Abstract
In contrast to the upper boundary of mortality, the lower boundary has so far largely been neglected. Based on the three key features—location, sex-specific difference, and level—I analyze past and present trends in the lower boundary of human mortality. The analysis is based on cohort mortality data for 38 countries, covering all the cohorts born between 1900 and 1993. Minimum mortality is analyzed using observed as well as smoothed estimates. The results show that the ages at which minimum mortality is reached have shifted to lower ages. Although the differences have become almost negligible over time, males are showing higher levels of minimum mortality than females. The level of minimum mortality was halved more than five times over the analyzed time horizon. The results also suggest that even after more than 150 years of mortality improvements, minimum mortality has not yet reached a lowest limit and is likely to decrease further in the near future. Trends in the three key features also raise questions about the importance of evolutionary, social, and biological determinants for the recent and future development of minimum mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Whereas the upper boundary of mortality (maximum mortality) is a topic that has previously attracted the attention of scholars (e.g., Gampe 2010; Rau et al. 2017), the topic of the lower boundary (minimum mortality) has so far largely been neglected. In this study, I aim to analyze past and current trends in the ages and levels of minimum mortality as well as the sex-specific differences in minimum mortality.
The steady decline in mortality is one of the greatest success stories in human history (Oeppen and Vaupel 2002; Riley 2001). Mortality rates across almost all ages have been consistently declining to lower and lower levels for more than 150 years. Although the successive improvements have been unprecedented, the mortality trajectory has retained its key features (see upcoming Fig. 1). For example, levels of infant mortality have been consistently similar to mortality levels between ages 60 and 80. Moreover, adult mortality has shown a log linear increase over age, and mortality levels between infancy and early adulthood have followed a U-shaped pattern.
Age-specific mortality in France, females: Years 1850, 1900, 1950, and 2000. Mortality rates are smoothed. Source: Own illustration using age-specific death counts and exposures-to-risk from the Human Mortality Database (n.d.)
As mortality declined in developed countries, the main improvements in life expectancy shifted from younger to higher ages (Christensen et al. 2009). Currently, the contributions of the youngest ages to the increase of the average age at death are almost negligible. Nevertheless, in almost all countries of the world, mortality at younger ages has been decreasing continuously (Armour-Marshall et al. 2012; Verguet et al. 2014). Consequently, the U-shaped mortality trajectory between infancy and juvenile ages has become more and more pronounced over time (see Fig. 1). Minimum mortality represents the inflection point of this pattern; that is, it marks the lowest mortality level across ages and the threshold between mortality decrease and increase over age.
Together with the maximum level, minimum mortality embraces the range of age-specific mortality. The maximum mortality level has been estimated at a level of approximately 7,000 deaths per 10,000 person-years lived, indicating the magnitude of the late-life mortality plateau (Gampe 2010). Minimum mortality cannot be assessed to a specific level. Minimum mortality declined from approximately 30 deaths per 10,000 person-years lived to a level of less than 1 per 10,000 over the time horizon of 150 years (see Fig. 1). The plasticity of the lower boundary compared with the stability of the upper boundary points to the most important difference between the two. Explanations for the stable upper boundary are diverse and range from a more homogeneous population composition at those ages to physiological and genetic aging processes (Missov and Vaupel 2015; Pletcher and Curtsinger 1998; Vaupel et al. 1998; Wachter 1999). Minimum mortality, by contrast, appears to (still) be alterable. Most importantly, improved living standards (e.g., better sanitation and nutrition) and medical breakthroughs (such as antibiotics and vaccinations) are the main reasons for the survival gains at childhood and juvenile ages (Blum 2009; Cutler et al. 2006; Gore et al. 2011). The major causes of death at those ages have shifted away from infectious diseases and toward behavioral causes (Blum 2009). Today, injuries and noncommunicable diseases are the leading causes of death for people aged 5–14 in low-mortality countries (Patton et al. 2009).
After the degree of alterability, the location is the second major difference between minimum and maximum mortality. Maximum mortality is located at the end of the lifespan, whereas minimum mortality is reached within a tiny age range at the end of the first decade of life. It marks a specific point over the life course at which physical and social development levels are most favorable for withstanding the risk of death. The explanations of why mortality levels are lowest in this exact age range are mainly drawn from evolutionary mechanisms, such as high selection pressure prior to the beginning of the reproductive period: that is, the proximity of these ages to the onset of sexual maturity (Burger et al. 2012; Chu et al. 2008; Levitis 2011). However, for both males and females, scholars have observed temporal changes in related processes, such as faster body growth or the earlier onset of puberty, over the past century (Frisch 1978; Goldstein 2011; Schönbeck et al. 2012; Tanner 1973). The location of minimum mortality might be similarly affected by these shifts.
Male-female differences are the third key feature that could reveal further disparities between maximum and minimum mortality. The question of whether there are sex-specific differences in maximum mortality cannot be answered clearly. Gampe (2010) found no relevant differences between the male and female levels, whereas Rau et al. (2017) documented higher levels for males. Among children and adolescents, mortality is higher for males despite the fact that the absolute gap becomes smaller with decreasing levels of mortality (Gissler et al. 2009). Surprisingly, external causes of death as an indicator for sex-specific risk-adverse behavior explain only a minor part of the male-female differences (Gissler et al. 2009). For example, Gissler et al. (2009) measured a higher rate of nonexternal causes for boys than for girls. It therefore appears that additional factors must be responsible for these differences.
