Abstract
To reduce mucosal damage in the gastrointestinal tract caused by aspirin, aspirin microcrystals were loaded in soluble polymeric microneedle (MN) tips. Aspirin was prepared into aspirin microcrystals by jet milling. Aspirin microcrystals with particle sizes of 0.5–5 μm were loaded on MN tips with a height of 250 µm or 300 µm. The aspirin microcrystals suspended in a polymer solution were concentrated in the MN tips under negative pressure. The aspirin microcrystals had high stability in the MNs since they were not dissolved in solution during the fabrication process. The MN patch packaged in an aluminum-plastic bag containing silica gel desiccant can be stored at 4 °C. The MN tips implanted in the skin of Institute of Cancer Research (ICR) mice dissolved within 30 min. Isolated porcine ear skin was punctured by MNs with heights of 300 μm and 250 μm to depths of 130 μm and 90 μm, respectively. The fluorescent red (FR) release from MNs reached 98.59% within 24 h. The MNs delivered aspirin microcrystals to the epidermis and dermis, providing a smooth plasma concentration in rats. The MNs loaded with aspirin microcrystals did not evoke primary irritation on the dorsal skin of Japanese white rabbits. In summary, MNs loaded with aspirin microcrystals provide a new approach to improve the stability of aspirin in MN patches.
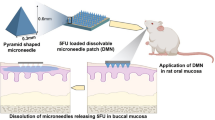
Graphical Abstract












Similar content being viewed by others
Availability of data and materials
All authors agree that any materials and data that are reasonably requested by others will be made available for noncommercial purposes.
References
Anand SS, Bosch J, Eikelboom JW, Connolly SJ, Diaz R, Widimsky P, et al. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: an international, randomised, double-blind, placebo-controlled trial. Lancet. 2018;391(10117):219–29.
Angiolillo DJ, Rollini F, Storey RF, Bhatt DL, James S, Schneider DJ, et al. International expert consensus on switching platelet P2Y12 receptor-inhibiting therapies. Circulation. 2017;136(20):1955–75.
Fahmy SA, Ponte F, Grande G, Fawzy IM, Mandour AA, Sicilia E, et al. Synthesis, characterization and host-guest complexation of asplatin: improved in vitro cytotoxicity and biocompatibility as compared to cisplatin. Pharmaceuticals. 2022;15(2):259–73.
Al-Abdouh A, Abusnina W, Mhanna M, Radideh Q, Alzu’bi H, Rmilah AA, et al. P2Y12 inhibitors versus aspirin monotherapy for long-term secondary prevention of atherosclerotic cardiovascular disease events: a systematic review and meta-analysis. Curr Probl Cardiol. 2022;47(10):101292–310.
Hahn JY, Song YB, Oh JH, Cho DK, Lee JB, Doh JH, et al. 6-month versus 12-month or longer dual antiplatelet therapy after percutaneous coronary intervention in patients with acute coronary syndrome (SMART-DATE): a randomised, open-label, non-inferiority trial. Lancet. 2018;391(10127):1274–84.
Group ASC, Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–39.
Xu XR, Yousef GM, Ni H. Cancer and platelet crosstalk: opportunities and challenges for aspirin and other antiplatelet agents. Blood. 2018;131(16):1777–89.
Laine L, Takeuchi K, Tarnawski A. Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology. 2008;135(1):41–60.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18820 patients. Br Med J. 2004;329:15–9.
Chen SX, Ma M, Xue F, Shen S, Chen Q, Kuang Y, et al. Construction of microneedle-assisted co-delivery platform and its combining photodynamic/immunotherapy. J Control Release. 2020;324:218–27.
Li W, Tang J, Terry RN, Li S, Brunie A, Callahan RL, et al. Long-acting reversible contraception by effervescent microneedle patch. Sci Adv. 2019;5(11):1–12.
