Abstract
Aim
Diabetes mellitus is recognised as a major chronic pandemic disease that does not consider any ethnic and monetary background. There is a dearth of literature on the cost of diabetes in the Indian context. Therefore, the present study aims to capture the evidence from the literature on the cost of diabetes mellitus in India.
Methods
An extensive literature was reviewed from ACADEMIA, NCBI, PubMed, ProQuest, EBSCO, Springer, JSTOR, Scopus and Google Scholar. The eligibility criterion is based on ‘PICOS’ procedure, and only those studies which are available in the English language, published between 1999 and February 2019, indexed in ABDC, EBSCO, ProQuest, Scopus and peer-reviewed journals are included.
Results
A total of thirty-two studies were included in the present study. The result indicates that the median direct cost of diabetes was estimated to be ₹18,890/- p.a. for the north zone, ₹10,585/- p.a. for the south zone, ₹45,792/- p.a. for the north-east zone and ₹8822/- p.a. for the west zone. Similarly, the median indirect cost of diabetes was ₹18,146/- p.a. for the north zone, ₹1198/- p.a. for the south zone, ₹18,707/- p.a. for the north-east and ₹3949/- p.a. for the west zone.
Conclusion
The present study highlighted that diabetes poses a high economic burden on individuals/households. The study directed the need to arrange awareness campaign regarding diabetes and associated risk factors in order to minimise the burden of diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
‘Diabetes is a metabolic disease characterised by hyperglycemia resulting from defects in insulin secretion, insulin action or both’ [1]. With rising pervasiveness globally, diabetes is conceded as a major chronic pandemic disease which does not consider any ethnic background and monetary levels both in developing and developed economies and has also been designated with the status of ‘public health priority’ in the majority of the countries [2, 3]. Individuals with diabetes are more susceptible to develop any of the associated complications, viz. macrovascular or microvascular. As a consequence, people experience frequent and exhaustive confrontation with the health care systems [4]. The treatment cost for diabetes and its associated complications exert an enormous economic burden both at the household and national levels [5,6,7,8,9].
In a developing nation like India, the majority of diabetes patients experience a substantial cost burden from out-of-pocket (OOP). Also, the dearth of insurance schemes and policies escalate the cost of diabetes care [2]. Instantaneous urbanisation and socio-economic transitions, viz. rural to urban migration, low exercise regimen, lifestyle disorder, etc., have resulted in an escalation of diabetes prevalence in India over the last couple of decades [10,11,12,13,14]. According to the International Diabetes Federation [15], ‘India is the epicentre of diabetes mellitus and it was found that in 2017 India had the second-largest populace of 73 million diabetic patients, after China. And the figure is expected to be just double 134 million by 2045’. Considering that fact, the epidemiologic transition of diabetes has a colossal economic burden [16]. The estimated country-level health care expenditure on diabetes mellitus in India after amending purchasing power difference was 31 billion US dollars in 2017, pushing India in fourth place globally after the USA, China and Germany. Looking at the economic burden, in India, diabetes alone exhausts 5 to 25% share of an average Indian household earning [17,18,19].
Chronic nature and the rising epidemic of diabetes have everlasting consequences on the nation’s economy and health status [20]. Therefore, managing diabetes and its comorbidities is a massive challenge in India due to several issues and stumbling blocks, viz. dearth of awareness regarding diabetes, its risk factors, prevention strategies, health care systems, poverty-stricken economy, non-adherence to medicines, etc. Altogether, these issues and problems remarkably contribute to the economic menace of diabetes in India [20,21,22,23,24].
After a perspicuous representation of the economic menace of diabetes in India, policymakers and health experts should provide healthier prospects to enhance the quality of life of millions [19]. Thus, the present study aims at capturing the evidence from the literature on the cost of diabetes mellitus in India, reviewing the materials and methods used to estimate the costs and, lastly, exploring future research area. For the accomplishment of the objective, the paper has been divided into five sections. The ‘Introduction’ section of the study discusses diabetes and its economic burden. The ‘Materials and methods’ section deals with materials and methods applied for data extraction and quality assessment. The ‘Results’ section of the present study reports the results of the study. The ‘Discussion’ section concludes the discussion along with policy implications and limitations.
