Abstract
Introduction
Anogenital warts (AGW) are a relevant clinical issue in the field of sexually transmitted disease, and to date no treatment provides a satisfactory clearance rate. Treatment can be both medical and surgical, and be provided by a healthcare provider or by the patient. Cryotherapy (CRYO) is among the most common treatments for AGW. Nitrizinc® Complex solution (NZCS) is a solution containing organic acids, nitric acid and zinc and copper salts that is applied topically to warts, producing mummification of the damaged tissue. It is considered to be an effective and well-tolerated treatment for genital and common warts. The aim of our study was to compare NZCS to CRYO in the treatment of AGW.
Methods
We performed a prospective, multicentre, single-blind, randomised, superiority clinical study involving 120 patients, aged 18–55 years, diagnosed with a first episode of AGW, with each patient having from three to ten AGW. The patients were treated either with NZCS or CRYO for a maximum of four treatments. Primary endpoints were: (1) comparison of the clinical efficacy of CRYO and NZCS, based on response to treatment (clearance of AGW) within four treatment sessions; and (2) tolerability, assessed via a short questionnaire at the end of each treatment session. Secondary endpoints were: (1) number of treatments needed for clearance; and (2) recurrence at 1 and 3e months after confirmed clearance. The results were analysed on an intention-to-treat basis.
Results
A complete response was achieved in 89.7% of the NZCS group and in 75.4% of the CRYO group (p = 0.0443). NZCS was found to be better tolerated. There was no difference between the NZCS and CRYO treatment arms in the number of sessions needed to clear the lesions. Recurrence occurred after 1 month in 18.4% of the NZCS group and 38.1% of the CRYO group (p = 0.0356), and after 3 months in 25 and 40.6% of these groups, respectively (p = 0.1479).
Conclusions
Nitrizinc® Complex solution can be considered to be as effective as CRYO for the treatment of small (< 5 mm) external AGW, with a better tolerability profile and lower rate of recurrence.
Trial Registration
ISRCTN identifier, ISRCTN36102369.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anogenital warts (AGW) are a relevant clinical issue in the field of sexually transmitted disease, and to date no treatment provides a satisfactory clearance rate. Treatment can be both medical and surgical and applied by a healthcare provider or by the patient him/herself. |
The aim of our study was to compare Nitrizinc® Complex Solution (NZCS) to cryotherapy (CRYO) in the treatment of AGW. |
The results show that NZCS was as effective as CRYO for the treatment of small (< 5 mm), external AGW, and showed a higher efficacy, a lower rate of reccurence and a better tolerability profile. |
These results suggest that NZCS should be considered one of the main treatments for AGW. |
NZCS is not mentioned in the last European IUSTI (International Union Against Sexually Transmitted Infections) guidelines as an official treatment for AGW. We hope that the results of this comparative study will support the inclusion of NZCS as treatment for AGW in future treatment guidelines. |
Introduction
Anogenital warts (AGW) are benign lesions of the epidermis caused by several genotypes of human papilloma virus [1] that affect the anogenital region of both women and men [2]. Low-risk HPV types 6 and 11 are responsible for > 90% of cases of AGW [3]. AGW are the most commonly diagnosed disease in centres for sexually transmitted diseases worldwide. Patients affected with AGW often feel embarrassment, shame, anger, depression and guilt [4]. AGW place an important economic burden on public healthcare as patients have a high number of recurrences and no current therapy provides a satisfactory clearance rate [5, 6].
In their recent meta-analyses on the effectiveness of treatments for AGW, Barton et al. [15] conclude that laser CO2 seems to be the most effective method but also that patient preference tends towards nonablative methods. Bertolotti et al. [16, 17] indicate electrosurgery and 0.5% podophyllotoxin as the most effective methods and recommend an randomised controlled trial on the combined therapies.
Cryotherapy (CRYO) is among the most common treatments of AGW [12, 13]. Nitrizinc® Complex solution (NZCS) is a solution containing organic acids, nitric acid and zinc and copper salts that is applied topically to warts, producing mummification of the damaged tissue [7]. It is considered to be an effective and well-tolerated treatment for genital and common warts [8,9,10,11]. NZCS has recently been mentioned in the guidance on management of AGW in daily practice [5, 14]. The aim of our study was to compare NZCS to CRYO for the treatment of AGW in terms of efficacy, tolerability and recurrence rate.