An assessment of minimum mortality could also have implications for the development of methods and models in mortality research. For instance, mortality forecasting approaches usually assume that death rates have no lower limit. Instead, the logarithm of death rates is used, which allows rates to decline infinitely while staying between 0 and 1 (see, e.g., Hyndman and Ullah 2007; Lee and Carter 1992). A proof seems impossible given that the question of whether mortality rates can decline infinitely has yet to be answered. Examining trends in minimum mortality can help us better understand the dynamics at the lower edge of human mortality. Moreover, attempts were made in previous parametric mortality models, such as the Siler model (Siler 1983) or the Heligman-Pollard model (Heligman and Pollard 1980), to include mortality at all ages—and thus the decreasing and increasing parts of age-specific mortality, which are connected by minimum mortality. Mortality modeling could benefit from an investigation of minimum mortality in, for instance, the refinement of existing models or the development of new models.
Based on these considerations, three essential key sets of questions should be asked when seeking to identify the characteristics of the lower boundary of mortality. First, how pronounced are the sex differences in the lower boundary of age-specific mortality? Second, at which ages is minimum mortality located, and how have these ages changed over time? Third, how has the level of minimum mortality evolved, and is minimum mortality still decreasing? Given the unprecedented mortality improvements of the past, it is not far-fetched to hypothesize that minimum mortality might be the first mortality rate that finally hits a lower (natural) limit and that therefore indicates the absolute frontiers of human mortality improvement.
Data
I use a cohort perspective to estimate minimum mortality. Only a cohort follow-up ensures a life course perspective and thus the clear identification of the lowest mortality rate over age. Because the mortality rates of several cohorts are combined in a period perspective, period-based estimates could be distorted by peculiarities across cohorts (such as fluctuating birth cohort sizes) or unexpected external shocks and changes (such as political crises or medical breakthroughs). In addition, many forces shaping minimum mortality, such as selection, work in cohort direction. Hence, a cohort perspective allows one to evaluate and discuss the trends in light of these potential explanations and determinants. This is not readily possible in a period-based comparison. Furthermore, a cohort perspective still covers a sufficient observation time and provides current values because minimum mortality is located at an early stage of life.
I use cohort data from the Human Mortality Database (n.d.). Death counts are given by Lexis triangles. Accordingly, the full death counts for one age are the sum of two consecutive triangles in cohort direction. The two triangles are spread over two periods, and thus the end-year/start-year population between them is used as the exposures to risk (see the online appendix for an illustration). For most countries, the majority of raw data for death counts in the Human Mortality Database are given by Lexis triangles. Especially at the beginning of the twentieth century, this number was growing. For other countries and periods with raw data of a different structure, a regression approach is applied to split the death counts within a Lexis square into counts by a Lexis triangle (for further details, see Wilmoth et al. 2007). All estimates are based on data for ages 1–20. The earliest cohort considered includes those born in 1900. For some countries, the data start later in time. The last cohort available also varies by country. Countries with data covering fewer than 20 cohorts are excluded from the analysis (see the online appendix for further details).
Methods
Although data from the Human Mortality Database cover national populations and can thus be considered complete enumerations, the data are still subject to stochastic variation (Kirkby and Currie 2010; Klotz 2016; Udry et al. 1979). For instance, Udry et al. (1979) demonstrated that the smaller a population, the more unstable the respective mortality rates. In addition, the underlying mortality process is usually assumed to be smooth (see also Kirkby and Currie 2010). Minimum mortality could be considered to be especially vulnerable to population size and stochastic variation because of its low intensity. Hence, near the age of minimum mortality, mortality could be quite noisy. Minimum mortality contains another rather technical and theoretical problem: namely, that mortality rates are bound at 0 at the lower end. In low-mortality countries with a small population, mortality at some ages below 20 is already at such low levels that the number of age intervals without any deaths is consistently increasing over time (see the online appendix for further details). To deal with zero death rates and stochastic variation, I complement the analysis of observed trends with estimates based on a two-dimensional smoothing approach. Although using other approaches is also conceivable, I use a smoothing approach for count data developed by Camarda (2012) and apply it over age and cohort. This approach was developed to capture the data-generating process behind mortality, which is assumed to be Poisson (Brillinger 1986). Therefore, the approach can also process intervals with zero death counts. Furthermore, the approach provides a sufficient fit to both mortality and the age of minimum mortality (see the online appendix for further details on method evaluation and selection). However, model testing and evaluation were necessary to determine the best calibration for the problem at hand.
The approach by Camarda (2012) uses P-splines within a generalized linear array model. This or a similar approach is widely used in practice to smooth observed mortality rates (see, e.g., Bohk-Ewald and Rau 2017; Colchero et al. 2016; Currie et al. 2004). The method relies on the assumption that death counts are Poisson-distributed over age and time. The Poisson assumption implies that the mean and the variance are equal. However, for most countries in the data set, variance is considerably higher (or lower) than the mean, and the Poisson assumption is therefore violated (see the online appendix for further details). This phenomenon is known as extra Poisson variation, or (under-) overdispersion (Breslow 1984; Djeundje and Currie 2011). Data may be overdispersed for a number of reasons. In many cases, population heterogeneity and unexpected events, such as period shocks, are responsible for the overdispersion. Because variance is higher than the mean, incorporating overdispersion is especially important when seeking to generate robust standard errors. The approach by Camarda (2012) can integrate this specific feature by allowing the variance to change proportional to the mean. Furthermore, because the Poisson assumption allows for the incorporation of age intervals without any deaths, the approach is able to use this information. The method is readily available via the package MortalitySmooth for the statistical programing language R (R Development Core Team 2016).
