Abstract
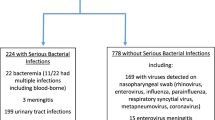
Fever is one of the most common presenting complaints among infants brought to pediatric emergency. Although most of the infants have benign, self-limiting viral infections, approximately 10% of all may have serious bacterial infection. Clinical examination alone is insufficient to detect serious bacterial infection in well appearing infants, and a standardized approach is always sought for. However, guidelines used in the United States or European countries may not be applicable in a tropical country like India. Deviation from these guidelines leads to challenges of unwarranted hospitalization and antibiotic usage, extra cost of care and risk of antimicrobial resistance. Various prediction rules can detect a low risk infant with negative predictive values ranging from 93.7–100%. While use of biomarkers such as C reactive protein and procalcitonin can be reliable, it is costly and may not be applicable to the local population. Validation studies over varied population are needed in future.
Similar content being viewed by others
References
Balmuth F, Henretig FM, Alpern ER. Fever. In: RG Bachur and KN Shaw (eds.) Fleisher & Ludwig’s Textbook of Pediatric Emergency Medicine, 7th edition. Lippincott Williams and Wilkins. 2016. p. 176–85.
Mace SE, Gemme SR, Valente JH, et al. Clinical policy for well-appearing infants and children younger than 2 years of age presenting to the emergency department with fever. Ann Emerg Med. 2016;67:625–39.
Biondi EA, Byington CL. Evaluation and management of febrile, well appearing young infants. Infect Dis Clin North Am. 2015;29:575–85.
Furyk JS, Swann O, Molyneux E. Systematic review: Neonatal meningitis in the developing world. Trop Med Int Health. 2011;16:672–79.
BaraffL J, Bass JW, Fleisher GR, et al. Practice guideline for the management of infants and children 0 to 36 months of age with fever without source. Agency for Healthcare Policy and Research. Ann Emergency Med. 1993;22:1198–210.
For Academic College of Emergency Experts in India (ACEE-INDIA) — INDO US Emergency and Trauma Collaborative, Mahajan P, Batra P, Thakur N, et al. Consensus Guidelines on Evaluation and Management of the Febrile Child Presenting to the Emergency Department in India. Indian Pediatr. 2017;54:652–60.
Kozel TR, Burnham-Marusich AR. Point-of-Care testing for infectious diseases: Past, present, and future. J Clin Microbiol. 2017;55:2313–20.
Meehan WP, Fleegler E, Bachur RG. Adherence to guidelines for managing the well-appearing febrile infant: Assessment using a case-based, interactive survey. Pediatr Emerg Care. 2010;26:875–80.
Baskin MN, O’Rourke EJ, Fleisher GR. Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone. J Pediatr. 1992;120:22–7.
Baker MD, Bell LM, Avner JR. Outpatient management without antibiotics of fever in selected infants. N Engl J Med. 1993;329:1437–41.
Powell KR. Evaluation and management of febrile infants younger than 60 days of age. Pediatr Infect Dis J. 1990;9:153–7.
Rogers AJ, Kuppermann N, Anders J, et al. Practice variation in the evaluation and disposition of febrile infants ≥ 60 days of age. J Emerg Med. 2019;56:583–91.
Powell EC, Mahajan PV, Roosevelt G, et al. Febrile Infant Working Group of the Pediatric Emergency Care Applied Research Network (PECARN). Epidemiology of bactere-mia in febrile infants aged 60 days and younger. Ann Emerg Med. 2018;71:211–6.
Scarfone R, Murray A, Gala P, Balamuth F. Lumbar puncture for all febrile infants 29–56 days old: A retrospective cohort reassessment study. J Pediatr. 2017;187:200–5.
Chua KP, Neuman MI, McWilliams JM, Aronson PL. Febrile Young Infant Research Collaborative. Association between clinical outcomes and hospital guidelines for cerebrospinal fluid testing in febrile infants aged 29–56 days. J Pediatr. 2015;167:1340–46.
Wallace SS, Brown DN, Cruz AT. Prevalence of concomitant acute bacterial meningitis in neonates with febrile urinary tract infection: A retrospective cross-sectional study. J Pediatr. 2017;184:199–203.
