Abstract
Background
Depression is present in individuals with type 2 diabetes mellitus.
Objective
We evaluated the sociodemographic, anthropometric, and clinical features of Mexican individuals with clinical depressive symptoms in order to identify predictors for depression symptoms; finally, we evaluated if HbA1c levels could be used as a probable diagnostic of depressive symptoms in individuals with type 2 diabetes mellitus.
Methods
The population studied consisted of 376 Mexicans with diabetes who were interviewed to collect information about comorbidities and habits. The evaluation of depressive symptoms was performed using the Hamilton scale. For a possible clinical association between HbA1c levels and depressive symptoms, we performed chi-square tests (χ2)/ t tests. A multivariate logistic regression model with the backward conditional method was used to identify predictors of depressive symptoms. An ROC curve was plotted to assess the possible role of HbA1c as a diagnostic predictive test of depression symptoms.
Results
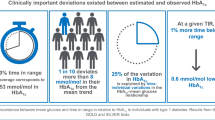
A total of 42.8% (n = 161) individuals showed clinical depressive symptoms. When comparing individuals with and without depression symptoms, those with depression symptoms showed higher levels of glucose and HbA1c; additionally, gender (p = 0.04), age (p = 0.006), HbA1c (p < 0.01), and complications related to diabetes were predictive factors for clinical depressive symptoms (p < 0.01). However, HbA1c showed a low diagnostic accuracy for depressive symptoms, with an area under the ROC curve of 0.59.
Conclusions
Our findings provided evidence of the sex, age, HbA1c levels, and medical complications as predictors of clinical depressive symptoms in individuals with diabetes mellitus. Nevertheless, HbA1c levels are not useful as a diagnostic instrument for depressive symptom severity in these Mexican individuals.

Similar content being viewed by others
Data Availability
Data is available on request.
References
Pordzik J, et al. Significance of circulating microRNAs in diabetes mellitus type 2 and platelet reactivity: bioinformatic analysis and review. Cardiovasc Diabetol. 2019;18(1):113–113.
Atlas, D. International diabetes federation. IDF Diabetes Atlas, 7th edn. Brussels, Belgium: International Diabetes Federation. (2015);33(2).
Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición de Medio Camino 2016 (ENSANUT 2016). Secretaria de Salud: Informe final de resultados. México; 2016.
Calero Bernal ML, Varela Aguilar JM. Infant-juvenile type 2 diabetes. Revista Clinica Espanola. 2018;218(7):372–81.
Hussain S, et al. Prevalence of depression among type 2 diabetes mellitus patients in India: a meta-analysis. Psychiatry Res. 2018;270:264–73.
Sughra U, Imran M. Co-morbid depression in individuals with type 2 diabetes mellitus. JPMA J Pakistan Med Assoc. 2018;68(1):109–11.
Khaledi M, et al. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 2019;56(6):631–50.
Luca M, et al. Gut microbiota in Alzheimer’s disease, depression, and type 2 diabetes mellitus: the role of oxidative stress. Oxid Med Cell Longev. 2019;2019:4730539–4730539.
Yuan S, Larsson SC. An atlas on risk factors for type 2 diabetes: a wide-angled Mendelian randomisation study. Diabetologia. 2020;63(11):2359–71.
Cui R. Editorial: A Systematic Review of Depression. Curr Neuropharmacol. 2015;13(4):480.
Melin EO, et al. Depression differed by midnight cortisol secretion, alexithymia and anxiety between diabetes types: a cross sectional comparison. BMC Psychiatry. 2017;17(1):335.
Akpalu J, et al. Depression and glycemic control among type 2 diabetes patients: a cross-sectional study in a tertiary healthcare facility in Ghana. BMC Psychiatry. 2018;18(1):357–357.
Azniza MR, et al. Depression and potential risk factors among the elderly with type 2 diabetes mellitus in Kedah, Malaysia. Med J Malaysia. 2019;74(2):103–8.
Khan P, et al. Incidence of anxiety and depression among patients with type 2 diabetes and the predicting factors. Cureus. 2019;11(3):e4254–e4254.
Ehrenthal JC, et al. Levels of personality functioning and not depression predict decline of plasma glucose concentration in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2019;151:106–13.
