Abstract
Purpose
Non-invasive high-grade (HG) bladder cancer is a heterogeneous disease that is characterized insufficiently. First-line Bacillus Calmette-Guérin instillation fails in a substantial amount of cases and alternative bladder-preserving treatments are limited, underlining the need to promote a further molecular understanding of non-invasive HG lesions. Here, we characterized pure HG papillary urothelial bladder cancer (pure pTa HG), a potential subgroup of non-invasive HG bladder carcinomas, with regard to molecular subtype affiliation and potential for targeted therapy.
Methods
An immunohistochemistry panel comprising luminal (KRT20, ERBB2, ESR2, GATA3) and basal (KRT5/6, KRT14) markers as well as p53 and FGFR3 was used to analyze molecular subtype affiliations of 78 pure pTa HG/papillary pT1(a) HG samples. In 66 of these, ERBB2 fluorescence in situ hybridization was performed. Additionally, targeted sequencing (31 genes) of 19 pTa HG cases was conducted, focusing on known therapeutic targets or those described to predict response to targeted therapies noted in registered clinical trials or that are already approved.
Results
We found that pure pTa HG/papillary pT1(a) HG lesions were characterized by a luminal-like phenotype associated with frequent (58% of samples) moderate to high ERBB2 protein expression, rare FGFR3 alterations on genomic and protein levels, and a high frequency (89% of samples) of chromatin-modifying gene alterations. Of note, 95% of pTa HG/papillary pT1 HG cases harbored at least one potential druggable genomic alteration.
Conclusions
Our data should help guiding the selection of targeted therapies for investigation in future clinical trials and, additionally, may provide a basis for prospective mechanistic studies of pTa HG pathogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Bladder cancer (BC) is the most common malignancy of the urinary tract with an estimated number of 380,000 new cases and 150,000 deaths per year worldwide [1]. In Europe and North America more than 90% of diagnosed bladder cancers are urothelial carcinomas [2]. The majority of BC patients present with non-invasive, low-grade papillary carcinomas (pTa LG), characterized by frequent FGFR3 gene alterations and a good prognosis (5-year survival of ~ 90%). Although frequently recurring, these tumors only infrequently progress to muscle-invasive disease. In contrast, muscle-invasive bladder cancer (MIBC) has an unfavorable prognosis (5-year survival < 50%) and a high risk of progression to metastasis [2]. MIBC mainly arises via carcinoma in situ (CIS), a flat high-grade (HG) lesion characterized by TP53 mutations, and papillary lesions of HG (pTa HG) [2, 3]. The conventional model postulates development of pTa HG from pTa LG lesions [2]. Based on our observations and those made by others [4], we hypothesize that a subgroup of non-invasive pTa HG lesions arises de novo (i.e., without a LG history). The AUA/SUO (American Urological Association/Society of Urologic Oncology) and the EAU (European Association of Urology) guidelines for non-MIBC (NMIBC) strongly recommend an essentially uniform therapy for HG NMIBC: Intravesical instillation of BCG (Bacillus Calmette-Guérin) post transurethral resection of the bladder tumor (TURBT) or after confirmative re-TURBT, respectively, is the recommended first-line treatment, whereas radical cystectomy (RC) should be considered in case of BCG failure or in first-line for the subgroup of highest risk tumors [5, 6]. BCG failure is observed in a significant portion of patients [7] and even though early RC is associated with an excellent tumor-specific survival [8], not all patients are eligible for this aggressive treatment or refuse RC [9]. In sum, there is an unmet need for effective bladder-preserving alternative therapies in addition to BCG for high-risk NMIBC.
In this study and related work [10, 11], we aimed to further understand the heterogeneous group of non-invasive urothelial HG lesions as they are understudied compared to MIBC [12]. In the present study, a cohort of pure pTa HG/papillary pT1(a) HG tumors was established and analyzed with regard to molecular subtype affiliation using an established panel of luminal (KRT20, GATA3, ERBB2, ESR2) and basal (KRT5/6, KRT14) immunohistochemical markers recently used to characterize urothelial CIS [10]. Additionally, a targeted sequencing panel (recently described [11]) was applied on the pTa HG lesions, focusing on genetic alterations (GAs) in genes either encoding known therapeutic targets or genes described to predict response to targeted therapies noted in registered clinical trials or already FDA/EMA-approved. Combined with data obtained by analogous investigations on urothelial CIS, this study aims to further dissect differences and similarities within the heterogeneous group of non-invasive urothelial HG lesions that might be of relevance for therapy stratification.
2 Materials and methods
2.1 Patients
It is accepted that HG papillary carcinomas may arise from LG papillary lesions [2]. Based on our own observations and those made by other groups [4] we hypothesize that a subgroup of HG papillary lesions might develop “de novo” without a preceding LG component. We carefully selected a cohort of patients presenting with HG papillary urothelial BC without a history of previous or concomitant pTa LG or MIBC lesions. In two cases, a LG lesion was simultaneously present at a localization in the bladder distinctly different from the pTa HG tumor. Our retrospective immunohistochemistry (IHC) cohort comprised 78 samples from 48 patients (44 pTa HG, 34 papillary pT1(a) HG samples) treated at the RWTH Aachen University and the LMU Munich University Hospitals between 2012 and 2018 (Online Resources 1 and 2). To analyze the stability of IHC marker expression in the course of progression, we compared marker expression in matched pairs of exophytic papillary HG cancer to concomitant stroma-invasive tumor areas in 32 biopsies from 20 patients (Online Resource 1). To study the presence of GAs with potential impact on targeted therapy response, targeted sequencing was conducted in 23 samples from 23 patients, comprising 16 pTa HG/papillary pT1 HG tumor specimens without a history of pTa LG/MIBC lesions, three papillary pT1 HG samples with a history of pTa LG or muscle-invasive disease (Online Resource 3) and four normal smooth muscle specimens as controls. An experienced pathologist (RK) confirmed the diagnosis of each patient by reviewing corresponding histological samples.