Methods
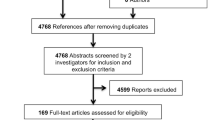
This study was a prospective, multicentre, single-blind, randomised, superiority clinical study with the aim to compare the efficacy and safety of NZCS and CRYO in the treatment of AGW. To ensure objective evaluation of the efficacy and safety of the two different treatments, two investigators (dermatologists) were involved in the study at each study centre, with one applying the treatment according to the randomisation list and the other evaluating the treatment response; both investigators were blinded to which treatment had been applied. The number of patients considered to be an adequate number to draw clinically relevant conclusions was 120.
Consequently, 120 patients were enrolled in the study from October 2017 to July 2019. All were being treated at one of the three participating centres in in Italy: Centre of Sexually Transmitted Diseases, U.O.C. Dermatology, IRCCS Ca 'Granda Ospedale Maggiore Policlinico of Milan; Centre for Sexually Transmitted Diseases, U.O. Dermatology, A.O. Policlinico Sant’Orsola-Malpighi, Bologna; and Centre of Genital Dermatology and Sexually Transmitted Infections relating to Complex Structure Dermatology, A.O.U. Città della salute e della Scienza, Turin.
The study was approved by the Ethics Committees of all three participating hospitals and performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All patients provided written informed consent to participate. This clinical trial was registered with the ISRCTN site with code ISRCTN36102369.
All patients who met all inclusion criteria were enrolled. After reading and signing the informed consent, patients were assigned to one of the two treatment arms according to a randomised schedule. Two lists of randomisations (block of 4) were generated, one for women and one for men, to ensure gender balance in each treatment arm. Sixty patients were treated with NZCS and 60 patients with CRYO. The inclusion criteria were: age 18–55 years; first episode of AGW; number of AGW ranging from three to ten; diameter of each AGW ranging from 1 to 4 mm; AGW located on penis, vulva, perianal region. The exclusion criteria were: previously treated AGW; immunosuppression due to pathological and/or iatrogenic causes; diabetes mellitus; pregnancy.
Women of childbearing potential who were eligible enrolment in the study were requested to use adequate contraceptive methods for the duration of the study.
Therapeutic Protocols
Cryotherapy treatment is based on the application of liquid nitrogen. Nitrogen is an inert, non-flammable gas that in the liquid state reaches − 196 °C, a temperature suitable for the induction of cytolysis of pathological tissue. Liquid nitrogen can be applied to the wart by means of various devices, among which the most commonly used are those that allow the product to be sprayed [18]. In this study,all participating centres used the same CRY-AC-3® liquid nitrogen cryosurgery device (Brymill, Ellington, CT, USA). The duration of application varies according to the lesion treated, but lasts on average a few seconds.
NZCS (Verrutop®; ISDIN, Barcelona, Spain; medical device class II) has a targeted action on pathological tissue (sparing healthy tissue); it is well tolerated and does not cause scarring. In addition to its ablative action, it also has an antiviral action, mediated by nitric oxide generated during therapy, to reduce the risk of recurrence. The product comes as a solution in disposable ampoules; it is extracted from the vial by means of a capillary and applied directly to the wart by direct contact. NZCS applied on the warts causes a change in colour (white-yellowish) and a hardening of the treated tissue, thus promoting detachment of the wart. The application, carried out by medical personnel, can be repeated several times at the same location and during the same session until the lesion takes on a yellowish-white color [9, 19, 20].
Study Design
For both treatment arms (CRYO or NZCS), the enrolled patients were re-evaluated at 10 days after the first treatment session. If AGW persisted, the application of the treatment was repeated, with a maximum of four treatment sessions. The number and location (anal or genital area) of AGW observed and demographic data (gender, age, nationality) were recorded at each session.
At the end of the course of treatment, the investigating dermatologist, who was blinded to treatment, assessed the response at 10 days after the last application as: complete clearance; partial clearance (≥ 50% reduction in the number of lesions); or no clearance (< 50% reduction in the number of lesions).
