Abstract
Infections, in particular pneumonia, are common complications in patients with acute stroke and are associated with a less favorable neurologic and functional outcome. Patients with severe stroke and dysphagia are at highest risk of infection. Experimental and clinical data suggest stroke-induced immunodeficiency as a major factor contributing to the high incidence of infection after stroke. Preclinical studies support the potential benefit of preventive antibiotic therapy in acute stroke for lowering the incidence of infection and improving clinical outcome. Several smaller clinical trials on preventive antibiotic therapy in patients with stroke conducted during the last 10 years yielded inconclusive results. Recently, 2 large, open-label, controlled trials failed to demonstrate an improved clinical outcome after preventive antibiotic therapy in patients with acute stroke treated in specialized stroke units. In the “Preventive Antibiotics in Stroke Study”, antibiotic therapy lowered the rate of infection but did not influence outcome. In the STROKE-INF study, performed in patients with dysphagia after stroke, antibiotic therapy did not lower the incidence of pneumonia and had no prognostic significance. At present, preventive antibiotic therapy cannot be recommended as a therapeutic option for acute stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although stroke is a major cause of death and permanent disability, most patients are not eligible for specific therapies with proven benefit currently available. To date, there is no evidence-based treatment for hemorrhagic stroke. Treatment in a dedicated stroke unit per se has been associated with a better outcome [1]. However, it is not known which factors actually contribute to the improved prognosis associated with treatment in a stroke unit, as most therapies and interventions performed daily in stroke units lack solid scientific evidence, underscoring the need for new therapies. Within this context, over the last few years, prophylactic antibiotic therapy has emerged as a promising new therapy for patients with acute stroke. If proven effective, it could be easily performed without causing copious expenses, a need for additional manpower, or much discomfort for the patient. After several clinical studies performed during the last 10 years have produced negative or inconclusive results, however, the enthusiasm for prophylactic antibiotic therapy in acute stroke has now plummeted considerably. After the negative results of 2 large clinical trials—the STROKE-INF [2] and PASS [3] trials published in 2015—an editorial commentator mused that the concept of preventive antibiotic therapy after stroke may have utterly “PASSed away” [4].
The present review discusses the rationale behind the concept of preventive antibiotic therapy in acute stroke, provides an overview on the evidence from controlled trials, and gives an overview over the current status of discussion along with clinical implications.
Methods
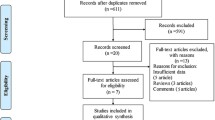
For this narrative clinical review, all randomized controlled trials on preventive antibiotic versus control therapy in stroke were searched using the Medline (1966–April 2016) and Cochrane databases. In an effort to identify further published, unpublished, and ongoing trials, the ClinicalTrials.gov (www.clinicaltrials.gov) and Stroke Trials Registry (www.strokecenter.org/trials) research and trial registers were searched. Reference lists of retrieved relevant articles were scanned. Trials conducted in all languages were searched, and translations for trial reports published in languages other than English were arranged. Each study was assessed for key methodological issues.
Rationale Behind Prophylactic Antibiotic Therapy in Stroke
The relationship between infection and stroke is bidirectional. Precedent infection is a well-recognized risk factor for ischemic, as well as hemorrhagic, stroke [5–7]. However, infection is a frequent complication in patients with acute stroke, and associated with a worse prognosis. Indeed, infection is the most common complication during the acute treatment of patients with stroke, and is a leading cause of death after stroke [6,8]. The frequency of infection in patients with acute stroke has been the subject of numerous clinical studies. Owing to different designs, patient selection criteria, diagnostic criteria, timing of assessment, and duration of follow-up, the results vary considerably, with a reported incidence of infection up to 90 % [9–13]. Almost all studies described pneumonia as the most frequent type of infection after stroke, followed by urinary tract infection [6]. Studies regarding the effects of infection on worsening stroke symptoms have yielded ambiguous results [14]. While several studies could not demonstrate an independent association between infection and worsening of neurological deficit after stroke [15–17], the majority of studies showed that infections in hospitalized patients in the acute phase after stroke are associated with a worse functional outcome and increased mortality [6,18–20]. In the largest study, Katzan et al. [21] described a 30-day mortality of 27 % after poststroke pneumonia compared with a mortality rate of 4 % in patients without pneumonia. In many studies, the extent to which confounding factors such as severity and size of stroke, other comorbidity, fever, and medical interventions contribute to the worse prognosis after infection is not easily distinguished. Therefore, it remains to be seen whether infection is an independent predictor of a less favorable outcome, although, on the whole, the association between infection and a worse prognosis is undisputed.
