loss to follow-up (5.4%), and other reasons (26.5%) [18, 23]. In this study, we relied on physician-documented reason for discontinuation. Among 2L non-initiators, 14 of 15 had toxicity documented as the reason for discontinuation compared with none among the 4 2L non-initiators. While reliance on physician-documented reason for discontinuation may favor capture of toxicity as a reason, particularly for patients who did not tolerate treatment, our findings suggest tolerability is the most frequently documented reason for discontinuation, particularly among those who do not go on to initiate other treatments for locally advanced or metastatic BCC.
Until recently (2020), the National Comprehensive Cancer Network (NCCN) guidelines recommended surgery, radiation therapy, or a clinical trial after discontinuation of an HHI [3, 6]. In our study, we observed that most patients who discontinued HHIs because of toxicity or progression rather than complete response did not initiate a subsequent treatment. At the end of a median of approximately 10 months of follow-up, most 2L non-initiators either died (33%) or were lost to follow-up (40.0%), when they may have died, entered hospice, or stopped seeking care. It is possible that some patients may have also initiated treatment elsewhere (e.g., through a transfer to an academic medical center), although this is unlikely since transfers are usually documented in patients’ medical records and we specifically searched for transfers during chart abstraction. We observed that only 4 patients initiated a subsequent 2L treatment, and that all of them initiated different treatments. At the end of approximately 6 months of follow-up, 75% of patients who initiated a treatment had died (25%) or were lost to follow-up (50%). Our findings underscore that there was an important unmet need for effective therapeutic options with acceptable risk–benefit profiles for patients with BCC who discontinue initial 1L HHI because of disease progression or toxicity and not complete response. Current NCCN guidelines (version 2.2021) now recommend cemiplimab-rwlc for patients who were previously treated with an HHI or for whom an HHI is not appropriate [3]. Future studies should examine how treatment patterns and outcomes have changed following the introduction of novel immunotherapies [24].
The study utilized clinical data from the EHR system of The US Oncology Network, a large system of community oncology practices. The use of real-world data is advantageous because it reflects community oncology practice trends as opposed to tightly controlled clinical trials. Moreover, results for this study were drawn from both structured and unstructured EHR data. By verifying patients’ eligibility and key study variables through a manual review of records, the study dataset was enhanced beyond structured records.
Despite the advantages of this real-world data source, the results of this study should be contextualized by a number of limitations. Most prominently, while it provides insights into the rarity of subsequent treatment for BCC, we identified few patients meeting the study eligibility criteria. While this study applied several steps to verify that the appropriate patients were selected for inclusion, other information of interest may be incomplete, inaccurate, or inconsistently documented in the EHR. For example, some patients who died or transferred to hospice care may have been misclassified as being lost to follow-up because of incomplete capture of these events in the EHR or the LADMF. Owing to lack of information on care provided in academic medical centers, it is possible that 2L non-initiators lost to follow-up may have been treated in an academic medical center, although we would anticipate this to be rare. Use of HHIs, including whether they were used as adjuvant to surgery/radiation, could have been misclassified. Reasons for discontinuation were unlikely to have been recorded for all patients, resulting in a smaller and more select group of patients experiencing HHI treatment failure; and, owing to known tolerability issues with HHIs, physicians may have been more likely to record toxicity as a reason for discontinuation. To ensure that the study population was ineligible for curative surgery or radiation, the index date for the 2L non-initiator cohort was defined to be 90 days following 1L treatment discontinuation and comparisons between the cohorts were further precluded. Lastly, it was not possible to contextualize treatment decisions, including reasons 2L non-initiators were not treated with systemic treatments.
Conclusions
The results of this study encompass a small number of patients, but still serve to illustrate the lack of standardized care options for patients with BCC who are ineligible for curative therapies following 1L HHI treatment failure in the US community oncology setting. In addition to the high proportion of patients who did not advance to subsequent treatment following 1L HHI discontinuation, unfavorable outcomes were also observed irrespective of whether patients received 2L treatment. This suggests an unmet need for effective treatment options with acceptable risk–benefit profiles after 1L HHI discontinuation. Further studies are necessary to evaluate the impact of newer treatment options recommended by NCCN guidelines for patients who were previously treated with an HHI or for whom an HHI is not appropriate.