Tolerability was assessed at each evaluation by the investigating dermatologist (blinded also to treatment) and by the patient based on three parameters:
-
Pain. As reported by the patient and assessed on a numeric rating scale as: 0, absent; 1, mild; 2, moderate; 3, intense.
-
Itching. As reported by the patient and assessed on a numeric rating scale as: 0, absent; 1, mild; 2, moderate; 3, intense.
-
Inflammation. Assessed on a numeric rating scale as: 0, absent; 1, erythema; 2, erosion; 3, blisters; 4, ulcer.
Tolerability of each study product was also evaluated at the last study evaluation (10 days after the last application) with a short questionnaire that asked patients to rate the treatment’s tolerability as high, moderate or low.
Patients with complete clearance within the constraint of four treatment sessions then started follow-up (FT0), while patients with partial or no clearance after the fourth treatment session were started on a different, conventional treatment. Follow-up visits were carried out at 1 month (FT1) and 3 months (FT3) after the last study treatment application. In the event of recurrence during the follow-up, the patient was switched to a different, conventional treatment. The results obtained were analysed for efficacy, tolerability and recurrence.
Objectives
The primary endpoints were:
-
Clinical efficacy of CRYO and NZCS for the treatment of external AGW, as determined by a comparative procedure. Response to treatment (clearance), with a maximum of four sessions, was evaluated.
-
Tolerability of the treatments, assessed with a short questionnaire at the end of each treatment session.
The secondary endpoints were:
-
Number of treatments needed to achieve clearance, for each treatment.
-
Evaluation of recurrence at 1 and 3 months after confirmed clearance, for each treatment.
Statistical Analysis
A descriptive statistical analysis was carried out for all variables. Continuous variables were described as the number of valid cases, mean and standard deviation. Categorical variables were described as absolute and relative frequency over the total valid values (N). In cases of missing values, their number has been described per group.
Categorical variables were compared using the chi-square test to evaluate the homogeneity of the values between groups and between sessions. Continuous variables were compared using the Student's t test for unpaired data for comparisons between different groups of patients and for paired data for comparisons between different times for the same patients. For all comparisons, statistical significance was set at 0.05. All analyses were performed on the data set using all available information on an intention-to-treat basis. The statistical analysis was carried out using the SAS (Statistical Analysis System) program, version 9.2.
Results
Demographic Data
Of the 120 patients recruited, 60 were enrolled in the CRYO treatment arm and 60 in the NZCS treatment arm (20 patients in each arm at each site; 40 patients total per site). There were no relevant between-group differences in baseline characteristics (Table 1). The average age of the patients was 31.73 ± 9.37 years, with no significant differences between NZCS (31.53 ± 9.43) and CRYO (31.93 ± 9.38) groups. Of the enrolled patients, 58.3% were men, with a similar percentage in the two treatment arms. Five patients were lost to follow-up during the study treatment period.
At enrolment, the total number of AGW diagnosed in all patients was 647 (mean 5.39 ± 2.84 per patient), of which 311 AGW (mean 5.18 ± 2.57) and 336 AGW (mean 5.66 ± 3.09) were treated with NCZS and CRYO, respectively. The majority of AGW were located in the genital area, with 235 warts (mean 3.92 ± 2.95) in the NZCS group and 237 warts (mean 3.95 ± 3.47) in the CRYO group.
Evaluation of Effectiveness
Nitrizinc Complex solution was more effective than CRYO (89.7 vs. 75.4%), with a maximum of four treatment applications. This difference did not reach statistical significance. There was no response in three patients (2.6%): one in the NZCS group and two in the CRYO group.
As a secondary approach to further analyse complete response, the number of subjects with no response was merged with the number of subjects with partial response. In this comparison, the difference in efficacy of NZCS versus CRYO, within a maximum of four treatment applications, did reach statistical significance (p = 0.044) (Table 2).
Evaluation of the Number of Sessions Required for Clinical Clearance
The mean number of sessions required for complete resolution of AGW was 1.83 ± 0.83 visits for those treated with NZCS and 1.88 ± 0.91 for those treated with CRYO. The difference between the two groups was not statistically significant (Table 3).
Evaluation of Recurrence
Patients in the NZCS treatment group who achieved complete AGW resolution showed lower recurrence at FT1 (18.4%) and FT2 (25%) than did those in the CRYO treatment group at these same time points (38.1 and 40.6%, respectively). The difference was statistically significant at the 1-month follow-up visit (FT1) (p = 0.0356) but not at the 3-month follow-up visit (FT2) (Table 4).