Various risk factors for infection after stroke such as severe neurological deficit at presentation, bedridden state, older age, and dysphagia have been described [6,20].
During the last few years, findings from animal models of focal ischemia, as well as clinical studies, have led to the concept of poststroke immunosuppression, which is being covered by other articles in this special issue of Neurotherapeutics and has also been subject to various extensive reviews [22–24]. Stroke-induced immunodeficiency via the hypothalamic axis and the sympathetic nervous system can be detected as early as a few hours after cerebral ischemia and may persist over a few weeks. Owing to various alterations of the cell-mediated immune response, susceptibility to infections in patients with acute stroke is increased, probably contributing to the high incidence of infection after stroke [22–24].
Infection is also the main cause of fever, which has consistently been associated with a worse prognosis after stroke. In recent years, the prognostic importance of body temperature during the acute phase of ischemic stroke has been increasingly recognized. Several clinical studies have consistently shown that in the early phase after stroke, fever (>37.5 °C) is very common, occurring in up to 61 % of patients, increases with the severity of stroke, and is a strong predictor of an unfavorable outcome [25–27]. A multitude of different biochemical and inflammatory mechanisms responsible for the detrimental effects of fever during the acute phase of stroke have been identified, including 1) enhanced release of excitatory neurotransmitters; 2) increased metabolic demands; 3) exaggerated free oxygen radical production; 4) increased breakdown of the blood–brain barrier; 5) elevated rate of potentially damaging depolarizations in the ischemic penumbra; 6) impaired recovery of energy metabolism and enhanced inhibition of protein kinases; and 7) worsening of cytoskeletal proteolysis [28]. As a consequence, current guidelines recommend lowering fever in patients with acute stroke [29].
However, in many patients, symptomatic treatment of fever is difficult and frequently delayed. Several small studies on antipyretic medication in febrile patients after stroke, most frequently using acetaminophen in various combinations, were either not at all or only moderately effective in lowering fever, and could not demonstrate valid effects on clinical outcome [30–32]. Invasive catheter-based heat exchange systems influence body temperature more effectively but may not be suitable for the general stroke unit setting, owing to technical and staff requirements, possible complications, and the substantial costs of this invasive technique requiring insertion of a large catheter into the femoral artery and propagation of the heat exchange device into the inferior vena [33–37]. Given the prognostic significance of fever and the limitations of its current symptomatic treatment options, it appears reasonable to ascertain and treat the causes of fever, and, if possible, to prevent its occurrence altogether.
The concept of prophylactic antibiotic therapy for patients with an excess risk of infection is not innovative. Preventive antibiotic therapy is routinely performed in patients with severe immunodepression, for example in patients with severe leukopenia due to chemotherapy, or in people with AIDS following HIV infection. In selected surgical patient collectives with high risk of infection, prophylactic antibiotic therapy has been the subject of various studies, yielding heterogeneous results [38–40]. To date, only a few studies have investigated the effect of prophylactic antibiotic therapy in patients with acute severe central nervous system disease other than stroke. A randomized study in patients with severe head trauma showed reduced incidence of ventilator-associated pneumonia under prophylactic therapy with Cefuroxim, although this strategy has not yet been implemented into the general care of patients with head trauma [41]. In an animal model of focal cerebral ischemia, preventive antibiotic therapy improved markers of pneumonia and functional outcome [42]. However, animal studies of poststroke infection should be viewed with caution as observed inflammatory and infectious changes could also result from surgical and anaesthetic stress [43].
Clinical Studies on Preventive Antibiotic Therapy After Stroke
Key characteristics of the number of controlled clinical studies on prophylactic antibiotic therapy in stroke performed during the last 20 years are summarized in Table 1. Inclusion criteria, criteria for diagnosis of infection, antibiotic therapy, and primary outcomes varied greatly. Therefore, comparability of these studies is severely limited. Nonetheless, 3 meta-analyses of the studies (published until 2008), written by the same group of authors, and predictably reaching comparable results, have already been published [52–54]. Not surprisingly, one of the authors’ main conclusions was that the studies were heterogeneous [54]. To add to the confusion, a small number of controlled studies using Minocycline after acute stroke have to be considered [46,49–51]. In these studies, minocycline, a second-generation tetracycline derivative that is not a first- or second-line antibiotic for most infections commonly present after stroke, was used not to prevent infections but to analyze its potential neuroprotective properties. Although the rationale behind minocycline treatment was not to prevent infections, minocycline may influence numerous inflammatory processes after stroke and has antibacterial properties that—somehow unintentionally—may prevent bacterial infection [55,56]. Almost all available clinical studies suffer from various limitations and at least some degree of potential bias. Most studies, including the newest and largest studies, were open-label. Although usually various attempts were made to standardize the diagnosis of infection, this problem remains a considerable source of bias as the presence of infection cannot always easily be established in clinical practice.