The occurrence of period shocks, such as the Spanish flu pandemic or a war, can lead to problematic estimates when two-dimensional smoothing approaches are applied because the respective mortality rates in such situations are subject to more than just stochastic variation (Kirkby and Currie 2010; Palloni 1990). When the two dimensions are cohort and age, the situation becomes especially difficult because the period shocks are located on a backward 45-degree line in the age-cohort surface. Hence, in the model calibration, I investigate the influence of such ruptures by fitting them with and without information about ages, which are affected by period shocks. Because of the data structure, I exclude the 1915–1919 and 1938–1947 periods, which cover the Spanish flu pandemic and World Wars I and II. The P-spline approach that I use interpolates the emerging gaps, which are generated when the mortality of the respective ages is ignored.
Based on the evaluation and model testing, I use the following settings to obtain smooth minimum mortality estimates (see the online appendix for further details). Irrespective of the impact in the specific country, I exclude war years to ensure a consistent analysis framework. To avoid potential distortions, I restrict the range of ages to be searched for the minimum mortality to the ages 5–15, which is theoretically reasonable given the range of observed ages. I also control for overdispersion across all countries to provide consistency. Even after these restrictions are applied, overdispersion or underdispersion are found in almost all the countries (see the online appendix for further details).
Results
Level of Minimum Mortality
Figure 2 shows the level of minimum mortality for males and females in France. The online appendix contains the minimum mortality trajectories for all other countries. The graph depicts the level of minimum mortality per 100,000 person-years lived. Levels are shown on a log-scale, using the logarithm of 2 to emphasize level halving. Accordingly, the horizontal contour lines mark the consecutive halving of the mortality level. The solid lines are minimum mortality estimates based on the age-cohort smoothing, and the colored area around this line indicates the 95 % confidence interval. The plus signs indicate observed minimum mortality. The squares mark the observed minimum mortality for cohorts who spent at least one year in the omitted periods (1915–1919, 1938–1947). Females are colored in red and males in blue.
Minimum mortality in France, females and males: Birth cohorts 1900–1993. The graph depicts the observed (squares and crosses) as well as the smoothed (solid line) minimum mortality. The observed rates marked with a square indicate the cohorts who spent at least one year in the omitted periods (World Wars I and II). The colored area around the smoothed minimum mortality estimates depicts the 95 % confidence interval as calculated by the approach of Camarda (2012). Minimum mortality rates are illustrated using the logarithm with basis two. The solid gray grid lines and the Roman numerals mark the different periods of development. Source: Own illustration using age- and cohort-specific death counts and exposure-to-risk from the Human Mortality Database (n.d.)
Figure 2 shows that minimum mortality declined from almost 250 deaths per 100,000 person-years lived to approximately 10 deaths per 100,000 person-years lived over the cohorts born between 1900 and 1993. Over the course of this decline, the trajectories for French males and females show four periods with distinct developments (see tags in Fig. 2). Minimum mortality improves only slowly in the first period (I), which encompasses the cohorts born between 1900 and 1920. The second period (II) is characterized by rapid improvements. This period spans the cohorts born between 1920 and 1950. In the third period (III), minimum mortality improvements decelerated and were close to stagnation at certain points. This trend lasts up to the cohorts born in the early 1960s. The fourth period (IV), which runs until the most recent cohorts, again shows steady improvements. The trajectory of France is exemplary of the trajectories observed in the majority of countries analyzed. Variation can be found only in small temporal differences and in the manifestation of patterns in the four periods described. Only the minimum mortality levels for a few countries, such as those of Russia or Belarus, deviate from the general trend. In these countries, the improvements in minimum mortality over the analyzed cohorts are marginal to nonexistent.
Figure 3 shows the minimum mortality levels for three recent cohorts (1970, 1980, and 1990) for all the countries observed. The countries are ordered based on the minimum mortality level of the 1990 cohort, with the lowest to the highest values being displayed from left to right. To identify the significance of differences in the most recent estimates (1990), minimum mortality for the 1990 cohort is depicted with the corresponding 95 % confidence interval, which is illustrated by the bar around the respective median estimate. Note that the axes for males and females have different ranges.
Minimum mortality, females and males: Birth cohorts 1970, 1980, and 1990. The graph depicts the levels of minimum mortality for the 1970, 1980, and 1990 birth cohorts for all countries analyzed. For Bulgaria, the last available cohort was born in 1989. Countries are ordered according to the minimum mortality level for the cohort born in 1990, with the lowest to the highest levels displayed from left to right. The bars around the median estimate of the 1990 birth cohort depict the 95 % confidence interval, as calculated by the approach of Camarda (2012). Note that the vertical axis has different ranges for males and females. Source: Own illustration using age- and cohort-specific death counts and exposure-to-risk from the Human Mortality Database (n.d.)