Wang K, Hao Y, Wang C, Zhao X, He X, Sun CC. Simultaneous improvement of physical stability, dissolution, bioavailability, and antithrombus efficacy of Aspirin and Ligustrazine through cocrystallization. Int J Pharm. 2022;616:121541–9.
Zhe W, Wenjuan Z, Haihan W, Zhiwei W, Jing C. Oxidation of acetylsalicylic acid in water by UV/O3 process: removal, byproduct analysis, and investigation of degradation mechanism and pathway. J Environ Chem Eng. 2021;9(5):106259–67.
Coutinho IT, Maia-Obi LP, Champeau M. Aspirin-loaded polymeric films for drug delivery systems: comparison between soaking and supercritical CO2 impregnation. Pharmaceutics. 2021;13(6):824–43.
Akkad S, Serpell CJ. Degradable polymers and nanoparticles built from salicylic acid. Macromol Rapid Commun. 2018;39(14):1800182–6.
Vali A, Malayeri HZ, Azizi M, Choi H. DPV-assisted understanding of TiO2 photocatalytic decomposition of aspirin by identifying the role of produced reactive species. Appl Catal B. 2020;266:118646–53.
Veronica N, Liew CV, Heng PWS. Insights on the role of excipients and tablet matrix porosity on aspirin stability. Int J Pharm. 2020;580:119218–27.
Qu M, Kim HJ, Zhou X, Wang C, Jiang X, Zhu J, et al. Biodegradable microneedle patch for transdermal gene delivery. Nanoscale. 2020;12(32):16724–9.
Lin S, Lin H, Yang M, Ge M, Chen Y, Zhu Y. A two-dimensional MXene potentiates a therapeutic microneedle patch for photonic implantable medicine in the second NIR biowindow. Nanoscale. 2020;12(18):10265–76.
Luo J, Ren G, Campbell BM, Zhang D, Cao T, Mishra R, et al. Spontaneous seed formation during electrodeposition drives epitaxial growth of metastable bismuth selenide microcrystals. J Am Chem Soc. 2022;144(40):18272–85.
Oshi MA, Naeem M, Bae J, Kim J, Lee J, Hasan N, et al. Colon-targeted dexamethasone microcrystals with pH-sensitive chitosan/alginate/Eudragit S multilayers for the treatment of inflammatory bowel disease. Carbohydr Polym. 2018;198:434–42.
Lu X, Sun Y, Han M, Chen D, Wang A, Sun K. Silk fibroin double-layer microneedles for the encapsulation and controlled release of triptorelin. Int J Pharm. 2022;613:121433–42.
Zhu J, Zhang C, Jia J, Wang H, Leng H, Xu Y, et al. Osteogenic effects in a rat osteoporosis model and femur defect model by simvastatin microcrystals. Ann N Y Acad Sci. 2021;1487(1):31–42.
Tse D, Kuppusamy P. Biocompatibility of oxygen-sensing paramagnetic implants. Cell Biochem Biophys. 2019;77(3):197–202.
Xu W, Cai Z, Li F, Dong J, Wang Y, Jiang Y, et al. Embedding lead halide perovskite quantum dots in carboxybenzene microcrystals improves stability. Nano Res. 2017;10(8):2692–8.
Xing M, Yang G, Zhang S, Gao Y. Acid-base combination principles for preparation of anti-acne dissolving microneedles loaded with azelaic acid and matrine. Eur J Pharm Sci. 2021;165:105935–45.
Brustugun J, Notaker N, Paetz LH, Tho I, Bjerknes K. Adjusting the dose in paediatric care: dispersing four different aspirin tablets and taking a proportion. Eur J Hosp Pharm. 2021;28(2):76–82.
Liu T, Chen M, Fu J, Sun Y, Lu C, Quan G, et al. Recent advances in microneedles-mediated transdermal delivery of protein and peptide drugs. Acta Pharm Sin B. 2021;11(8):2326–43.
Yang L, Yang Y, Chen H, Mei L, Zeng X. Polymeric microneedle-mediated sustained release systems: design strategies and promising applications for drug delivery. Asian J Pharm Sci. 2021;17(1):70–86.