In 1982, Majkowski et al. [57] conducted a first, relatively large clinical study on prophylactic antibiotic therapy in patients with stroke. This study, published in a Polish-language journal during the Cold War, was not widely recognized at the time. In total, 103 patients were randomized for treatment as usual or antibiotic therapy with either ampicillin or penicillin over 10 days. The authors observed lower rates of infection in the 2 groups receiving preventive treatment. However, owing to several problems with the design of the study and description of the findings, the validity of the results remains questionable. Unfortunately, the same is true for the study by Santangelo et al. [44] (n.b., this study is occasionally incorrectly cited as “De Falco et al.”; in fact, De Falco was the senior author). In their paper, many crucial details of the study design were not sufficiently explained, such as duration and dosage of antibiotic therapy, observation period, and randomization procedures. In light of these drawbacks, the positive results from this study must be interpreted with great caution.
The first study using a design complying with modern standards was the “Early Systemic Prophylaxis of Infection After Stroke” (ESPIAS) study [45]. This was a large, well-designed controlled study. Perhaps unwisely, Chamorro et al. [45] used levofloxacin, a third-generation, extended-spectrum (“respiratory”) fluoroquinolone antibiotic, an antibiotic that was new at the time when this study was being planned. Interestingly, its primary outcome was the difference in infection rate between the 2 groups. After the disappointing results of their study became evident, the authors mentioned that the safety of levofloxacin had never been explored in patients with stroke, that there might be inhibitory effects of levofloxacin on γ-aminobutyric acid neurotransmission or, on the contrary, that glutaminergic effects could be responsible for the unexpected negative effect on treatment outcome in the active treatment group [58]. Another methodological problem of this study was that patients with ischemic, as well as hemorrhagic, stroke were included. The study was prematurely stopped following an interim futility analysis. Rate of early infection (within the first 7 days of stroke) was not different. Disturbingly, patients in the active treatment group had a worse outcome after 90 days.
In our “Mannheim Infection in Stroke Study” (MISS) [47], the primary outcome parameter was not infection but the incidence and height of fever as one of the pivotal risk factors for a worse outcome after stroke. We included 60 severely affected, bedridden patients with acute ischemic stroke. Active treatment was sulbactam plus mezlocillin over 4 days. As expected, antibiotic therapy reduced fever and rate of infection. Although the study was not powered to detect prognostic benefits, we were able to show that after 90 days outcome was better after active treatment. The main limitations of this study were its small sample size and the open-label design.
Also in 2008, Harms et al. [48] published the results of the PANTHERIS trial, a small (n = 80) controlled, randomized study on moxifloxacin in patients with moderate-to-severe ischemic stroke. Active treatment was associated with a lower rate of early infection (the primary endpoint of the study). However, the authors found no difference in clinical outcome after 180 days. The authors discussed the potential superiority of moxifloxacin compared with other antibiotic drugs. At the time of this study, moxifloxacin, a fourth-generation fluoroquinolone with—compared with older fluoroquinolone generations—improved activity against Gram-positive bacteria and anaerobes, was being heavily promoted. However, owing to rare but potentially life-threatening liver and skin complications, moxifloxacin has in some way fallen from grace. In 2011, the Food and Drug Administration also added box warnings owing to the risk of tendinitis, including tendon rupture, and of worsening symptoms from myasthenia gravis; in Europe, the European Medicines Agency ruled that moxifloxacin can only be prescribed when other antibiotics have failed or cannot be administered.
The 4 studies on minocycline after acute stroke are not discussed in detail here [46,49–51] (see Table 1). Remarkably, these studies, aimed at neuroprotection after stroke, used a narrower time window than the other studies on prevention of infection. Within the framework of these studies infection was, in fact, not of major concern, and was not monitored. Three of 4 studies reported an association of minocycline treatment with improved clinical outcome. However, owing to their small sample size and other methodological problems, these promising results now have to be replicated by a larger phase III trial.
In 2015, 2 large studies on preventive antibiotic therapy after stroke yielded negative results, undoubtedly, at least for the time being, putting the final nails in the coffin of the concept of prophylactic antibiotic therapy in stroke.