2.2 Immunohistochemistry
We used formalin-fixed, paraffin-embedded (FFPE) tissues to create tissue microarrays (TMAs). These TMAs were generated using one to five punches per sample if available to consider potential tumor heterogeneity. Negative and positive staining controls were included on all TMAs. TMA sections (2 µm) were incubated in antigen retrieval solution PT Link (Dako, Agilent, Santa Clara, California) of pH 6 (KRT14, KRT20, GATA3, ERBB2, FGFR3) and pH 9 (KRT5/6, ESR2, p53) at 95 °C for deparaffinization, rehydration and epitope retrieval. Next, slides were transferred to an automated immunostainer (Dako, Agilent) and covered with EnVision™ Flex Peroxidase Blocking-Reagent (Dako, Agilent) for five minutes to block endogenous peroxidase activity. Immunostaining was performed with antibodies specific for KRT20, GATA3, ESR2, ERBB2, KRT5/6, KRT14, p53 and FGFR3. Subsequently, tissue sections were treated with a secondary reagent (Dako, Agilent) for 15 min, followed by incubation with a horseradish peroxidase-conjugated polymer (Dako, Agilent) for 20 min. Visualization of staining was accomplished using a DAB + Substrate Chromogen System (Dako, Agilent). Finally, the TMAs were counterstained using Mayer’s hematoxylin.
Immunohistochemical staining was assessed by an experienced pathologist (RK) blinded to patient identity. The percentage of positively stained cells was evaluated for the cytoplasmic markers KRT20, KRT5/6, KRT14 and nuclear p53. Cases were considered positive for cytokeratin expression if > 50% of cells showed positivity for the respective marker. Aberrant p53 expression was assumed if either 100% of cells showed intense nuclear staining or in case of complete absence of nuclear staining (null phenotype) [13]. ESR2 and GATA3 status was assessed using an adapted semi-quantitative immunoreactive scoring system described by Remmele and Stegner [14], multiplying a score for nuclear staining intensity (from 0 to 3) with a score expressing the percentage of stained cells (from 0 to 4). A Remmele score ranging from 3 to 12 was considered “positive” as described recently [10]. The Dako score was used to quantify ERBB2 protein expression, combining staining intensity and the percentage of positive cells: 0–1 (negative), 2 (moderate) and 3 (positive, overexpressed) [15]. FGFR3 protein expression was assessed using a semi-quantitative score (0–3) recently described [16].
2.3 Fluorescence in situ hybridization (FISH)
FISH analysis was applied in order to correlate ERBB2 protein expression with the genomic ERBB2 gene status using a ZytoLight SPEC ERBB2/CEN17 Dual Color Probe kit (Zytovision, Bremerhaven, Germany) on 66 pure pTa HG/papillary pT1(a) HG samples with available ERBB2 protein expression data (Online Resource 2). Concerning the stroma-invasive specimens, only the exophytic tumor area was considered. The test is based on the use of two fluorescently labeled oligonucleotide probes, one specifically binding to a centromeric region of chromosome 17 (CEN17) (ZyOrange) and the other targeting a sequence within the ERBB2 gene locus on chromosome 17 (ZyGreen). The assay was conducted in accordance with the manufacturer’s instructions: FFPE tissue sections (2 µm) were dried (60 °C, overnight), followed by deparaffinization, rehydration and incubation in pretreatment buffer (98 °C for 20 min). Next, pepsin digestion (37 °C for 10 min) was performed preceding the application of ERBB2/CEN17-specific probes. Subsequently, complementary target DNA and FISH probes were co-denatured at 75 °C and allowed to hybridize at 37 °C overnight. After stringent washing and DAPI counterstaining, hybridized probes were visualized by fluorescence microscopy. Thirty tumor nuclei were assessed per case and a mean ratio of green (ERBB2) over red (CEN17) hybridization signals was calculated. Tumor samples were classified as “amplified” (ratio ≥ 2.2) and polysomic (polysomy 17; > 3 CEN17 signals per nucleus) according to commonly applied thresholds [17].
2.4 Library preparation and targeted sequencing
In order to analyze the presence of therapeutically relevant genetic alterations in a cohort of 16 pure pTa HG/papillary pT1 HG tumor specimens and three papillary pT1 HG samples with a history of LG or muscle-invasive disease from altogether 19 patients (Online Resource 3), targeted sequencing was conducted. Four normal smooth muscle specimens from four individuals without a known cancer disease served as control samples. For NGS analysis only the exophytic tumor areas were considered. The target gene panel (recently described [11]) comprised genes frequently affected in MIBC [18] and was primarily focussed on potentially druggable alterations in genes described to predict response to targeted therapies that are FDA/EMA-approved or that are in registered clinical trials (Online Resource 4). Deparaffinized tissue sections (10 µm) were prepared and target tissue material was carefully dissected. Following proteinase K (Promega, Madison, Wisconsin) digestion of isolated cell material (37 °C, overnight), DNA isolation was carried out with a Maxwell 16 instrument (Promega) using the Maxwell 16 FFPE tissue LEV DNA purification Kit (Promega). DNA was subsequently quantified using a Qubit fluorometric assay (Thermo Fisher Scientific, Waltham, Massachusetts). The quality of the isolated DNA was assessed using a TruSeq FFPE DNA Library Prep QC kit (Illumina, San Diego, California). Library preparation was performed using a TruSeq Costum Amplicon Low Input kit (Ilumina) according to the manufacturer’s instructions. In brief, 60–100 ng DNA was used for hybridization to the custom oligonucleotide pools. In order to improve sequence data validity, a dual strand sequencing protocol enabling analysis of both complementary DNA strands was applied. Normalized libraries were sequenced on a NextSeq 500 platform (Illumina) using a NextSeq 500/550 Mid Output kit (2 × 150 cycles) (Illumina). SNV analysis was performed using Sequence Pilot Software version 4.4 (SeqNext module, JSI medical systems, Ettenheim, Germany). For SNV analysis over 97% of bases had a coverage of at least 300x in the analyzed regions of interest for all samples. Missense and silent variants with an allele frequency > 2% in the normal population (according to “1000 genomes” (http://www.internationalgenome.org/; Nov 05, 2019) or “dbSNP v153” (https://www.ncbi.nlm.nih.gov/snp; Nov 05, 2019)) as well as non-splicing-relevant silent and intronic variants in general were considered “non-pathogenic”. Additionally, missense and UTR variants annotated as “benign” or “likely benign” in ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/; Nov 05, 2019) were also excluded. The TERT gene promoter was checked for two known recurrent mutations c.-124C > T and c.-146C > T. The variant allele frequency cut-off was set to 5%. As reference genome for panel design hg19 was used, whereas hg38 served as reference genome for annotation of mutations. A recently developed in-house algorithm, based on an exponential growth model for amplification of PCR products, was applied for CNV analysis. For every gene analyzed for CNVs, at least 10 amplicons were included in the panel design. Coverage data were normalized and amplicon clustering, based on the PCR efficiency among all samples, was performed (for each amplicon). Genes were considered exhibiting a CNV if ≥ 30% of the amplicons of a gene were recognized as outliers in the majority of the five response models built within a cluster. The underlying reference genome for the panel design was hg19. The raw sequencing data of this study are deposited in the NCBI Sequence Read Archive (SRA) version 2.15.0 (https://www.ncbi.nlm.nih.gov/sra; Nov 05, 2019): accession no. PRJNA591851.
