Abstract
Background
Even though skeletal muscle (SM) is the largest body compartment in most adults and a key phenotypic marker of sarcopenia and cachexia, SM mass was until recently difficult and often impractical to quantify in vivo. This review traces the historical development of SM mass measurement methods and their evolution to advances that now promise to provide in-depth noninvasive measures of SM composition.
Methods
Key steps in the advancement of SM measurement methods and their application were obtained from historical records and widely cited publications over the past two centuries. Recent advances were established by collecting information on notable studies presented at scientific meetings and their related publications.
Results
The year 1835 marks the discovery of creatine in meat by Chevreul, a finding that still resonates today in the D3-creatine method of measuring SM mass. Matiegka introduced an anthropometric approach for estimating SM mass in 1921 with the vision of creating a human “capacity” marker. The 1940s saw technological advances eventually leading up to the development of ultrasound and bioimpedance analysis methods of quantifying SM mass in vivo. Continuing to seek an elusive SM mass “reference” method, Burkinshaw and Cohn introduced the whole-body counting-neutron activation analysis method and provided some of the first detailed reports of cancer cachexia in the late 1970s. Three transformative breakthroughs leading to the current SM mass reference methods appeared in the 1970s and early 1980s as follows: the introduction of computed tomography (CT), photon absorptiometry, and magnetic resonance (MR) imaging. Each is advanced as an accurate and/or practical approach to quantifying whole-body and regional SM mass across the lifespan. These advances have led to a new understanding of fundamental body size-SM mass relationships that are now widely applied in the evaluation and monitoring of patients with sarcopenia and cachexia. An intermediate link between SM mass and function is SM composition. Advances in water-fat MR imaging, diffusion tensor imaging, MR elastography, imaging of connective tissue structures by ultra-short echo time MR, and other new MR approaches promise to close the gap that now exists between SM anatomy and function.
Conclusions
The global efforts of scientists over the past two centuries provides us with highly accurate means by which to measure SM mass across the lifespan with new advances promising to extend these efforts to noninvasive methods for quantifying SM composition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Sarcopenia, sarcopenic obesity, and cachexia all share a common phenotype: relative reductions in the amount, composition, and function of skeletal muscle [1]. Although often the largest compartment at the tissue-organ level of body composition [2], quantifying the total mass and composition of skeletal muscle in living subjects proved remarkably difficult over the past century compared to fat, bone mineral, body fluids, and other relatively large compartments of clinical interest.
The complexity of measuring skeletal muscle mass seems hard to imagine today when we have several easily applied and widely available measurement techniques that provide accurate regional and whole-body estimates from birth onward. We review here the history of this struggle and the recent advances that provide us with powerful tools to study the disorders that involve loss of skeletal muscle mass and related function. This remarkable journey unfolds over almost two centuries, covers several continents, and represents the imaginative contributions of scientists across the globe.
2 Foundation discoveries
2.1 A muscle-urine connection
While it is hard to precisely identify the first historical step in quantifying skeletal muscle mass, the likely initial discovery of a measurement approach belongs to the renowned French chemist and polymath Michel-Éugène Chevreul, who in 1835 first identified a chemical compound in meat extracts that he named creatine, the Greek word for flesh [3]. Otto Folin, working almost two decades later at Harvard, transformed the field by developing a highly sensitive measurement method in 1905 and then going on to establish the “creatinine coefficient” as a focus of research that persists today, more than one-century later [4]. Folin astutely recognized that individuals excrete a relatively stable amount of creatinine in the urine over time, and he calculated his coefficient as grams per 24 h/kg body weight reflecting a link between creatine production and body mass [4]. Max Bürger, working with muscle disease patients at the University of Kiel, first estimated a creatinine equivalence in 1919 reported as 1 g/day urinary creatinine = 22.9 kg of whole skeletal muscle [5]. By 1928, Hahn and Meyer closed the loop by establishing the source of urinary creatinine as the stable nonenzymatic breakdown of creatine, 98 % of which is in skeletal muscle at fairly stable concentrations [6]. Nathan Talbot at Harvard, in a widely cited 1938 paper [7], provided support for a creatinine equivalence of 17.9 kg/g with ingestion of a general diet. By the late 1960s, investigators such as Joan Graystone working at Johns Hopkins University were further refining the creatinine equivalence (20 kg/g) and used this method to describe aspects of childhood skeletal muscle growth and development [8, 9].
Urine is difficult to collect over several days as is ideally required for the creatinine-skeletal muscle mass method. This limitation led investigators to seek an alternative strategy, and one based on isotopic measurement of the creatine pool size emerged in the early 1970s. With this approach, investigators apply the general formula, skeletal muscle mass = creatine pool/skeletal muscle creatine concentration. Kreisberg et al., working at the University of Alabama in Birmingham, used this approach in 1970 with 14C-labeled creatine [10], and Picou et al. in 1976 working at the Tropical Metabolism Unit in Jamaica made similar measurements with 15N-creatine [11].
A consistent theme through all of this research was the lack of an in vivo reference method for quantifying skeletal muscle mass in humans. Reliance was largely based on data from animal studies, a few available human cadaver dissections, or skeletal muscle biopsies. Remarkably, it was not until 1996 that “official” proof of concept for the creatine-creatinine approach for estimating skeletal muscle was obtained in humans. Wang et al. [12], working at Columbia University, collected urine over several days from 12 healthy adult men who had total body skeletal muscle mass measured by the emerging whole-body computed tomography (CT) method. Wang confirmed the strong link between urinary creatinine and total body skeletal muscle mass in healthy men with an R of 0.92 and an SEE of 1.89 kg (p < 0.0001). The power of modern three-dimensional whole-body imaging brings us to the present when Stimson et al. [13] used magnetic resonance imaging (MRI) to estimate skeletal muscle mass and the stable isotope deuterated creatine (DCR) to quantify the creatine pool size in adults. The isotope, enclosed in a gel capsule, is ingested, and a urine sample collected several days later is used to estimate DCR by mass spectroscopy. The measured dilution space is strongly correlated (r = 0.87) with total body skeletal muscle mass as measured with MRI [13].
