Abstract
Introduction
Few data on possible local factors that can influence the achievement of response in nonsegmental vitiligo (NSV) treated with narrowband ultraviolet B (Nb-UVB) phototherapy are available. Our objective is to evaluate possible correlations between therapeutic outcomes and dermoscopic and local (lesional) clinical findings of vitiligous lesions undergoing Nb-UVB phototherapy to find positive and/or negative response predictor factors to such treatment.
Methods
For each target patch, we calculated the extension area using a computer-aided method and assessed dermoscopic and local (lesional) clinical findings at baseline. After 30 phototherapy sessions (twice weekly), surface area of the lesions was reevaluated to assess clinical improvement, correlating the therapeutic outcome with initial clinical and dermoscopic features.
Results
A total of 70 lesions were finally included in the study. At the end of therapy, 18 patches (25.7%) achieved improvement, and the presence of perifollicular pigmentation on baseline dermoscopic examination was found to be associated with a 12-fold higher probability of having a positive therapeutic outcome. Similarly, face localization was also correlated with clinical amelioration, with a sevenfold higher probability for improvement. No association (p > 0.05) between therapeutic outcomes (either good or poor) and other dermoscopic or local clinical variables (including leukotrichia) was observed.
Conclusions
Therapeutic response of vitiligo to Nb-UVB phototherapy may be positively affected by local features of the lesions, i.e., face localization and presence of perifollicular pigmentation on baseline dermoscopic examination, which might be considered as positive response predictor factors to optimize treatment of vitiligo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Limited data on the possible influence of local (lesional) factors on therapeutic response in vitiligo treated with narrowband ultraviolet B phototherapy are available. |
Correlations between baseline clinical/dermoscopic features of vitiligous lesions and therapeutic outcomes were assessed. |
What was learned from the study? |
Therapeutic response of vitiligo to narrowband ultraviolet B phototherapy may be positively influenced by local features of the lesions, namely face localization and perifollicular pigmentation on baseline dermoscopic examination. |
Vitiligo lesions localized on the face or featuring perifollicular pigmentation on dermoscopy have a higher probability of improvement when treated with narrowband ultraviolet B phototherapy. |
Introduction
Vitiligo is the most frequent acquired disorder of pigmentation, typically manifesting with more or less diffuse well-defined white patches, which are often responsible for a relevant psychological and social impairment in affected patients [1, 2]. Two main clinical variants exist, i.e., segmental vitiligo (SV) and nonsegmental vitiligo (NSV) [3,4,5,6]. SV is far less common and classically presents with dermatomeric lesions which stabilize after a rapid onset, while NSV is more frequent and is typified by symmetric distribution, later onset, and progressive course, with alternating phases of disease stability and worsening [2,3,4,5,6].
Narrowband ultraviolet B (Nb-UVB) therapy (wavelength ranging from 311 to 313 nm) is one of the most prescribed treatments for NSV, with variable therapeutic results being reported in daily clinical practice [7]. According to literature data, several factors may negatively affect the outcome of Nb-UVB therapy in NSV, including disease activity, associated autoimmune diseases, extensive involvement, family history of vitiligo, long duration of disease, mucosal involvement, presence of koebnerization and leukotrichia [1,2,3,4,5,6,7,8]. However, darker phototypes, early therapeutic response, and facial involvement are associated with a good treatment outcome [9]. Nevertheless, knowledge on possible influencing local (lesional) factors remains still limited.
Over the last few years, dermoscopy has been showed to be a useful support for both diagnosis and therapeutic management of several inflammatory dermatoses thanks to its ability to display relevant findings not visible to the naked eye examination [10,11,12,13,14,15,16]. The main dermoscopic features of vitiligo include well-defined milky/bright white structureless areas, perifollicular pigmentation or depigmentation, white hair (leukotrichia), and pigmentary (structureless or network-like) patches [16,17,18,19,20]. Besides diagnostic purposes, dermoscopy may also have a role in defining disease activity and predicting response to treatment [16,17,18,19,20].
The main aim of this prospective observational study is to evaluate the possible association between baseline dermoscopic features of vitiligo lesions and therapeutic response to Nb-UVB therapy. Possible correlations between treatment outcomes and baseline local (lesional) factors were also investigated.
The research was conducted in accordance with ethics guidelines and the declaration of Helsinki 1964 and its later amendments, and all the participants gave their informed consent to participation in the study and use of personal records or photos for scientific purposes. Local ethical committee [Comitato Etico Unico Regionale (CEUR) del Friuli Venezia Giulia] approval was obtained (study ID: 2284; code: VIT-fot_DERMOSC.01).