The “Preventive Antibiotics in Stroke Study” (PASS) was a well-designed, large multicenter study conducted in 30 stroke units in the Netherlands [3]. Over a 4-year period, 2550 patients were assigned to prophylactic Ceftriaxone or treatment as usual. The study was open label; assessment of outcome parameters was performed by blinded evaluators. Primary outcome was functional outcome after 3 months as assessed with the modified Rankin Scale. Unfortunately, the authors again failed to detect differences between the 2 groups regarding the primary endpoint. Prophylactic antibiotic treatment was, however, associated with a lower rate of infection (18 % vs 10 %). This effect was mainly driven by a lower rate of urinary tract infection; rates of pulmonary infection were similar between the ceftriaxone and control group. In a post-hoc subgroup analysis, the authors reported improved outcomes after treatment with antibiotics in patients receiving intravenous thrombolysis. Critical points of this study included an overall low rate of infection, inclusion of patients with very mild stroke [median National Institutes of Health Stroke Scale (NIHSS) score 5], and open-label design with risk of detection bias regarding infection.
The latest study on prophylactic antibiotic therapy after stroke was the STROKE-INF trial on prophylactic antibiotics after acute stroke for reducing pneumonia in patients with stroke-associated dysphagia [2]. Patients with dysphagia after stroke have the greatest risk of developing pneumonia. This was a large multicenter trial conducted in 48 stroke units in the UK. Over a period of 6 years, the stroke units were randomly assigned to standard care or prophylactic antibiotic therapy. For intention-to-treat analysis, 1217 patients were clustered within 37 units. The main inclusion criteria were dysphagia within 48 h of onset of ischemic or hemorrhagic stroke. Antibiotic therapy with different drugs was continued over 7 days. The primary endpoint was diagnosis of pneumonia in the first 14 days after stroke according to a (masked) standardized diagnostic algorithm, and by physician diagnosis. Overall, the authors found no difference in the incidence of algorithm-based diagnosis of pneumonia between the active treatment and control group (13 % vs 10 %). On the whole, however, the incidence of pneumonia was lower than reported in previous studies. After 14 days, NIHSS score was slightly but significantly higher in the active treatment group (11.7 vs 10.1). Interestingly, patients in the active treatment group also tended to have a longer hospital stay. Finally, there were no positive effects from antibiotic prophylaxis on a number of additional secondary outcome parameters assessed by the authors. The STROKE-INF trial was a large, well-conducted study. However, potential selection bias in a cluster-randomized trial, and diagnostic bias due to open-intervention allocation cannot be completely ruled out.
In summary, current evidence from controlled studies did not show improved clinical outcomes after prophylactic antibiotic therapy following stroke. With regard to prevention of early infection after stroke, however, the results are ambiguous.
Discussion
The most obvious explanation of the generally negative findings reported by controlled studies on prophylactic antibiotic therapy after acute stroke is the fact that this therapy simply does not work, despite the reasonable rationale behind this therapy and a rather large body of compelling evidence from preclinical studies.
There are, however, a number of potential reasons possibly explaining the disappointing results on preventive antibiotic therapy after stroke. The most plausible explanation is that in almost all studies, patients were managed in specialist, state-of-the art stroke units. In this setting, prophylactic antibiotics obviously may not add to existing preventive measures such as general hygiene precautions, early mobilization, positioning, regular suction, swallowing techniques, modified diet, and early initiation of antibiotics in patients with suspected infection [2]. Infections after stroke most likely result from complex interactions of bacterial, chemical, mechanical (e.g., indwelling catheters), and immunological mechanisms that might not be prevented by antibiotics alone [2].
Moreover, in daily clinical practice, a low threshold for initiating antibiotic therapy may occur, leading to unintended “prophylactic” antibiotic treatment in a considerable number of patients. Compared with older studies, incidence of infection in the trials on prophylactic antibiotic therapy was generally lower, which may underscore this point. The diagnosis of infection in patients with stroke is not trivial. Algorithm-based diagnosis of infection may lead to markedly different results than physician-diagnosed infection [2]. In particular, diagnosing pneumonia in acute stroke poses challenges, and chest X-rays are of limited use in the early stages of pneumonia. In a study on how pneumonia is diagnosed in clinical stroke research, Kishore et al. [59] found considerable variation in terminology and diagnostic approach. In one study, inter-rater reliability for diagnosing pneumonia after hemorrhagic stroke was disturbingly low (k = 0.3), despite the use of standardized diagnostic criteria [60]. At present, there is no established gold standard for diagnosing pneumonia in patients with acute stroke. Recently, a “Pneumonia in Stroke Consensus Group” published recommendations for operational criteria for the diagnosis of pneumonia, largely based on Centers for Disease Control criteria for pneumonia [61]. Regarding urinary tract infection, the second frequent infection after stroke, it is frequently difficult to distinguish clinically relevant infection from asymptomatic colonization, in particular in patients with indwelling bladder catheters. In the studies on antibiotic prophylaxis after stroke, definitions for infection were heterogeneous which also impairs the comparability of their results [54].