2.2 Muscle as a human capacity marker
Just after the collapse of the Habsburg monarchy, Jindřich Matiegka, working at the University of Prague a few years after World War I, communicated his body composition vision in a May 7, 1920 letter to the prominent US physical anthropologist Aleš Hrdlička: “I shall send my proposal for establishing a commission that would work out a method for assessing work efficiency of the human body. I justify my proposal by pointing out that it is a duty of anthropology to develop a method for testing human physical capacity, similar to the methods worked out by psychologists to test mental capacity. Mental and physical capacities together constitute the working capacity and determine the working efficiency of the person” [14]. A year later, Matiegka published what is likely the seminal paper describing anthropometric measurement of skeletal muscle mass and three other functional body compartments [15].
Matiegka’s system considered body weight (W) the sum of four components,
where O is skeletal (osseous) weight, D is skin plus subcutaneous adipose tissue weight, M is skeletal muscle weight, and R is remaining weight. Using measuring devices that would be considered crude by modern standards, Matiegka developed his model based on height, bone and extremity breadths, skinfolds, and calculated body surface area.
Sarcopenia, sarcopenic obesity, and cachexia are all circumscribed by adverse outcomes captured by Matiegka’s vision of a connection between musculoskeletal mass and function as it relates to human “working efficiency.” Another seven decades were needed before anthropometric measurements and models as pioneered by Matiegka could be directly linked to actual measurements of whole-body skeletal muscle mass, either by dissection [16] or with in vivo CT and MRI measurements [17].
Matiegka’s anthropometric method provides an opportunity to ask the question, what exactly do we mean by skeletal muscle mass? The five-level model reported by Wang and colleagues at Columbia University in 1992 [2] provides a framework for responding to this question. Wang’s model describes the human body as five interconnected areas starting with an elemental level followed by molecular, cellular, tissue-organ, and whole-body levels. With body surface measurements, anthropometry provides a skeletal muscle mass estimate at the tissue-organ level that includes skeletal muscle fibers, nerves, blood vessels, progenitor cells, connective tissue, tendons, intermuscular adipose tissue, and even in some cases bone. By contrast, the creatine-creatinine method largely maps the creatine pool located within skeletal muscle cells [18]. Wang’s model provides an important framework for linking the mechanistic basis of a method with specific measured skeletal muscle structures. Each method provides a skeletal muscle mass estimate that can be categorized and modeled as one of Wang’s five levels. Wang’s model also provides a context for discussing the emerging topic of muscle “quality” that can be framed as ranging from whole-muscle to cells, intracellular organelles, and individual molecular substrates.
2.3 Piecing elements together
The opening of the nuclear age following World War II led to the introduction of new body composition techniques such as whole-body 40K counting and prompt-γ neutron activation analysis for measuring total body potassium (TBK) and total body nitrogen (TBN), respectively [19]. Burkinshaw et al. at the University of Leeds [20] and Cohn et al. at Brookhaven National Laboratory [21] introduced the historically important TBK-TBN elemental method of estimating total body skeletal muscle mass between 1978 and 1980. The Burkinshaw-Cohn model assumes that the K to N ratios of skeletal muscle and nonskeletal muscle lean mass are constant at 3.03 and 1.33 mmol/g, respectively. Skeletal muscle mass (in kilograms) can then be calculated as = [TBK (in millimoles) − 1.33 × TBN (in grams)]/51.0. This innovate method was applied to early studies of cancer cachexia by Cohn et al. [21, 22] and Burkinshaw [23]. The lack of other suitable skeletal muscle mass reference methods at the time led Lukaski et al. at the United States Department of Agriculture in Grand Forks [24] to provide the first validation of the urinary 3-methylhistidine method for estimating skeletal muscle mass against skeletal muscle mass values derived from Burkinshaw-Cohn’s method in 1981. The 3-methylhistidine method for measuring skeletal muscle mass is not in use today, being replaced by contemporary advanced and more practical methods such as CT and MRI.
An early conceptual precursor to the models derived by Burkinshaw and Cohn was reported by Chinn in 1967 who was working at the United States Army Research and Nutrition Laboratory in Denver [25]. Chinn developed a mathematical model for estimating skeletal and nonskeletal muscle protein from measured TBK and 24-h urinary creatinine.
While imaginative in their design, this group of methods is of little practical value today due to the complexity of instrumentation required, the potential for radiation exposure, and the need to collect serial burdensome 24-h urine samples. What these methods do reveal are the lengths to which investigators went in trying to quantify the remarkably large but elusive skeletal muscle compartment in vivo. These efforts were motivated by the need to quantify skeletal muscle mass, not only body fat, the two main tissue targets of wasting diseases such as cancer.
3 Modern era
3.1 Growth of biomedical imaging
X-rays
Few would have predicted that Röentgens’ discovery of X-rays in 1895 at the University of Würzburg [26] would ultimately be the basis of a whole family of biomedical imaging methods that today serve as the main tool for quantifying skeletal muscle mass and composition. More than half a century later, Harold C. Stuart and his colleagues at Harvard first applied an X-ray method for estimating extremity fat and muscle “widths” in growing children [27]. While Stuart’s method gained acceptance among the research community at the time, it was to be three more decades before major advances transformed the field. Within a very short time span in the early 1970s, all three of our main contemporary clinical and reference methods, CT, MRI, and dual-energy X-ray absorptiometry (DXA), came into existence.