Methods
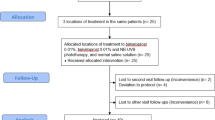
Adult patients (age ≥ 18 years) with NSV and at least three vitiligo patches scheduled to undergo Nb-UVB phototherapy were selected for this study. Patients under treatment for vitiligo who had used systemic/topical medication for vitiligo in the previous 12 weeks or who had been exposed to sun during the prior 8 weeks were not considered eligible. We also excluded patients suffering from other relevant dermatoses as well as pregnant or breastfeeding women.
Therapeutic regimen was not influenced at all by this study as it followed our standard internal protocol for vitiligo, with treatment being administered twice per week for 15 weeks for a total of 30 sessions. Starting ultraviolet B (UVB) dose, increments, and maximum UVB dose were chosen based on skin phototype following standardized guidelines [21]. Importantly, patients requiring additional systemic/topical treatments over the whole study period or subjects not completing the treatment course were excluded from the analysis.
Three or more target vitiligo patches were randomly selected for each patient to be documented and followed; anatomical localization of chosen lesions was identified by photographs and (when possible) recording distances from static benchmarks (e.g., bony prominences).
At baseline (before starting Nb-UVB therapy), each selected lesion was evaluated from a dermoscopic and clinical point of view by two independent expert physicians (E.E. for dermoscopic and C.P. for clinical examination). Dermoscopic analysis consisted in assessing the presence of several variables identified according to literature data, our preliminary observations, and standardized criteria for evaluation of nonneoplastic dermatoses [16,17,18,19,20, 22], i.e., leukotrichia (white hair), perifollicular pigmentation, brown structureless/reticular areas (nonfollicular pigmentation), and follicular red dots. Dermoscopy was performed with a hand-held polarized-light dermoscope (DermLite DL3 × 10; 3Gen, San Juan Capistrano, CA). Regarding clinical examination, we assessed the presence of leukotrichia, perifollicular pigmentation, and nonfollicular pigmentation (“pigmented islands”) as well as calculated the area of depigmentation from clinical pictures by a computer-aided method using Fiji (an open-source software for image analysis) and applying a 1-cm [2] white adhesive label on perilesional skin as a size reference.
At the end of treatment, we evaluated clinical improvement of target lesions (defined as repigmentation ≥ 25% compared with baseline) correlating the therapeutic outcome with baseline dermoscopic and local clinical features. Notably, posttreatment repigmentation was assessed by both the above-mentioned computer-aided method and clinical images comparison with baseline photos (according to a standardized procedure taking into account visual examples of different percentages of depigmentation) [23], yet only the former was considered for statistical analysis as this was more reproducible and less user-dependent.
Statistical Analysis
Quantitative variables were checked for normal distribution via Kolmogorov–Smirnov test for normality. Pearson’s chi-square test was used for different-exposure group comparisons.
Collinearity was assessed via a correlation matrix, using Spearman’s rho correlation coefficient. Relative risks were calculated for all dichotomous variables. Crude odds ratios, adjusted odds ratios, and corresponding 95% confidence intervals (95% CI) were calculated by univariate and conditional multivariate logistic regression, respectively. Interrater agreement was tested with Cohen’s kappa. Alpha level was set at 0.05, while an alpha level of 0.10 was used as cutoff for variable removal in the automated model selection for multivariate regression. All p values were derived from two-sided statistical tests. Statistical analyses were performed using the IBM SPSS 23·0 package (IBM SPSS Statistics for Windows, version 23·0; IBM Corp, Armonk, NY).
Results
A total of 70 vitiligo lesions (36 located on the trunk, 20 on the limbs, 6 on the face, 5 on the hands, and 3 on the feet) from 22 patients (19 females and 3 males with an average age of 42.9 ± 16.1 years and Fitzpatrick’s phototypes 8 II and 14 III) were finally included in the study. Their average baseline surface area was 14.53 ± 20.69 cm [2]. Tables 1 and 2 summarize all baseline dermoscopic and local clinical findings, respectively
At baseline, perifollicular pigmentation was found in 21.4% (15/70) and 4.3% (3/70) of cases on dermoscopic and clinical examination, respectively, with a statistically significant difference in the two methods (p < 0.001). Similarly, leukotrichia was significantly more common on dermoscopic examination compared with clinical assessment (37.1% versus 10.0%; p < 0.001). However, no difference in prevalence of nonfollicular pigmentation was found between baseline clinical and dermoscopic examination (30.0% versus 32.9%; p > 0.05). Finally, follicular red dots were seen in 32.9% of lesions (23/70).