In most studies, the time window before start of preventive antibiotic therapy was considerably long—up to 48 h after stroke—which may be too long, bearing in mind the immunological mechanisms and immunodepression taking effect immediately after the stroke [22]. Studies on the prognostic significance of hyperthermia have demonstrated that the first 24 h constitute the crucial period that determines most of the detrimental consequences of hyperthermia after stroke [62,63]. Furthermore, duration of preventive antibiotic therapy (3–7 days) in the clinical trials may have been too short to prevent secondary infection [64].
It could also be argued that most studies did not include the ideal candidates who could benefit most from antibiotic prophylactic therapy. Most authors found that the incidence of infection after stroke is highest in severely ill patients [18,65]. Thus, only severely ill patients who carry the highest risk for infection should be considered as candidates for prophylactic antibiotic treatment. In contrast to this assumption, many studies included patients with very mild stroke. In the largest study, the PASS trial [3], a NIHSS score of 1 was sufficient to be included in the study, for example. As a consequence, the overall median NIHSS in this study was only 5, indicating that the majority of study participants suffered from mild stroke. Not surprisingly, the overall incidence of infection in this study was low. It is difficult to imagine how patients with very mild stroke, for example, with a slight hypoesthesia at 1 extremity only, might benefit from prophylactic antibiotic therapy. A rather large sample would be necessary to demonstrate beneficial effects from prophylactic therapy in a population with only a small event rate. Furthermore, negative side effects from antibiotic therapy would probably gain more weight if the majority of patients would be treated unnecessarily. Thus, in future studies, only severely ill patients who carry the highest risk for infection should be considered as candidates for prophylactic antibiotic treatment. At the same time, however, the STROKE-INF study [2], which included only patients with dysphagia, who are without a doubt at high risk for pulmonary infection, preventive antibiotic therapy did not affect incidence of infection. In this light, it appears questionable whether meta-analyses or subgroup analyses of pooled patient data from the—overall negative—trials would identify a certain subgroup of patients who could be selected for future trials.
A methodological problem of most studies—including the 2 largest trials—was incomplete blinding. Patients and their treating physicians were aware of treatment allocation which may have been a source of diagnostic bias. The authors of most studies attempted to overcome this problem by various methods to assess or re-evaluate the diagnosis of infection by a blinded evaluator. It is doubtful, however, that blinding could be successfully maintained in all instances.
Finally, the choice of the antibiotic drug may be of importance. The choice of the optimum antibiotic drug for infections in patients with acute stroke remains hypothetical. Chamorro et al. [45] hypothesized that harmful central nervous system effects of levofloxacin may have been responsible for the negative results of their study. To date, there have been no controlled studies on the potentially differential effects of antibiotic drugs in patients with acute stroke. Following theoretical considerations, it may not be wise to use fluoroquinolones with glutaminergic effects such as ciprofloxacine or levofloxacine as first-line drugs in patients with acute stroke. Some antibiotics, in particular minocycline [55,56], and also β-lactam antibiotics such as ceftriaxone, used in the PASS trial [3], may exert neuroprotective properties [66,67]. Although the rate of complications from antibiotic drug therapy was almost negligible in most studies, the choice of antibiotic drug influences unwanted side effects from treatment. Fluoroquinolones, for example, have been associated with QT prolongation [68,69], which renders these drugs not preferable in patients with stroke, who often suffer from cardiac comorbidity. Despite their excellent efficacy, broad antibacterial spectrum and good tolerability, cephalosporins, which rapidly induce drug-resistant bacteria, are arguably not the ideal drugs for preventive therapy [70,71]. Previous studies on prophylactic antibiotic treatment in other settings did not support the assumption that short-term prophylactic antibiotic drug treatments facilitate the development of antibiotic drug resistance [38,72]. However, if antibiotic prophylaxis should be implemented into the daily routine of stroke units, and large numbers of patients would be treated with the same antibiotic drugs within a single ward, the development of drug resistance could constitute a point of concern. The studies on preventive antibiotic therapy mentioned either no complications from antibiotic treatment at all, or, equally implausible, a very low incidence of mostly minor side effects, conceivably a consequence of insufficient adverse event monitoring. In the majority of studies, systematic microbiological monitoring including analysis of antibiotic resistance or screening for Clostridium difficile infections following prophylactic antibiotic therapy was not employed.