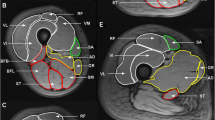
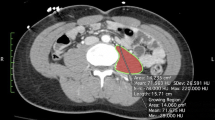
The first of these approaches to gain acceptance in clinical medicine was CT, initially applied in 1971 to a clinical patient by Godfrey Hounsfield working at EMI near London [28]. Hounsfield’s approach was formulated on theoretical underpinnings provided earlier by Allan M. Cormack at the University of Cape Town and later at Tufts University [29]. Unlike Stuart’s two-dimensional plain X-rays [27], CT provided high-contrast cross-sectional images with pixel attenuation related to tissue physical density [30]. Pixels, or picture elements, could now be easily separated into those traversing adipose tissue (density, ∼0.92 g/cm3) and those passing through whole skeletal muscle tissue (∼1.04 g/cm3). By 1975, Hounsfield and his colleagues built a whole-body CT scanner, and within a few months of each other, three papers appeared in 1978–1979 that used this revolutionary imaging approach for quantifying regional skeletal muscle areas [31–33]. Several years later, Tokunaga et al. at Osaka University in 1983 [34] and Sjöström et al. at the University of Gothenburg in 1984 [35] reported the first evaluations of total body composition by CT using a multi-slice head-toe approach. The emphasis in these early studies was on the evaluation of regional and total body adipose tissue.
Each CT pixel or volume element (voxel) represents tissue attenuation and is defined in Hounsfield units (HU). A value of 0 HU represents water, −1,000 HU represents air, with negative and positive values characteristic of fat and lean tissues, respectively. An early observation following the introduction of CT was the impact of conditions such as hepatic steatosis and hemosiderosis to quantitatively influence the measured CT numbers [36]. Investigators today continue to use and expand on the use of CT numbers to provide qualitative and functional information on skeletal muscle tissue beyond measures of size and shape [37].
Magnetic resonance
Isidor Rabi, working at Columbia University in 1938, led pioneering investigations into the magnetic resonance properties of atomic nuclei [38].
Rabi’s research was advanced independently in 1946 by Felix Bloch at Stanford [39] and Edward Purcell at Harvard [40] with their discovery of nuclear magnetic resonance (NMR). The Bloch-Purcell research provided basic information about a molecule’s chemical and structural properties in liquids and solids. Paul Lauterbur, working at the State University of New York (SUNY) at Stony Brook, wrote a classic paper in 1973 on an imaging approach he referred to as zeugmatography that took unidimensional NMR spectroscopy to a second dimension of spatial orientation [41]. Peter Mansfield, at the University of Nottingham, showed during the early 1970s that a useful imaging technique could be created by advancing magnetic field gradients with appropriate mathematical analysis [42]. Raymond Damadian, working at SUNY Downstate, completed construction of the first whole-body MRI scanner in 1977 [43] and equipment for hospitals became available during the early 1980s. Foster and colleagues, working with an early prototype scanner at the University of Aberdeen, reported sequences in 1984 that discriminated well between adipose and skeletal muscle tissues [44]. Cadaver and regional human validation studies followed and by 1991, Robert Ross and colleagues at Queens University in Kingston showed good agreement between whole-body adipose tissue estimates by multi-slice MRI and CT in the rat [45]. Ross et al. in the mid-1990s advanced their MRI studies to humans, quantifying both whole-body adipose tissue and skeletal muscle mass [46, 47]. Selberg et al. reported whole-body anatomical skeletal muscle mass estimates by nuclear magnetic resonance in 1993 [48].
Two Swiss scientists, Kurt Wüthrich and Richard Ernst, contributed further to the field with their pioneering NMR studies [49, 50] that contribute to in vivo chemical analysis of skeletal muscle and other tissues. Magnetic resonance spectroscopy is widely used today as a means of assessing skeletal muscle quality, particularly with the examination of such components as intramyocellar lipid.
The profound contribution to medical science by the development of imaging methods, notably CT and MRI, have led to ten Nobel Prizes as follows: Röentgen (1901), Rabi (1944), Bloch and Purcell (1952), Hounsfield and Cormack (1979), Ernst (1991), Lauterbur and Mansfield (2003), and Wüthrich (2002).
Differential absorptiometry
While CT and MRI are not widely available or affordable whole-body methods for conducting sarcopenia and cachexia trials, DXA has now largely met that unmet need by providing surrogate estimates of regional and whole-body skeletal muscle mass at relatively low cost and with minimal radiation exposure. Systems are available throughout the world and are well-calibrated for monitoring patients over time or for conducting between-center research.
Often linked with sarcopenia and frailty, osteoporosis with pathological fractures is an important medical condition requiring clinical evaluation and treatment monitoring. Bone quality was typically evaluated with plain X-rays until the introduction of single-photon absorptiometry (SPA) by Cameron and Sorenson at the University of Wisconsin in 1963 [51]. Bone mineral density was typically evaluated with SPA at sites such as the wrist that consist mainly of skeleton with a photon source such as 125I. In addition to bone, skin, overlying adipose tissue, and skeletal muscle also lead to photon attenuation, and thus axial skeletal sites such as the spine and hip could not be reliably evaluated for osteoporosis with SPA. This problem was solved in 1970 by Mazess et al. at the University of Wisconsin [52] who proposed a dual-photon method of separating soft tissue from bone using isotope sources such as 241Am or 153Gd. The novel approach included partitioning soft tissue into lean and fat components using the differential photon characteristics of traversed tissue elements such as carbon, hydrogen, oxygen, and electrolytes [53]. The first whole-body dual-photon absorptiometry systems appeared at medical facilities in the early 1980s and were later replaced in 1987 with DXA systems. The low radiation exposure, widespread availability, and relatively low per patient scan cost provided a new practical opportunity for investigators to quantify body composition in children and adults.
An important feature of DPA and DXA is an ability to isolate body regions during the analysis procedure and thus investigators for the first time could evaluate fat, lean soft tissue, and bone mineral separately for the extremities, trunk, and other selected body regions. Heymsfield and colleagues at Columbia University reported a method of estimating appendicular skeletal muscle mass from DPA in 1990 [54], and two years later, Fuller et al. at Cambridge [55] reported a similar approach using DXA. The DPA and DXA approaches relied on the observation that a large proportion of measured appendicular lean soft tissue is skeletal muscle. Additionally, a large percentage (∼50 %) of total body skeletal muscle mass is in the extremities. These developments opened an important new window to the study of conditions such as frailty and sarcopenia. The coevolution of MRI provided an opportunity to relate measured appendicular lean soft tissue to total body skeletal muscle mass as first reported by Kim et al. at Columbia University in 2002 [56].