Japan currently has the lowest minimum mortality levels at approximately 8 deaths for females and 10 deaths for males per 100,000 person-years lived. For the females of the 1990 birth cohort, the three countries with the lowest minimum mortality levels are Japan, Sweden, and Northern Ireland. For the males of the 1990 birth cohort, the three countries with the lowest minimum mortality levels are Japan, Austria, and Sweden. The estimates for Luxembourg and Iceland rest on data with many zero death rates and should therefore be interpreted with care. The levels among the best-practice countries are very close to one another, which is reflected in the black solid trend and the overlapping confidence intervals. This overlapping, which applies to almost one-half of the countries, suggests that the differences are marginal and are not statistically significant. Therefore, efforts to rank or select clear leaders would be inappropriate. However, among the countries with the highest minimum mortality levels, clear distinctions can be made. Russian males and females have by far the highest levels. Males and females in other eastern European and Baltic countries, as well as in Portugal, also have relatively high minimum mortality levels. Among the G7 countries—or the countries with the greatest economic power—no uniform pattern can be observed. These countries are spread over the remaining rankings above the group of the worst performing countries.
The finding that mortality has declined continuously across almost all countries—and especially among the most recent cohorts—supports the assumption that minimum mortality for both males and females is likely to decrease in the near future. All countries studied show at least a marginal decline in mortality over time. Moreover, in the majority of these countries, a stable pattern of improvement is observed in the cohorts born since the 1970s, and this trend may be expected to continue.
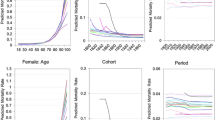
Age of Minimum Mortality
The results for the minimum mortality ages are shown in Fig. 4. The observed mortality rates as well as the smoothed mortality rates are given by age. Hence, the ages of minimum mortality are also measured in integers. Because of stochastic fluctuations and the impact of the world wars, minimum mortality ages based on the smoothed mortality estimates are considered as the basis. Furthermore, the trends across countries are very homogeneous and show only small variations. Therefore, I pool the ages of minimum mortality across countries and summarize the results for 10 consecutive cohort groups. Because of the varying length of the data, the number of ages in each of these 10 groups differs.
Distribution of minimum mortality ages for all countries together, females and males: Grouped birth cohort 1900–1994. The bars show the relative frequency of the ages in the respective cohort groups pooled over all of the available countries. The age of minimum mortality is measured in integers. The number of countries varies over time in each cohort group and is indicated by N. The highlighted bar represents the modal age in the respective year. The bars correspond to full ages. Source: Own illustration using age- and cohort-specific death counts and exposure-to-risk from the Human Mortality Database (n.d.)
The age of minimum mortality decreased over the cohorts studied. This trend is also visible in the ages based on the observed mortality estimates. For the cohorts up to those born in 1920–1929, the modal value jumps between ages 11 and 12. The distribution of males and females for the 1930–1939 and 1940–1949 cohorts are right-skewed, meaning that ages higher than the mode are observed more frequently than younger ages. This is, however, likely an effect of World War II. Although minimum mortality among the cohorts born in 1950–1959 or later has been relatively consistently located at age 11, the distribution is shifting toward younger ages. The shift is indicated quite well by the growing frequency of age 10 as the age of minimum mortality over the respective groups. Accordingly, for the last two cohort groups, the modal value is already located at age 10; and ages above and below the mode are almost evenly observed. However, the growing frequency of age 9 over the last two cohort groups could suggest that the shift toward younger ages might be continuing.
In addition to the location of minimum mortality, I also analyze the form of the U-shape pattern, using the ratio of death rates at ages adjacent to the age of minimum mortality (see the online appendix for more details). However, no clear trend exists across cohorts, countries, or sexes. For some countries, the U-shape remained almost constant; in other countries, considerable differences are visible. Therefore, the location of minimum mortality is much more clear in some countries than in others.
Sex-Specific Differences
The sex-specific differences in the ages of minimum mortality are declining over the cohort groups. For the first three cohort groups, the frequency of the modal value is more pronounced for females than for males. However, especially for the postwar cohorts, the distributions for both males and females are almost similar.
Figure 5 shows the absolute male–female differences in the levels of minimum mortality for all the countries analyzed. The trajectories of Japan, Russia, France, and Norway are highlighted. A negative difference expresses higher mortality for females and vice versa.
Absolute male–female minimum mortality differences in Japan, Russia, France, and Norway: Birth cohorts 1900–1994. The gray lines depict all other countries included in the analysis. The sex differences are calculated based on the smoothed minimum mortality estimates. Source: Own illustration using age- and cohort-specific death counts and exposure-to-risk from the Human Mortality Database (n.d.)