Materials and methods
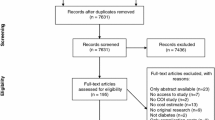
A comprehensive literature review was carried out by following the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines’ [25]. The article suggests a minimum set of guidelines and procedures of writing items to enhance the quality of the systematic review. A search was performed between February and March 2019 for the accumulation and review of studies published up to January 2019.
Literature search
An extensive desk search was executed for all published articles and book chapters in relevant databases such as ACADEMIA, NCBI, PubMed, ProQuest, EBSCO, Springer, ResearchGate, Google Scholar, JSTOR and Scopus. For better insight, a literature search was performed on the World Health Organization (WHO) and International Diabetes Federation (IDF) libraries available online. Additional articles were investigated by scrutinising the backward referencing lists or references of the included articles. The search terms and keywords were adjusted by following different databases using words or phrases, viz. ‘India’, ‘Diabetes Mellitus or Diabetes’, ‘Economic Burden’, ‘Economic Menace’, ‘Costs of Diabetes’, ‘Health Care Utilization’, ‘Cost of Illness’, ‘Out-of-Pocket Expenditure’, ‘Diabetes Care’, ‘Health Economics’, ‘Direct/Indirect Costs’, ‘Cost Analysis’, ‘Hospitalization’, ‘Diabetic Complications’, ‘Developing Countries’, ‘Lifestyle Modification’, ‘Non-communicable diseases’, ‘Expenses by patients’, ‘Comorbidity Burden’ and ‘Treatment Costs’ were utilised to attain expected results. A total of 412 studies were acquired including duplicates by exercising the desk search criteria. Further, a comprehensive analysis of the studies was performed as per the recommendations suggested by Moher et al. [25]. Later, 187 articles were identified to be duplicate and removed immediately.
Inclusion criterion
Of the total 225 articles, limited studies managed to clear the eligibility criterion based upon the significant elements of the ‘Patient Intervention Comparison Outcome Study (PICOS)’ procedure [26]. Title, abstract and keywords of the remaining 225 studies were assessed to determine their relevance. Those articles which have been included (a) were available in English language; (b) were published between 1999 and February 2019; (c) were indexed under ABDC, EBSCO, ProQuest and Scopus; (d) were under journals that are to be peer-reviewed in nature; (e) highlighted unprecedented research outcomes on costs; and (f) were comprising at least one or more demographic zones. Thus, the screening procedure facilitated the selection of 32 articles. Majority of research publications were excluded on the grounds if they (a) did not provide the detailed analysis of how costs were estimated; (b) were conference articles or posters; (c) only presented the costs of diabetes prevention; and (d) were published in non-peer-reviewed journals.
Data extraction and quality assessment of included studies
The exploration includes those articles which highlight the cost burden of diabetes in India. Whilst performing the analysis, two interdependent excel spreadsheets were developed for data to be summarised. In the very first spreadsheet, a predefined category was used, viz. publication title/year, study type, location, diabetes type, methodology and findings. Relevant information is drawn out and presented in Table 1, highlighting the study characteristics of the included articles. The second excel spreadsheet focuses its attention on the list of technical criteria applied to assess the quality of the articles incorporated in the review process. Copious checklist has been put forward for the quality assessment of the included studies and majority of them emphasise on the economic assessment, viz. cost analysis, cost-benefit analysis (CBA), health care utility analysis, etc. [27, 28]. Therefore, the quality indicators developed for the present study were grounded on the criterions suggested by prior literature [29,30,31,32].
A symbol of (√) yes, (×) no and (±) moderately available was assigned to individual quality indicator. Each symbol was allocated with a score of 1, which leads to a maximum attainable score of 10 for each study reviewed. Hence, a complete detailed analysis of the parameters utilised is presented in Table 2.
Results
Study characteristics
The characteristics of the included thirty-two studies are presented in Table 1. A majority of 66% (21) of the studies were published between 2010 and 2019 and the remaining 11 studies (34%) were published in 1999–2009. Year of costing was 1999–2003 for 5 studies; between 2009 and 2013, 10 studies (31%) were included; and for 2014–2019, 12 studies (37%) were included. The cost of diabetes was estimated from various locations such as the south zone (n = 11), followed by the north zone (n = 8), the north-east zone (n = 1) and the west zone (n = 1). A large proportion of 11 studies (34%) were defined under India as a whole.
