Abstract
Background
The capillary blood glucose monitoring program at home a challenge in primary health care. Therefore, it is fundamental to identify the glycemic control of people with diabetes mellitus through HBA1c and to analyze its associated factors.
Objective
To identify the glycemic profile of people with Diabetes Mellitus (DM) through HbA1c and analyze factors associated.
Materials & methods
Cross-sectional study developed in Ribeirão Preto, São Paulo, Brazil. Secondary data from the electronic health record of people registered in the Primary Health Care system were used. A sample of 3181 participants was obtained. People with HbA1c < 7.0% (53 mmol/mol) were considered to have adequate glycemic control. For people aged ≥ 55 years, a less stringent target, < 8.0% (64 mmol/mol), was also considered. The odds ratio was the measure of effect analyzed with their respective 95% Confidence Intervals (95% CI).
Results
Adequate glycemic control with HbA1c < 7.0% (53 mmol/mol) was found in 44.8% of people and, when using the less rigid target, HbA1c < 8.0% (64 mmol/mol) for people aged ≥ 55 years-old, 70.6% had adequate glycemic control. Age and drug therapy were associated with adequate glycemic control (p < 0.001), which was more frequent among older people and those who used only metformin.
Conclusion
The study shows that the achievement of adequate glycemic control is still a challenge, especially with regard to younger people and those who use insulin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic Non-Communicable Diseases (NCDs) are the leading cause of mortality worldwide and accounted for 71.0% of all deaths that occurred in 2016. While there has been a reduction in the overall rates of premature mortality (age 30–70 years) from chronic respiratory diseases, cardiovascular diseases and cancer, the diabetes mellitus (DM), in contrast, showed an increase of 5.0% between the years 2000 and 2016 [1, 2].
Estimates indicate that in 2019, every eight seconds a person aged 20–79 years died from DM, with almost half of the 4.2 million deaths occurring before the age of 60 years. The worldwide expenditure on DM complications is approaching U$760 billion. In addition, it is one of the diseases whose frequency is increasing in several countries around the world, with a projection of reaching 700 million people in 2045. Thus, DM imposes a high burden on society, in the form of high medical and hospital costs, loss of productivity, premature mortality, and compromised quality of life [2,3,4,5].
DM-related complications such as cardiovascular disease, retinopathy, nephropathy, neuropathy are related to hyperglycemia. After classical studies showed the correlation of hyperglycemia with the presence of complications of DM, glycated hemoglobin (HbA1c) has been consolidated as one of the main markers of glycemic control [6, 7]. In type 2 DM, for each 1.0% reduction in HbA1c there is a 21.0% decrease in the risk of any outcome related to the disease, 21.0% for deaths, 14.0% for myocardial infarction and 37.0% for microvascular complications [8,9,10]. The goal of glycemic control through HbA1c recommended by the main guidelines is below 7.0% (53 mmol/mol) and may be more flexible depending on the clinical conditions of each person, life expectancy and episodes of hypoglycemia [9, 10].
Despite advances in therapy, adequate glycemic control of people with DM is a challenge in several regions of the world. A meta-analysis showed that globally, only 42.8% of people achieved optimal HbA1c targets, with Europe and North America showing the best results [11]. Recent studies found adequate glycemic control rates of 31.8% in Mexico, 53.4% in Colombia, 48.9% in Argentina, and 50.4% and 53.4%, respectively, in men and women in Korea [12,13,14,15]. In Brazil, a study in the southern region showed 30.2% of people enrolled in primary health care (PHC) with adequate glycemic control [16].
Recently, the new coronavirus pandemic has directed even more attention to people with NCDs, since the pre-existence of these comorbidities dramatically elevates mortality rates by COVID-19 [17, 18]. People with uncontrolled DM have impairment in innate immunity, the first line of defense against Sars-Cov-2, and other important alterations in the inflammatory response, which may lead to aggravation of COVID-19. On the other hand, infection by COVID-19 worsens dysglycemia, causing a vicious circle between DM and COVID-19 with unfavorable clinical outcomes. DM and hyperglycemia at hospital admission are associated with worse prognosis [18, 19].