2.5 Statistical analysis
Differential expression of luminal and basal protein markers in matched pairs of exophytic and stroma-invasive tumor areas of pure papillary pT1(a) HG carcinomas was assessed using the Wilcoxon matched-pairs signed rank test in GraphPad Prism 7.0 (GraphPad Software, San Diego, California). In order to correlate ERBB2 genomic FISH and ERBB2 protein expression data, as well as cytokeratin expression, a two-tailed Fisher’s exact test was conducted applying SPSS Statistics software version 20.0 (IBM, Armonk, New York). For all analyses the level of significance was set to p < 0.05.
3 Results
3.1 Phenotypic characterization of papillary high-grade bladder cancer
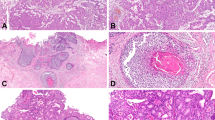
In order to analyze the molecular subtype affiliation of pure pTa HG/papillary pT1(a) HG tumors, extensively studied for MIBC recently [18, 19], protein expression of luminal (KRT20, ERBB2, ESR2, GATA3) and basal markers (KRT5/6, KRT14), as well as of p53 and FGFR3, was examined in a cohort of 78 samples (44 pTa HG and 34 papillary pT1(a) HG samples) from 48 patients (Online Resources 1 and 2). For stroma-invasive papillary HG samples, only expression in exophytic tumor areas was considered. The results are summarized in Table 1 and compared to marker expression recently described for urothelial CIS [10]. Representative images for IHC marker expression in pure pTa HG specimens and exophytic tumor areas of pure papillary pT1(a) HG samples, respectively, are shown in Fig. 1. We found that the majority of samples exhibited positivity for luminal markers: in 74% (58/78) of the samples an aberrant positivity for KRT20 was observed and 99% (77/78) of the samples were scored as “positive” for GATA3 expression. Additionally, positive staining for ESR2 was noted in 96% (75/78) and ERBB2 overexpression (Dako score 3) was observed in 28% (22/78) of the samples. In contrast, the majority of specimens lacked expression of basal markers: 3% (2/78) and 9% (7/78) stained positive for the basal cytokeratins KRT5/6 and KRT14, respectively. A correlation of luminal and basal cytokeratin expression is shown in Online Resource 5. Aberrant p53 expression was detected in 35% (27/78), whereas high FGFR3 protein expression was observed in 10% (7/72) of the samples. Taken together, we found that pure pTa HG/papillary pT1(a) HG carcinomas are characterized by a luminal-like IHC-based phenotype, comparable to that observed for urothelial CIS.
Immunohistochemical detection of luminal and basal marker expression in pure pTa HG and papillary pT1(a) HG specimens. Photographs are representative of median protein expression observed (except for p53). Aberrant KRT20 expression (a). ERBB2 Dako score 2 (b). ESR2 Remmele score 12 (c). GATA3 Remmele score 12 (d). KRT5/6 negativity in tumor cells, positivity limited to basal urothelial cells (e). KRT14 negative tumor cells (f). Aberrant p53 expression (35% of samples; null phenotype not shown) (g). FGFR3 negativity (h). Scale bar: 50 µm
Recently, a potential switch from luminal to basal marker expression during stromal invasion of urothelial CIS was noted [10]. When comparing the expression of the above mentioned marker proteins (except for p53) in matched pairs (n = 32 biopsies from 20 patients) of exophytic and concomitant stroma-invasive tumor areas (Online Resource 1), no significant difference in the expression of marker proteins, except for a reduction in KRT20 protein expression in the stroma-invasive tumor area (p < 0.01), was noted (Online Resource 6).
3.2 ERBB2 fluorescence in situ hybridization of papillary high-grade tumors
To correlate protein expression levels of the known therapeutic target ERBB2 with potential underlying ERBB2 locus amplification or polysomy 17, ERBB2 fluorescence in situ hybridization was performed in 66 pure pTa HG and pure papillary pT1(a) HG samples (Online Resource 2). Concerning stroma-invasive specimens, only the exophytic tumor part was considered. A polysomy 17 was observed in 17% (11/66) and ERBB2 gene locus amplification in 5% (3/66) of the specimens. Although no statistically significant correlation between ERBB2 protein expression (Dako score 0,1 + vs. 2+, 3+) and the presence of ERBB2 amplification or polysomy 17 (neutral vs. AMP/Poly 17) was observed (two-tailed Fisher’s exact test: p = 0.073), we noted that all ERBB2-amplified specimens showed ERBB2 protein overexpression (Dako 3+) (Table 2; Fig. 2).
ERBB2 fluorescence in situ hybridization analysis (n = 66 samples). Neutral (non-amplified, non-polysomic for chromosome 17) (a), polysomy 17 (b), ERBB2 amplification (c), distribution of ERBB2-amplified, chromosome 17 polysomic and neutral samples among the ERBB2 Dako score groups “0/1”, “2” and “3” (d). Red hybridization signals indicate the centromeric region of chromosome 17 (CEN17), green signals localize to the ERBB2 gene locus on chromosome 17
3.3 Potentially actionable genomic alterations in papillary high-grade bladder cancer
Next, we applied a targeted sequencing panel that was recently used to characterize urothelial CIS [11], focusing on genetic alterations (GAs) in genes either encoding known therapeutic targets or that are described to predict response to targeted therapies (currently in registered clinical trials or FDA/EMA-approved). The tissue cohort comprised 19 FFPE tumor biopsies, each sample taken from an individual bladder cancer patient (16 pure pTa HG/papillary pT1 HG tumor specimens and three samples from cases with a history of LG or MIBC disease), and four normal smooth muscle control specimens from patients without a history of cancer (Online Resource 3). For targeted NGS analysis only the exophytic tumor areas were used.