The parallel development tracks and major milestones for development of X-ray-based and magnetic resonance-based imaging methods are presented in Figs. 1 and 2, respectively.
Brief chronology of X-ray research highlights on the path to developing methods of measuring human skeletal muscle mass in vivo. Nobel Prize awardees are noted in italics. ASM appendicular skeletal muscle, CT computed tomography, DPA dual-photon absorptiometry, DXA dual-energy X-ray absorptiometry, MRI magnetic resonance imaging, SM skeletal muscle, SPA single photon absorptiometry
Defining muscle structural relations with emerging imaging methods
The new flow of information on human skeletal muscle mass stimulated ideas on how to integrate whole body and regional measurements into existing body composition paradigms. It was Quetelet at the Brussels Observatory in 1835 who is credited with the concept that body weight scales in humans as height2 [57]. This observation gave rise to body mass index (weight/height2), a measure of body shape and adiposity that is independent of height. Theodore VanItallie, working at Columbia University, extended Quetelet’s concept in 1990 by suggesting that body composition also be expressed as height-normalized indices [58]. Seeking a means of “diagnosing” sarcopenia as part of an epidemiology study, Baumgartner et al. at the University of New Mexico [59] developed the appendicular skeletal muscle mass index (appendicular lean mass/height2) in 1998 based on DXA extremity lean soft tissue estimates. Heymsfield et al. at Columbia University confirmed in 2007 [60] and later in 2011 [61] that total body skeletal muscle mass as measured by MRI and appendicular lean soft tissue as measured by DXA scale similar to height as does body weight, approximately as height2.
A related concept was advanced by Webster et al. at the Harrow MRC Clinical Research Center in 1983 who showed that fat mass adjusted for height2, and by inference fat-free mass index, is highly correlated with body mass index [62]. This observation led Webster and his colleagues to propose a stable composition of “excess weight” as about one fourth fat-free mass. In other words, as a person’s adiposity increases so does their lean mass, including skeletal muscle. Forbes, working at the University of Rochester, advanced this concept by introducing the “companionship” rule describing a curvilinear relationship between fat-free mass and total body fat. Forbes and others since have confirmed the longitudinal validity of “Forbes’ Rule” by showing relatively large gains or loss of fat-free mass with changes in energy balance at low levels of subject adiposity [63]. Since a large fraction of fat-free mass is skeletal muscle, we can infer that with alterations in energy and protein balance, relatively large changes in skeletal muscle will occur in sarcopenic or cachectic patients who may have low baseline levels of adiposity.
Bioimpedance analysis
Nyboer (1959, Wayne State University, Detroit [64]), Thomasset (1962, University Claude Bernard, Lyonn [65]), and Hoffer (1969, University of Alabama, Birmingham [66]) all made substantial contributions to bioimpedance analysis concepts and technology in the late 1950s and 1960s. The path to current applications for measuring skeletal muscle mass with bioimpedance technology was paved largely by the seminal contribution of Leslie Organ’s group at the Medical University of South Carolina in 1994 [67]. Organ introduced a practical six-electrode technique for segmental bioimpedance analysis that provided separate resistance and reactance measurements for each extremity and the trunk using only peripheral electrode sites. This approach has evolved to the widely used eight contact-electrode method now in use today. As with DPA and DXA, Organ’s method allows for separate measurements of the extremities and trunk. A few years later, Tan et al. at Columbia University in 1997 reported the first contact electrode system based on Organ’s concept devoted specifically to measuring appendicular impedance that was then used to develop prediction equations for total body skeletal muscle mass [68]. Methods such as multifrequency bioimpedance spectroscopy and derived measures such as phase angle [69] are increasingly being used to go beyond estimation of skeletal muscle mass to evaluation of muscle quality.
Ultrasound
Karl Dussik, a neurologist at the University of Vienna, first used ultrasound technology in 1942 for diagnosing brain tumors [70]. Several years later, George Ludwig, at the United States Naval Research Institute, described the use of ultrasound to diagnose gallstones [71]. Ultrasound technology has since evolved to include many different technologies and is in widespread clinical use. The value of ultrasound in the clinical setting comes in part from portability and lack of ionizing radiation exposure as with many other clinical methods. Bullen et al. at Copenhagen’s Bispebjerg Hospital [72] and Booth et al. at Birmingham’s Dudley Road Hospital [73] used A-mode ultrasound in the early 1960s as an alternative to skinfold calipers in measuring subcutaneous fat layer thickness. Ikai and Fukunaga, at the University of Tokyo, reported the use of ultrasound for measuring skeletal muscle cross-sectional areas in 1968 [74]. Ultrasound is gaining increasing acceptance today as a clinical and research tool for evaluating skeletal muscle mass at baseline and over time with various interventions. Technologies such as ultrasound elastography provide additional information about skeletal muscle quality [75], beyond that of simply muscle shape or size.
4 Recent advances and future potential
A remarkable range of technologies is now available for quantifying regional and total body skeletal muscle mass in almost any setting and at any age, even in utero. An important observation undergoing intense discussion in the sarcopenia field is the observation that skeletal muscle mass and function decline at different rates during the aging process [76, 77]. What are the mechanisms of these effects? Should “functional” measures replace or complement “structural” measures as diagnostic components of conditions associated with skeletal muscle changes over time? Important focuses in this debate are the linkages between skeletal muscle structure, composition, and function. At the center of this chain, and one that holds future promise, is the assessment of skeletal muscle composition.
Separating adipose and muscle tissues
Matiegka’s anthropometric skeletal muscle compartment would by necessity include some adipose tissue interspersed between muscle fibers and compartments [15]. This marbling effect of intramuscular adipose tissue (IMAT) has been recognized in the animal science literature for decades, and ultrasound is the traditional measurement method of choice. The IMAT compartment, weighing several kilograms in adults [78] and a feature of sarcopenia, can now be accurately quantified my CT, MRI, or ultrasound. Anatomic skeletal muscle can be separated into two parts, IMAT and IMAT-free skeletal muscle.