Brazil is one of the countries with the highest prevalence of DM in the world. Recent studies have shown that most people who perform home self-monitoring experienced greater variability in blood glucose during the pandemic, in addition to many having postponed medical appointments and routine exams [20, 21]. In view of the recommendations for monitoring glycemic control, the Ministry of Health of Brazil instituted the evaluation of HbA1c in 2020 as an indicator of PHC performance in the country, and municipalities that meet the evaluation goals receive financial resources related to good performance in this indicator [10].
Few studies assessed glycemic control of Brazilian patients in PHC. Therefore, in order to provide subsidies for the planning of health care and actions, this study has the following objectives: to identify the glycemic profile of people with DM through HbA1c and analyze factors associated with glycemic control.
Methods
Study design and participants
Quantitative, observational, cross-sectional study developed in Ribeirão Preto, São Paulo, Brazil. Secondary data from the electronic health record of people registered in the PHC system were used. People aged ≥ 18 years, using oral antidiabetics (OAD) and/or injectables provided in the Brazilian PHC system (metformin, glibenclamide, gliclazide, regular insulin, and NPH insulin) and who had at least one record of HbA1c value in 2018 were included in the sample. The stratified random sampling method was applied, and people from the five health districts of Ribeirao Preto (North, South, East, West and Central) were proportionally selected. Therefore, a sample of 3181 participants was obtained. We adopted a significance level of 5.0%, relative error of 5.0% and prevalence of 27.0% of expected event [22].
Data collection
Data were extracted from electronic health records and recorded on a structured form containing sociodemographic variables: sex (male and female) and age (< 25 years, from 25 to 34, from 35 to 44, from 45 to 54, from 55 to 64, from 65 to 74 and ≥ 75 years of age); and clinical variables: drug therapy (metformin only, sulfonylurea only, insulin only, metformin + sulfonylurea and ADO + insulin) and HbA1c value.
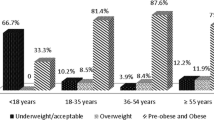
People with HbA1c < 7.0% (53 mmol/mol) were considered to have adequate glycemic control. For people aged ≥ 55 years, a less stringent target, < 8.0% (64 mmol/mol), was also considered. For people with HbA1c values < 6.5%, the cut-off value for diabetes diagnosis, an investigation of the electronic health record was performed, searching for previous laboratory tests and/or medical records that would confirm or not the diagnosis of diabetes. This procedure was justified since some people with pre-diabetes also use ADO such as metformin, as shown in Fig. 1.
High-Efficiency Liquid Chromatography and Immunoturbidimetry were the laboratory analysis methods used in the reference laboratories of Ribeirao Preto's PHC.
Statistical analysis
Statistical Package for Social Sciences (SPSS) for windows version 20.0 was used for statistical analysis. Frequency calculations were performed by basic descriptive analysis. The relationship between glycemic control and sociodemographic and clinical variables was analyzed by means of Binary Logistic Regression, and the odds ratio (OR) was the measure of effect analyzed with their respective 95% Confidence Intervals (95% CI). The model was adjusted by selecting the independent variables that presented statistical significance in the univariate analysis, obtaining the adjusted odds ratio (ORaj).
Ethical aspects
The project was approved by the Research Ethics Committeê of the School of Nursing of the University of Ribeirão Preto by opinion no. 3,340,774 on May 22, 2019.
Results
Among people being treated with ADOs in PHC, there was a predominance of females (60.5%) and adults and elderly, and most people (92.0%) were older than 45 years, according to Table 1. Metformin was the most used drug (60.8%), being used in isolation by 27.5% of people. Among the sulfonylurea drugs, gliclazide was used by 42.0% of people. Only 19.7% of people used sulfonylurea, while 21.1% used metformin + sulfonylurea. As for insulins, 13.4% used insulin alone and 18.3% associated with OAD.