References
Mohan SV, Chang AL. Advanced basal cell carcinoma: epidemiology and therapeutic innovations. Curr Dermatol Rep. 2014;3(1):40–5.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
National Comprehensive Cancer Network. Clinical practice guidelines in oncology: basal cell skin cancer. 2021. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nmsc.pdf.
de Piva FP, Senna CG, Tabai M, Chone CT, Altemani A. Metastatic basal cell carcinoma: a rare manifestation of a common disease. Case Rep Med. 2017;2017:8929745.
Goldenberg G, Karagiannis T, Palmer JB, Lotya J, O’Neill C, Kisa R, et al. Incidence and prevalence of basal cell carcinoma (BCC) and locally advanced BCC (LABCC) in a large commercially insured population in the United States: a retrospective cohort study. J Am Acad Dermatol. 2016;75(5):957–66.
Tongdee E, Psomadakis CE, Paka P, Marghoob N, Markowitz O. Emerging noninvasive treatments of nonmelanoma skin cancers. Cutis. 2020;105(3):138–42.
Cozzani R, Del Aguila R, Carrizo M, Sanchez S, Gonzalez A, ML29740 Investigators. Efficacy and safety profile of vismodegib in a real-world setting cohort of patients with advanced basal cell carcinoma in Argentina. Int J Dermatol. 2020;59(5):627–32.
Verkouteren BJA, Wakkee M, Reyners AKL, Nelemans P, Aarts MJB, Rácz E, et al. Eight years of experience with vismodegib for advanced and multiple basal cell carcinoma patients in the Netherlands: a retrospective cohort study. Br J Cancer. 2021;124(7):1199–206.
The US Oncology Network. Our company. 2021. Available from: https://www.usoncology.com/our-company.
Ontada. iKnowMed: Oncology Practice EHR System. 2021. Available from: https://www.mckesson.com/Specialty/Oncology-Electronic-Health-Records/.
Busby LT, Sheth S, Garey J, Ginsburg A, Flynn T, Willen MA, et al. Creating a process to standardize regimen order sets within an electronic health record. J Oncol Pract. 2011;7(4):e8–14.
Robert N, Espirito J, Haydon W, Jenson K, Montelongo N, Spark S, editors. Development of playbook for chart review in real-world data. The Professional Society for Health Economics and Outcomes Research (ISPOR) Annual Conference; 21 May 2019; New Orleans, LA, USA.
National Technical Information Services. Limited access death master file download. Available from: https://dmf.ntis.gov/index.html.
Boyd M, Fulcher N, Annavarapu S, editors. Concordance of death date assessments between the Social Security Death Master File and electronic health records in a US community oncology setting. The Professional Society for Health Economics and Outcomes Research (ISPOR) Annual Conference; 16–20 May 2020; Orlando, FL, USA.
Casey D, Demko S, Shord S, Zhao H, Chen H, He K, et al. FDA approval summary: sonidegib for locally advanced basal cell carcinoma. Clin Cancer Res. 2017;23(10):2377–81.
Sekulic A, Migden MR, Basset-Seguin N, Garbe C, Gesierich A, Lao CD, et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: final update of the pivotal ERIVANCE BCC study. BMC Cancer. 2017;17(1):332.
Lear JT, Migden MR, Lewis KD, Chang ALS, Guminski A, Gutzmer R, et al. Long-term efficacy and safety of sonidegib in patients with locally advanced and metastatic basal cell carcinoma: 30-month analysis of the randomized phase 2 BOLT study. J Eur Acad Dermatol Venereol. 2018;32(3):372–81.
Basset-Seguin N, Hauschild A, Kunstfeld R, Grob J, Dreno B, Mortier L, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334–48.