Whilst conducting review studies, it is imperative to initially define the type, study interest, sample size, data source and outlook of the study. The included studies majorly focus on type 2 diabetes (n = 9), followed by both type 1 and type 2 studies (n = 8), 2 studies were identified under type 1 diabetes and only 1 study was acknowledged under gestational/foot ulcer category, whilst the remaining 12 studies did not define any diabetes type (Table 1). Of the total 32 studies, 94% of studies focus on general costs and the remaining 2 studies emphasise on foot ulcers and others. Whilst discussing the cost interests, the complications associated with diabetes were estimated by merely10 studies and the remaining 22 studies (69%) estimated the diabetes cost without any complications. Defining sample size is the utmost priority of the study, 27 studies (83%) of the total 32 studies have properly identified the sample size to be ≤ 100 respondents, only 2 studies specified the population size to be > 100 respondents and 3 studies (10%) did not define or provide the sample size.
Under the source of the cost data section, 16 studies (50%) retrieved data on cost from the patients themselves; for 11 studies (34%), source of cost data was obtained from medical institutes; and the remaining 5 studies (16%) acquired the data on cost from publications. Studies on the economic burden of illness could be done through several perspectives, viz. household, patient, societal and governmental. In the particular study, the patient’s perspective was most commonly acknowledged by 19 studies (61%), 9 studies considered societal perspective, followed by government perspective for 7 studies and lastly, household perspective was adopted by 6 studies as highlighted in Table 1.
Quality of the reviewed articles
The quality of the included studies is broadly presented in Table 2. For all 32 studies, research questions and findings were discussed and explained in a very well-defined manner. The presentation of the results was completely in synchronisation with the aim and conclusions derived from the reviewed articles. It was found that 60% (19) of the studies have comprehensively defined the epidemiological definition such as type of diabetes (type 1 and type 2). Limitations experienced by the majority of studies that hampered the quality of the reviewed articles were the absence of a broad definition of diabetes and a lack of adequate sample size. A major proportion of 25 studies (78%) did not extensively define diabetes and 18 studies (56%) moderately considered the sample size.
For most of the reviewed articles, the sampling technique for data collection was addressed and only 1 study did not define the sampling technique. However, 56% (18) of studies lucidly defined the tools and technique employed in the reviewed articles and the remaining 14 studies moderately describe the tools and technique. A majority of 27 studies (84%) have properly classified the cost of diabetes and the remaining 5 studies defined moderately. Hence, based on quality index scores, the majority of the studies (n = 11) scored ‘6 Yes’ on a 10-point scale. Interestingly, 5 studies attained a marginally higher score of ‘8 Yes’ of the total 32 studies as presented in Table 2.
Cost of diabetes
The economic burden of diabetes mellitus has led to numerous studies on the cost of illness. The cost exerted by diabetes can be categorised into three groups: direct cost, indirect cost and intangible cost [55, 56]. Direct cost includes both direct health care costs (diagnosis, treatment, care and prevention) and direct non-health care costs (transport, housekeeping, social service and legal cost) [1, 57]. Indirect cost includes cost for absenteeism, loss of productivity and disability [58, 59]. Lastly, intangible costs embrace cost for social isolation and dependence, low socio-economic status, mental health and behavioral disorder and loss of quality of life [56, 60, 61]. All twenty-one reviewed studies put forward data and statistics to evaluate per capita cost of individual/household at zone level and the remaining eleven studies highlighted the cost of diabetes at the national level (Table 3). To have a clear insight on cost, the reviewed articles have been categorised into four different zones, viz. north zone, west zone, south zone and north-east zone.
Under the north zone, 8 studies were included to calculate both direct and indirect costs of diabetes at the individual/household level (Fig. 1). The median direct cost of diabetes is estimated to be ₹18,890/- per annum, ranging from ₹999/- to ₹1,09,344/- [19, 35, 39, 44, 46, 48,49,50]. The most commonly measured costing items under direct cost were expenditure on medicines (7 studies), diagnostic expenses (2 studies), transportation cost (1 study), hospitalisation (2 studies) and consultation fee (3 studies). The median indirect cost of diabetes for the north zone was evaluated to be ₹18,146/- per annum, ranging from ₹4642/- to ₹98,808/- [19, 35, 46, 49]. For all indirect cost studies, costing items, viz. wage loss and leisure time forgone, were used majorly.
