Abstract
As therapeutic monoclonal antibodies (mAbs) become more humanized, traditional tryptic peptide approaches used to measure biologics in serum become more challenging since unique clonotypic peptides used for quantifying the mAb may also be found in the normal serum polyclonal background. An alternative approach is to monitor the unique molecular mass of the intact light chain portion of the mAbs using liquid chromatography-mass spectrometry (LC-MS). Distinguishing a therapeutic mAb from a patient’s normal polyclonal immunoglobulin (Ig) repertoire is the primary limiting factor when determining the limit of quantitation (LOQ) in serum. The ability to selectively extract subclass specific Igs from serum reduces the polyclonal background in a sample. We present here the development of an LC-MS method to quantify eculizumab in serum. Eculizumab is a complement component 5 (C5) binding mAb that is fully humanized and contains portions of both IgG2 and IgG4 subclasses. Our group developed a method that uses Life Technologies CaptureSelect IgG4 (Hu) affinity matrix. We show here the ability to quantitate eculizumab with a LOQ of 5 mcg/mL by removing the higher abundance IgG1, IgG2, and IgG3 from the polyclonal background, making this approach a simple and efficient procedure.

ᅟ
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monoclonal therapeutic antibodies (mAbs) are an important class of drugs used to treat diseases ranging from autoimmune disorders to B cell lymphomas. Over the past years there have been many novel advances made in mass spectrometry (MS)-based characterization of immunoglobulins (Igs) driven primarily by pharmaceutical companies who have invested substantial resources in characterizing mAbs during both the development and production phases. Many of these advancements are just now being applied in clinical laboratories and are altering the way in which Igs are analyzed outside of a research setting. The rise in the use of therapeutic mAbs has opened up new challenges for clinical chemists interested in therapeutic drug monitoring (TDM) using MS since mAbs are larger and more complex than most therapeutic drugs. In addition, most therapeutic mAbs currently on the market have the same structure as endogenous Igs.
TDM is typically not performed during therapeutic mAb treatment regimens due to the low toxicity of biologics. Measurement of therapy efficacy is usually empirical, based on clinical presentation and improvement of symptoms, although this landscape is changing, as it is recognized that patients undergoing therapies may develop immunogenicity, an immune response to the drug with the appearance of anti-drug antibodies, which may lead to loss of response to therapy [1–3]. TDM may be useful when assessing response to therapy requires an invasive procedure, a subjective evaluation of well-being by the clinician, or is simply difficult. Another instance where TDM is warranted is when the effective dose of a drug is known and patients need to be above a certain therapeutic mAb concentration in order to improve the odds of a clinical response, but very few therapeutic mAbs on the market have a mandatory companion diagnostic test. A companion diagnostic test, according to the Food and Drug Administration (FDA), is to provide the information that is essential for the safe and effective use of a corresponding drug or biological product. The test can be ordered by physicians, and in most circumstances the required companion diagnostic tests are to be used prior to therapy initiation, as prognostic markers of response, not therapeutic monitoring (e.g., programmed -death receptor 1 (PD-1) staining on cancer tissue biopsies before prescription of PD-1 inhibitors such as pembrolizumab for non-small-cell lung cancer or metastatic melanoma, or evaluation of human epidermal growth factor receptor 2 (HER-2) in breast cancer before prescription of herceptin).
There are limited options for measuring the concentration of therapeutic mAbs in a routine clinical laboratory setting after therapy has been initiated. In the United States, all available assays are laboratory developed tests (LDTs), since there are no FDA-approved immunoassays available for any therapeutic mAb on the market, although several ce-cleared ELISA kits are available in Europe. Especially in the gastroenterology practice, monitoring response to therapeutic mAbs has been associated with improved prognosis and outcomes. Adjustments in therapeutic regimens can be made, both decreasing healthcare costs and saving patients from unnecessary interventions. With this in mind, our group has been actively pursuing quantitative methods for therapeutic mAbs that can be performed in a clinical laboratory. Past examples of this work include the measurement of rituximab using microLC-ESI-Q-TOF MS in serum from patients with vasculitis [4], and a tryptic peptide approach for measurement of infliximab using liquid chromatography tandem mass spectrometry (LC-MS/MS) [5].
Therapeutic mAbs are administered intravenously or subcutaneously and are intended to remain in circulation for as long as possible to increase efficacy. Pharmaceutical companies have continuously redesigned recombinant therapeutic mAbs in order to optimize binding efficiency, lower immunogenicity, and increase time in circulation [6–9].
