Abstract
Background
Several studies have reported that increased pentraxin-3 (PTX3) levels are associated with impaired renal function in chronic kidney disease (CKD). PTX3 levels increase progressively with diabetic nephropathy (DN) and may be a biomarker for early diagnosis of DN.
Objective
The study evaluates serum PTX3 levels and their association with the development of DN. We also aim to find out whether serum PTX3 is a better marker than high-sensitive CRP (hs-CRP) for DN.
Methods
In this study, we evaluated serum PTX3 levels in 150 patients which were distributed into three groups that are 50 patients with DN, 50 patients with diabetes mellitus (DM) without DN and 50 controls (not any evidence of DM). DN patients were subdivided: 32 patients with microalbuminuria and 18 patients with macroalbuminuria. Serum PTX3 levels were evaluated using an enzyme-linked immunosorbent assay (ELISA) kit.
Results
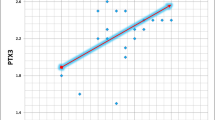
DN group patients had a higher value of PTX3 (p < 0.001) as compared to DM without DN and control groups. hs-CRP levels were higher in DM without DN patients compared to DN patients and controls. PTX3 (p = 0.33) and hs-CRP (p = 0.10) levels among microalbuminuria and macroalbuminuria patients were statistically not significant.
Conclusion
This study concludes that serum PTX3 can be used as a diagnostic marker for DN before the development of apparent chronic kidney disease and PTX3 was found to be a better marker than hs-CRP for diagnosing DN.


Similar content being viewed by others
References
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. https://doi.org/10.1038/s41598-020-71908-9. (Internet).
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research and Clinical Practice. 2021;183(109119):109119. https://doi.org/10.1016/j.diabres.2021.109119.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. https://doi.org/10.1016/j.diabres.2009.10.007. (Internet).
Gewurz H, Zhang XH, Lint TF. Structure and function of the pentraxins. CurrOpin Immunol. 1995;7(1):54–64. https://doi.org/10.1016/0952-7915(95)80029-8. (Internet).
Nauta AJ, De Haij S, Bottazzi B, Mantovani A, Borrias MC, Aten J, et al. Human renal epithelial cells produce the long pentraxin PTX3. Kidney Int. 2005;67(2):543–53. https://doi.org/10.1111/j.1523-1755.2005.67111.x. (Internet).
Zhu H, Yu W, Xie Y, Zhang H, Bi Y, Zhu D. Association of pentraxin 3 gene polymorphisms with susceptibility to diabetic nephropathy. Med Sci Monit [Internet]. 2017;23:428–36.
Suliman ME, Yilmaz MI, Carrero JJ, Qureshi AR, Saglam M, Ipcioglu OM, et al. Novel links between the long pentraxin 3, endothelial dysfunction, and albuminuria in early and advanced chronic kidney disease. Clin J Am Soc Nephrol. 2008;3(4):976–85. https://doi.org/10.2215/CJN.03960907. (Internet).
Prasad RM, Bali A, Tikaria R. Microalbuminuria. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563255/.
Zelmanovitz T, Gerchman F, Balthazar AP, et al. Diabetic nephropathy Diabetol Metab Syndr. 2009;1:10. https://doi.org/10.1186/1758-5996-1-10.
Rodríguez-Gutiérrez R, Montori VM. Glycemic control for patients with type 2 diabetes mellitus: our evolving faith in the face of evidence. Circ Cardiovasc Qual Outcomes. 2016;9(5):504–12. https://doi.org/10.1161/circoutcomes.116.002901. (Internet).
Wang R, Zhang J, Hu W. Association of serum pentraxin 3 concentrations with diabetic nephropathy. J Investig Med. 2016;64(6):1124–7. https://doi.org/10.1136/jim-2016-000082. (Internet).
Uzun S, Ozari M, Gursu M, Karadag S, Behlul A, Sari S, et al. Changes in the inflammatory markers with advancing stages of diabetic nephropathy and the role of pentraxin-3. Ren Fail. 2016;38(8):1193–8. https://doi.org/10.1080/0886022x.2016.1209031. (Internet).
Dawood AA, Kamel MA, Omar TA. Study of serum pentraxin 3 level in patients with diabetic nephropathy. Egypt J Intern Med. 2020;32(1). https://doi.org/10.1186/s43162-020-00002-3.
Al-Barshomy S, Mostafa ME, Shaker G, Wahab L. Serum and urinary pentraxin-3 levels in type 2 diabetes and its relation to diabetic nephropathy. Egypt J Intern Med. 2018;30(4):182. https://doi.org/10.4103/ejim.ejim_9_18. (Internet).
El-Senosy F, Elwakeel ME, Mohamed RE. Study of pentraxin-3 as an early marker of diabetic nephropathy in type 2 diabetes mellitus. Int J Diabetes Res. 2018;7(3):41–9. https://doi.org/10.5923/j.diabetes.20180703.01.
Mezil SA, Ghudhaib KK, Allawi AA. Evaluation of serum pentraxin 3 level in Iraqi patients with diabetic nephropathy. Biochem Cell Arch. 2018;18:2473–7.
Valente MJ, Rocha S, Coimbra S, Catarino C, Rocha PP, Bronze-da-Rocha E, et al. Long pentraxin 3 as a broader biomarker for multiple risk factors in end-stage renal disease: association with all-cause mortality. Mediators of Inflammation. 2019;2019:1–12.
Zlibut A, Bocșan IC, Agoşton-Coldea L. Pentraxin-3 and endothelial dysfunction. Adv Clin Chem. 2019;1:163–79.
Lestariningsih L, Hardisaputro S, Nurani A, Santosa D, Santoso G. High sensitivity C-reactive protein as a predictive of intima-media thickness in patients with end-stage renal disease on regular hemodialysis. Int J Gen Med. 2019;12:219–24. https://doi.org/10.2147/ijgm.s205506. (Internet).
Sjöberg B, Qureshi AR, Heimbürger O, Stenvinkel P, Lind L, Larsson A, et al. Association between levels of pentraxin 3 and incidence of chronic kidney disease in the elderly. J Intern Med. 2016;279(2):173–9. https://doi.org/10.1111/joim.12411. (Internet).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Ananyaa Dixit and Sumithra N. Unni C. The first draft of the manuscript was written by Ananyaa Dixit, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dixit, A., Unni, S.N., Prabhu, S. et al. Role of serum pentraxin-3 levels in patients with and without diabetic nephropathy. Int J Diabetes Dev Ctries (2024). https://doi.org/10.1007/s13410-024-01335-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-024-01335-3