Analysis of mutations and CNVs in 31 genes (Online Resource 4) revealed 96 genetic alterations in total, including multiple aberrations per gene in a given sample. On average, pTa HG/papillary pT1 HG samples harbored 5.1 alterations (range: 1–13) (Online Resources 7 and 8). Affected genes per patient are summarized in Fig. 3. TERT gene promoter mutations, detected in 63% (12/19) of the cases, were identified to be the most frequent GAs in our analysis (Fig. 3). Moreover, in 5% (1/19) of the cases TERT gene amplification was observed. Genes encoding chromatin-modifying proteins (KDM6A, ARID1A, CREBBP, EP300, SMARCA4) were impacted with a frequency of 89% (17/19) of the cases, followed by 63% (12/19) of specimens harboring at least one mutation in genes of the PI3K/MAPK pathway (PIK3CA, ERBB2, FGFR3, NF1, AKT2). Moreover, DNA damage response (DDR) genes (ATM, ERCC2, BRCA2, BRCA1) and genes of the TP53/cell cycle pathway (TP53, CCNE1, MDM2, CDKN1A, CDKN2A, FBXW7) exhibited variants in 47% (9/19) of pTa HG/papillary pT1 HG specimens, respectively.
86% (83/96) of all alterations were considered “potentially actionable” using targeted therapies, including variants of yet unknown significance in genes with predictive potential (Online Resources 7 and 8). On average, 4.4 potentially actionable alterations were detected per patient (range: 0–13) and 95% (18/19) of pTa HG/papillary pT1 HG cases exhibited at least one alteration in genes potentially impacting the selection of targeted therapies. Frequently impacted genes found in pTa HG/papillary pT1 HG cases that were considered “potentially actionable” and related potential targeted therapies are summarized in Fig. 4.
Potentially actionable mutations detected in pTa HG/papillary pT1 HG samples and suggested targeted therapy. Impacted pathways and frequency of cases exhibiting at least one potentially actionable alteration in the respective pathway (upper part). The three most frequently affected genes of each pathway are depicted. Potential targeted therapies are shown (lower part)
4 Discussion
Non-invasive urothelial HG bladder cancer constitutes a heterogeneous group of tumors (i.e., flat urothelial CIS and pTa HG lesions [2]) that is characterized insufficiently [12]. Bladder-preserving treatment options in addition to intravesical BCG instillation are limited and reliable prognostic markers are lacking [5], underlining the need to specifically promote molecular understanding of non-invasive HG lesions. A carefully diagnosed non-invasive state is the best justification for local and bladder-preserving therapy since the chance of metastasis has not yet been taken into account. In the present study, we distinctly selected a cohort of pure pTa HG/papillary pT1(a) HG tumors, a potential subgroup of pTa HG carcinomas without a history of previous or concomitant pTa LG or MIBC disease.
First, we aimed to analyze this putative subgroup with regard to molecular bladder cancer subtype affiliation described for MIBC [18], applying an immunohistochemistry (IHC) panel recently used to characterize urothelial CIS [10]. The majority of pure pTa HG/papillary pT1(a) HG samples exhibited a luminal-like phenotype, i.e., positivity for KRT20 and a lack of basal cytokeratin (KRT5/6 and KRT14) expression in tumor cells. This phenotype is comparable to that observed for urothelial CIS [10] and in accordance with recent studies in NMI urothelial papillary carcinomas of the urinary bladder [20] and the upper tract [21], describing an association between a luminal-like phenotype and high tumor cell grade. Importantly, a luminal-like phenotype has been correlated with unfavorable patient outcome in NMIBC [22,23,24] and NMI urothelial papillary cancer of the upper tract [21, 25], in contrast to observations made in MIBC [18]. As no follow-up data were available for the here analyzed, carefully selected patient cohort, it will be interesting to see in upcoming studies if luminal-like pure pTa HG tumors are indeed associated with a worse prognosis compared to non-luminal cases within this subgroup.
The here studied pTa HG/papillary pT1 HG samples and unselected pTa HG specimens of a recently published reference cohort [26] exhibited a similar pattern of alteration frequencies in the analyzed genes. Remarkably, pTa HG/papillary pT1 HG tumors in the present study and the reference cohort showed a high frequency of alterations in genes encoding chromatin-modifying proteins, including KDM6A, ARID1A, EP300 and CREBBP, which is in line with a recent report analyzing a mixed cohort of urothelial papillary bladder cancers of low and high grade [27]. Notably, pTa HG/papillary pT1 HG samples in this study showed a lower alteration rate in the FGFR3 (16% vs. 59%) and CDKN2A (5% vs. 22%) genes compared to unselected pTa HG lesions [26]. In accordance with this observation, a low rate (7/72; 10%) of high FGFR3 protein expression was noted in the present study. Alterations in FGFR3 and CDKN2A have been shown to co-occur [28] and to be implicated in the conventional Ta developmental pathway, whereby Ta HG tumors evolve from precedent LG lesions [2]. Of note, a recent study suggested CDKN2A deletions to appear prior to grade progression in Ta LG lesions [29]. The observed reduction in FGFR3 mutational frequency in unselected pTa HG lesions (59%) compared to pTa LG lesions (~ 70–80%) [26, 30] may be explained by a putative higher rate of grade progression in LG cell clones without FGFR3 alterations compared to those harboring FGFR3 mutations and/or a putative separate developmental pathway of Ta HG lesions. Interestingly, a recent study found that the same FGFR3 mutations were detectable in LG and adjacent HG areas of the same tumors [29], suggesting grade progression of FGFR3-mutated cell clones. Of note, one of the three here analyzed FGFR3-mutated samples (patient ID 52, harboring the only CDKN2A deletion in the cohort) was known to have a LG history. In future studies it will be interesting to corroborate these data by analyzing FGFR3 mutational frequencies in larger cohorts of pure pTa HG without LG and MIBC history and also by including papillary bladder cancers with grade heterogeneity.