Another MRI approach is to separate skeletal muscle tissue into two molecular level components, fat and fat-free muscle. A range of methods has been developed to accomplish this end that collectively is referred to as fat-suppression techniques [79]. These approaches all rely on the observation that hydrogen nuclei in the chemical environments of water and fat have different MRI relevant parameters, primarily relaxation time, and resonance frequency or so-called chemical shift. These differences can be exploited to suppress the fat-bound proton signal, and two main groups of techniques are available, relaxation-dependent (e.g., short inversion-time inversion recovery) and chemical shift-dependent (e.g., Dixon-based fat suppression) [80]. Scanning protocols now in development will soon provide estimates of regional and total body fat-free skeletal muscle volume. Possibilities exist to either fully or partially automate the analysis protocol, thus removing a major current task of expert hand image segmentation as is required for quantitative CT and MRI muscle analysis.
Separating muscle extracellular and intracellular compartments
With aging and development of sarcopenia or with cachexia-induced skeletal muscle atrophy, there is a relative expansion of the extracellular space that includes fluid and connective tissue with loss of muscle fibers [81, 82]. Several new magnetic resonance techniques hold promise for providing information related to the extracellular compartment [83].
The first of these methods is referred to as T1 mapping equilibrium contrast magnetic resonance that gives estimates of myocardial and potentially skeletal muscle extracellular volume fraction [84]. The protocol requires the use of an imaging contrast agent and so far has shown promise in detecting pathological changes in human myocardial tissue, representing a relative increase in extracellular volume and fibrosis [85]. Noncontrast T1-mapping also provides measures of cardiac fibrosis [86].
A second developing approach, magnetic resonance elastography [87, 88], provides information on skeletal muscle viscoelastic and mechanical properties that may represent increased connective tissue with functional consequences. The method has been used to measure skeletal muscle stiffness, a property that can change significantly depending upon the contractile state of the muscle [89, 90]. Skeletal muscle magnetic resonance elastography can also be used for studying the physiological response of diseased and damaged muscles [91].
Bone and connective tissue are not usually visualized on conventional MRI scans, and a third new method for evaluating the extracellular compartment involves the use of a two-dimensional ultra-short echo time (2D UTE) sequence with an inversion pulse for long T(2) water and fat signal suppression [92, 93]. This important new method allows visualization of cortical bone and connective tissue structures within skeletal muscle.
Evaluating muscle fibers
Magnetic resonance spectroscopy techniques are available for quantifying muscle fiber intracellular lipid, high-energy intermediates such as creatine-phosphate, glycogen, and other substrates [94–96].
A rapidly evolving promising nonspectroscopic approach to studying muscle microstructure and architectural organization cell was first introduced by Denis Le Bihan and his colleagues at the University of Paris in 1985 [97]. Le Bihan’s method, now referred to as diffusion MRI, is based on the diffusion properties of water in nerve fibers exposed to a strong magnetic field gradient. Le Bihan was able to exploit non-random water axonal movement to recreate in vivo brain tractography images. Elongated muscle fibers that also display anisotropic water diffusion similar to that observed in nerve fibers can now be studied with diffusion tensor imaging (DTI). In addition to images, DTI provides quantitative measures including three eigenvalues, fractional anisotropy, and apparent diffusion coefficient [98]. Recent studies suggest that these DTI-measured properties of skeletal muscle can be used to estimate physiologic cross-sectional area, pennation angle, fiber length, and proportion of muscle as type-I fibers [98, 99].
An imaging technique referred to as chemical exchange saturation transfer (CEST) magnetic resonance can now be used to create spatial and temporal images of free skeletal muscle creatine [100, 101]. Intracellular creatine exhibits a concentration-dependent CEST effect between its amine (-NH2) protons and bulk water protons (CrCEST). This promising method can be used to study muscle energetics with exercise [100] and potentially other interventions.
Our brief review of these multiple new techniques conveys the important impression that our field is rapidly moving from simply measuring “anatomy” or “structure” to a new level that allows dissection of muscle tissue into components that can help us understand corresponding “functional” dimensions.
5 Conclusions
Almost two centuries have passed since Chevreul observed that meat is a primary source of creatine [3], a pivotal discovery from which has emerged many new methods for measuring human skeletal muscle mass and composition. These advances are timely, as they will provide the tools needed to study the muscle disturbances of our ever-growing aging population with the emergence of noncommunicable diseases as the primary cause of disability and death.
References
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. 2010;91:1123S–7S. doi:10.3945/ajcn.2010.28608A.
Wang ZM, Pierson Jr RN, Heymsfield SB. The five-level model: a new approach to organizing body-composition research. Am J Clin Nutr. 1992;56:19–28.
Chevreul E. Sur la composition chimique du bouillon de viandes (On the chemical composition of meatbroth). J Pharm Sci Access. 1835;21:231–42.
Folin O. Laws governing the chemical composition of urine. Am J Insanity. 1904;60:709–10.
Bürger M. Beiträge zum Kreatininstoffwechsel. Z f d g Exp Med. 1919;9:361–99. doi:10.1007/bf03002912.
Hahn A, Meyer G. On the mutual transformation of creatine and creatinine. Z Biol. 1928;78:111–5.
Talbot NB, Broughton F. Measurement of obesity by the creatinine coefficient. Am J Dis Child. 1938;55:42–50. doi:10.1001/archpedi.1938.01980070051004.
Graystone J. Creatinine excretion during growth, in human growth. Philadelphia: Lea & Febiger; 1968.
Graystone JE, Cheek DB. The effects of reduced caloric intake and increased insulin-induced caloric intake on the cell growth of muscle, liver, and cerebrum and on skeletal collagen in the postweanling rat. Pediatr Res. 1969;3:66–76.
Kreisberg R, Bowdoin B, Meador CK. Measurement of muscle mass in humans by isotopic dilution of creatine-14C. J Appl Physiol. 1970;28:264–7.