We removed from the sample 111 people who, after obtaining data from medical records, did not confirm the diagnosis of DM. In addition, due to the low representation in the sample, it was decided to exclude people under 25 years of age. Thus, among people with confirmed DM diagnosis and age ≥ 25 years (n = 3063), HbA1c ranged from 3.3% (13 mmol/mol) to 18.1% (174 mmol/mol), with a mean of 7.6% (60 mmol/mol) [95% CI 7.5—7.6% (59—60 mmol/mol)]. Adequate glycemic control, HbA1c < 7.0% (53 mmol/mol), was found in 44.8% of participants with DM (95% CI 42.9—46.6%). Men and women had similar frequencies of adequate glycemic control.
According to Table 2, age and drug therapy were associated with glycemic control (p < 0.001). The frequency of adequate glycemic control increased progressively with age, and in people aged ≥ 75 years, the chance of achieving adequate glycemic control is 2.79 times higher than in people aged 25–34 years [ORaj = 2.79 (95% CI 1.35—5.76)]. People using insulin had the lowest frequencies of adequate glycemic control. The chance of achieving adequate glycemic control is 91.0% lower among people using insulin only [ORaj = 0.09 (95% CI 0.07—0.12)] and 93.0% lower among those using insulin + ADO [ORaj = 0.07 (95% CI 0.05—0.09)] when compared to those using metformin only.
Age is one of the factors to be considered in adjusting the HbA1c target, which may be less strict among older people. Thus, regarding the achievement of the less stringent glycemic target, HbA1c < 8.0% (64 mmol/mol), among people aged ≥ 55 years (n = 2356) it was observed that 70.6% (95% CI 68.8—72.6%) had adequate glycemic control. HbA1c ranged from 3.3% (13 mmol/mol) to 16.0% (151 mmol/mol), with a mean of 7.4% (57 mmol/mol) [95% CI 7.3—7.5% (56—58 mmol/mol)].
Even in cases of less stringent glycemic target, according to Table 3, age and drug therapy remained associated with glycemic control (p < 0.001). In people aged ≥ 75 years, the chance of finding HbA1c < 8.0% (64 mmol/mol) is 1.86 times higher than in people aged 25–34 years [ORaj = 1.86 (95% CI 1.42—2.43)]. Those using insulin had the lowest frequencies of adequate glycemic control. When compared to people using metformin only, the chance of finding adequate glycemic control for this goal is 93.0% lower in people using insulin only [ORaj = 0.07 (95% CI 0.04—0.10)] and 94.0% lower in people using insulin + ADO [ORaj = 0.06 (95% CI 0.04—0.10)].
Discussion
In our sample, 44.8% (95% CI 43.0—46.5%) showed adequate glycemic control with no differences between males and females. A study conducted in England among people with DM and aged ≥ 20 years, considering identical criteria to the present study to classify glycemic control, showed a frequency of adequate glycemic control of 49.7%, i.e., slightly higher than that found in the present investigation [23, 24]. Similar findings were recorded in countries such as Japan among people aged 20 to 69 years and also in China among those ≥ 18 years, in which 44.9% and 49.2%, respectively, had adequate glycemic control [25, 26].
On the other hand, in Portugal, 63.2% of people with DM and age between 25 and 74 years had adequate glycemic control. However, the criterion used in the study was having HbA1c ≤ 7.0% (53 mmol/mo) [27].
In our findings, age and drug therapy were associated with glycemic control. A municipality in the southern region of Brazil had similar findings, with elderly ≥ 70 years showing less elevation of HbA1c than people aged 50—69 years [16]. Similarly, in the United States, people with DM ≥ 75 years old had 40.0% more adequate glycemic control compared to those aged 40 to 49 years. According to the authors, the elderly were treated more intensively (use of insulin or two or more hypoglycemic medications) than young adults to achieve the goal of HbA1c < 7.0% (53 mmol/mol) [28].
Adherence to drug treatment is an important factor to be considered in achieving adequate glycemic control. Study in Sudan showed the relationship between low adherence and higher levels of HbA1c; and further, that people with low adherence were younger, which reiterates that the older the age the higher the frequency of adequate glycemic control, a fact that is presumed to have been strengthened by greater adherence to treatment by older people [29].