South zone includes 11 studies, majorly from Karnataka state (6 studies), followed by Tamil Nadu (4 studies) and Andhra Pradesh (1 study). The median direct cost was assessed to be ₹10,585/-- per annum (Fig. 1), ranging from ₹377/- to ₹21,258/- per annum [2, 6,7,8,9, 33, 37, 38, 40, 42, 45]. Direct costing items, viz. medicine cost (9 studies), consultation fees (4 studies) and hospitalisation (3 studies), were used in the reviewed article. The median indirect cost of diabetes was ₹1198/- per annum, ranging from ₹462/- to ₹3572/- per annum with major cost items such as monitoring cost (1 study), absenteeism (3 studies) and impairment (1 study) [7,8,9, 33, 37].
Under the north-east and west zone, only one-one study was observed, to evaluate the direct and indirect cost of diabetes at the individual/household level [47, 51]. The median direct cost of diabetes for north-east was evaluated to be ₹45,792/- per annum and ₹8822/- per annum was observed for the west zone (Fig. 1). Commonly estimated costing items were surgical procedures, expenditure on drugs/medicines, clinical fees, etc. The median indirect cost estimated for the north-east zone was ₹18,707/- per annum and ₹3949/- per annum was analysed for the west zone. Indirect costing items identified for both reviewed studies were loss of wage, spendings on health class, travelling expenditure and spendings on diet control. Lastly, 11 studies were incorporated to estimate the cost of diabetes for India as a whole at the individual/household level [5, 20, 22,23,24, 34, 36, 43, 51,52,53]. The median direct cost of diabetes for India as a whole was ₹9996/- per annum, ranging from ₹4724/- to ₹25,391/- per annum. Also, the median indirect cost of diabetes at the individual/household level was estimated to be ₹5237/- per annum, ranging from ₹2435/- to ₹12,756/- annually (Figs. 1 and 2).
Complications
Diabetes mellitus is associated with a large number of serious and chronic complications, which act as a major cause of hospitalisation, morbidity and premature mortality in diabetic patients [2, 7, 8, 42]. Diabetes mellitus is commonly associated with chronic complications both macrovascular and microvascular origin [2, 3]. Microvascular complications of diabetes mellitus include retinopathy, autonomic neuropathy, peripheral neuropathy and nephropathy [3, 53]. The macrovascular complication of diabetes mellitus broadly includes coronary and peripheral arterial disease [2, 7]. Of the total reviewed studies, only 10 studies estimated the cost of complications associated with diabetes (Table 3). A couple of studies on diabetes assessed the cost of illness to be 1.4 times higher for individuals with complications as exhibited in Table 3 [8, 52]. A similar study by Sachidananda et al. [42] concluded that the cost of diabetes is 1.8 times higher for complicated non-hospitalised patients and 2.4 times higher for complicated hospitalised patients. Kapur [38] inferred that individuals with three or more comorbidities encounter 48% more cost of care, amounting to ₹10,593/- annually. According to Cavanagh et al. [5], India is the most expensive country for a patient with a complex diabetic foot ulcer, where 68.8 months of income was required to pay for treatment. Three reviewed studies incorporated in the study estimated the cost of individual/household with both macrovascular and microvascular complications [2, 7, 53]. Of these 3 reviewed articles, a couple of them primarily concentrate on the cost of illness prompted by renal (kidney) complication [2, 53]. Lastly, Eshwari et al. [9] estimated the total cost for the treatment of diabetes with comorbidities was ₹9133/- annually. Direct cost with complications was ₹8185/- per annum and indirect cost amounts to be ₹508/- annually.
Discussion
Rising menace of diabetes has been a major concern for India. With a frightening increase in population with diabetes, India is soon going to be crowned as ‘diabetes capital’ of the world. A swift cultural and social alteration, viz. rising age, diet modification, rapid urbanisation, lack of regular exercise regimen, obesity and a sedentary lifestyle, will result in the continuous incidence of diabetes in India. The primary objective of this article is to detect and capture the evidence from published literature on the per capita cost at the individual/household level for both direct and indirect costs of diabetes in India which are available and published since 1999. Of the total 412 records, 32 studies were identified to meet the inclusion criterion. Therefore, the findings of the present study suggest that per annum median direct and indirect cost of diabetes at the individual/household level is very colossal in India.