Papillary HG tumors and CIS are concurrently diagnosed in a substantial portion of patients [26]. In this and a preceding study in urothelial CIS [11], we aimed to identify GAs having the potential to guide investigation of targeted therapies in future clinical trials in high-risk NMIBC. In contrast to CIS, the here analyzed pTa HG/papillary pT1 HG samples were characterized by a higher mutational rate in PI3K/MAPK pathway genes (63% vs. 36%), mainly due to a higher mutational frequency in the PIK3CA and FGFR3 genes [11]. Of note, FGFR1 amplifications were exclusively found in CIS specimens [11]. Moreover, CIS samples exhibited a higher mutational rate in genes of the TP53/cell cycle pathway compared to pTa HG/papillary pT1 HG lesions (72% vs. 47%), mainly due to differences in the alteration frequencies of TP53 and CCND1 [11]. These observations are in accordance with the accepted model of a distinct development of papillary bladder cancer and CIS [2]. Both, pTa HG/papillary pT1 HG tumors in this study and CIS specimens were characterized by a high proportion of alterations in chromatin-modifying genes (89% and 68%), with a significantly higher percentage of KDM6A alterations in pTa HG/papillary pT1 HG tumors [11]. Additionally, both lesions exhibited frequent alterations in DDR genes, with CIS lesions showing a higher mutational rate in homologous recombination (HR)-related genes (BRCA1, BRCA2, ATM), whereas pTa HG/papillary pT1 HG lesions specifically exhibited a high frequency of ERCC2 mutations [11].
Of note, 95% of the analyzed pTa HG/papillary pT1 HG samples in this study exhibited at least one GA potentially predicting response to targeted therapy. Shared (in pTa HG/papillary pT1 HG and CIS) frequent alterations in the chromatin-modifying genes KDM6A, ARID1A, CREBBP and EP300 should encourage clinical testing of inhibitors of EZH2 [31], PARP [32] and EP300/CREBBP bromodomain [33] for high-risk NMIBC, having either entered clinical trials (https://clinicaltrials.gov/; Oct 25, 2019; NCT03854474, NCT03568656) or being (in the case of PARP inhibitors) FDA-approved. Likewise, the high percentage of alterations in the HR-related BRCA2, ATM and BRCA1 genes in both HG entities [11] underlines the potential of PARP inhibitors [34]. As suggested recently for urothelial CIS [10, 11], anti-ERBB2 therapy, especially the use of antibody-drug conjugates (e.g. T-DM1), might be a rational therapy for high-risk NMIBC. A substantial portion of both lesions exhibited moderate to strong positivity for ERBB2 protein (58% and 65% of samples), mutations including known pathogenic variants as well as polysomy 17 and, less frequently, ERBB2 amplifications. Although TP53 mutations are more frequent in CIS [2], a significant portion (~ 20%) of pTa HG/papillary pT1 HG tumors in this study and a recent work [26] harbored alterations in this gene. As suggested for urothelial CIS [11], TP53-mutated pTa HG tumors might also be vulnerable to WEE1/CHEK1 inhibition [35, 36]. Additionally, MDM2 amplifications were detected in a similar limited fraction of CIS [11] and the here analyzed pTa HG/papillary pT1 HG samples (~ 10–15%), justifying testing of MDM2 inhibitors in clinical trials. PIK3CA, one of the top mutated genes (37%) found in this study, is impacted in a limited percentage (12%) of CIS specimens [11] as well. FDA-approved PI3K inhibitors are thus assumed to be highly effective in targeting pTa HG/papillary pT1 HG and, to a lesser extent, CIS cells [37]. In addition to targeted strategies potentially impacting flat and papillary HG lesions, actionable GAs being more specific for pTa HG/papillary pT1 HG lesions were also identified. These included GAs in FGFR3, CCNE1, and NF1 that might be predictive of response to FGFR [38], CDK2 [39] and MTOR inhibitors [40]. Remarkably, a high frequency of ERCC2 (32%) mutations was detected as noted recently [26] that have been found to be associated with an improved response to platinum chemotherapy in advanced urothelial carcinoma [41].
Larger-scale studies are needed to validate these preliminary findings, also by including papillary lesions with grade heterogeneity. NMI urothelial HG lesions frequently co-occur in the urinary bladder of the same patient and it will be important to analyze if the here identified potentially actionable GAs are detectable in concurrent NMI HG lesions of the same patients. Moreover, due to our primary motive of identifying therapy targets, matched control samples were not included for pTa HG/papillary pT1 cases and a certain discrimination of germline and somatic variants was thus not possible.
In summary, non-invasive, pure high-grade papillary urothelial bladder cancers, characterized by a luminal-like phenotype, a low FGFR3/CDKN2A alteration frequency and a high rate of mutations in genes encoding chromatin-modifying proteins, harbor at least one potentially actionable GA in the majority of cases. Our previous similar findings in CIS encourage the idea of new strategies for bladder-preserving therapy. The data presented should help guiding the selection of targeted therapies that should be investigated in future clinical trials.