Obaidat R, BaniAmer F, Assaf SM, Yassin A. Fabrication and evaluation of transdermal delivery of carbamazepine dissolving microneedles. AAPS PharmSciTech. 2021;22(8):253–68.
Cahill EM, Keaveney S, Stuettgen V, Eberts P, Ramos-Luna P, Zhang N, et al. Metallic microneedles with interconnected porosity: a scalable platform for biosensing and drug delivery. Acta Biomater. 2018;80:401–11.
Resnik D, Mozek M, Pecar B, Janez A, Urbancic V, Iliescu C, et al. In vivo experimental study of noninvasive insulin microinjection through hollow Si microneedle array. Micromachines. 2018;9(1):40–56.
Tang M, Mukundan M, Yang J, Charpentier N, LeCluyse EL, Black C, et al. Antiplatelet agents aspirin and clopidogrel are hydrolyzed by distinct carboxylesterases, and clopidogrel is transesterificated in the presence of ethyl alcohol. J Pharmacol Exp Ther. 2006;319(3):1467–76.
Chiplunkar PP, Zhao X, Tomke PD, Noro J, Xu B, Wang Q, et al. Ultrasound-assisted lipase catalyzed hydrolysis of aspirin methyl ester. Ultrason Sonochem. 2018;40:587–93.
Liu H, Zhang S, Zhou Z, Xing M, Gao Y. Two-layer sustained-release microneedles encapsulating exenatide for type 2 diabetes treatment. Pharmaceutics. 2022;14(6):1255–70.
Kr V, Yalavarthi PR, Vadlamudi HC, Kalluri JKY, Rasheed A. Process, physicochemical characterization and in vitro assessment of albendazole microcrystals. Adv Pharm Bull. 2017;7(3):419–25.
Nasr M. Influence of microcrystal formulation on in vivo absorption of celecoxib in rats. AAPS PharmSciTech. 2013;14(2):719–26.
Abrbekoh NF, Salimi L, Saghati S, Amini H, Karkan SF, Moharamzadeh K, et al. Application of microneedle patches for drug delivery; doorstep to novel therapies. J Tissue Eng. 2022;13:1–25.
Wang B, Zhang S, Yang G, Zhou Z, Xing M, Liu H, et al. Dissolvable polymeric microneedles loaded with aspirin for antiplatelet aggregation. Asian J Pharm Sci. 2023;18(1):100776–87.
Sawyer M, Kumar V. A rapid high-performance liquid chromatographic method for the simultaneous quantitation of aspirin, salicylic acid, and caffeine in effervescent tablets. J Chromatogr Sci. 2003;41(8):393–7.
Xing M, Zhang S, Ma Y, Chen Y, Yang G, Zhou Z, et al. Preparation and evaluation of dissolving microneedle loaded with azelaic acid for acne vulgaris therapy. J Drug Deliv Sci Tec. 2022;75:103667–76.
Zhou Z, Zhang S, Yang G, Gao Y. Enhanced delivery efficiency and sustained release of biopharmaceuticals by complexation-based gel encapsulated coated microneedles: rhIFNalpha-1b example. Asian J Pharm Sci. 2021;16(5):612–22.
Wang B, Zhang S, Zhao X, Lian J, Gao Y. Preparation, characterization, and in vivo evaluation of levonorgestrel-loaded thermostable microneedles. Drug Deliv Transl Res. 2022;12(4):944–56.
Zafar R, Khan IU, Sharif S, Farid S, Iqbal H, Khan SI. High performance liquid chromatographic-diode array detector method for simultaneous determination of aspirin, caffeine and ephedrine in weight loss formulations, human plasma and in vitro drug-drug interaction studies. J Anal Chem. 2020;75(12):1589–98.
Li W, Terry RN, Tang J, Feng MR, Schwendeman SP, Prausnitz MR. Rapidly separable microneedle patch for the sustained release of a contraceptive. Nat Biomed Eng. 2019;3(3):220–9.