In Brazilian PHC, ADOs are prescribed on a large scale which was evidenced in the present investigation which recorded the use of metformin by 60.8% either alone or associated with sulfonylureas (gliclazide or glibenclamide). Before prescribing antidiabetics, professionals take into consideration the patient's general condition, the presence of comorbidities or obesity, the cost and the risk of hypoglycemia. Currently, metformin is the initial drug of choice recommended by the Brazilian Diabetes Society algorithm and, in the persistence of hyperglycemia, the combination with sulfonylureas becomes the option available at the Unified Health System [10]. In addition, the use of metformin has been related to the reduction of cardiovascular mortality, overall mortality, and cardiovascular events in people with coronary artery disease, besides being considered better than sulfonylureas in reducing the incidence of cardiovascular events [30]. It is worth noting that currently there are investigations that have shown encouraging results with the use of herbal medicines such as ginger and cinnamon in reducing the glycemic levels of ADO users [31, 32].
With regard to insulin, the chance of finding adequate glycemic control was 91.0% lower among people using insulin alone. In our findings, insulin was used by 31.7% of people, being similar to the study by Mendes et al. [22] where 34.0% of patients with type 2 diabetes were on insulin treatment. In clinical practice, in the initial presentation of type 2 DM, modifications in lifestyle habits associated with the use of metformin are indicated. The frequency of insulin use becomes higher as the duration of diabetes increases, given the natural progression of type 2 DM, which causes a gradual decrease in insulin production by the pancreas. Generally, after a decade of disease progression, it is necessary to associate the use of insulin with ADO. Thus, the Brazilian Diabetes Society stresses the importance of the timely initiation of insulin therapy, which often does not happen due to therapeutic inertia, fear of weight gain, fear of hypoglycemia, among other reasons [10].
However, even when setting less strict glycemic goals, people using insulin showed lower frequencies of adequate glycemic control. It is noteworthy that the less stringent glycemic target was established only considering the criterion of advanced age. Therefore, among people with DM and age ≥ 55 years, 70.6% (95% CI 68.8—72.6%) had HbA1c < 8.0% (64 mmol/mol). These findings are similar to others obtained by researchers who adopted the less rigid goal in the evaluation of people with DM. In this direction, we highlight the investigation developed in the southeastern United States, which identified adequate glycemic control in 63.5% of participants [33]. On the other hand, national data showed a slightly lower percentage, i.e., 60.0% with HbA1c < 8.0% (64 mmol/mol) [20].
It was evidenced in all analyses that the chance of finding adequate glycemic control is significantly lower in people using insulin than in those using metformin alone. Scholars pointed out that people who did not reach their HbA1c target were treated with substantially higher insulin doses than those who did. Therefore, it is noted that even by intensifying the dose of drug therapy, adequate glycemic control remains difficult to achieve [23]. The delay in intensifying drug treatment after the identification of elevated levels of HbA1c can reach, on average, more than one year, being even more significant in situations in which a larger number of antidiabetic drugs are used [34].
Furthermore, researchers draw attention to a worrying finding: 44.0% of people with HbA1c levels ≥ 9.0% (75 mmol/mol) did not have their drug therapy intensified [35]. It is also emphasized that therapeutic inertia may result from a combination of factors related to patients, health professionals and the health system, being a complex conduct that needs to be better investigated [36].
It is worth considering that adherence to insulin treatment is multifactorial, since it may be related to low socioeconomic status, fear of hypoglycemia, the fact that it is injectable and, in most cases, requires more than one daily application [37, 38]. In addition, the technique of insulin application requires specific knowledge and skills, and errors regarding self- application or application by others are not uncommon, especially due to decreased visual acuity which can compromise the achievement of adequate glycemic control [39,40,41].
The present study did not distinguish between the different types of diabetes and neither the time of diagnosis due to incomplete information in the electronic health record. However, it is recognized that both are important in the analysis of the frequency of insulin use. Another limitation of the study is the fact that the data refer to drugs dispensed by pharmacies in the primary health care network, not having computed those acquired by other means. In this regard, the study on access, use and promotion of rational use of medicines showed that 97.8% of people diagnosed with diabetes reported having access to prescribed antidiabetic drugs and 70.7% get them completely free of charge [42].