Nearly all therapeutic mAbs containing a complete Ig molecule have an IgG heavy chain and a kappa light chain. Eculizumab has this same basic Ig structure combined with some distinctive features. The antigen binding region of eculizumab contains murine complementarity-determining regions grafted onto human framework light and heavy chain variable regions. The isotype-specific region of the heavy chain constant region of eculizumab contains portions of both IgG subclass 2 and IgG subclass 4. Having the unique combination of an IgG2/4 constant region makes this molecule fail to bind to Fc receptors (IgG2) and does not activate complement (IgG4), which reduces the pro-inflammatory potential of the antibody [10]. This is important, since eculizumab is designed to selectively bind to complement component 5 (C5), thereby inhibiting the terminal portion of the complement cascade decreasing inflammation and cell destruction. The drug is FDA-approved for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and atypical hemolytic uremic syndrome (aHUS), and once treatment for these rare diseases is initiated, it is usually life-long [11–13]. Eculizumab is also the most expensive prescription drug in the world at approximately $440,000 a year in the United States [14]. A method that can accurately measure eculizumab in serum may decrease healthcare costs and increase therapy efficacy, if associated with TDM.
Our group recently reported using microLC-ESI-Q-TOF MS to quantify the therapeutic mAb rituximab in serum from patients with vasculitis [4]. In that study patient samples were enriched for Igs using Melon Gel followed by reduction of the sample with dithiothreitol (DTT) before detection using microLC-ESI-Q-TOF MS. Multiple charge states from the kappa light chain were used to obtain peak area values for quantification of rituximab using an in-house developed software package. In addition, endogenous Igs expressed above the polyclonal background during the course of treatment were analyzed. We have also published a clonotypic-selected-reaction monitoring approach run on a triple-quadrupole mass spectrometer, which is currently in production in our clinical laboratories to quantify infliximab [5]. Briefly, serum was enriched for Igs using a saturated ammonium sulfate crash and digested. Peptides were separated by reversed-phase C8 liquid chromatography and detected by tandem-MS. Peptides specific to the light and heavy chains of infliximab are monitored and quantitated.
For the eculizumab method development shown here, we evaluated the intact light chain approach using a single charge state of the kappa light chain from eculizumab to quantify the mAb as detected using microLC-ESI-Q-TOF MS. We have developed two methods to detect and quantitate the intact light chains of eculizumab with different pre-analytical sample extraction that allows for selective enrichment for all Igs or a selected class of Igs. We have used Melon Gel, which is a resin that binds to non-Ig molecules in mild pH conditions enriching for total Ig, and CaptureSelect anti-human IgG4 camelid nanobodies bound to polymer beads, to purify a select class of Ig prior to analysis. The data presented here represents a broad assessment of a new methodology for IgG4 mAbs that will be readily transferrable to different mass spectrometer platforms as well as to new therapeutic mAbs that may require TDM.
Methods
Reagents
Ammonium bicarbonate, DTT, and formic acid were purchased from Sigma-Aldrich (St. Louis, MO, USA). Water and acetonitrile were purchased from Honeywell Burdick and Jackson (Muskegon, MI, USA). Melon Gel and Pierce spin columns was purchased from ThermoFisher Scientific (Waltham, MA, USA). CaptureSelect IgG4 (Hu) affinity matrix was purchased from Life Technologies (Carlsbad, CA, USA). Normal human serum (NHS) was purchased from EMD Millipore (Billerica, MA, USA).
Monoclonal Therapeutic Antibodies
Residual vials of eculizumab (Alexion Pharmaceuticals, New Haven, CT, USA) and pembrolizumab (Merck and Company, Kenilworth, NJ, USA) were obtained from the institution’s pharmacy. Standard curves and controls were prepared by spiking eculizumab in purchased NHS. No IRB approval was required for this study.
IgG Enrichment
A volume of 20 mcL unknown and 20 mcL protein internal standard (150 mcg/mL pembrolizumab in Melon Gel buffer), were added to a 1.5 mL microcentrifuge tube along with 200 mcL Melon Gel slurry. The 1.5 mL microcentrifuge tube was laid on an orbital mixer for 15 min to give maximum surface area for mixing. The microcentrifuge tube was then placed in a test tube rack to allow for the Melon Gel slurry to settle. A volume of 20 mcL of the supernatant, along with 10 mcL 200 mM DTT and 20 mcL of 50 mM ammonium bicarbonate were placed into a well of a 96-well plate. Samples were reduced at 55 °C for 30 min.