A large proportion of health care cost is confronted by the patients themselves, which affects the fulfilment of health care because of financial restraints [62]. The proportion of public health expenditure by the Indian government is the lowest in the world. As a consequence, out-of-pocket (OOP) spending constitutes to be 70% of the total health expenditure. Hence, financing and delivering health care facilities in India is majorly catered by the private sector for more than 70% of diseases in both rural and urban areas [24].
Direct cost items (expenditure on medicines, diagnostic expenses, transportation cost, hospitalisation and consultation fee) and indirect cost items (loss of wage, spendings on health class and travelling expenditure) were most commonly reported costing items in the present study [8, 9, 19, 37, 46, 48]. Most of the reviewed studies on the cost of diabetes highlighted expenditure on drugs/medicine as the foremost costing item which accounts for a significant share of all direct costs. The finding of the present study is consistent with Yesudian et al. [62], ‘cost on drugs constitutes 50% of the total direct costs’. The majority of the reviewed articles included in the study justify that the primary cause for such abnormal costs of medicines is the common practice adopted by physicians to prescribe brand-named medicines, rather than generic medicines.
In context to the quality of tools and techniques incorporated by the included studies, a large number of articles (56%) witnessed to acknowledge the standards of tools and techniques. Similarly, the classification of the cost of diabetes was also determined by the majority of reviewed articles (27 articles). But the absence of a comprehensive definition of diabetes and a small size of individuals/households produce dubiousness about the standards or quality of the study. Hence, the limitations experienced by the majority of reviewed articles hampered the quality of the present study. Thus, it is beneficial to develop and suggest standard procedures and framework to conduct a comprehensive and exhaustive study on the cost of diabetes.
Limitations of the study
The present study holds few limitations. Primarily the exclusion of the relevant articles presented as conference papers and those studies published under non-peer-reviewed journals. With the omission of the above literature, some biasness might have been introduced into the review process. Furthermore, the major limitation of the present study is the non-availability of published articles under the central and east zone of India. Also, the studies published under the north-east zone and west zone were only one. Lastly, the heterogeneity in material and methodology used in cost estimation are not analogous. As a consequence, conducting a meta-analysis is not feasible.
Conclusion
The above discussion highlighted a huge economic burden of diabetes in India and variations were recorded in the different zones. It was observed that the cost of drugs/medicines accounts for a major burden of the cost of diabetes. The study suggested few policy interventions to cope with the high economic burden of diabetes. There is a dire need in the country to arrange awareness programmes on diabetes and associated risk factors. The menace of diabetes can be controlled by devising new health care policies, introducing new generic medicines and taxing alcohol/tobacco. Diabetes is a lifestyle disease so along with the above measures, a change in dietary habits, physical activity, beliefs and behavior can reduce its economic burden.
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Supplement 1):S67–74.
Kumpatla S, Kothandan H, Tharkar S, Viswanathan V. The costs of treating long term diabetic complications in a developing country: a study from India. JAPI. 2013;61(1):1–17.
Unnikrishnan R, Anjana RM, Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016;12(6):357–70.
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H, WHO Multinational Study Group. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(2):S14.
Cavanagh P, Attinger C, Abbas Z, Bal A, Rojas N, Xu ZR. Cost of treating diabetic foot ulcers in five different countries. Diabetes Metab Res Rev. 2012;28:107–11.
Shivaprakash G, Nishith RS, Basu A, Shivaprakash P, Adhikari P, Gopalakrishna HN, et al. Dispensing patterns and cost of glucose-lowering therapies in diabetes mellitus patients at a tertiary care hospital in Southern India. Drug Invent Today. 2012;4(12).
Akari S, Mateti UV, Kunduru BR. Health-care cost of diabetes in South India: a cost of illness study. J Res Pharm Pract. 2013;2(3):114–7.
Acharya LD, Rau NR, Udupa N, Rajan MS, Vijayanarayana K. Assessment of cost of illness for diabetic patients in South Indian tertiary care hospital. J Pharm Bioallied Sci. 2016;8(4):314–20.
Eshwari K, Kamath VG, Rao CR, Kamath A. Annual cost incurred for the management of type 2 diabetes mellitus—a community-based study from coastal Karnataka. Int J Diabetes Dev Ctries. 2019;39(3):590–5.
Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes. 2012;3(6):102–10.
Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–80.