References
J. Ferlay, H.-R. Shin, F. Bray, D. Forman, C. Mathers, D.M. Parkin, Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 127, 2893–2917 (2010)
M.A. Knowles, C.D. Hurst, Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat. Rev. Cancer 15, 25–41 (2015)
H.W. Herr, Tumor progression and survival of patients with high grade, noninvasive papillary (TaG3) bladder tumors: 15-year outcome. J. Urol. 163, 60–61 (2000)
H.A. Al-Ahmadie, G. Iyer, M. Janakiraman, O. Lin, A. Heguy, S.K. Tickoo, S.W. Fine, A. Gopalan, Y. Chen, A. Balar, J. Riches, B. Bochner, G. Dalbagni, D.F. Bajorin, V.E. Reuter, M.I. Milowsky, D.B. Solit, Somatic mutation of fibroblast growth factor receptor-3 (FGFR3) defines a distinct morphological subtype of high-grade urothelial carcinoma. J. Pathol. 224, 270–279 (2011)
M. Babjuk, M. Burger, E.M. Compérat, P. Gontero, A.H. Mostafid, J. Palou, B.W.G. van Rhijn, M. Rouprêt, S.F. Shariat, R. Sylvester, R. Zigeuner, O. Capoun, D. Cohen, J.L.D. Escrig, V. Hernández, B. Peyronnet, T. Seisen, V. Soukup, European Association of Urology guidelines on non-muscle-invasive bladder cancer (TaT1 and carcinoma in situ) – 2019 Update. Eur. Urol. 76, 639–657 (2019)
S.S. Chang, S.A. Boorjian, R. Chou, P.E. Clark, S. Daneshmand, B.R. Konety, R. Pruthi, D.Z. Quale, C.R. Ritch, J.D. Seigne, E.C. Skinner, N.D. Smith, J.M. McKiernan, Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO Guideline. J. Urol. 196, 1021–1029 (2016)
T.K. Nykopp, J. Batista da Costa, M. Mannas, P.C. Black, Current clinical trials in non-muscle invasive bladder cancer. Curr. Urol. Rep. 19, 101 (2018)
H.W. Herr, P.C. Sogani, Does early cystectomy improve the survival of patients with high risk superficial bladder tumors? J. Urol. 166, 1296–1299 (2001)
D.H. Tang, S.S. Chang, Management of carcinoma in situ of the bladder: best practice and recent developments. Ther. Adv. Urol. 7, 351–364 (2015)
I. Barth, U. Schneider, T. Grimm, A. Karl, D. Horst, N.T. Gaisa, R. Knüchel, S. Garczyk, Progression of urothelial carcinoma in situ of the urinary bladder: a switch from luminal to basal phenotype and related therapeutic implications. Virchows Arch. 472, 749–758 (2018)
S. Garczyk, N. Ortiz-Brüchle, U. Schneider, I. Lurje, K. Guricova, N.T. Gaisa, E. Lorsy, K. Lindemann-Docter, A. Heidenreich, R. Knüchel, Next-generation sequencing reveals potential predictive biomarkers and targets of therapy for urothelial carcinoma in situ of the urinary bladder. Am. J. Pathol. (2019). doi:https://doi.org/10.1016/j.ajpath.2019.10.004
G. Sjödahl, C.L. Jackson, J.M.S. Bartlett, D.R. Siemens, D.M. Berman, Molecular profiling in muscle-invasive bladder cancer: more than the sum of its parts. J. Pathol. 247, 563–573 (2019)
A. Hodgson, B. Xu, M.R. Downes, p53 immunohistochemistry in high-grade urothelial carcinoma of the bladder is prognostically significant. Histopathology 71, 296–304 (2017)
W. Remmele, H.E. Stegner, [Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue]. Pathologe 8, 138–140 (1987)
G. Pauletti, S. Dandekar, H. Rong, L. Ramos, H. Peng, R. Seshadri, D.J. Slamon, Assessment of methods for tissue-based detection of the HER-2/neu alteration in human breast cancer: a direct comparison of fluorescence in situ hybridization and immunohistochemistry. J. Clin. Oncol. 18, 3651–3664 (2000)
D. Tomlinson, O. Baldo, P. Harnden, M. Knowles, FGFR3 protein expression and its relationship to mutation status and prognostic variables in bladder cancer. J. Pathol. 213, 91–98 (2007)
A.C. Wolff, M.E.H. Hammond, J.N. Schwartz, K.L. Hagerty, D.C. Allred, R.J. Cote, M. Dowsett, P.L. Fitzgibbons, W.M. Hanna, A. Langer, L.M. McShane, S. Paik, M.D. Pegram, E.A. Perez, M.F. Press, A. Rhodes, C. Sturgeon, S.E. Taube, R. Tubbs, G.H. Vance, M. van de Vijver, T.M. Wheeler, D.F. Hayes, American Society of Clinical Oncology, College of American Pathologists, American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J. Clin. Oncol. 25, 118–145 (2007)
A.G. Robertson, J. Kim, H. Al-Ahmadie, J. Bellmunt, G. Guo, A.D. Cherniack, T. Hinoue, P.W. Laird, K.A. Hoadley, R. Akbani, M.A.A. Castro, E.A. Gibb, R.S. Kanchi, D.A. Gordenin, S.A. Shukla, F. Sanchez-Vega, D.E. Hansel, B.A. Czerniak, V.E. Reuter, X. Su, B. de Sa Carvalho, V.S. Chagas, K.L. Mungall, S. Sadeghi, C.S. Pedamallu, Y. Lu, L.J. Klimczak, J. Zhang, C. Choo, A.I. Ojesina, S. Bullman, K.M. Leraas, T.M. Lichtenberg, C.J. Wu, N. Schultz, G. Getz, M. Meyerson, G.B. Mills, D.J. McConkey, J.N. Weinstein, D.J. Kwiatkowski, S.P. Lerner, R. Akbani, H. Al-Ahmadie, M. Albert, I. Alexopoulou, A. Ally, T. Antic, M. Aron, M. Balasundaram, J. Bartlett, S.B. Baylin, A. Beaver, J. Bellmunt, I. Birol, L. Boice, M.S. Bootwalla, J. Bowen, R. Bowlby, D. Brooks, B.M. Broom, W. Bshara, S. Bullman, E. Burks, F.M. Cárcano, R. Carlsen, B.S. Carvalho, A.L. Carvalho, E.P. Castle, M.A.A. Castro, P. Castro, J.W. Catto, V.S. Chagas, A.D. Cherniack, D.W. Chesla, C. Choo, E. Chuah, S. Chudamani, V.K. Cortessis, S.L. Cottingham, D. Crain, E. Curley, B.A. Czerniak, S. Daneshmand, J.A. Demchok, N. Dhalla, H. Djaladat, J. Eckman, S.C. Egea, J. Engel, I. Felau, M.L. Ferguson, J. Gardner, J.M. Gastier-Foster, M. Gerken, G. Getz, E.A. Gibb, C.