Picou D, Reeds PJ, Jackson A, Poulter N. The measurement of muscle mass in children using [15N] creatine. Pediatr Res. 1976;10:184–8. doi:10.1203/00006450-197603000-00008.
Wang ZM, Sun YG, Heymsfield SB. Urinary creatinine-skeletal muscle mass method: a prediction equation based on computerized axial tomography. Biomed Environ Sci. 1996;9:185–90.
Stimpson SA, Turner SM, Clifton LG, Poole JC, Mohammed HA, Shearer TW, et al. Total-body creatine pool size and skeletal muscle mass determination by creatine-(methyl-D3) dilution in rats. J Appl Physiol. 1985;112:1940–8. doi:10.1152/japplphysiol.00122.2012. 2012.
Brozek J, Prokopec M. Historical note: early history of the anthropometry of body composition. Am J Hum Biol. 2001;13:157–8. doi:10.1002/1520-6300(200102/03)13:2<157::AID-AJHB1023>3.0.CO;2-L.
Matiegka J. The testing of physical efficiency. Am J Phys Anthropol. 1921;4:223–30. doi:10.1002/ajpa.1330040302.
Clarys JP, Martin AD, Drinkwater DT. Gross tissue weights in the human body by cadaver dissection. Hum Biol. 1984;56:459–73.
Lee RC, Wang Z, Heo M, Ross R, Janssen I, Heymsfield SB. Total-body skeletal muscle mass: development and cross-validation of anthropometric prediction models. Am J Clin Nutr. 2000;72:796–803.
Heymsfield SB, Arteaga C, McManus C, Smith J, Moffitt S. Measurement of muscle mass in humans: validity of the 24-h urinary creatinine method. Am J Clin Nutr. 1983;37:478–94.
Heymsfield SB, Wang Z, Baumgartner RN, Ross R. Human body composition: advances in models and methods. Annu Rev Nutr. 1997;17:527–58. doi:10.1146/annurev.nutr.17.1.527.
Burkinshaw L, Hill GL, Morgan DB. Assessment of the distribution of protein in the human body by in vivo neutron activation analysis. In International Symposium on Nuclear Activation Techniques in the Life Sciences. IAEA: Vienna; 1978. p. 787-796.
Cohn SH, Vartsky D, Yasumura S, Sawitsky A, Zanzi I, Vaswani A, et al. Compartmental body composition based on total-body nitrogen, potassium, and calcium. Am J Physiol. 1980;239:E524–30.
Cohn SH, Gartenhaus W, Sawitsky A, Rai K, Zanzi I, Vaswani A, et al. Compartmental body composition of cancer patients by measurement of total body nitrogen, potassium, and water. Metabolism. 1981;30:222–9.
Burkinshaw L. Some aspects of body composition in cancer. Infusionstherapie. 1990;17 Suppl 3:57–8.
Lukaski HC, Mendez J, Buskirk ER, Cohn SH. Relationship between endogenous 3-methylhistidine excretion and body composition. Am J Physiol. 1981;240:E302–7.
Chinn KS. Prediction of muscle and remaining tissue protein in man. J Appl Physiol. 1967;23:713–5.
Nitske WR. The life of Wilhelm Conrad Röntgen, discoverer of the X-ray. Tucson: University of Arizona Press; 1971.
Stuart HCDP. The growth of bone, muscle, and overlying tissues in children 6 to 10 years of age as revealed by studies of roentgenograms of the leg area. Monogr Soc Res Child Dev. 1942;13:195.
Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol. 1973;46:1016–22.
Cormack AM. Nobel award address. Early two-dimensional reconstruction and recent topics stemming from it. Med Phys. 1980;7:277–82.
Heymsfield SB, Noel R, Lynn M, Kutner M. Accuracy of the soft tissue density predicted by CT. J Comput Assist Tomogr. 1979;8:859.
Bulcke JA, Termote JL, Palmers Y, Crolla D. Computed tomography of the human skeletal muscular system. Neuroradiology. 1979;17:127–36.
Haggmark T, Jansson E, Svane B. Cross-sectional area of the thigh muscle in man measured by computed tomography. Scand J Clin Lab Invest. 1978;38:355–60.
Heymsfield SB, Olafson RP, Kutner MH, Nixon DW. A radiographic method of quantifying protein-calorie undernutrition. Am J Clin Nutr. 1979;32:693–702.
Tokunaga K, Matsuzawa Y, Ishikawa K, Tarui S. A novel technique for the determination of body fat by computed tomography. Int J Obes. 1983;7:437–45.
Sjöström S. Chefer och människor. 1. uppl. ed. Solna: SIPU; 1984.
Heymsfield SB, Noel R. Radiographic analysis of body composition by computerized axial tomography. Nutr Cancer. 1981;17:161–72.
Goodpaster BH, Thaete FL, Simoneau JA, Kelley DE. Subcutaneous abdominal fat and thigh muscle composition predict insulin sensitivity independently of visceral fat. Diabetes. 1997;46:1579–85.
Rabi II, Millman S, Kusch P, Zacharias JR. The molecular beam resonance method for measuring nuclear magnetic moments. The magnetic moments of Li63, Li73, and F199. Phys Rev. 1939;55:526–35.
Bloch F. The principle of nuclear induction. Science. 1953;118:425–30. doi:10.1126/science.118.3068.425.
Purcell. Research in nuclear magnetism in Nobel lectures, physics: 1942–1962. Amsterdam: Elsevier; 1962. p. 232.
Lauterbur. Image formation by induced local interactions: examples employing nuclear magnetic resonance. Nature. 1973;242:190–1.
Garroway A. Solid state NMR, MRI, and Sir Peter Mansfield: (1) from broad lines to narrow and back again; and (2) a highly tenuous link to landmine detection. MAGMA. 1999;9:103–8. doi:10.1007/bf02594604.
Damadian R. Tumor detection by nuclear magnetic resonance. Science. 1971;171:1151–3.
Foster MA, Hutchison JM, Mallard JR, Fuller M. Nuclear magnetic resonance pulse sequence and discrimination of high- and low-fat tissues. Magn Reson Imaging. 1984;2:187–92.