The development of sex-specific differences over time shows two distinct patterns: (1) higher female mortality with a consistently growing male disadvantage followed by (2) a trend toward convergence. In all the countries observed from the 1900 birth cohort onward, the female minimum mortality levels were higher in the first 10 to 20 cohorts, albeit with vastly differing magnitudes. For instance, in the 1900 birth cohort, the minimum mortality level of females was approximately 25 deaths per 100,000 person-years higher than that of males in France, whereas the female minimum mortality level was only approximately 7 deaths higher than that of males in Norway. However, the starting level is also the point at which the female disadvantage was the greatest. The gender gap decreased steadily, with males and females reaching similar levels of minimum mortality somewhere between the 1905 and the 1920 birth cohorts. Thereafter, these varying developments continued, and the sex-specific differences widened once again. The gender gap in minimum mortality rates peaked among the 1940 birth cohort. For example, French males of the cohorts born between 1935 and 1940 had minimum mortality levels that were approximately 15 deaths per 100,000 person-years higher than the minimum mortality levels of their female peers. The growing male disadvantage was mainly driven by the rapid improvements in minimum mortality among females in the cohorts born between 1920 and 1940. After the male disadvantage reached its maximum level, the levels converged steadily in almost all the countries. Russia, however, is an exception to this overall pattern. Among the most recent Russian cohorts analyzed, men have a minimum level that is still approximately 20 deaths per 100,000 person-years higher than that of females. Comparatively, in (for example) Japan, France, and Norway, the absolute male-female differences are almost negligible.
Discussion and Conclusion
Whereas the upper boundary of mortality is a topic that has previously attracted the attention of scholars, the issues surrounding the development and characteristics of the lower boundary have so far been neglected. The lower boundary—minimum mortality—is the lowest mortality rate across ages. It is located at the bottom of the U-shaped pattern, which describes the trajectory of childhood and early adolescent mortality. In this article, I address the past and the present developments of three key features of minimum mortality: level, location, and sex-specific differences.
The analysis rests on cohort mortality data. The lengths of the available time series vary by country, with a maximum range covering the cohorts born between 1900 and 1993. In addition to using observed trends, I complement the analysis with smoothed mortality estimates using a two-dimensional P-spline approach over age and cohort (Camarda 2012). I select this approach after comparing it with a locally weighted regression, testing it, and assessing it under different model specifications (see the online appendix for more details). To prevent the distortion of the minimum mortality estimates by period shocks, I exclude the data for the ages that were affected by World Wars I and II.
Although I remove the war years, a remaining effect of the two world wars cannot be ruled out completely. The temporary acceleration in the decline of minimum mortality for the 1920–1950 cohorts in the smoothed as well as in the observed estimates is visible in almost all the countries, but the pattern is especially pronounced in countries such as Italy, France, or England and Wales, which experienced war on their territories. Those estimates probably do not reflect the real minimum mortality and are additionally influenced by postwar improvements. Thus, the estimates might not reflect the minimum mortality levels that would have been observed in the absence of war.
A further problem for small populations with decreasing mortality is the emergence of age intervals without any deaths. Although the P-spline approach is able to handle this phenomenon, the estimates for Iceland and Luxembourg in particular are not reliable and should be interpreted with care. The number of such intervals within one cohort increases constantly over time and reaches problematic levels. For example, the Icelandic cohorts born between 1975 and 1992 contain an average of 11 such intervals for males and 12 such intervals for females between ages 1 and 20. Given their sudden appearance, the zeroes in Iceland might even be subject to data problems.
The level of minimum mortality decreased continuously over the observed period. Furthermore, the pace of improvement among recent cohorts has been relatively steady. Therefore, recent trends do not suggest an imminent end to this decline. Among the best-practice countries, the current levels are approximately 8 deaths per 100,000 person-years lived for females and 10 deaths per 100,000 person-years lived for males. However, the lower boundary of mortality has not been decreasing constantly. Especially among the postwar cohorts, improvements slowed temporarily, with some countries even experiencing stagnating or slightly increasing levels. The reasons for why minimum mortality stagnated and declined again are open to speculation. The introduction of mass immunization for several diseases in the 1960s could hint at potential explanations (Riley 2001). Other factors, such as the changing fertility-related behavior at that time (Billari and Kohler 2004) or changes in childcare (Vandell et al. 2010), might also serve as potential explanations. Given that the current levels are unprecedented, it is even more intriguing that the lower boundary of mortality has still not reached a lowest limit after almost 170 years of continuous mortality improvements. The question of whether minimum mortality has a lower limit remains open and continues to present challenges. If such a limit does exist, mortality might follow a constant force of mortality, whereby simply good or bad luck are the essential mortality determinants. However, recent developments in childhood health challenge such optimistic and futuristic thoughts. For instance, Brüne and Hochberg (2013) found that chronic diseases in childhood such as obesity, diabetes, or autoimmune diseases have been increasing, especially since the late 1980s. They argued that changes in the environment favor this development; speculating that evolutionary and medical factors—such as thrifty genes, hygiene, fetal programming, or the extensive intake of cow’s milk—might explain this trend. Although rising prevalence of chronic diseases in childhood might not have an immediate effect on death, they could potentially increase the vulnerability, and thus have an indirect effect on the level of minimum mortality. However, based on the results of this study, I cannot confirm any negative influence of such a development on the improvement of minimum mortality up to the most recent cohorts.