Although the glycemic control data found in this study approximate those for developed countries, it was found that just under half of people with DM achieved the more stringent goal of adequate glycemic control, even before the covid-19 pandemic. It is believed that the changes arising from this current health scenario contribute even more to inadequate glycemic control, both by lockdowns and by the limitation of care, and even by the fear of crowding and contagion. Therefore, in the current pandemic context, we emphasize the need for investment in strategies to overcome the new challenges imposed, such as the use of distance interaction technologies, teleconsultations, digital educational materials and guaranteed access to essential medicines and continuity of care [43].
Conclusion
The present study showed that less than half of the participants achieved adequate glycemic control and younger people with DM and on insulin treatment showed the lowest rates of adequate glycemic control. In addition, the study data showed that in the population studied, only 63.9% of people with DM had their HbA1c evaluated. As this is a component of the performance evaluation for PHC recently incorporated by the MS, there is an imminent need for further expansion of access and professional training so that HbA1c appears in the assessments of people with DM and, in this way, health teams guarantee the associated financial resources to this indicator.
References
World Health Organization. World health statistics 2020: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020.
Williams R, Colagiuri S, Chan J, Gregg E, Ke C, Lim, L-L, Yang X. IDF Diabetes Atlas 9th Edition 2019. Belgium: International Diabetes Federation;2019. Available in: https://www.researchgate.net/publication/337253094_IDF_Atlas_9th_Edition_2019.
Yang W, Dall TM, Beronjia K, Lin J, Semilla AP, Chakrabarti R, et al. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–28. https://doi.org/10.2337/dci18-0007.
Malta DC, Bernal RTI, Lima MG, de Araújo SSC, da Silva MMA, de Fatima Freitas MI, et al. Noncommunicable diseases and the use of health services: Analysis of the National Health Survey in Brazil. Rev Saude Publica. 2017;51(1):1–10. https://doi.org/10.1590/S1518-8787.2017051000090.
Lima RAD, Istilli PT, Teixeira CRS, Zanetti ML, Torquato MTCG. Diabetes mellitus mortality in a municipality in the state of São Paulo, 2010 to 2014. Rev Saude Publica. 2019;53:1–9.
Turner R. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–53. https://doi.org/10.1016/S0140-6736(98)07019-6.
The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long- Term Complications in Insulin-Dependent Diabetes Mellitus. N Engl J Med 1993; 329:977–86. https://doi.org/10.1056/NEJM199309303291401.
Stratton IM, Adler AI, Neil HAW, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ. 2000;321:405–12. https://doi.org/10.1136/bmj.321.7258.405.
American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes - 2021. Diabetes Care. 2021;44(sup 1):73–84. https://doi.org/10.2337/dc21-S006.
Sociedade Brasileira de Diabetes. Guidelines of the Brazilian Society of Diabetes 2019–2020. São Paulo: Clanad; 2019.
Khunti K, Ceriello A, Cos X, de Block C. Achievement of guideline targets for blood pressure, lipid, and glycemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract. 2018;137:137–48. https://doi.org/10.1016/j.diabres.2017.12.004.
Shin J-Y. Trends in the prevalence and management of diabetes in Korea: 2007–2017. Epidemiol Health. 2019;41:e2019029. https://doi.org/10.4178/epih.e2019029.
Basto-Abreu A, Barrientos-Gutiérrez T, Rojas-Martínez R, Aguilar-Salinas CA, López- Olmedo N, Cruz-Góngora V, et al. Prevalence of diabetes and poor glycemic control in Mexico: results from Ensanut 2016. Salud Publica Mex. 2020;62(1):50–9. https://doi.org/10.21149/10752.
Piñeros-Garzón FS, Rodríguez-Hernández JM. Factores de riesgo asociados al control glucémico y síndrome metabólico en pacientes con diabetes mellitus tipo 2. Villavicencio, Colombia. US 2018;21 (1):61–71. https://doi.org/10.22267/rus.192101.140.
Elgart JF, Silvestrini C, Prestes M, Gonzalez L, Rucci E, Gagliardino JJ. Drug treatment of type 2 diabetes: Its cost is significantly associated with HbA1c levels. Int J Clin. 2019;73:1–7. https://doi.org/10.1111/ijcp.13336.