Ross R, Leger L, Guardo R, De Guise J, Pike BG. Adipose tissue volume measured by magnetic resonance imaging and computerized tomography in rats. J Appl Physiol. 1985;70:2164–72. 1991.
Ross R, Rissanen J, Pedwell H, Clifford J, Shragge P. Influence of diet and exercise on skeletal muscle and visceral adipose tissue in men. J Appl Physiol. 1985;81:2445–55. 1996.
Ross R, Pedwell H, Rissanen J. Effects of energy restriction and exercise on skeletal muscle and adipose tissue in women as measured by magnetic resonance imaging. Am J Clin Nutr. 1995;61:1179–85.
Selberg O, Burchert W, Graubner G, Wenner C, Ehrenheim C, Muller MJ. Determination of anatomical skeletal muscle mass by whole body nuclear magnetic resonance. Basic Life Sci. 1993;60:95–7.
Wüthrich K, Wider G, Wagner G, Braun W. Sequential resonance assignments as a basis for determination of spatial protein structures by high resolution proton nuclear magnetic resonance. J Mol Biol. 1982;155:311–319.
Kumar A, Ernst R, Wuthrich K. A two-dimensional nuclear overhauser enhancement (2D NOE) experiment for the elucidation of complete proton-proton cross-relaxation networks in biological macromolecules. Biochem Biophys Res Commun. 1980;95:1–6. doi:10.1016/0006-291x(80)90695-6.
Cameron JR, Sorenson J. Measurement of bone mineral in vivo: an improved method. Science. 1963;142:230–2.
Mazess RB, Cameron JR, Sorenson JA. Determining body composition by radiation absorption spectrometry. Nature. 1970;228:771–2.
Pietrobelli A, Formica C, Wang Z, Heymsfield SB. Dual-energy X-ray absorptiometry body composition model: review of physical concepts. Am J Physiol. 1996;271:E941–51.
Heymsfield SB. Anthropometric measurements: application in hospitalized patients. Infusionstherapie. 1990;17 Suppl 3:48–51.
Fuller NJ, Laskey MA, Elia M. Assessment of the composition of major body regions by dual-energy X-ray absorptiometry (DEXA), with special reference to limb muscle mass. Clin Physiol. 1992;12:253–66.
Kim J, Wang Z, Heymsfield SB, Baumgartner RN, Gallagher D. Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr. 2002;76:378–83.
Quetelet A. Sur l’homme et le développement de ses facultés, essai d’une physique sociale. Paris: Bachelie;1835.
VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr. 1990;52:953–9.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Heymsfield SB, Gallagher D, Mayer L, Beetsch J, Pietrobelli A. Scaling of human body composition to stature: new insights into body mass index. Am J Clin Nutr. 2007;86:82–91.
Heymsfield SB, Heo M, Thomas D, Pietrobelli A. Scaling of body composition to height: relevance to height-normalized indexes. Am J Clin Nutr. 2011;93:736–40. doi:10.3945/ajcn.110.007161.
Webster JD, Hesp R, Garrow JS. The composition of excess weight in obese women estimated by body density, total body water, and total body potassium. Hum Nutr Clin Nutr. 1984;38:299–306.
Forbes GB. Human body composition: growth, aging, nutrition, and activity. New York: Springer-Verlag; 1987. p. 28–49.
Nyboer J. Workable volume and flow concepts of bio-segments by electrical impedance plethysmography. TIT J Life Sci. 1972;2:1–13.
Thomasset A. Bioelectrical properties of tissue impedance measurements. Lyon Med. 1962;208:107–18.
Hoffer EC, Meador CK, Simpson DC. Correlation of whole-body impedance with total body water volume. J Appl Physiol. 1969;27:531–4.
Organ LW, Bradham GB, Gore DT, Lozier SL. Segmental bioelectrical impedance analysis: theory and application of a new technique. J Appl Physiol. 1985;77:98–112. 1994.
Tan YX, Nunez C, Sun Y, Zhang K, Wang Z, Heymsfield SB. New electrode system for rapid whole-body and segmental bioimpedance assessment. Med Sci Sports Exerc. 1997;29:1269–73.
Paiva SI, Borges LR, Halpern-Silveira D, Assuncao MC, Barros AJ, Gonzalez MC. Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Support Care Cancer. 2010;19:187–92. doi:10.1007/s00520-009-0798-9.
Dussik KT. The ultrasonic field as a medical tool. Am J Phys Med. 1954;33:5–20.
Ludwig GD, Bolt RH, Heuter TF, Ballantine Jr HT. Factors influencing the use of ultrasound as a diagnostic aid. Trans Am Neurol Assoc. 1950;51:225–8.
Bullen BA, Quaade F, Olessen E, Lund SA. Ultrasonic reflections used for measuring subcutaneous fat in humans. Hum Biol. 1965;37:375–84.
Booth RA, Goddard BA, Paton A. Measurement of fat thickness in man: a comparison of ultrasound, Harpenden calipers and electrical conductivity. Br J Nutr. 1966;20:719–25.
Ikai M, Fukunaga T. Calculation of muscle strength per unit cross-sectional area of human muscle by means of ultrasonic measurement. Int Z Angew Physiol. 1968;26:26–32.
Sarvazyan AP, Urban MW, Greenleaf JF. Acoustic waves in medical imaging and diagnostics. Ultrasound Med Biol. 2013;39:1133–46. doi:10.1016/j.ultrasmedbio.2013.02.006.
Heymsfield SB, Stevens V, Noel R, McManus C, Smith J, Nixon D. Biochemical composition of muscle in normal and semistarved human subjects: relevance to anthropometric measurements. Am J Clin Nutr. 1982;36:131–42.
Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012;246:623–7. doi:10.1097/BOR.0b013e328358d59b.
Gallagher D, Kuznia P, Heshka S, Albu J, Heymsfield SB, Goodpaster B, et al. Adipose tissue in muscle: a novel depot similar in size to visceral adipose tissue. Am J Clin Nutr. 2005;81:903–10.