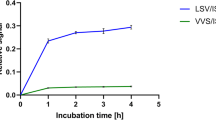
IgG4 Enrichment
A volume of 100 mcL CaptureSelect IgG4 (Hu) affinity matrix was added to a spin column. The matrix was washed two times with 400 mcL phosphate buffered saline (PBS). A volume of 50 mcL unknown, 50 mcL protein internal standard (50 mcg/mL pembrolizumab in PBS), and 400 mcL PBS were added to the spin column. The spin column was capped and mixed at room temperature for 1 h. The column was then washed two times with 500 mcL water. A volume of 200 mcL 5% acetic acid was used for elution after 30 min room temperature incubation. A volume of 100 mcL of 100 mM DTT in 1 M ammonium bicarbonate was added, and the samples were reduced 55 °C for 30 min.
LC Conditions
An Eksigent Ekspert 200 microLC (Dublin, CA, USA) was used for separation; mobile phase A was water + 0.1% formic acid, and mobile phase B was 90% acetonitrile + 10% 2-propanol + 0.1% formic acid. A 2-mcL injection was made onto a 1.0 × 75 mm Poroshell 300SB-C3 column flowing at 25 mcL/min set in a column oven at a temperature of 60 °C. A 25 min gradient was started at 80% A/20% B, held for 1.0 min, ramped to 74% A/26% B over 2.0 minutes, ramped to 64% A/36% B over 8.5 min, ramped to 53% A/47% B over 5.0 min, ramped to 6% A/94% B over 1.5 min, held for 4.0 min, then ramped to 80% A/20% B over 1.0 min, and finally re-equilibrated at 80% A/20% B for 2.0 min before the next injection.
ESI-Q-TOF MS
Spectra were collected on a AB Sciex TripleTOF 5600 quadrupole time-of-flight (TOF) mass spectrometer (AB Sciex, Vaughan, ON, Canada) in ESI positive mode with a Turbo V dual-ion source with an automated calibrant delivery system (CDS). Source conditions were: GS1, 35; GS2, 30, CUR, 45; TEM, 500; ISVF, 5500; DP, 100; and CE, 10. TOF MS scans were acquired from m/z 600–2500 with an acquisition time of 200 ms. The instrument was calibrated every 10 injections through the CDS using calibration solution supplied by the manufacturer.
Data Analysis
Analyst TF v1.6 was used for instrument control. Data were viewed using Analyst TF v1.7.1 and PeakView v2.2. Extract ion of the mAb +11 m/z ± 0.4 was used to gauge the retention time of known mAb to extract from the total ion current (TIC). Retention time (0.3 min) of the mAb was summed and extracted to give TOF MS spectrum showing the charge state spectrum for the specific light chain. The +11 charge state peak was integrated and the area under the peak used for calculation of standard curve and then to calculate unknowns from standard curve using regression. Multiply charged ion peak centroids were used to calculate average molecular mass through Bio Tool Kit in PeakView. Protein reconstruction was done using an output mass range between 20,000 and 30,000 Da, with a step size of 1.
Results and Discussion
We first evaluated the performance characteristics of eculizumab using a previously published Melon Gel intact light chain quantitative approach [4, 15]. The LOD was defined as an analyte response that was distinguishable from the purchased NHS with a signal-to-noise (S/N) of at least 5. No peak specific for eculizumab was detected in NHS (Figure 1a). The LOD was found to be 50 mcg/mL with S/N of 5.9 (Figure 1b). The lower limit of quantitation (LLOQ) was then determined to be 100 mcg/mL; N = 20, mean peak area response of 33.21, S/N > 10, repeatability of 3.6% CV (coefficient of variation) (Table 1). Linearity was assessed over a total of six runs using six concentration levels of mAb spiked into NHS; 50, 100, 200, 300, 400, and 500 mcg/mL, all generated from unique dilutions; no serial dilutions were used. Linear regression analysis of the peak response showed a slope of 1.017, a y-intercept of −9.896 and an R2 = 0.985. Repeatability and within-laboratory imprecision were evaluated. Repeatability was less than 10% for three levels analyzed with N = 12 replicates (91.1 mcg/mL, 3.6%; 206 mcg/mL, 6.0%; 422 mcg/mL, 6.0%). Within-laboratory imprecision was less than 15% for the six different concentrations evaluated over a 6-mo time period (50.7 mcg/mL, 10.3%; 72.2 mcg/mL, 8.0%; 84.6 mcg/mL, 8.8%; 143 mcg/mL, 10.4%; 170 mcg/mL 12.3%; 296 mcg/mL 7.6%) (Table 1). Carryover was assessed by running the purchased NHS after the high standard of 500 mcg/mL on each run (>20). No carryover was observed.