Evaluation of Tolerability
After a maximum of four treatment sessions, NZCS was assessed as better tolerated than CRYO, with the treatment tolerability evaluated as “high” by 75.9 and 62.5% of patients in the NZCS and CRYO treatment arms, respectively (Table 5). This difference was statistically significant (p = 0.0097).
Discussion
Our study is innovative in that, to the best of our knowledge, it is the first randomised controlled study to assess the effectiveness of NZCS against another treatment in the treatment of AGW. In our study, the comparator treatment was CRYO, which is one of the reference treatments for AGW [5, 21].
In order to minimise bias in the evaluation of the clinical results, two investigators participated at each centre, with one applying the treatment according to the randomisation schedule and the other (blined to treatment) independently interpreting the data. While this resulted in a number of in terms of the logistics of the study, but it did ensure an objective analysis of each treatment’s efficacy and safety.
NZCS is an aqueous solution containing organic acids (lactic, oxalic and acetic acid), a small proportion of metal ions (zinc and copper) and 65% nitric acid as the main component. Its application changes the structure of the wart through denaturation of the cellular and viral proteins, thereby facilitating devitalisation of the tissue proteins of the lesion (mummification process). It also has an antiviral effect through the reduction of viral DNA in the treated tissue [20].
The efficacy of NZCS has been described previously in five studies [8–11, 17]. The first of these, published in 2015 by Cusini et al. [17] showed that NZCS has an 87% efficacy in 30 patients after one to four applications [17].The second study, published by Rozas-Munoz et al. in 2019 [10], involved 15 patients and reported an efficacy of 88.3% and no recurrence in the 3-month follow-up. The third study, by Ciccarese et al. [8], also published in 2019, is one of the most interesting due to the number of patients treated (100), the number of AGW treated (418) and the length of follow-up (6 months). NZCS was reported by these authors to be effective in treating 92% of warts in ≤ 4 therapy sessions, with 23% of patients showing recurrence at 3 months and 5% at 6 months [8]. In a more recently published study, Kelati et al. [9] reported on the use of NZCS in 11 patients with recurring AGW after different previous treatments, with 100% efficacy of NZCS after one application. One patient had recurrence of AGW but not in the same location [9]. In the latest published study on NZCS, Puviani et al. [11] demonstrated that NZCS had better efficacy and tolerability compared to several other treatments. However, this study had a number of limitations such as a small number of patients and the lack of evaluation of complete clearance.
The results obtained in our study with NZCS show a similar level of efficacy (89.7%) as those reported in these earlier studies, confirming the effectiveness of this treatment. A 75.4% rate of efficacy was obtained in the CRYO arm of our study, which is comparable to previously reported values, ranging from 46 to 96% [13, 22]. In comparison, treatment efficacy in the NZCS after a maximum of four sessions was slightly higher, and this difference was statistically significant (p = 0.044).
The study demonstrated no significant difference in the number of sessions needed to clear the lesions (1.83 NZCS vs 1.86 CRYO).
The number of recurrences after one month was lower in the NZSC (18.4%) than the CRYO group (38.1%) (p = 0.0356). At three months’ follow-up the number of recurrences was still lower in the NZCS group (25%) than the CRYO group (40%) but not statistically significant (p = 0.1479). NZCS showed better tolerability than CRYO (p = 0.0097).
There were a low number of dropouts in our study, likely reflecting the good tolerability of both treatments and the high, negative psychological impact of new genital warts on patients, resulting in a strong motivation for fast, effective treatment.
Our study demonstrates the benefits of NZCS in the treatment of AGW. Both efficacy and tolerability were higher in the NZCS treatment arm than in the CRYO treatment arm. In addition, in a direct comparison of NZCS and CRYO, there were fewer recurrences in the NZCS treatment arm at the 1-month follow-up. For some of the parameters evaluated, the study did not show statistical significance, but the trend seemed to be in favour of NZCS.