Bley TA, Wieben O, Francois CJ, Brittain JH, Reeder SB. Fat and water magnetic resonance imaging. J Magn Reson Imaging. 2010;31:4–18. doi:10.1002/jmri.21895.
Dixon WT. Simple proton spectroscopic imaging. Radiology. 1984;153:189–94. doi:10.1148/radiology.153.1.6089263.
Sions JM, Tyrell CM, Knarr BA, Jancosko A, Binder-Macleod SA. Age- and stroke-related skeletal muscle changes: a review for the geriatric clinician. J Geriatr Phys Ther. 2012;35:155–61. doi:10.1519/JPT.0b013e318236db92.
Yamada Y, Schoeller DA, Nakamura E, Morimoto T, Kimura M, Oda S. Extracellular water may mask actual muscle atrophy during aging. J Gerontol A Biol Sci Med Sci. 2010;65:510–6. doi:10.1093/gerona/glq001.
Young IR, Bydder GM. Magnetic resonance: new approaches to imaging of the musculoskeletal system. Physiol Meas. 2003;24:R1–R23.
Fontana M, White SK, Banypersad SM, Sado DM, Maestrini V, Flett AS, et al. Comparison of T1 mapping techniques for ECV quantification. Histological validation and reproducibility of ShMOLLI versus multibreath-hold T1 quantification equilibrium contrast CMR. J Cardiovasc Magn Reson. 2012;14:88. doi:10.1186/1532-429X-14-88.
Miller CA, Naish JH, Bishop P, Coutts G, Clark D, Zhao S, et al. Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ Cardiovasc Imaging. 2013;6:373–83. doi:10.1161/CIRCIMAGING.112.000192.
Bull S, White SK, Piechnik SK, Flett AS, Ferreira VM, Loudon M, et al. Human non-contrast T1 values and correlation with histology in diffuse fibrosis. Heart. 2013;99:932–7. doi:10.1136/heartjnl-2012-303052.
Mariappan YK, Glaser KJ, Ehman RL. Magnetic resonance elastography: a review. Clin Anat. 2010;23:497–511. doi:10.1002/ca.21006.
Glaser KJ, Manduca A, Ehman RL. Review of MR elastography applications and recent developments. J Magn Reson Imaging. 2012;36:757–74. doi:10.1002/jmri.23597.
Dresner MA, Rose GH, Rossman PJ, Muthupillai R, Manduca A, Ehman RL. Magnetic resonance elastography of skeletal muscle. J Magn Reson Imaging. 2001;13:269–76.
Ringleb SI, Bensamoun SF, Chen Q, Manduca A, An KN, Ehman RL. Applications of magnetic resonance elastography to healthy and pathologic skeletal muscle. J Magn Reson Imaging. 2007;25:301–9. doi:10.1002/jmri.20817.
Basford JR, Jenkyn TR, An KN, Ehman RL, Heers G, Kaufman KR. Evaluation of healthy and diseased muscle with magnetic resonance elastography. Arch Phys Med Rehabil. 2002;83:1530–6.
Du J, Carl M, Bydder M, Takahashi A, Chung CB, Bydder GM. Qualitative and quantitative ultrashort echo time (UTE) imaging of cortical bone. J Magn Reson. 2010;207:304–11. doi:10.1016/j.jmr.2010.09.013.
Du J, Hamilton G, Takahashi A, Bydder M, Chung CB. Ultrashort echo time spectroscopic imaging (UTESI) of cortical bone. Magn Reson Med. 2007;58:1001–9. doi:10.1002/mrm.21397.
Barker AR, Armstrong N. Insights into developmental muscle metabolism through the use of 31P-magnetic resonance spectroscopy: a review. Pediatr Exerc Sci. 2010;22:350–68.
Lanza IR, Nair KS. Mitochondrial metabolic function assessed in vivo and in vitro. Curr Opin Clin Nutr Metab Care. 2010;13:511–7. doi:10.1097/MCO.0b013e32833cc93d.
Chang G, Wang L, Cardenas-Blanco A, Schweitzer ME, Recht MP, Regatte RR. Biochemical and physiological MR imaging of skeletal muscle at 7 T and above. Semin Musculoskelet Radiol. 2010;14:269–78. doi:10.1055/s-0030-1253167.
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M. MR Imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiol. 1986;161:401–407.
Longwei X. Clinical application of diffusion tensor magnetic resonance imaging in skeletal muscle. Muscles Ligaments Tendons J. 2012;2:19–24.
Scheel M, von Roth P, Winkler T, Arampatzis A, Prokscha T, Hamm B, et al. Fiber type characterization in skeletal muscle by diffusion tensor imaging. NMR Biomed. 2013;26:1220–4. doi:10.1002/nbm.2938.
Kogan F, Haris M, Singh A, Cai K, Debrosse C, Nanga RP, et al. Method for high-resolution imaging of creatine in vivo using chemical exchange saturation transfer. Magn Reson Med. 2014;71:164–72. doi:10.1002/mrm.24641.
Haris M, Nanga RP, Singh A, Cai K, Kogan F, Hariharan H, et al. Exchange rates of creatine kinase metabolites: feasibility of imaging creatine by chemical exchange saturation transfer MRI. NMR Biomed. 2012;25:1305–9. doi:10.1002/nbm.2792.
Acknowledgement
The authors acknowledge the support of Ms. Robin Post in manuscript preparation.
Ethical statement
All the authors certify that they comply with the ethical guidelines for authorship and publishing of the Journal of Cachexia, Sarcopenia and Muscle (von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. 2010; 1:7–8.)
Conflict of interest
Steven B. Heymsfield, Michael Adamek, M. Cristina Gonzalez, Guang Gia, and Diana M. Thomas declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Heymsfield, S.B., Adamek, M., Gonzalez, M.C. et al. Assessing skeletal muscle mass: historical overview and state of the art. J Cachexia Sarcopenia Muscle 5, 9–18 (2014). https://doi.org/10.1007/s13539-014-0130-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13539-014-0130-5