The minimum mortality age shifted toward lower ages. For the oldest birth cohorts analyzed, minimum mortality was mainly located at age 12. Over time, however, the modal value shifted toward lower ages, and the distribution around this modal value moved to lower ages. In the most recent cohorts, the lower boundary of age-specific mortality is located at age 10. The location of the lowest mortality across ages is closely associated with the onset of sexual maturity. Evolutionary theories of aging argue that evolutionary fitness, defined as the intrinsic rate of natural increase, is most sensitive to mortality changes around the age of sexual maturity (Hamilton 1966). Accordingly, selection pressure on age-specific mortality should be highest around the onset of the reproductive period, when the respective mortality rates are pushed to their lowest possible levels. Similarly, the age of maturity itself should be under strong selection pressure as a key age that defines the onset of reproduction. Other authors have also argued that intergenerational transfers, such as parental care, shape selection pressure and are an important determinant of the shape of human life history and thus of mortality (Gurven et al. 2012). Consequently, the investments of older generations in younger generations lead to a concave shape of selection pressure, which may push mortality down even further at the onset of the reproductive period, when such investments start to pay off (Bogin 1997; Chu et al. 2008; Lee 2003). As a result of the close relationship between the location of minimum mortality and sexual maturity, it could be hypothesized that the earlier occurrence of minimum mortality might be related to temporal changes in different aspects of childhood development such as body growth and, perhaps as a consequence, to the earlier occurrence of puberty and sexual maturity, which has been reported by a number of authors (Frisch 1978; Goldstein 2011; Schönbeck et al. 2012; Tanner 1973). However, the similar locations of minimum mortality of males and females could be seen as a sign against this idea because different studies provide evidence for a slightly earlier onset of the puberty of females, which also holds for the transition through the different development stages of sexual maturity (Lee 1980; Susman et al. 2010). In addition to these factors, Levitis and Martínez (2013) offered further hypotheses for why juvenile mortality is U-shaped and for why we therefore see an inflection point between the decreasing and the increasing parts of mortality over age. However, the plasticity of minimum mortality challenges all these concepts. Given the enormous gains that have been made over a short period, it is possible to speculate about whether human progress has decoupled minimum mortality from evolutionary mechanisms—or has, at least, weakened the relationship between them.
The development of absolute sex-specific differences in the lower boundary of mortality shows two distinct patterns: higher female mortality with a consistently growing male disadvantage, followed by a trend toward convergence. In the oldest cohort analyzed, females had higher minimum mortality levels. Tuberculosis could be one potential explanation for this female excess mortality. Different authors have documented higher tuberculosis death rates of females in the respective age range (10–14) for similar cohorts as well as for calendar years in which the respective cohorts reached their minimum mortality (Frost 1995; Springett 1952).
Further reasons, such as discrimination related to sex or birth order (Modin 2002), are conceivable but remain as vague speculations. The female disadvantage turned relatively rapidly into a male disadvantage, which reached its maximum level at some point among the interwar cohorts. Since then, a continuous trend toward convergence can be observed. The male disadvantage is the result of slower improvements in the minimum mortality levels of males than of females. These pace differences are striking because the usual determinants of sex-specific differences, such as lifestyle and behavioral factors, should be less relevant at these ages. We can speculate that excess mortality caused by environmental conditions is decreasing more quickly among females than among males. Furthermore, it is possible that after this type of excess mortality is no longer relevant, the gender gap will be primarily driven by biological factors. Currently, communicable diseases can be excluded as a potential driver, and external causes of death explain only a small part of the gender gap (Gissler et al. 2009). Accordingly, nonbehavioral causes and noncommunicable diseases could be emerging as the potential drivers. Studies that used cancer—a leading cause of death in childhood in the developed countries—to illustrate this development found that boys are more likely than girls to develop a childhood cancer (Dorak and Karpuzoglu 2012; Kaatsch 2010).
It is clear that at the minimum mortality age, the physiological and social constitutions of humans are most capable of withstanding death. Following Belsky et al. (2015), I argue that aging research should focus on the age groups that are still in the very early stages of the aging process. In their study, they focused on individuals aged 26–38. Minimum mortality as such marks the inflection point between decreasing and increasing mortality and could thus be interpreted as the point at which aging begins. Hence, investigating the aging process starting from the age of minimum mortality might prove to be even more intriguing, leading to the following questions. Are there some lessons to be learned from the findings on minimum mortality about how aging and mortality might be postponed to or altered at later ages? Can minimum mortality levels be extended to the point of developing a second mortality plateau at younger ages? Or does minimum mortality reflect the baseline level of mortality if humans did not age? These are all nontrivial questions for which there may be no clear answers. However, they all invite further investigation into the lower boundary of human mortality.
References
Armour-Marshall, J., Wolfe, I., Richardson, E., Karanikolos, M., & McKee, M. (2012). Childhood deaths from injuries: Trends and inequalities in Europe. European Journal of Public Health, 22, 61–65.
Belsky, D. W., Caspi, A., Houts, R., Cohen, H. J., Corcoran, D. L., Danese, A., . . . Moffitt, T. E. (2015). Quantification of biological aging in young adults. Proceedings of the National Academy of Sciences, 112, E4104–E4110. https://doi.org/10.1073/pnas.1506264112
Billari, F., & Kohler, H.-P. (2004). Patterns of low and lowest-low fertility in Europe. Population Studies, 58, 161–176.
Blum, R. W. (2009). Young people: Not as healthy as they seem. Lancet, 374, 853–854.
Bogin, B. (1997). Evolutionary hypotheses for human childhood. American Journal of Physical Anthropology, 104(25), 63–89.