Conclusions
Based on the body of evidence from clinical studies currently available, the use of prophylactic antibiotic therapy in patients suffering from acute stroke and treated in specialized stroke units cannot be recommended. Prophylactic antibiotic therapy may arguably reduce the incidence of infection but does not influence clinical outcome. In my opinion, it seems highly unlikely that the concept of preventive antibiotic therapy may be reanimated in the near future. Theoretically, studies with a more tailored approach using stricter inclusion criteria and including biomarkers might identify patients who could benefit from preventive antibiotic therapy after stroke. However, after the negative results of the PASS and STROKE-INF trials, I doubt that such studies will be initiated in the near future.
Regarding the prognostic significance of infection after stroke, admission into a special stroke unit, close monitoring for early signs of infection according to standardized criteria, and immediate treatment after the diagnosis of infection has been established seem to be the most judicious recommendations.
References
Stroke Unit Trialists Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013;9:CD000197.
Kalra L, Irshad S, Hodsoll J, et al. Prophylactic antibiotics after acute stroke for reducing pneumonia in patients with dysphagia (STROKE-INF): a prospective, cluster-randomised, open-label, masked endpoint, controlled clinical trial. Lancet 2015;386:1835-1844.
Westendorp WF, Vermeij JD, Zock E, et al. The Preventive Antibiotics in Stroke Study (PASS): a pragmatic randomised open-label masked endpoint clinical trial. Lancet 2015;385:1519-1526.
Meisel A. Preventive antibiotic therapy in stroke: PASSed away? Lancet 2015;385:1486-1487.
Grau AJ, Urbanek C, Palm F. Common infections and the risk of stroke. Nat Rev Neurol 2010;6:681-694.
Emsley HC, Hopkins SJ. Acute ischaemic stroke and infection: recent and emerging concepts. Lancet Neurol 2008;7:341-353.
Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke 2003;34:2518-2532.
Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol 2010;9:105-118.
Friedant AJ, Gouse BM, Boehme AK, et al. A simple prediction score for developing a hospital-acquired infection after acute ischemic stroke. J Stroke Cerebrovasc Dis 2015;24:680-686.
Johnston KC, Li JY, Lyden PD, et al. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. RANTTAS Investigators. Stroke 1998;29:447-453.
Kalra L, Yu G, Wilson K, Roots P. Medical complications during stroke rehabilitation. Stroke 1995;26:990-994.
Bamford J, Dennis M, Sandercock P, Burn J, Warlow C. The frequency, causes and timing of death within 30 days of a first stroke: the Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatry 1990;53:824-829.
Heuschmann PU, Kolominsky-Rabas PL, Roether J, et al. Predictors of in-hospital mortality in patients with acute ischemic stroke treated with thrombolytic therapy. JAMA 2004;292:1831-1838.
Chamorro A, Urra X, Planas AM. Infection after acute ischemic stroke: a manifestation of brain-induced immunodepression. Stroke 2007;38:1097-1103.
Kammersgaard LP, Jorgensen HS, Reith J, et al. Early infection and prognosis after acute stroke: the Copenhagen Stroke Study. J Stroke Cerebrovasc Dis 2001;10:217-221.
Vargas M, Horcajada JP, Obach V, et al. Clinical consequences of infection in patients with acute stroke: is it prime time for further antibiotic trials? Stroke 2006;37:461-465.
Dziewas R, Ritter M, Schilling M, et al. Pneumonia in acute stroke patients fed by nasogastric tube. J Neurol Neurosurg Psychiatry 2004;75:852-856.
Aslanyan S, Weir CJ, Diener HC, Kaste M, Lees KR. Pneumonia and urinary tract infection after acute ischaemic stroke: a tertiary analysis of the GAIN International trial. Eur J Neurol 2004;11:49-53.
Vermeij FH, Scholte op Reimer WJ, de Man P, et al. Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: data from the Netherlands Stroke Survey. Cerebrovasc Dis 2009;27:465-471.
Ionita CC, Siddiqui AH, Levy EI, Hopkins LN, Snyder KV, Gibbons KJ. Acute ischemic stroke and infections. J Stroke Cerebrovasc Dis 2011;20:1-9.
Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003;60:620-625.
Famakin BM. The immune response to acute focal cerebral ischemia and associated post-stroke immunodepression: a focused review. Aging Dis 2014;5:307-326.
Chamorro A, Meisel A, Planas AM, Urra X, van de Beek D, Veltkamp R. The immunology of acute stroke. Nat Rev Neurol 2012;8:401-410.
Kamel H, Iadecola C. Brain-immune interactions and ischemic stroke: clinical implications. Arch Neurol 2012;69:576-581.
Rocco A, Pasquini M, Cecconi E, et al. Monitoring after the acute stage of stroke: a prospective study. Stroke 2007;38:1225-1228.
Caplan L. Intracerebral haemorrhage. Lancet 1992;339:656-658.