R. Gomez-Fernandez, D.A. Gordenin, G. Guo, D.E. Hansel, J. Harr, A. Hartmann, L.M. Herbert, T. Hinoue, T.H. Ho, K.A. Hoadley, R.A. Holt, C.M. Hutter, S.J.M. Jones, M. Jorda, R.J. Kahnoski, R.S. Kanchi, K. Kasaian, J. Kim, L.J. Klimczak, D.J. Kwiatkowski, P.H. Lai, P.W. Laird, B.R. Lane, K.M. Leraas, S.P. Lerner, T.M. Lichtenberg, J. Liu, L. Lolla, Y. Lotan, Y. Lu, F.R. Lucchesi, Y. Ma, R.D. Machado, D.T. Maglinte, D. Mallery, M.A. Marra, S.E. Martin, M. Mayo, D.J. McConkey, A. Meraney, M. Meyerson, G.B. Mills, A. Moinzadeh, R.A. Moore, E.M.M. Pinero, S. Morris, C. Morrison, K.L. Mungall, A.J. Mungall, J.B. Myers, R. Naresh, P.H. O’Donnell, A.I. Ojesina, D.J. Parekh, J. Parfitt, J.D. Paulauskis, C.S. Pedamallu, R.J. Penny, T. Pihl, S. Porten, M.E. Quintero-Aguilo, N.C. Ramirez, W.K. Rathmell, V.E. Reuter, K. Rieger-Christ, A.G. Robertson, S. Sadeghi, C. Saller, A. Salner, F. Sanchez-Vega, G. Sandusky, C. Scapulatempo-Neto, J.E. Schein, A.K. Schuckman, N. Schultz, C. Shelton, T. Shelton, S.A. Shukla, J. Simko, P. Singh, P. Sipahimalani, N.D. Smith, H.J. Sofia, A. Sorcini, M.L. Stanton, G.D. Steinberg, R. Stoehr, X. Su, T. Sullivan, Q. Sun, A. Tam, R. Tarnuzzer, K. Tarvin, H. Taubert, N. Thiessen, L. Thorne, K. Tse, K. Tucker, D.J. Van Den Berg, K.E. van Kessel, S. Wach, Y. Wan, Z. Wang, J.N. Weinstein, D.J. Weisenberger, L. Wise, T. Wong, Y. Wu, C.J. Wu, L. Yang, L.A. Zach, J.C. Zenklusen, J.(.J.). Zhang, J. Zhang, E. Zmuda, E.C. Zwarthoff, Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 171, 540–556.e25 (2017)
Damrauer JS, Hoadley KA, Chism DD, Fan C, Tiganelli CJ, Wobker SE, Yeh JJ, Milowsky MI, Iyer G, Parker JS, Kim WY (2014) Intrinsic subtypes of high-grade bladder cancer reflect the hallmarks of breast cancer biology. Proc. Natl. Acad. Sci. U. S. A. 111:3110–3115
K.T. Mai, T.A. Flood, P. Williams, Z. Kos, E.C. Belanger, Mixed low- and high-grade papillary urothelial carcinoma: histopathogenetic and clinical significance. Virchows Arch. 463, 575–581 (2013)
M. Jung, B. Kim, K.C. Moon, Immunohistochemistry of cytokeratin (CK) 5/6, CD44 and CK20 as prognostic biomarkers of non-muscle-invasive papillary upper tract urothelial carcinoma. Histopathology 74, 483–493 (2019)
J. Rebola, P. Aguiar, A. Blanca, R. Montironi, A. Cimadamore, L. Cheng, V. Henriques, P. Lobato-Faria, A. Lopez-Beltran, Predicting outcomes in non-muscle invasive (Ta/T1) bladder cancer: the role of molecular grade based on luminal/basal phenotype. Virchows Arch. 475, 445–455 (2019)
J. Breyer, R.M. Wirtz, W. Otto, P. Erben, M.C. Kriegmair, R. Stoehr, M. Eckstein, S. Eidt, S. Denzinger, M. Burger, A. Hartmann, BRIDGE Consortium, In stage pT1 non-muscle-invasive bladder cancer (NMIBC), high KRT20 and low KRT5 mRNA expression identify the luminal subtype and predict recurrence and survival. Virchows Arch. 470, 267–274 (2017)
Hedegaard J, Lamy P, Nordentoft I, Algaba F, Høyer S, Ulhøi BP, Vang S, Reinert T, Hermann GG, Mogensen K, Thomsen MBH, Nielsen MM, Marquez M, Segersten U, Aine M, Höglund M, Birkenkamp-Demtröder K, Fristrup N, Borre M, Hartmann A, Stöhr R, Wach S, Keck B, Seitz AK, Nawroth R, Maurer T, Tulic C, Simic T, Junker K, Horstmann M, Harving N, Petersen AC, Calle ML, Steyerberg EW, Beukers W, van Kessel KEM, Jensen JB, Pedersen JS, Malmström PU, Malats N, Real FX, Zwarthoff EC, Ørntoft TF, Dyrskjøt L, Comprehensive transcriptional analysis of early-stage urothelial carcinoma. Cancer Cell 30:27–42 (2016)
M. Jung, J. Lee, B. Kim, J. Park, K. Moon, Transcriptional analysis of immunohistochemically defined subgroups of non-muscle-invasive papillary high-grade upper tract urothelial carcinoma. Int. J. Mol. Sci. (2019). https://doi.org/10.3390/ijms20030570
E.J. Pietzak, A. Bagrodia, E.K. Cha, E.N. Drill, G. Iyer, S. Isharwal, I. Ostrovnaya, P. Baez, Q. Li, M.F. Berger, A. Zehir, N. Schultz, J.E. Rosenberg, D.F. Bajorin, G. Dalbagni, H. Al-Ahmadie, D.B. Solit, B.H. Bochner, Next-generation sequencing of nonmuscle invasive bladder cancer reveals potential biomarkers and rational therapeutic targets. Eur. Urol. 72, 952–959 (2017)
C.D. Hurst, O. Alder, F.M. Platt, A. Droop, L.F. Stead, J.E. Burns, G.J. Burghel, S. Jain, L.J. Klimczak, H. Lindsay, J.-A. Roulson, C.F. Taylor, H. Thygesen, A.J. Cameron, A.J. Ridley, H.R. Mott, D.A. Gordenin, M.A. Knowles, Genomic subtypes of non-invasive bladder cancer with distinct metabolic profile and female gender bias in KDM6A mutation frequency. Cancer Cell 32, 701–715.e7 (2017)
S. Rebouissou, A. Hérault, E. Letouzé, Y. Neuzillet, A. Laplanche, K. Ofualuka, P. Maillé, K. Leroy, A. Riou, M.-L. Lepage, D. Vordos, A. de la Taille, Y. Denoux, M. Sibony, F. Guyon, T. Lebret, S. Benhamou, Y. Allory, F. Radvanyi, CDKN2A homozygous deletion is associated with muscle invasion in FGFR3-mutated urothelial bladder carcinoma. J. Pathol. 227, 315–324 (2012)
M.R. Downes, B. Weening, B.W.G. van Rhijn, C.L. Have, K.M. Treurniet, T.H. van der Kwast, Analysis of papillary urothelial carcinomas of the bladder with grade heterogeneity: supportive evidence for an early role of CDKN2A deletions in the FGFR3 pathway. Histopathology 70, 281–289 (2017)