Rossaneis MA, de Andrade SM, Gvozd R, Pissinati PSC, Haddad MCL. Factors associated with glycemic control in people with diabetes mellitus. Ciênc saúde colet. 2019;24(3):997–1006. https://doi.org/10.1590/1413-81232018243.02022017.
Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42. https://doi.org/10.1001/jama.2020.2648.
Pal R, Bhadada SK. COVID-19 and diabetes mellitus: An unholy interaction of two pandemics. Diabetes Metab Syndr Clin Res Rev. 2020;14(4):513–7. https://doi.org/10.1016/j.dsx.2020.04.049.
Liu S, Zhang Q, Wang W, Zhang M, Liu C, Xiao X, et al. Hyperglycemia is a strong predictor of poor prognosis in COVID-19. Diabetes Res Clin Pract. 2020;167(108338):1–7. https://doi.org/10.1016/j.diabres.2020.108338.
Carvalho Malta D, Duncan B, Schmidt M, Machado Í, Silva A, Bernal R, et al. Prevalence of diabetes mellitus determined by glycated hemoglobin in the Brazilian adult population, National Health Survey. Rev Bras Epidemiol. 2019;22(Sup 2):1–13. https://doi.org/10.1590/1980-549720190006.supl.2.
Barone MTU, Harnik SB, de Luca PV, Lima BLS, Wieselberg RJP, Ngongo B, et al. The impact of COVID-19 on people with diabetes in Brazil. Diabetes Res Clin Pract. 2020;166:108304. https://doi.org/10.1016/j.diabres.2020.108304.
Mendes ABV, Fittipaldi JAS, Neves RCS, Chacra AR, Moreira ED. Prevalence and correlates of inadequate glycemic control: Results from a nationwide survey in 6,671 adults with diabetes in Brazil. Acta Diabetol. 2010;47:137–45. https://doi.org/10.1007/s00592-009-0138-z.
Jalving AC, Gant CM, Binnenmars SH, Soedamah-Muthu SS, Bakker SJL, Navis G, et al. glycemic control in the diabetes and Lifestyle Cohort Twente: A cross-sectional assessment of lifestyle and pharmacological management on Hba1c target achievement. Diabetes Obes Metab. 2018;20:2494–9. https://doi.org/10.1111/dom.13399.
McAlister FA, Lethebe BC, Lambe C, Williamson T, Lowerison M. Control of glycemia and blood pressure in British adults with diabetes mellitus and subsequent therapy choices: a comparison across health states. Cardiovasc Diabetol. 2018;17(27):1–11. https://doi.org/10.1186/s12933-018-0673-4.
Hu H, Hori A, Nishiura C, Sasaki N, Okazaki H, Nakagawa T, et al. Hba1c, blood pressure, and lipid control in people with diabetes: Japan epidemiology collaboration on occupational health study. PLoS ONE. 2016;11:1–13. https://doi.org/10.1371/journal.pone.0159071.
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317:2515–23. https://doi.org/10.1001/jama.2017.7596.
Barreto M, Kislaya I, Gaio V, Rodrigues AP, Santos AJ, Namorado S, et al. Prevalence, awareness, treatment and control of diabetes in Portugal: Results from the first National Health examination Survey (INSEF 2015). Diabetes Res Clin Pract. 2018;140:271–8. https://doi.org/10.1016/j.diabres.2018.03.052.
Casagrande S, Cowie CC, Fradkin JE. Intensive glycemic control in younger and older U.S. adults with type 2 diabetes. J Diabetes Complicat. 2017;31:1299–304. https://doi.org/10.1016/j.jdiacomp.2017.05.006.
Mirghani HO. An evaluation of adherence to anti-diabetic medications among type 2 diabetic patients in a Sudanese outpatient clinic. Pan Afr Med J Conf Proc 2019;34. https://doi.org/10.11604/pamj.2019.34.34.15161.
Han Y, Xie H, Liu Y, Gao P, Yang X, Shen Z. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: A systematic review and an updated meta-analysis. Cardiovasc Diabetol. 2019;18(1):1–16. https://doi.org/10.1186/s12933-019-0900-7.