Luke B. Adverse effects of female obesity and interaction with race on reproductive potential. Fertil Steril. 2017;107(4):868–77.
Hamilton M. The Hamilton Depression Scale—accelerator or break on antidepressant drug discovery. Psychiatry. 1960;23:56–62.
National Institute for Health and Care Excellence. Depression in adults: recognition and management. London: National Institute for Health and Care Excellence; 2018.
Cortés J, Berlanga C, Bauer J. Adaptación y validación de la Escala de Depresión de Carroll en español. 1992;15(4):36–430.
Sharif S, et al. Frequency of depression in patients with type 2 diabetes mellitus and its relationship with glycemic control and diabetic microvascular complications. Cureus. 2019;11(7):e5145–e5145.
Yasui-Furukori N, et al. Coping behaviors and depressive status in individuals with type 2 diabetes mellitus. Ann Gen Psychiatry. 2019;18:11–11.
Alzahrani A, et al. Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: a cross-sectional study. Int J Ment Heal Syst. 2019;13:48–48.
Park LT, Zarate CA Jr. Depression in the primary care setting. N Engl J Med. 2019;380(6):559–68.
Stickel S, et al. Neural correlates of depression in women across the reproductive lifespan - An fMRI review. J Affect Disord. 2019;246:556–70.
Mansori K, et al. Association between depression with glycemic control and its complications in type 2 diabetes. Diabetes Metab Syndr. 2019;13(2):1555–60.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37(3):278–316.
Kim HJ, et al. The association of diabetes duration and glycemic control with depression in elderly men with type 2 diabetes mellitus. J Res Med Sci. 2019;24:17–17.
Jaworski M, et al. Severe depressive episode with psychotic symptoms and type 2 diabetes: a 2010–2017 longitudinal study. Med Sci Monit: Int Med J Exp Clin Res. 2019;25:1760–8.
Afroz A, et al. Macro- and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr. 2019;13(5):2939–46.
Bilu C, et al. Linking type 2 diabetes mellitus, cardiac hypertrophy and depression in a diurnal animal model. Sci Rep. 2019;9(1):11865–11865.
Arambewela MH, et al. Prevalence of depression and associated factors among patients with type 2 diabetes attending the diabetic clinic at a tertiary care hospital in Sri Lanka: a descriptive study. Psychiatry J. 2019;2019:7468363–7468363.
Alajmani DSA, et al. Prevalence of undiagnosed depression in patients with type 2 diabetes. Front Endocrinol. 2019;10:259–259.
Ma Y, et al. Association between cognitive vulnerability to depression - dysfunctional attitudes and glycemic control among in-patients with type 2 diabetes in a hospital in Beijing: a multivariate regression analysis. Psychol Health Med. 2018;23(2):189–97.
Li CI, et al. Competing risk analysis on visit-to-visit glucose variations and risk of depression: the Taiwan diabetes study. Diabetes Metab. 2020;46(3):223–9.
Atif M, et al. Extent and predictors of poor glycemic control among elderly Pakistani patients with type 2 diabetes mellitus: a multi-centre cross-sectional study. Medicina (Kaunas). 2019;55(1):21.
Bąk E, et al. An assessment of diabetes-dependent quality of life (ADDQoL) in women and men in Poland with type 1 and type 2 diabetes. Ann Agric Environ Med: AAEM. 2019;26(3):429–38.
Dhillon H, Nordin RB, Ramadas A. Quality of life and associated factors among primary care Asian patients with type 2 diabetes mellitus. Int J Environ Res Public Health. 2019;16(19):3561.
González-Castro TB, et al. Higher risk of depression in individuals with type 2 diabetes and obesity: results of a meta-analysis. J Health Psychol. 2021;26(9):1404–19.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Clearance
This study was approved by the ethics and research committee and the ethics committee of the High Specialization Regional Hospital Dr. Gustavo A. Rovirosa Pérez (00228/16).
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Juárez-Rojop, I.E., Tovilla-Vidal, G., López-Narváez, M.L. et al. Evaluation of HbA1c levels as probable diagnostic of depression symptoms in Mexican individuals with type 2 diabetes mellitus. Int J Diabetes Dev Ctries (2023). https://doi.org/10.1007/s13410-023-01232-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-023-01232-1