A.H. Nassar, R. Umeton, J. Kim, K. Lundgren, L. Harshman, E.M. Van Allen, M. Preston, F. Dong, J. Bellmunt, K.W. Mouw, T.K. Choueiri, G. Sonpavde, D.J. Kwiatkowski, Mutational analysis of 472 urothelial carcinoma across grades and anatomic sites. Clin. Cancer Res. 25, 2458–2470 (2019)
L.D. Ler, S. Ghosh, X. Chai, A.A. Thike, H.L. Heng, E.Y. Siew, S. Dey, L.K. Koh, J.Q. Lim, W.K. Lim, S.S. Myint, J.L. Loh, P. Ong, X.X. Sam, D. Huang, T. Lim, P.H. Tan, S. Nagarajan, C.W.S. Cheng, H. Ho, L.G. Ng, J. Yuen, P.-H. Lin, C.-K. Chuang, Y.-H. Chang, W.-H. Weng, S.G. Rozen, P. Tan, C.L. Creasy, S.-T. Pang, M.T. McCabe, S.L. Poon, B.T. Teh, Loss of tumor suppressor KDM6A amplifies PRC2-regulated transcriptional repression in bladder cancer and can be targeted through inhibition of EZH2. Sci. Transl. Med. 9, eaai8312 (2017)
J. Shen, Y. Peng, L. Wei, W. Zhang, L. Yang, L. Lan, P. Kapoor, Z. Ju, Q. Mo, I.-M. Shih, I.P. Uray, X. Wu, P.H. Brown, X. Shen, G.B. Mills, G. Peng, ARID1A deficiency impairs the DNA damage checkpoint and sensitizes cells to PARP inhibitors. Cancer Discov. 5, 752–767 (2015)
H. Ogiwara, M. Sasaki, T. Mitachi, T. Oike, S. Higuchi, Y. Tominaga, T. Kohno, Targeting p300 adiction in CBP-deficient cancers causes synthetic lethality by apoptotic cell death due to abrogation of MYC expression. Cancer Discov. 6, 430–445 (2016)
N. McCabe, N.C. Turner, C.J. Lord, K. Kluzek, A. Bialkowska, S. Swift, S. Giavara, M.J. O’Connor, A.N. Tutt, M.Z. Zdzienicka, G.C.M. Smith, A. Ashworth, Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 66, 8109–8115 (2006)
Y. Liu, D.J. Kwiatkowski, Combined CDKN1A/TP53 mutation in bladder cancer is a therapeutic target. Mol. Cancer Ther. 14, 174–182 (2015)
R. Moser, C. Xu, M. Kao, J. Annis, L.A. Lerma, C.M. Schaupp, K.E. Gurley, I.S. Jang, A. Biktasova, W.G. Yarbrough, A.A. Margolin, C. Grandori, C.J. Kemp, E. Méndez, Functional kinomics identifies candidate therapeutic targets in head and neck cancer. Clin. Cancer Res. 20, 4274–4288 (2014)
S.-X. Zeng, Y. Zhu, A.-H. Ma, W. Yu, H. Zhang, T.-Y. Lin, W. Shi, C.G. Tepper, P.T. Henderson, S. Airhart, J.-M. Guo, C.-L. Xu, R.W. deVere White, C.-X. Pan, The phosphatidylinositol 3-kinase pathway as a potential therapeutic target in bladder cancer. Clin. Cancer Res. 23, 6580–6591 (2017)
Y. Loriot, A. Necchi, S.H. Park, J. Garcia-Donas, R. Huddart, E. Burgess, M. Fleming, A. Rezazadeh, B. Mellado, S. Varlamov, M. Joshi, I. Duran, S.T. Tagawa, Y. Zakharia, B. Zhong, K. Stuyckens, A. Santiago-Walker, P. De Porre, A. O’Hagan, A. Avadhani, A.O. Siefker-Radtke, BLC2001 Study Group, Erdafitinib in locally advanced or metastatic urothelial carcinoma. N. Engl. J. Med. 381, 338–348 (2019)
G. Au-Yeung, F. Lang, W.J. Azar, C. Mitchell, K.E. Jarman, K. Lackovic, D. Aziz, C. Cullinane, R.B. Pearson, L. Mileshkin, D. Rischin, A.M. Karst, R. Drapkin, D. Etemadmoghadam, D.D.L. Bowtell, Selective targeting of Cyclin E1-amplified high-grade serous ovarian cancer by cyclin-dependent kinase 2 and AKT inhibition. Clin. Cancer Res. 23, 1862–1874 (2017)
Johannessen CM, Reczek EE, James MF, Brems H, Legius E, Cichowski K (2005) The NF1 tumor suppressor critically regulates TSC2 and mTOR. Proc. Natl. Acad. Sci. U. S. A. 102:8573–8578
M.Y. Teo, R.M. Bambury, E.C. Zabor, E. Jordan, H. Al-Ahmadie, M.E. Boyd, N. Bouvier, S.A. Mullane, E.K. Cha, N. Roper, I. Ostrovnaya, D.M. Hyman, B.H. Bochner, M.E. Arcila, D.B. Solit, M.F. Berger, D.F. Bajorin, J. Bellmunt, G. Iyer, J.E. Rosenberg, DNA damage response and repair gene alterations are associated with improved survival in patients with platinum-treated advanced urothelial carcinoma. Clin. Cancer Res. 23, 3610–3618 (2017)
Acknowledgements
Open Access funding provided by Projekt DEAL. We thank Eva Lorsy (University Hospital Cologne) and Angela Maurer (University Hospital RWTH Aachen) for supporting the assessment of the NGS data. This research project is supported by the START-Program of the Faculty of Medicine, RWTH Aachen University. Grant Number: 06/17 (SG).
Author information
Authors and Affiliations
Contributions
Conceptualization (SG, RK); Methodology (SG, NOB, US, KG); Investigation (TS, SG, RK, US); Formal analysis (TS, SG, NOB, KG, AB, RK); Software (KG, NOB); Writing – original draft preparation (TS); Writing – review and editing (SG, RK, NTG, NOB, AH, AB, IL, US, KG, GBS); Resources (AB, AH); Supervision (SG, RK); Funding acquisition (SG).
Corresponding author
Ethics declarations
The study has been approved by the institutional research ethics committee of the University Hospital RWTH Aachen (approval no 291/16) and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
(XLSX 13 kb)
Online Resource 2
(XLSX 16 kb)
Online Resource 3
(XLSX 11 kb)
Online Resource 4
(XLSX 10 kb)
Online Resource 5
(XLSX 10 kb)
Online Resource 6
(PDF 170 kb)
Online Resource 7
(XLSX 20 kb)
Online Resource 8
(XLSX 10 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schnitzler, T., Ortiz-Brüchle, N., Schneider, U. et al. Pure high-grade papillary urothelial bladder cancer: a luminal-like subgroup with potential for targeted therapy. Cell Oncol. 43, 807–819 (2020). https://doi.org/10.1007/s13402-020-00524-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-020-00524-6