Bohk-Ewald, C., & Rau, R. (2017). Probabilistic mortality forecasting with varying age-specific survival improvements. Genus, 73, 1–37. https://doi.org/10.1186/s41118-016-0017-8
Breslow, N. E. (1984). Extra-Poisson variation in log-linear models. Journal of the Royal Statistical Society, Series C: Applied Statistics, 33, 38–44.
Brillinger, D. R. (1986). A biometrics invited paper with discussion: The natural variability of vital rates and associated statistics. Biometrics, 42, 693–734.
Brüne, M., & Hochberg, Z. (2013). Secular trends in new childhood epidemics: Insights from evolutionary medicine. BMC Medicine, 11, 206. https://doi.org/10.1186/1741-7015-11-226
Burger, O., Baudisch, A., & Vaupel, J. W. (2012). Human mortality improvement in evolutionary context. Proceedings of the National Academy of Sciences, 109, 18210–18214.
Camarda, C. G. (2012). MortalitySmooth: An R package for smoothing Poisson counts with P-splines. Journal of Statistical Software, 50. https://doi.org/10.18637/jss.v050.i01
Christensen, K., Doblhammer, G., Rau, R., & Vaupel, J. W. (2009). Ageing populations: The challenges ahead. Lancet, 374, 1196–1208.
Chu, C. C., Chien, H.-K., & Lee, R. D. (2008). Explaining the optimality of U-shaped age-specific mortality. Theoretical Population Biology, 73, 171–180.
Colchero, F., Rau, R., Jones, O. R., Barthold, J. A., Conde, D. A., Lenart, A., . . . Vaupel, J. W. (2016). The emergence of longevous populations. Proceedings of the National Academy of Sciences, 113, E7681–E7690.
Currie, I. D., Durban, M., & Eilers, P. H. (2004). Smoothing and forecasting mortality rates. Statistical Modelling, 4, 279–298.
Cutler, D., Deaton, A., & Lleras-Muney, A. (2006). The determinants of mortality. Journal of Economic Perspectives, 20(3), 97–120.
Djeundje, V., & Currie, I. (2011). Smoothing dispersed counts with applications to mortality data. Annals of Actuarial Science, 5, 33–52.
Dorak, M. T., & Karpuzoglu, E. (2012). Gender differences in cancer susceptibility: An inadequately addressed issue. Frontiers in Genetics, 3, 268. https://doi.org/10.3389/fgene.2012.00268
Frisch, R. E. (1978). Population food intake and fertility. Science, 199, 22–30.
Frost, W. H. (1995). The age selection of mortality from tuberculosis in successive decades. American Journal of Epidemiology, 141, 4–9.
Gampe, J. (2010). Human mortality beyond age 110. In H. Maier, J. Gampe, B. Jeune, J.-M. Robine, & J. W. Vaupel (Eds.), Supercentenarians (pp. 219–230). Heidelberg, Germany: Springer.
Gissler, M., Rahkonen, O., Mortensen, L., Arntzen, A., Cnattingius, S., Andersen, A.-M. N., & Hemminki, E. (2009). Sex differences in child and adolescent mortality in the Nordic countries, 1981–2000. Scandinavian Journal of Public Health, 37, 340–346.
Goldstein, J. R. (2011). A secular trend toward earlier male sexual maturity: Evidence from shifting ages of male young adult mortality. PLoS One, 6(8), e14826. https://doi.org/10.1371/journal.pone.0014826
Gore, F. M., Bloem, P. J., Patton, G. C., Ferguson, J., Joseph, V., Coffey, C., . . . Mathers, C. D. (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet, 377, 2093–2102.
Gurven, M., Stieglitz, J., Hooper, P. L., Gomes, C., & Kaplan, H. (2012). From the womb to the tomb: The role of transfers in shaping the evolved human life history. Experimental Gerontology, 47, 807–813.
Hamilton, W. D. (1966). The moulding of senescence by natural selection. Journal of Theoretical Biology, 12, 12–45.
Heligman, L., & Pollard, J. H. (1980). The age pattern of mortality. Journal of the Institute of Actuaries, 107, 49–80.
Human Mortality Database. (n.d.). Berkeley, University of California; and Rostock, Germany: Max Planck Institute for Demographic Research. Retrieved from www.mortality.org or www.humanmortality.de
Hyndman, R. J., & Ullah, M. S. (2007). Robust forecasting of mortality and fertility rates: A functional data approach. Computational Statistics & Data Analysis, 51, 4942–4956.
Kaatsch, P. (2010). Epidemiology of childhood cancer. Cancer Treatment Reviews, 36, 277–285.
Kirkby, J., & Currie, I. (2010). Smooth models of mortality with period shocks. Statistical Modelling, 10, 177–196.
Klotz, J. (2016, June). Inference for statistics based on complete enumerations? Paper presented at the European Conference on Quality in Official Statistics, Madrid, Spain.
Lee, P. A. (1980). Normal ages of pubertal events among American males and females. Journal of Adolescent Health Care, 1, 26–29.
Lee, R. D. (2003). Rethinking the evolutionary theory of aging: Transfers, not births, shape senescence in social species. Proceedings of the National Academy of Sciences, 100, 9637–9642.