Misra R, Misra A, Kamalamma N, Vikram NK, Gupta S, Sharma S, et al. Difference in prevalence of diabetes, obesity, metabolic syndrome and associated cardiovascular risk factors in a rural area of Tamil Nadu and an urban area of Delhi. Int J Diab Dev Ctries. 2011;31(2):82–90.
Dhanaraj S. Economic vulnerability to health shocks and coping strategies: evidence from Andhra Pradesh, India. Health Policy Plan. 2016;31(6):749–58.
Oommen AM, Abraham VJ, George K, Jose VJ. Prevalence of risk factors for non-communicable diseases in rural and urban Tamil Nadu. Indian J Med Res. 2016;144(3):460–71.
International Diabetes Federation: IDF Diabetes Atlas (2017) http://www.idf.org/idf-diabetes-atlas-eight-edition. Accessed Jan 2018.
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Charles AK, Grepstad M, Visintin E, Ferrario A. The economic burden of diabetes in India: a review of the literature. Glob Health. 2014;10(8):2–18.
Holla R, Prabhu S, Shetty S, Deshpande S, Balla S, Hegde S, et al. Awareness about diabetes among adolescents of Mangalore, South India. NUJHS. 2014;4(2):118–20.
Kansra P. Economic burden of diabetes among women: a comparison of outpatient and inpatient care. J Health Manag. 2018;20(3):401–9.
Viswanathan V, Rao VN. Problems associated with diabetes care in India. Diabetes Manag. 2013;3(1):31–40.
Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes. 2009;1(1):18–28.
Tharkar S, Devarajan A, Kumpatla S, Viswanathan V. The socioeconomics of diabetes from a developing country: a population based cost of illness study. Diabetes Res Clin Pract. 2010;89(3):334–40.
Rao KD, Bhatnagar A, Murphy A. Socio-economic inequalities in the financing of cardiovascular and diabetes inpatient treatment in India. Indian J Med Res. 2011;133(1):57.
Tripathy JP, Prasad BM. Cost of diabetic care in India: an inequitable picture. Diabetes Metab Syndr Clin Res Rev. 2018;12(3):251–5.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14(1):579.
Molinier L, Bauvin E, Combescure C, Castelli C, Rebillard X, Soulié M, et al. Methodological considerations in cost of prostate cancer studies: a systematic review. Value Health. 2008;11(5):878–85.
Kleine-Budde K, Touil E, Moock J, Bramesfeld A, Kawohl W, Rössler W. Cost of illness for bipolar disorder: a systematic review of the economic burden. Bipolar Disord. 2014;16(4):337–53.
Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. The Milbank Memorial Fund Quarterly. Health and Society. 1982:429–462.
Rice DP. Cost of illness studies: what is good about them? Inj Prev. 2000;6(3):177–9.
Akobundu E, Ju J, Blatt L, Mullins CD. Cost-of-illness studies. Pharmacoeconomics. 2006;24(9):869–90.
Mutyambizi C, Pavlova M, Chola L, Hongoro C, Groot W. Cost of diabetes mellitus in Africa: a systematic review of existing literature. Glob Health. 2018;14(1):3.
Rayappa PH, Raju KNM, Kapur A, Bjork S, Sylvest C, Kumar KD. Economic cost of diabetes care: the Bangalore urban district diabetes study. Int J Diab Dev Ctries. 1999;19(3):87–6.
Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care. 2007;30(2):252–6.
Grover S, Avasthi A, Bhansali A, Chakrabarti S, Kulhara P. Cost of ambulatory care of diabetes mellitus: a study from north India. Postgrad Med J. 2005;81(956):391–5.
Ramachandran A. Socio-economic burden of diabetes in India. J Assoc Phys India. 2007;55(L):9.
Sharma KM, Ranjani H, Zabetian A, Datta M, Deepa M, Moses CA, et al. Excess cost burden of diabetes in Southern India: a clinic-based, comparative cost-of-illness study. Glob Health Epidemiol Genomics. 2016;1:e8.
Kapur A. Economic analysis of diabetes care. Indian J Med Res. 2007;125(3):473–82.
Joshi A, Mohan K, Grin G, Perin DMP. Burden of healthcare utilization and out-of-pocket costs among individuals with NCDs in an Indian setting. J Community Health. 2013;38(2):320–7.
Shobhana R, Rao PR, Lavanya A, Williams R, Vijay V, Ramachandran A. Expenditure on health care incurred by diabetic subjects in a developing country—a study from southern India. Diabetes Res Clin Pract. 2000;48(1):37–42.