Limit of detection of the two enrichment methods for quantitation of eculizumab. Mass spectra of eculizumab extract ion (2103.7 m/z) for normal pooled serum (a) from Melon Gel, and (c) IgG4 affinity matrix showing the absence of peak in pooled serum for both methods. (b) The LOD for Melon Gel was found to be 50 mcg/mL with S/N = 5.9. (d) In comparison, the IgG4 affinity matrix allows for an over 10× increase in sensitivity; LOD = 5 mcg/mL with S/N = 7.4
Further method exploration was prompted as the Melon Gel Ig enrichment intact light chain assay for eculizumab had a high LLOQ (100 mcg/mL) that would not allow it to be readily useful for TDM, where therapeutic concentrations are expected to be above 35 mcg/mL for PNH, for instance [10]. This limitation motivated the development of a more sensitive assay using an enrichment method specific for IgG4.
The application of the Life Technologies CaptureSelect affinity matrix for purifying specific immunoglobulin isotypes was recently shown for screening of monoclonal gammopathy using MALDI-TOF MS [16, 17]. This polymer bead-based camelid nanobody purification technique has been used by pharma in the development and validation of new therapeutic mAbs. We surmised that the IgG4 specific CaptureSelect affinity matrix beads could be used to selectively enrich for eculizumab. Furthermore, since IgG4 has the lowest concentration compared with the other subclasses, the overall IgG polyclonal background should be lowered. Figure 2a shows two TICs from microLC-ESI-Q-TOF MS analyzed serum where the black trace represents Melon Gel enriched IgGs and the red trace represents IgG4 CaptureSelect IgG4s. The figure shows that the IgG4 affinity matrix provides lower background as evident by the reduced overall intensity of the TIC. Figure 2b shows the mass spectra generated by summing spectra over 5 to 8 min with the Melon Gel enriched IgGs in the black trace and IgG4 CaptureSelect purified IgGs in the red trace.
An additional phenomenon that was identified during the IgG4 affinity matrix development process was the impact the reducing agent had on the chromatography of the intact light chain and, therefore, peak area calculations and S/N. In early development, tris(2-carboxyethyl)phosphine (TCEP) was used as the reducing agent as it fit in with the acid elution step for the affinity matrix; for example, eluting from the affinity matrix with 200 mcL 100 mM TCEP in 5% acetic acid. TCEP resulted in variable reduction of intra-disulfide bonds on the light chains. This variable reduction resulted in multiple, chromatographically separated peaks for the eculizumab light chain (Figure 3; red trace). We therefore switched to using DTT as the reducing agent, which does not reduce light chain intra-disulfide bonds ensuing in reproducible retention times and peak area calculations.
Different reducing agents were tested during method development. The choice of reducing agent can affect the elution of eculizumab as shown in the chromatogram. (a) Reduction by DTT reduces the disulfide bond connecting the light chain to the heavy chain; black trace. A stronger reducer, such as TCEP, can give inconsistent reduction to chromatographically separate charge state distributions as seen in (b) and (c); red trace
Next we evaluated the performance characteristics of the IgG4 purification method versus the Melon Gel purification method with the same LC-MS conditions. A 10-fold drop in the LOD was observed; from 50 mcg/mL using the Melon Gel approach to 5 mcg/mL using the IgG4 approach (Figure 1b and d). We determined our LLOQ to be equivalent to the LOD at 5 mcg/mL as we still obtained acceptable imprecision at the lowest standard of 1.5 mcg/mL, N = 20, mean peak area response 2.42, repeatability of 14.9% CV. Linearity for the IgG4 purification method was assessed over a total of six runs using six concentration levels of mAb spiked into NHS; 1.5, 15, 75, 100, 150, and 200 mcg/mL. The IgG4 purification method was found to be linear from 1.5 mcg/mL to 200 mcg/mL with the linear regression analysis of the peak response for the standards having a slope of 0.995, a y-intercept of 1.839, and an R2 value of 0.989. Repeatability and within-laboratory imprecision were evaluated for the IgG4 purification method and are presented in Table 2. Repeatability was less than 11% for four levels analyzed with N = 19 replicates (1.1 mcg/mL, 10.4%; 1.2, 10.8%; 18.3 mcg/mL, 5.6%; 88.2 mcg/mL, 5.5%). Within-laboratory imprecision was less than 16% for five levels evaluated over a 6-mo time period (1.6 mcg/mL, 14.9%; 16.0 mcg/mL, 8.0%; 57.0 mcg/mL, 15.2%; 79.3 mcg/mL, 9.3%; 153 mcg/mL 9.2%). Carryover was assessed by running the purchased NHS after the high standard of 200 mcg/mL on each run (>20). No significant carryover (greater than LOD) was observed. This data has concluded the method development stage for the assay.