Neto JCGL, Damasceno MMC, Ciol MA, et al. Analysis of the effectiveness of cinnamon (Cinnamomum verum) in the reduction of glycemic and lipidic levels of adults with type 2 diabetes: A study protocol. Medicine (Baltimore). 2020;99(1):e18553. https://doi.org/10.1097/MD.0000000000018553.
Carvalho GCN, Lira-Neto JCG, de Araújo MFM, de Freitas RWJF, Zanetti ML, Damasceno MMC. Effectiveness of ginger in reducing metabolic levels in people with diabetes: a randomized clinical trial. Rev Latino-Am Enfermagem. 2020;28:1–10. https://doi.org/10.1590/1518-8345.3870.3369.
Walker RJ, Neelon B, Davis M, Egede LE. Racial differences in spatial patterns for poor glycemic control in the Southeastern United States. Ann Epidemiol. 2018;28:153–9. https://doi.org/10.1016/j.annepidem.2018.01.008.
Khunti K, Gomes MB, Pocock S, Shestakova MV, Pintat S, Fenici P, et al. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: A systematic review. Diabetes Obes Metab. 2018;20:427–37. https://doi.org/10.1111/dom.13088.
Pantalone KM, Misra-Hebert AD, Hobbs TM, Ji X, Kong SX, Milinovich A, et al. Clinical inertia in type 2 diabetes management: Evidence from a large, real-world data set. Diabetes Care. 2018;41:e113–4. https://doi.org/10.2337/dc18-0116.
John JO, Quiñones PM. Addressing Clinical Inertia in Type 2 Diabetes Mellitus: A Review. Advances in Therapy n.d.;35. 10.6084/m9.figshare.7200860.
Bermeo-Cabrera J, Almeda-Valdes P, Riofrios-Palacios J, Aguilar-Salinas CA, Mehta R. Insulin Adherence in Type 2 Diabetes in Mexico: Behaviors and Barriers. J Diabetes Res 2018; 1–8. https://doi.org/10.1155/2018/3190849.
Batais MA, Schantter P. Prevalence of unwillingness to use insulin therapy and its associated attitudes amongst patients with Type 2 diabetes in Saudi Arabia. Prim Care Diabetes. 2016;10:415–24. https://doi.org/10.1016/j.pcd.2016.05.007.
Dong Q, Huang J, Liu S, Yang L, Li J, Li B, et al. A survey on glycemic control rate of type 2 diabetes mellitus with different therapies and patients’ satisfaction in China. Patient Prefer Adherence. 2019;13:1303–10. https://doi.org/10.2147/PPA.S198908.
dos Reis P, Marcon SS, Nass EMA, de Arruda GO, Back IR, Lino IGT, et al. Performance of people with diabetes mellitus under insulin therapy. Cogitare. 2020;25:1–12. https://doi.org/10.5380/ce.v25i0.66006.
Carvalho GC, Freitas RW, Araújo MF, Zanetti ML, Damasceno MM. Visual acuity in the management of diabetes mellitus: preparation of the insulin dose. Acta Paul Enferm. 2017;30(1):25–30. https://doi.org/10.1590/1982.
Meiners MMMA, Tavares NUL, Guimarães LSP, Bertoldi AD, Pizzol TSD, Luiza VL, et al. Access and medication adherence among people with diabetes in Brazil: Evidence from PNAUM. Rev Bras Epidemiol. 2017;20:445–59. https://doi.org/10.1590/1980-5497201700030008.
Barone MTU, Ngongo B, Harnik SB, de Oliveira LX, Végh D, de Luca PV, et al. COVID-19 associated with diabetes and other noncommunicable diseases led to a global health crisis. Diabetes Res Clin Pract. 2021;171:1–10. https://doi.org/10.1016/j.diabres.2020.108587.
Acknowledgements
Coordination of Superior Level Staff Improvement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Calixto, A.A.S., Franco, L.J., La Banca Barber, R.O. et al. Glycemic outcomes of people with diabetes mellitus in Brazilian primary health care. Int J Diabetes Dev Ctries 44, 91–98 (2024). https://doi.org/10.1007/s13410-023-01203-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-023-01203-6