Lee, R. D., & Carter, L. R. (1992). Modeling and forecasting U.S. mortality. Journal of the American Statistical Association, 87, 659–671.
Levitis, D. A. (2011). Before senescence: The evolutionary demography of ontogenesis. Proceedings of the Royal Society, B: Biological Sciences, 278, 801–809.
Levitis, D. A., & Martínez, D. E. (2013). The two halves of U-shaped mortality. Frontiers in Genetics, 4, 1–6. https://doi.org/10.3389/fgene.2013.00031
Missov, T. I., & Vaupel, J. W. (2015). Mortality implications of mortality plateaus. SIAM Review, 57, 61–70.
Modin, B. (2002). Birth order and mortality: A life-long follow-up of 14,200 boys and girls born in early 20th century Sweden. Social Science & Medicine, 54, 1051–1064.
Oeppen, J., & Vaupel, J. W. (2002). Broken limits to life expectancy. Science, 296, 1029–1031.
Palloni, A. (1990). Assessing the levels and impact of mortality in crisis situations. In J. Vallin, S. D’Souza, & A. Palloni (Eds.), Measurement and analysis of mortality: New approaches (pp. 194–228). Oxford, UK: Clarendon Press.
Patton, G. C., Coffey, C., Sawyer, S. M., Viner, R. M., Haller, D. M., Bose, K., . . . Mathers, C. D. (2009). Global patterns of mortality in young people: A systematic analysis of population health data. Lancet, 374, 881–892.
Pletcher, S. D., & Curtsinger, J. W. (1998). Mortality plateaus and the evolution of senescence: Why are old-age mortality rates so low? Evolution, 52, 454–464.
R Development Core Team. (2016). R: A language and environment for statistical Computing. Vienna, Austria: R Foundation for Statistical Computing.
Rau, R., Ebeling, M., Peters, F., Bohk-Ewald, C., & Missov, T. I. (2017, January). Where is the level of the mortality plateau? Paper presented at the Living to 100 Symposium of the Society of Actuaries, Orlando, FL.
Riley, J. C. (2001). Rising life expectancy: A global history. Cambridge, UK: Cambridge University Press.
Schönbeck, Y., Talma, H., van Dommelen, P., Bakker, B., Buitendijk, S. E., HiraSing, R. A., & van Buuren, S. (2012). The world’s tallest nation has stopped growing taller: The height of Dutch children from 1955 to 2009. Pediatric Research, 73, 371–377.
Siler, W. (1983). Parameters of mortality in human populations with widely varying life spans. Statistics in Medicine, 2, 373–380.
Springett, V. (1952). An interpretation of statistical trends in tuberculosis. Lancet, 259, 521–525.
Susman, E. J., Houts, R. M., Steinberg, L., Belsky, J., Cauffman, E., Dehart, G., . . . Eunice Kennedy Shriver NICHD Early Child Care Research Network. (2010). Longitudinal development of secondary sexual characteristics in girls and boys between ages 9 1/2 and 15 1/2 years. Archives of Pediatrics & Adolescent Medicine, 164, 166–173.
Tanner, J. (1973). Trend towards earlier menarche in London, Oslo, Copenhagen, the Netherlands and Hungary. Nature, 243, 95–96.
Udry, J. R., Teddlie, C., & Suchindran, C. M. (1979). The random variation in rates based on total enumeration of events. Population Studies, 33, 353–364.
Vandell, D. L., Belsky, J., Burchinal, M., Steinberg, L., & Vandergrift, N. (2010). Do effects of early child care extend to age 15 years? Results from the NICHD study of early child care and youth development. Child Development, 81, 737–756.
Vaupel, J. W., Carey, J. R., Christensen, K., Johnson, T. E., Yashin, A. I., Holm, N. V., . . . Curtsinger, J. W. (1998). Biodemographic trajectories of longevity. Science, 280, 855–860.
Verguet, S., Norheim, O. F., Olson, Z. D., Yamey, G., & Jamison, D. T. (2014). Annual rates of decline in child, maternal, HIV, and tuberculosis mortality across 109 countries of low and middle income from 1990 to 2013: An assessment of the feasibility of post-2015 goals. Lancet Global Health, 2, e698–e709. https://doi.org/10.1016/S2214-109X(14)70316-X
Wachter, K. W. (1999). Evolutionary demographic models for mortality plateaus. Proceedings of the National Academy of Sciences, 96, 10544–10547.
Wilmoth, J. R., Andreev, K., Jdanov, D., Glei, D. A., Boe, C., Bubenheim, M., . . . Vachon, P. (2007). Methods protocol for the Human Mortality Database (Version 5). Berkeley: University of California; and Rostock, Germany: Max Planck Institute for Demographic Research. Retrieved from http://v5.mortality.org/Public/Docs/MethodsProtocol.pdf
Acknowledgments
I would like to thank Frederik Peters, Roland Rau, and Annette Baudisch for their comments during the project. I am also thankful to the three anonymous reviewers for their helpful and constructive comments.
Funding
Open access funding provided by Max Planck Society.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 459 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ebeling, M. How Has the Lower Boundary of Human Mortality Evolved, and Has It Already Stopped Decreasing?. Demography 55, 1887–1903 (2018). https://doi.org/10.1007/s13524-018-0698-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-018-0698-z