Treatment failure is a concern, given the expensive cost of therapeutic mAbs. Tools for optimizing therapy regimens are welcome in the clinic; however, laboratory test costs are a challenge for both patients and clinical laboratories. Other clinically available methods used to measure therapeutic mAbs, besides the tryptic peptide LC-MS/MS or the intact light chain quantitation shown here, include size-exclusion high performance liquid chromatography, cell line-based reporter gene assays, and immunoassays using labeled antibodies. The tests are often patented and licenses not available, or exclusive agreements are in place. Although cost estimates for these tests are not publicly available, from our own experience, once a mass spectrometer instrument is available in the laboratory and used for a multitude of applications, the cost of solvents, columns, and the IgG4 extraction protocol that can be employed for multiple assays is significantly lower than analyte-specific fluorophore-labeled antibodies, which can show significant lot-to-lot variability and may cost thousands of dollars. Nevertheless, all assays use the therapeutic mAb as a standard or calibrator, which adds to the cost of the assay. Labor costs should be taken into consideration for all available methods, given the mass spectrometry approaches, although amenable to pre-analytical automation, require specialized technologists for interpretation and troubleshooting.
This method development shows adequate robustness and precision over time, necessary characteristics for the clinical laboratory environment. It represents a strong basis for moving forward with the validation and implementation of a TDM assay for eculizumab using sera from patients undergoing therapy to evaluate accuracy, reportable ranges, interference, and complete a full clinical validation.
Conclusion
The therapeutic mAb assay development work presented here demonstrates the benefits of evaluating multiple methodologies. By exploring the isotype-specific affinity matrix purification strategy, we were able to lower our LOD for eculizumab while at the same time continue the development of the intact light chain LC-MS-based quantification methodology that works for fully humanized therapeutic mAbs and can be readily implemented in a clinical laboratory setting. Melon Gel is an inexpensive and fast way to enrich samples for IgGs but it also results in a high polyclonal background that may have a negative impact on the LOD, as observed in this study. Furthermore, for mAbs that target molecules in high concentration in serum, such as eculizumab, which binds to complement component 5, with an average concentration of 70 mcg/mL in serum, mAb-target complexes may bind to Melon Gel instead of remaining in the supernatant, which could result in measurement of only the free portion of the mAb, rather than total. The use of the IgG4 enrichment method captures total IgG4 by its Fc fraction and uses an acid elution release step from the beads, which not only significantly reduces background and cleans the sample, but measures total eculizumab. By exploring the isotype-specific affinity matrix purification strategy, we were able to lower the LOD for eculizumab by 10-fold. This method can be applied to other IgG4 humanized mAbs, which may not have adequate trypsin cleavage sites, or may be prescribed at lower doses and, therefore, be present in lower concentrations in circulation. Different pre-analytical steps as the ones shown here can help place the measurement of intact light chains of therapeutic mAbs as a widespread approach in a clinical laboratory setting. Neither of the techniques used for enrichment rely on the development of specialty reagents such as anti-mAb capture antibodies and target antigens, reducing cost and complexity. The next stages of development include performing clinical studies applying this robust and precise methodology to quantify mAbs and translating this approach to a typical clinical laboratory setting.
References
Afif, W., Loftus Jr., E.V., Faubion, W.A., Kane, S.V., Bruining, D.H., Hanson, K.A., Sandborn, W.J.: Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am. J. Gastroenterol. 105, 1133–1139 (2010)
van Schouwenburg, P.A., Rispens, T., Wolbink, G.J.: Immunogenicity of anti-TNF biologic therapies for rheumatoid arthritis. Nat. Rev. Rheumatol. 9, 164–172 (2013)
Willrich, M.A., Murray, D.L., Snyder, M.R.: Tumor necrosis factor inhibitors: clinical utility in autoimmune diseases. Transl. Res. (2014).