Although in our study we did not observe severe side effects in either treatment arm, hypopigmentation has been reported in the literature to be a real concern, especially on individuals with dark skin treated with CRYO. We observed, in contrast to other ablative methods, the absence of any cicatricial or dyschromic outcome (Fig. 1). In addition, the post-treatment management was very simple, without any ulcerative or infectious complications [18, 21, 24].
Regarding the use of NZCS in the setting of public healthcare centres, our results suggest that NZCS is a simple and quick treatment that requires no particular devices and as such should be considered as treatment in the context of both public sexually transmitted infection units and private practice. Healthcare providers can be easily trained to use devices to apply NZCS.
One limitation to our study was the short (3 month) follow-up, which was chosen because most recurrences occur within this period. However, it would be interesting to extend the follow-up period in future studies. Another important point to be emphasised is that we performed the study on small (< 5 mm) and limited numbers of AGW. Larger and more numerous lesions may need a higher number of sessions.
Conclusion
Nitrizinc® Complex Solution demonstrated good efficacy and safety compared with CRYO for the treatment of external AGW, with a higher efficacy than CRYO. We believe therefore that NZCS should be considered as one of the main treatments for AGW. At the time of writing this article, NZCS is not mentioned in the last European IUSTI (International Union Against Sexually Transmitted Infections) guidelines as an official treatment for AGW. We hope that the results of our comparative study will support the inclusion of NZCS as treatment for AGW in future guidelines [23, 25].
References
Buck HW Jr. Warts (genital). BMJ Clin Evid. 2010;2010:1602.
Lynde C, Vender R, Bourcier M, Bhatia N. Clinical features of external genital warts. J Cutan Med Surg. 2013;17(Suppl 2):S55–S60.
Patel H, Wagner M, Singhal P, Kothari S. Systematic review of the incidence and prevalence of genital warts. BMC Infect Dis. 2013;13:39. https://doi.org/10.1186/1471-2334-13-39.
Woodhall S, Ramsey T, Cai C, et al. Estimation of the impact of genital warts on health-related quality of life. Sex Transm Infect. 2008;84(3):161–6. [Published correction appears in Sex Transm Infect. 2008 Aug;84(4):328]. https://doi.org/10.1136/sti.2007.029512.
O'Mahony C, Gomberg M, Skerlev M, et al. Position statement for the diagnosis and management of anogenital warts. J Eur Acad Dermatol Venereol. 2019;33(6):1006–199. https://doi.org/10.1111/jdv.15570.
Pasqua A, Costa S, Salfa M, Lapi F, Suligoi B. Genital warts: data from the italian general pratictioner. Sex Transm Infect. 2013;89:A159. https://doi.org/10.1136/sextrans-2013-051184.0496.
Viennet C, Gheit T, Muret P, et al. Assessment of the efficacy of a new formulation for plantar wart mummification: new experimental design and human papillomavirus identification. Clin Exp Dermatol. 2013;38(1):85–8. https://doi.org/10.1111/ced.12025.
Ciccarese G, Drago F, Granger C, Parodi A. Efficacy assessment of a topically applied nitric-zinc complex solution for the treatment of external ano-genital warts in 100 patients. Dermatol Ther (Heidelb). 2019;9(2):327–35. https://doi.org/10.1007/s13555-019-0300-7.
Kelati A, Khemis A, Montaudié H, Lacour JP, Passeron T. Successful treatment of resistant condylomas with nitrizinc complex solution: a retrospective study in 11 patients. J Eur Acad Dermatol Venereol. 2019;33(2):e88–e89. https://doi.org/10.1111/jdv.15241.
Rozas-Muñoz E, Mir-Bonafé J, Piquero-Casals J. Refractory warts successfully treated with a nitric-zinc complex solution. J Dermatol. 2019;46(7):e250–e251251. https://doi.org/10.1111/1346-8138.14795.
Puviani M, Manfredini M, Eisendle K. The SILVER study. Efficacy of topical nitric-zinc complex solution in the treatment of resistant warts: a postmarketing evaluation. Dermatol Ther. 2019;32(4):e12940. https://doi.org/10.1111/dth.12940.
Bertolotti A, Dupin N, Bouscarat F, Milpied B, Derancourt C. Cryotherapy to treat anogenital warts in nonimmunocompromised adults: systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):518–26. https://doi.org/10.1016/j.jaad.2017.04.012.