Sixteen lesions (22.9%) from 12 patients achieved improvement according to clinical evaluation, while the figure was slightly higher when the assessment was performed by the above-mentioned computer-aided method, i.e., 25.7% (18/70—from 12 patients); an excellent concordance between the two evaluations was found (94%; κ = 0.85).
Most lesions experiencing improvement (55.6%) showed perifollicular pigmentation on dermoscopy, while only 9.6% of lesions not featuring this finding improved (p < 0.001), with a positive association between presence of dermoscopic perifollicular pigmentation and therapeutic response (OR 11.75, 95% CI 3.17–43.52; p < 0.001) (Fig. 1). The latter OR remained significant after adjustment for all dermoscopic variables and localization (OR 13.57, 95% CI 2.98–61.70; p = 0.001). However, no association (p > 0.05) between therapeutic outcomes and other dermoscopic variables (including leukotrichia) was observed (Table1).
Baseline clinical image of vitiligo involving right armpit (inset: dermoscopic examination shows presence of subclinical perifollicular pigmentation) (a); the same lesions seen by using Fiji software (b). Significant improvement at the end of the 30 sessions of Nb-UVB phototherapy is visible on clinical examination (c) and by using Fiji software (d)
With regard to clinical variables (Table 2), we found a positive correlation between improvement of lesions and face localization (OR 7.28, 95% CI 1.21–43.96; p = 0.030), while no significant correlation (p > 0.05) was seen between therapeutic response and other local clinical variables.
Finally, we observed a significant moderate correlation between face localization and presence of perifollicular pigmentation on dermoscopy (ρ = 0.338 p = 0.004), as this finding was found in 66.7% of cases in such a district versus 22.2% on limbs, 15.0% on trunk, and 0.0% on hands and feet. Moreover, dermoscopy-assessed leukotrichia was also associated to face localization (ρ = 0.398 p = 0.001), being recorded in 100.0% of facial patches versus 38.9% on limbs, 30.0% on trunk, and 0.0% on hands and feet (Fig. 2).
Discussion
According to our study, therapeutic response of NSV to Nb-UVB phototherapy may be affected by local (lesional) factors, with both perifollicular pigmentation on dermoscopy and face localization being correlated with a positive outcome.
The association between dermoscopic perifollicular pigmentation and therapeutic response observed in our analysis is consistent with the biological basis of repigmentation in vitiligo [24,25,26]. Indeed, it is well known that perifollicular areas are the main and initial repigmentation source of nonsegmental vitiligous lesions undergoing Nb-UVB due to activation, migration, proliferation, and differentiation of melanocytic stem cells residing in the hair bulge, which are notoriously more resistant to T cell-mediated attacks probably because their undifferentiated state prevents autoimmune recognition requiring expression of melanocytic differentiation factors/antigens [24,25,26]. In fact, perifollicular repigmentation may be induced by treatments (especially Nb-UVB therapy) but may also occur spontaneously (possibly facilitated by voluntary or accidental sun exposure in some cases) [26]. In such scenario, it is possible that evidence of perifollicular pigmentation on dermoscopy reflect that activation/migration of melanocytic stem cells of the hair bulge is already in place, with consequent greater chances to achieve clinical improvement by their further stimulation following Nb-UVB radiation. Notably, we did not observe any correlation between perifollicular pigmentation on clinical examination and positive therapeutic outcome, likely because naked-eye assessment underestimates the presence of such a finding, as showed in our comparative analysis.
Our findings are in line with previous data emphasizing that perifollicular pigmentation on dermoscopic assessment is, in general, more common in repigmenting vitiligous patches [16,17,18,19,20], though its possible role in predicting therapeutic outcome of a specific treatment has not been reported to date.
The strict association between activation of hair-associated melanocytic precursors and therapeutic response of vitiligo to Nb-UVB also explains the correlation between face localization and positive outcome observed in our analysis and previous studies. Indeed, such an anatomical district is notoriously characterized by a high density of follicular units, which increases the likelihood of gaining clinical improvement [26]. The greater presence of follicles on the face also explains the higher prevalence of dermoscopic follicular features that we found in this area, including perifollicular pigmentation and leukotrichia.