Mills, J.R., Cornec, D., Dasari, S., Ladwig, P.M., Hummel, A.M., Cheu, M., Murray, D.L., Willrich, M.A., Snyder, M.R., Hoffman, G.S., Kallenberg, C.G., Langford, C.A., Merkel, P.A., Monach, P.A., Seo, P., Spiera, R.F., St Clair, E.W., Stone, J.H., Specks, U., Barnidge, D.R.: Using mass spectrometry to quantify rituximab and perform individualized immunoglobulin phenotyping in ANCA-associated vasculitis. Anal. Chem. 88, 6317–6325 (2016)
Willrich, M.A., Murray, D.L., Barnidge, D.R., Ladwig, P.M., Snyder, M.R.: Quantitation of infliximab using clonotypic peptides and selective reaction monitoring by LC-MS/MS. Int. Immunopharmacol. 28, 513–520 (2015)
Buss, N.A., Henderson, S.J., McFarlane, M., Shenton, J.M., de Haan, L.: Monoclonal antibody therapeutics: history and future. Curr. Opin. Pharmacol. 12, 615–622 (2012)
Zhang, H., Cui, W., Gross, M.L.: Mass spectrometry for the biophysical characterization of therapeutic monoclonal antibodies. FEBS Lett. 588, 308–317 (2014)
Beck, A., Sanglier-Cianferani, S., Van Dorsselaer, A.: Biosimilar, biobetter, and next generation antibody characterization by mass spectrometry. Anal. Chem. 84, 4637–4646 (2012)
Nelson, A.L., Dhimolea, E., Reichert, J.M.: Development trends for human monoclonal antibody therapeutics. Nat. Rev. Drug Discov. 9, 767–774 (2010)
Wong, E.K., Kavanagh, D.: Anticomplement C5 therapy with eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome. Transl. Res. 165, 306–320 (2015)
Amadio, A., Tejani, A.M.: Eculizumab in atypical hemolytic-uremic syndrome. N. Engl. J. Med. 369, 1378 (2013)
Hillmen, P., Elebute, M., Kelly, R., Urbano-Ispizua, A., Hill, A., Rother, R.P., Khursigara, G., Fu, C.L., Omine, M., Browne, P., Rosse, W.: Long-term effect of the complement inhibitor eculizumab on kidney function in patients with paroxysmal nocturnal hemoglobinuria. Am. J. Hematol. 85, 553–559 (2010)
Kistler, A.D.: Eculizumab in atypical hemolytic-uremic syndrome. N. Engl. J. Med. 369, 1378 (2013)
Herper, M.: The world’s most expensive drugs. Available at: http://www.forbes.com/2010/02/19/expensive-drugs-cost-business-healthcare-rare-diseases.html. Forbes. (2010) Accessed 29 Aug 2016
Barnidge, D.R., Dasari, S., Botz, C.M., Murray, D.H., Snyder, M.R., Katzmann, J.A., Dispenzieri, A., Murray, D.L.: Using mass spectrometry to monitor monoclonal immunoglobulins in patients with a monoclonal gammopathy. J. Proteome Res. 13, 1419–1427 (2014)
Kohlhagen, M.C., Barnidge, D.R., Mills, J.R., Stoner, J., Gurtner, K.M., Liptac, A.M., Lofgren, D.I., Vanderboom, P.M., Dispenzieri, A., Katzmann, J.A., Willrich, M.A., Snyder, M.R., Murray, D.L.: Screening method for M-proteins in serum using nanobody enrichment coupled to MALDI-TOF mass spectrometry. Clin. Chem. 62, 1345–1352 (2016)
Mills, J.R., Kohlhagen, M.C., Dasari, S., Vanderboom, P.M., Kyle, R.A., Katzmann, J.A., Willrich, M.A., Barnidge, D.R., Dispenzieri, A., Murray, D.L.: Comprehensive assessment of M-proteins using nanobody enrichment coupled to MALDI-TOF mass spectrometry. Clin. Chem. 62, 1334–1344 (2016)
CLSI: Evaluation of precision performance of quantitative measurement methods; approved guideline - 2nd edition. CLSI document EP05-02. Clinical and Laboratory Standards Institute: Wayne, PA(2004).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ladwig, P.M., Barnidge, D.R. & Willrich, M.A. Quantification of the IgG2/4 kappa Monoclonal Therapeutic Eculizumab from Serum Using Isotype Specific Affinity Purification and Microflow LC-ESI-Q-TOF Mass Spectrometry. J. Am. Soc. Mass Spectrom. 28, 811–817 (2017). https://doi.org/10.1007/s13361-016-1566-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13361-016-1566-y