Chandra P, Gogate B, Gogate P, Thite N, Mutha A, Walimbe A. Economic burden of diabetes in urban Indians. Open Ophthalmol J. 2014;8:91–4.
Sachidanandaa A, Geok Linc J, Ushab A. Health care cost incurred by patients of diabetes mellitus in a tertiary care hospital setting in Coastal Karnataka district. J Glob Pharm Technol. 2010;2(6):8–12.
Bjork S, Kapur A, King H, Nair J, Ramachandran A. Global policy: aspects of diabetes in India. Health Policy. 2003;66(1):61–72.
Kumar A, Nagpal J, Bhartia A. Direct cost of ambulatory care of type 2 diabetes in the middle and high income group populace of Delhi: the DEDICOM survey. JAPI. 2008;56:667–74.
Shobhana R, Rao PR, Lavanya A, Williams R, Padma C, Vijay V, et al. Costs incurred by families having type 1 diabetes in a developing country—a study from southern India. Diabetes Res Clin Pract. 2002;55(1):45–8.
Thakur A, Ray TK, Goel MK. Expenditure pattern on diabetes care: a community based longitudinal study in resettlement colony of East Delhi. Indian J Community Health. 2017;29(2):209–12.
Khongrangjem T, Phadnis S, Kumar S. Cost of illness (COI) of type-II diabetes mellitus in Shillong, Meghalaya. Int J Diabetes Dev Ctries. 2019;39(1):201–5.
Singla R, Bindra J, Singla A, Gupta Y, Kalra S. Drug prescription patterns and cost analysis of diabetes therapy in India: audit of an endocrine practice. Indian J Endocrinol Metab. 2019;23(1):40–5.
Kumar D, Mukherjee K. Economic impact of type-2 diabetes mellitus on households in Hisar district of Haryana state, India. 2014.
Katam KK, Bhatia V, Dabadghao P, Bhatia E. High direct costs of medical care in patients with type 1 diabetes attending a referral clinic in a government-funded hospital in northern India. Natl Med J India. 2016;29(2):64–7.
Bjork S, Kapur A, Sylvest C, Kumar D, Kelkar S, Nair J. The economic burden of diabetes in India: results from a national survey. Diabetes Res Clin Pract. 2000;50:190.
Tharkar S, Satyavani K, Viswanathan V. Cost of medical care among type 2 diabetic patients with a co-morbid condition—hypertension in India. Diabetes Res Clin Pract. 2009;83(2):263–7.
Satyavani K, Kothandan H, Jayaraman M, Viswanathan V. Direct costs associated with chronic kidney disease among type 2 diabetic patients in India. Indian J Nephrol. 2014;24(3):141–7.
Oberoi S, Kansra P. Factors influencing medical tourism in India: a critical review. SAMVAD. 2019;17:9–16.
Pagano E, Brunetti M, Tediosi F, Garattini L. Costs of diabetes. Pharmacoeconomics. 1999;15(6):583–95.
Sobocki P, Lekander I, Borgstrom F, Strom O, Runeson B. The economic burden of depression in Sweden from 1997 to 2005. Eur Psychiatry. 2007;22(3):146–52.
Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26(3):917–32.
Herwaldt A, Cullen J, Scholz D, French P, Zimmerman B, Pfaller M, et al. A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol. 2006;27(12):1291–8.
Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multi- morbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–23.
Beran RG. The burden of epilepsy for the patient: the intangible costs. Epilepsia. 1999;40(8):40–3.
Rodwin BA, Spruill TM, Ladapo JA. Economics of psychosocial factors in patients with cardiovascular disease. Prog Cardiovasc Dis. 2013;55(6):563–73.
Yesudian CA, Grepstad M, Visintin E, Ferrario A. The economic burden of diabetes in India: a review of the literature. Glob Health. 2014;10(1):80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study is a review-based study, so it does not contain any studies with animals. The present study only reviews those studies which contain individual’s performance.
Informed consent
For the present study, it is not necessary to obtain any consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(XLSX 61 kb)
Rights and permissions
About this article
Cite this article
Oberoi, S., Kansra, P. Economic menace of diabetes in India: a systematic review. Int J Diabetes Dev Ctries 40, 464–475 (2020). https://doi.org/10.1007/s13410-020-00838-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00838-z