However, we did not find any association between therapeutic response to Nb-UVB (either good or poor) and presence of leukotrichia on either dermoscopic or clinical examination. This is in contrast with the general opinion that vitiligous patches featuring leukotrichia on clinical ground are associated with a lack of therapeutic response due to a possible reduction/absence of follicle-associated melanocytes in white hairs [1,2,3,4,5,6,7,8]. However, the speculated association between leukotrichia and poor therapeutic response is mainly based on studies on segmental vitiligo [27, 28], which is notoriously more resistant to treatments compared with NSV [1,2,3,4,5,6,7,8]. Additionally, some studies showed that it is still possible to find follicle-associated melanocytic precursors in white hairs, which if stimulated, might migrate and differentiate, thereby giving rise to pigment production [29, 30].
Our findings are also in contrast with a recent study that showed a reduced response rate to excimer laser therapy of vitiligous lesions displaying white hairs on dermoscopy [31]. Such difference might be due to the inclusion of a high number of lesions having white hair in the previous study [31] as well as to the different treatments used, since excimer laser and Nb-UVB therapy might have a diverse effect in stimulating follicle-based melanocytic precursors.
Study Limitations
Limitations of this study include the small number of patients and lesions localized on the face as well as the absence of a control group treated with a different therapy. Additionally, since our analysis was a lesion-based study aiming at evaluating possible influence of local factors on therapeutic outcome, we could not assess the influence of patient-based variables on treatment response, e.g., disease duration, age, sex, comorbidities, and phototype.
Conclusions
The results of our study underline that therapeutic response of vitiligo to Nb-UVB phototherapy may be positively affected by local features of the lesions, including face localization and presence of perifollicular pigmentation on baseline dermoscopic examination, which might be considered as positive response predictor factors useful to optimize treatment of vitiligo and better inform patients about their expected results.
Although we speculated that such findings might be related to a greater likelihood of repigmentation through activation/migration of melanocytic stem cells of the hair bulge, future studies assessing possible histological and immunohistochemical correlations are needed to confirm our assumption.
References
Krüger C, Schallreuter KU. A review of the worldwide prevalence of vitiligo in children/adolescents and adults. Int J Dermatol. 2012;51:1206–12.
Taïeb A, Picardo M. Vitiligo. N Engl J Med. 2009;360:160–9.
Bergqvist C, Ezzedine K. Vitiligo: a review. Dermatology. 2020;10:1–22.
Njoo MD, Westerhof W. Vitiligo: pathogenesis and treatment. Am J Clin Dermatol. 2001;2:167–81.
Stinco G, Trevisan G, Buligan C, Gregoraci G, De Marchi S, di Meo N, Patrone P. Narrow band-ultraviolet B versus clobetasol propionate foam in the treatment of vitiligo: a retrospective study. Dermatol Ther (Heidelb). 2013;3:95–105.
Stinco G, Buligan C, Grimaldi F, Valent F, Patrone P. Serological screening for autoimmune polyendocrine syndromes in patients with vitiligo. J Eur Acad Dermatol Venereol. 2012;26:1041–2.
Bae JM, Jung HM, Hong BY, et al. Phototherapy for vitiligo, a systematic review and meta-analysis. JAMA Dermatol. 2017;153:666–74.
Alkhateeb A, Fain PR, Thody A, Bennett DC, Spritz RA. Epidemiology of vitiligo and associated autoimmune diseases in Caucasian probands and their families. Pigment Cell Res. 2003;16:208–14.
Nicolaidou E, Antoniou C, Stratigos AJ, Stefanaki C, Katsambas AD. Efficacy, predictors of response, and long-term follow-up in patients with vitiligo treated with narrowband UVB phototherapy. J Am Acad Dermatol. 2007;56:274–8.
Errichetti E, Lallas A, Apalla Z, Di Stefani A, Stinco G. Dermoscopy of granuloma annulare: a clinical and histological correlation study. Dermatology. 2017;233:74–9.
Errichetti E, Piccirillo A, Stinco G. Dermoscopy as an auxiliary tool in the differentiation of the main types of erythroderma due to dermatological disorders. Int J Dermatol. 2016;55:e616–e618618.
Errichetti E, Piccirillo A, Viola L, Stinco G. Dermoscopy of subacute cutaneous lupus erythematosus. Int J Dermatol. 2016;55:e605–e607607.
Errichetti E, De Francesco V, Pegolo E, Stinco G. Dermoscopy of Grover's disease: variability according to histological subtype. J Dermatol. 2016;43:937–9.
Errichetti E, Stinco G. Dermatoscopy of granulomatous disorders. Dermatol Clin. 2018;36:369–75.