Basset-Seguin N, Hauschild A, Grob JJ, Kunstfeld R, Dreno B, Mortier L, et al. Vismodegib in patients with advanced basal cell carcinoma (STEVIE): a pre-planned interim analysis of an international, open-label trial. Lancet Oncol. 2015;16(6):729–36.
Dessinioti C, Plaka M, Soura E, Mortaki D, Papaxoinis G, Gogas H, et al. A practical guide for the follow-up of patients with advanced basal cell carcinoma during treatment with hedgehog pathway inhibitors. Oncologist. 2019;24(8):e755–64.
Dréno B, Kunstfeld R, Hauschild A, Fosko S, Zloty D, Labeille B, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18(3):404–12.
Lacouture ME, Dréno B, Ascierto PA, Dummer R, Basset-Seguin N, Fife K, et al. Characterization and management of hedgehog pathway inhibitor-related adverse events in patients with advanced basal cell carcinoma. Oncologist. 2016;21(10):1218–29.
Jalbert JJ, Chen C, Wu N, Fury M, Ruiz ES, Wenzhen G. Patterns of hedgehog inhibitor (HHI) treatment interruptions and re-initiations among patients with basal cell carcinoma (BCC) in real-world clinical practice. J Clin Oncol. 2020;38(suppl 15):2.
Food and Drug Administration. FDA approves cemiplimab-rwlc for metastatic or locally advanced cutaneous squamous cell carcinoma. 2019. Available from: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-cemiplimab-rwlc-metastatic-or-locally-advanced-cutaneous-squamous-cell-carcinoma.
Acknowledgements
Funding
Regeneron Pharmaceuticals, Inc., and Sanofi.
Author Contributions
CC, MF, TB, AG, JJJ, KMA, and LC provided substantial contributions to study design and interpretation of the results. KD provided substantial contributions to the acquisition of data and analysis of the results. KMA was responsible for drafting the manuscript and CC, MF, TB, AG, JJJ, KD, and LC provided critical revisions of the work. All authors provided final approval of the manuscript to be published.
Medical Writing, Editorial, and Other Assistance
The manuscript was initially written by Kathleen M. Aguilar, with editorial support provided by Dr. Lisa Kaspin-Powell (both employed by Ontada). Funding for this manuscript was provided by Regeneron Pharmaceuticals. The authors would like to thank Dr. Yunfei Wang for analytic support for this study. The authors would also like to thank the participants of the study.
Disclosures
Chieh-I. Chen, Matthew G. Fury, Timothy Bowler, Asieh Golozar, and Jessica J. Jalbert were employees of Regeneron Pharmaceuticals, Inc., at the time of the study (Timothy Bowler is now employed by Pfizer; Asieh Golozar is now employed by Odysseus Data Services). Patrick R. Lafontaine is an employee of Sanofi. Kathleen M. Aguilar is an employee of Ontada and Kalatu Davies was an employee of Ontada at the time of the study (Kalatu Davies is now employed by Astellas Pharma US, Inc.). Kathleen M. Aguilar, Kalatu Davies, and Lance Cowey provided contract research support to Regeneron Pharmaceuticals, Inc., and Sanofi.
Compliance with Ethics Guidelines
This study was conducted in accordance with legal and regulatory requirements, as well as with scientific purpose, value and rigor, and it followed generally accepted research practices. This study was granted an exception and waiver of consent by The US Oncology Inc. Institutional Review Board.
Data Availability
The health data used to support the findings of this study are restricted by the US Oncology Institutional Review Board in order to protect patient privacy. For this reason, data used to support the findings of this study have not been made available.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cowey, L., Chen, CI., Aguilar, K.M. et al. Real-World Treatment Patterns and Outcomes Among Patients with Basal Cell Carcinoma Following First-Line Hedgehog Inhibitor Discontinuation. Dermatol Ther (Heidelb) 12, 1211–1224 (2022). https://doi.org/10.1007/s13555-022-00724-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00724-y