Godley MJ, Bradbeer CS, Gellan M, Thin RN. Cryotherapy compared with trichloroacetic acid in treating genital warts. Genitourin Med. 1987;63(6):390–2. https://doi.org/10.1136/sti.63.6.390.
Delmonte S, Benardon S, Cariti C, Ribero S, Ramoni S, Cusini M. Anogenital warts treatment options: a pratical approach. G Ital Dermatol Venereol. 2018. https://doi.org/10.23736/S0392-0488.18.06125-4.
Barton S, Wakefield V, O'Mahony C, Edwards S. Effectiveness of topical and ablative therapies in treatment of anogenital warts: a systematic review and network meta-analysis. BMJ Open. 2019;9(10):e027765. https://doi.org/10.1136/bmjopen-2018-027765.
Bertolotti A, Milpied B, Fouéré S, Cabié A, Dupin N, Derancourt C. Local management of anogenital warts in immunocompetent adults: systematic review and pooled analysis of randomized-controlled trial data. J Am Acad Dermatol. 2019;81(5):1203–4. https://doi.org/10.1016/j.jaad.2019.04.008.
Bertolotti A, Ferdynus C, Milpied B, Dupin N, Huiart L, Derancourt C. Local management of anogenital warts in non-immunocompromised adults: a network meta-analysis of randomized controlled trials. Dermatol Ther (Heidelb). 2020;10(2):249–62. https://doi.org/10.1007/s13555-020-00357-z.
Zimmermann E-E, Crawford P. Cutaneous cryosurgery. Am Acad Family Physicians. 2012;86(12):1118–24.
Janniger CK, Schwartz RA. Efficacy and tolerability of a new topical nitric-zinc preparation for "difficult-to-treat" warts. Dermatol Ther. 2017. https://doi.org/10.1111/dth.12456.
Cusini M, Micali G, Lacarrubba F, Puviani M, Barcella A, Milani M. Efficacy and tolerability of nitric-zinc complex in the treatment of external genital warts and "difficult-to-treat" warts: a "proof of concept", prospective, multicentre, open study. G Ital Dermatol Venereol. 2015;150(6):643–8.
Jahic M. Cryotherapy of genital warts. Mater Sociomed. 2019;31(3):212–4. https://doi.org/10.5455/msm.2019.31.212-214.
Stone KM, Becker TM, Hadgu A, Kraus SJ. Treatment of external genital warts: a randomised clinical trial comparing podophyllin, cryotherapy, and electrodesiccation. Genitourin Med. 1990;66(1):16–9. https://doi.org/10.1136/sti.66.1.16.
Lacey CJ, Woodhall SC, Wikstrom A, Ross J. 2012 European guideline for the management of anogenital warts. J Eur Acad Dermatol Venereol. 2013;27(3):e263–e270. https://doi.org/10.1111/j.1468-3083.2012.04493.x.
Wetmore SJ. Cryosurgery for common skin lesions. Treatment in family physicians' offices. Can Fam Physician. 1999;45:964–74.
Workowski KA, Bolan GA, Centers for Disease Control, and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1–137. [Published correction appears in MMWR Recomm Rep. 2015 Aug 28;64(33):924].
Acknowledgements
The authors would like to thank the patients for their participation in this study.
Funding
The study was sponsored by the Interdisciplinary Society for Sexually transmitted Diseases (Società Interdisciplinare Malattie aTrasmissione Sessuale [SIMAST]). ISDIN funded the Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing Assistance
J. Marshall, a professional freelance medical writer, assisted in editing the manuscript, funded by ISDIN.
Disclosures
Paolo Pontini, Luca Mastorino, Valeria Gaspari, Corinne Granger, Stefano Ramoni, Sergio Delmonte, Valeria Evangelista and Marco Cusini have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Ethics Committees of all three participating hospitals and performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All patients provided written informed consent to participate.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12687944.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pontini, P., Mastorino, L., Gaspari, V. et al. A Multicentre, Randomised Clinical Trial to Compare a Topical Nitrizinc® Complex Solution Versus Cryotherapy for the Treatment of Anogenital Warts. Dermatol Ther (Heidelb) 10, 1063–1073 (2020). https://doi.org/10.1007/s13555-020-00430-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-020-00430-7