Errichetti E, Stinco G. Dermoscopy in differentiating palmar syphiloderm from palmar papular psoriasis. Int J STD AIDS. 2017;28:1461–3.
Errichetti E. Dermoscopy of inflammatory dermatoses (inflammoscopy): an up-to-date overview. Dermatol Pract Concept. 2019;9:169–80.
Chuh AAT, Zawar V. Demonstration of residual perifollicular pigmentation in localized vitiligo—a reverse and novel application of digital epiluminescence dermoscopy. Comput Med Imaging Graph. 2004;28:213–7.
Jha AK, Sonthalia S, Lallas A. Dermoscopy as an evolving tool to assess vitiligo activity. J Am Acad Dermatol. 2018;78:1017–9.
Errichetti E, Stinco G. Dermoscopy in general dermatology: a practical overview. Dermatol Ther (Heidelb). 2016;6:471–507.
Thatte S, Khopkar U. The utility of dermoscopy in the diagnosis of evolving lesions of vitiligo. Indian J Dermatol Venereol Leprol. 2014;80:505.
Mohammad TF, Al-Jamal M, Hamzavi IH, et al. The Vitiligo Working Group recommendations for narrowband ultraviolet B light phototherapy treatment of vitiligo. J Am Acad Dermatol. 2017;76:879–88.
Errichetti E, Zalaudek I, Kittler H, et al. Standardization of dermoscopic terminology and basic dermoscopic parameters to evaluate in general dermatology (non-neoplastic dermatoses): an expert consensus on behalf of the International Dermoscopy Society. Br J Dermatol. 2020;182:454–67.
Hamzavi I, Jain H, McLean D, Shapiro J, Zeng H, Lui H. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch Dermatol. 2004;140:677–83.
Birlea SA, Goldstein NB, Norris DA. Repigmentation through melanocyte regeneration in Vitiligo. Dermatol Clin. 2017;35:205–18.
Lee JH, Fisher DE. Melanocyte stem cells as potential therapeutics in skin disorders. Expert Opin Biol Ther. 2014;14:1569–79.
Bolognia JL, Orlow SJ. Melanocyte Biology. In: Bolognia JL, Schaffer JV, Cerroni L, editors. Dermatology. 4th ed. Oxford: Elsevier; 2018. p. 1092.
Lee DY, Kim CR, Park JH, Lee JH. The incidence of leukotrichia in segmental vitiligo: implication of poor response to medical treatment. Int J Dermatol. 2011;50:925–7.
Lee DY, Lee JH. White hairs in segmental vitiligo are related to poor response to phototherapy: demonstration with portable digital microscopy. J Dermatol. 2010;37:500–1.
Song HS, Choi GS, Shin JH. Preservation of melanoblasts of white hair follicles of segmental vitiligo lesions: a preliminary study. J Eur Acad Dermatol Venereol. 2011;25:240–2.
Jee HJ, Do JE, Noh S, Park SH, Oh SH. Leukotrichia in stable segmental vitiligo: implication of an alternate treatment option. Ann Dermatol. 2014;26:132–4.
Kim MS, Cho EB, Park EJ, Kim KJH, Kim KJH. Effect of excimer laser treatment on vitiliginous areas with leukotrichia after confirmation by dermoscopy. Int J Dermatol. 2016;55:886–92.
Acknowledgements
We would like to thank the patients for participation.
Funding
No Rapid Service Fee was received by the journal for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Enzo Errichetti is a member of the Editorial Board. Enrico Zelin, Caterina Pinzani, Athanassios Kyrgidis, Aimilios Lallas and Giuseppe Stinco have nothing to disclose.
Compliance with Ethics Guidelines
The research was conducted in accordance with ethics guidelines and the declaration of Helsinki 1964 and its later amendments. And all the participants gave their informed consent to take part in the study and use personal records or photos for scientific purposes. Local ethical committee (Comitato Etico Unico Regionale (C.E.U.R.) del Friuli Venezia Giulia) approval was obtained (study ID: 2284, code: VIT-fot_DERMOSC.01).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request..
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12689801.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Errichetti, E., Zelin, E., Pinzani, C. et al. Dermoscopic and Clinical Response Predictor Factors in Nonsegmental Vitiligo Treated with Narrowband Ultraviolet B Phototherapy: A Prospective Observational Study. Dermatol Ther (Heidelb) 10, 1089–1098 (2020). https://doi.org/10.1007/s13555-020-00431-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-020-00431-6