Ren L, Pan S, Li H, Li Y, He L, Zhang S, et al. Effects of aspirin-loaded graphene oxide coating of a titanium surface on proliferation and osteogenic differentiation of MC3T3-E1 cells. Sci Rep. 2018;8:15143–55.
Wang Y, Wang C, Li K, Song X, Yan X, Yu L, et al. Recent advances of nanomedicine-based strategies in diabetes and complications management: diagnostics, monitoring, and therapeutics. J Control Release. 2021;330:618–40.
Wang QL, Zhu DD, Liu XB, Chen BZ, Guo XD. Microneedles with controlled bubble sizes and drug distributions for efficient transdermal drug delivery. Sci Rep. 2016;6:38755–65.
Yang S, Wu F, Liu J, Fan G, Welsh W, Zhu H, et al. Phase-transition microneedle patches for efficient and accurate transdermal delivery of insulin. Adv Funct Mater. 2015;25(29):4633–41.
Zhao X, Zhang S, Yang G, Zhou Z, Gao Y. Exploring trehalose on the release of levonorgestrel from implantable PLGA microneedles. Polymers. 2020;11:59–75.
Battisti M, Vecchione R, Casale C, Pennacchio FA, Lettera V, Jamaledin R, et al. Non-invasive production of multi-compartmental biodegradable polymer microneedles for controlled intradermal drug release of labile molecules. Front Bioeng Biotechnol. 2019;7:296–309.
Mittal A, Malhotra D, Jain P, Kalia A, Shunmugaperumal T. Studies on aspirin crystals generated by a modified vapor diffusion method. AAPS PharmSciTech. 2016;17(4):988–94.
He M, Yang G, Zhang S, Zhao X, Gao Y. Dissolving microneedles loaded with etonogestrel microcrystal particles for intradermal sustained delivery. J Pharm Sci. 2018;107(4):1037–45.
Ho MJ, Jeong HT, Im SH, Kim HT, Lee JE, Park JS, et al. Design and in vivo pharmacokinetic evaluation of triamcinolone acetonide microcrystals-loaded PLGA microsphere for increased drug retention in knees after intra-articular injection. Pharmaceutics. 2019;11(8):419–34.
Cao S, Wang Y, Wang M, Yang X, Tang Y, Pang M, et al. Microneedles mediated bioinspired lipid nanocarriers for targeted treatment of alopecia. J Control Release. 2021;329:1–15.
Abedi F, Razavi BM, Hosseinzadeh H. A review on gentisic acid as a plant derived phenolic acid and metabolite of aspirin: comprehensive pharmacology, toxicology, and some pharmaceutical aspects. Phytother Res. 2020;34(4):729–41.
Acknowledgements
The authors are grateful to the Antimicrobial Testing Center of the Technical Institute of Physics and Chemistry, CAS, for guiding us in conducting in vivo animal imaging.
Funding
This research was funded by the STS Project of the Chinese Academy of Sciences (grant number KFJ-STS-QYZD-182).
Author information
Authors and Affiliations
Contributions
The manuscript was written by Baorui Wang. Baorui Wang, Han Liu, Aguo Cheng, Chenxin Yan, and Bo Xu all contributed to the experiments. Suohui Zhang and Yunhua Gao supervised the project.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal study protocols were approved by the Institutional Animal Care and Utilization Committee of the Technical Institute of Physics and Chemistry, CAS (approval numbers—IACUC-IPC-22045, IACUC-IPC-22053, and IACUC-IPC-22061; approval dates—25 June 2022, 16 August 2022, and 30 August 2022).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, B., Liu, H., Zhang, S. et al. Aspirin microcrystals deposited on high-density microneedle tips for the preparation of soluble polymer microneedles. Drug Deliv. and Transl. Res. 13, 2639–2652 (2023). https://doi.org/10.1007/s13346-023-01343-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01343-6