Poletto E, Zanetto L, Velasco R, Da Dalt L, Bressan S. Bacterial meningitis in febrile young infants acutely assessed for presumed urinary tract infection: A systematic review. Eur J Pediatr. 2019;178:1577–87.
Aronson PL, Thurm C, Williams DJ, et al. Febrile Young Infant Research Collaborative. Association of clinical practice guidelines with emergency department management of febrile infants >56 days of age. J Hosp Med. 2015;10:358–65.
Aronson PL, Thurm C, Alpern ER, et al., Febrile Young Infant Research Collaborative. Variation in care of the febrile young infant <90 days in US pediatric emergency departments. Pediatrics. 2014;134:666–67.
Aronson PL, Wang ME, Shapiro ED, et al. Risk stratification of febrile infants ≥ 60 days old without routine lumbar puncture. Pediatrics. 2018;142:e20181879.
McCarthy PL, Sharpe MR, Spiesel SZ, et al. Observation scales to identify serious illness in febrile children. Pediatrics. 1982;70:802–9.
Nigrovic LE, Mahajan PV, Blumberg SM, et al. The Yale Observation Scale score and the risk of serious bacterial infections in febrile infants. Pediatrics. 2017;140:e20170695.
Lyons TW, Garro AC, Cruz AT, et al. Performance of the modified Boston and Philadelphia criteria for invasive bacterial infections. Pediatrics. 2020;145:e20193538.
Kuppermann N, Dayan PS, Levine DA, et al. A clinical prediction rule to identify febrile infants 60 days and younger at low risk for serious bacterial infections. JAMA Pediatr. 2019;173:342–51.
Pulliam PN, Attia MW, Cronan KM. C-reactive protein in febrile children 1 to 36 months of age with clinically undetectable serious bacterial infection. Pediatrics. 2001;108:1275–9.
Grendel D, Raymond J, Coste J, et al. Comparison of procalcitonin with C-reactive protein, interleukin-6 and interferon-alpha for differentiation of bacterial versus viral infections. Pediatr Infect Dis J. 1999;18:875–81.
Grendel D, Bohuon C. Procalcitonin as a marker of bacterial infection. Pediatr Infect Dis J. 2000;19:679–88.
Jaye DL, Waites KB. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J. 1997;16:735–46.
Dandona P, Nix D, Wilson MF, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994;79:1605–8.
Van Rossum AMC, Wulkan RW, Oudesluys-Murphy AM. Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis. 2004;4:620–30.
Olaciregui I, Hernandez U, Muñoz JA, Emparanza JI, Landa JJ. Markers that predict serious bacterial infection in infants under 3 months of age presenting with fever of unknown origin. Arch Dis Child. 2009;94:501–5.
Mintegi S, Bressan S, Gomez B, et al. Accuracy of a sequential approach to identify young febrile infants at low risk for invasive bacterial infection. Emerg Med J. 2014;31:e19–24.
Gomez B, Mintegi S, Bressan S, Da Dalt L, Gervaix A, Lacroix L. Validation of the “step-by-step” approach in the management of young febrile infants. Pediatrics. 2016;138:e20154381.
Galetto-Lacour A, Zamora SA, Andreola B, et al. Validation of a laboratory risk index score for the identification of severe bacterial infection in children with fever without source. Arch Dis Child. 2010;95:968–73.
Mahajan P, Kuppermann N, Mejias A, et al. Association of RNA biosignatures with bacterial infections in febrile infants aged 60 days or younger. JAMA. 2016;316:846–57.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors
PB, PM: conceived the idea; VB, PB: drafted the manuscript; PM: reviewed it critically. All authors approved the final version of manuscript, and are accountable for all aspects related to the study.
Funding
None
Competing interest
None stated.
Rights and permissions
About this article
Cite this article
Bhaskar, V., Batra, P. & Mahajan, P. Identifying Serious Bacterial Infections in Febrile Young Infants. Indian Pediatr 58, 15–19 (2021). https://doi.org/10.1007/s13312-021-2089-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-021-2089-6