Hajat C, Hajat S, Sharma P. Effects of poststroke pyrexia on stroke outcome: a meta-analysis of studies in patients. Stroke 2000;31:410-414.
Ginsberg M, Busto R. Combating hyperthermia in acute stroke. Stroke 1998;29:529-534.
Jauch EC, Saver JL, Adams HP, Jr., et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870-947.
Sulter G, Elting JW, Maurits N, Luyckx GJ, De Keyser J. Acetylsalicylic acid and acetaminophen to combat elevated body temperature in acute ischemic stroke. Cerebrovasc Dis 2004;17:118-122.
Dippel DW, van Breda EJ, van der Worp HB, et al. Effect of paracetamol (acetaminophen) and ibuprofen on body temperature in acute ischemic stroke PISA, a phase II double-blind, randomized, placebo-controlled trial [ISRCTN98608690]. BMC Cardiovasc Disord 2003;3:2.
Kasner SE, Wein T, Piriyawat P, et al. Acetaminophen for altering body temperature in acute stroke: a randomized clinical trial. Stroke 2002;33:130-134.
De Georgia MA, Krieger DW, Abou-Chebl A, et al. Cooling for Acute Ischemic Brain Damage (COOL AID): a feasibility trial of endovascular cooling. Neurology 2004;63:312-317.
Georgiadis D, Schwarz S, Kollmar R, Schwab S. Endovascular cooling for moderate hypothermia in patients with acute stroke: first results of a novel approach. Stroke 2001;32:2550-2553.
Linares G, Mayer SA. Hypothermia for the treatment of ischemic and hemorrhagic stroke. Crit Care Med 2009;37:S243-249.
Choi HA, Badjatia N, Mayer SA. Hypothermia for acute brain injury--mechanisms and practical aspects. Nat Rev Neurol 2012;8:214-222.
Badjatia N. Hyperthermia and fever control in brain injury. Crit Care Med 2009;37:S250-257.
van Nieuwenhoven CA, Buskens E, van Tiel FH, Bonten MJ. Relationship between methodological trial quality and the effects of selective digestive decontamination on pneumonia and mortality in critically ill patients. JAMA 2001;286:335-340.
Barker FG, 2nd. Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery 2002;51:391-400.
Gumaste V. Prophylactic antibiotic therapy in the management of acute pancreatitis. J Clin Gastroenterol 2000;31:6-10.
Sirvent JM, Torres A, El-Ebiary M, Castro P, de Batlle J, Bonet A. Protective effect of intravenously administered cefuroxime against nosocomial pneumonia in patients with structural coma. Am J Respir Crit Care Med 1997;155:1729-1734.
Hetze S, Engel O, Romer C, et al. Superiority of preventive antibiotic treatment compared with standard treatment of poststroke pneumonia in experimental stroke: a bed to bench approach. J Cereb Blood Flow Metab 2013;33:846-854.
Campos-Martorell M, Ma Angeles M, Hernandez-Guillamon M, et al. Rat middle cerebral artery occlusion is not a suitable model for the study of stroke-induced spontaneous infections. PLOS ONE 2014;9:e99169.
Santangelo R, Majello L, Angelone P, de Falco FA. La profilassi antibiotica migliora l'outcome nello stroke ischemico. Riv Neurobiol 1998;44:63-67.
Chamorro A, Horcajada JP, Obach V, et al. The Early Systemic Prophylaxis of Infection After Stroke study: a randomized clinical trial. Stroke 2005;36:1495-1500.
Lampl Y, Boaz M, Gilad R, et al. Minocycline treatment in acute stroke: an open-label, evaluator-blinded study. Neurology 2007;69:1404-1410.
Schwarz S, Al-Shajlawi F, Sick C, Meairs S, Hennerici MG. Effects of prophylactic antibiotic therapy with mezlocillin plus sulbactam on the incidence and height of fever after severe acute ischemic stroke: the Mannheim infection in stroke study (MISS). Stroke 2008;39:1220-1227.
Harms H, Prass K, Halle E, Dirnagl U, Meisel A. Preventive antibacterial therapy in stroke - Results of the PANTHERIS trial. Cerebrovasc Dis 2007;23(Suppl. 2):10.
Padma Srivastava MV, Bhasin A, Bhatia R, et al. Efficacy of minocycline in acute ischemic stroke: a single-blinded, placebo-controlled trial. Neurol India 2012;60:23-28.
Kohler E, Prentice DA, Bates TR, et al. Intravenous minocycline in acute stroke: a randomized, controlled pilot study and meta-analysis. Stroke 2013;44:2493-2499.
Amiri-Nikpour MR, Nazarbaghi S, Hamdi-Holasou M, Rezaei Y. An open-label evaluator-blinded clinical study of minocycline neuroprotection in ischemic stroke: gender-dependent effect. Acta Neurol Scand 2015;131:45-50.
Westendorp WF, Nederkoorn PJ, Vermeij JD, Dijkgraaf MG, Van de Beek D. Post-stroke infection: a systematic review and meta-analysis. BMJ Neurol 2011;11:110.
van de Beek D, Wijdicks EF, Vermeij FH, et al. Preventive antibiotics for infections in acute stroke: a systematic review and meta-analysis. Arch Neurol 2009;66:1076-1081.
Westendorp WF, Vermeij JD, Vermeij F, et al. Antibiotic therapy for preventing infections in patients with acute stroke. Cochrane Database Syst Rev 2012;1:CD008530.
Vedatam S, Moller AR. Minocycline: a novel stroke therapy. J Neurol Stroke 2015;2:00073.
Fagan SC, Cronic LE, Hess DC. Minocycline development for acute ischemic stroke. Transl Stroke Res 2011;2:202-208.
Majkowski J, Kunicka J, Szabelska K, Cendrowski W. Profilaktyczne stosowanie penicyliny G i ampicyliny w udarach mozgowych. I. Obserwacje Kliniczne. Neurol Neurochir Pol 1982;16:261-267.
Dodd PR, Davies LP, Watson WE, et al. Neurochemical studies on quinolone antibiotics: effects on glutamate, GABA and adenosine systems in mammalian CNS. Pharmacol Toxicol 1989;64:404-411.
Kishore AK, Vail A, Chamorro A, et al. How is pneumonia diagnosed in clinical stroke research? A systematic review and meta-analysis. Stroke 2015;46:1202-1209.
Naidech AM, Liebling SM, Duran IM, Moore MJ, Wunderink RG, Zembower TR. Reliability of the validated clinical diagnosis of pneumonia on validated outcomes after intracranial hemorrhage. J Crit Care 2012;27:527.
Smith CJ, Kishore AK, Vail A, et al. Diagnosis of Stroke-associated pneumonia: Recommendations from the Pneumonia in Stroke Consensus Group. Stroke 2015;46:2335-2340.
Koennecke HC, Leistner S. Prophylactic antipyretic treatment with acetaminophen in acute ischemic stroke: a pilot study. Neurology 2001;57:2301-2303.
Diringer MN. Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med 2004;32:559-564.
Silvestri L, van Saene HK, Milanese M, Ros S, Zandstra DF. Parenteral antibiotics are not enough to prevent pneumonia in stroke. Lancet 2015;386:653.
Nakagawa T, Sekizawa K, Arai H, Kikuchi R, Manabe K, Sasaki H. High incidence of pneumonia in elderly patients with basal ganglia infarction. Arch Intern Med 1997;157:321-324.
Rothstein JD, Patel S, Regan MR, et al. Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature 2005;433:73-77.
Lipski J, Wan CK, Bai JZ, Pi R, Li D, Donnelly D. Neuroprotective potential of ceftriaxone in in vitro models of stroke. Neuroscience 2007;146:617-629.
Carbon C. Comparison of side effects of levofloxacin versus other fluoroquinolones. Chemotherapy 2001;47(Suppl. 3):9-14.
Stahlmann R. Clinical toxicological aspects of fluoroquinolones. Toxicol Lett 2002;127:269-277.
Rybak MJ. Resistance to antimicrobial agents: an update. Pharmacotherapy 2004;24:203S-215S.
Pfeifer Y, Cullik A, Witte W. Resistance to cephalosporins and carbapenems in Gram-negative bacterial pathogens. Int J Med Microbiol 2010;300:371-379.
Krueger WA, Lenhart FP, Neeser G, et al. Influence of Combined intravenous and topical antibiotic prophylaxis on the incidence of infections, organ dysfunctions, and mortality in critically ill surgical patients: a prospective, stratified, randomized, double-blind, placebo-controlled clinical trial. Am J Respir Crit Care Med 2002;166:1029-1037.
Acknowledgments
I have received an unrestricted research grant from Pfizer, the manufacturer of Sulbactam, for conducting 1 of the antibiotic drug studies on prevention of infection with antibiotics after stroke (MISS study). I have no other potential conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
13311_2016_466_MOESM1_ESM.pdf
Required Author Forms Disclosure forms provided by the authors are available with the online version of this article. (PDF 1224 kb)
Rights and permissions
About this article
Cite this article
Schwarz, S. Prophylactic Antibiotic Therapy for Preventing Poststroke Infection. Neurotherapeutics 13, 783–790 (2016). https://doi.org/10.1007/s13311-016-0466-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-016-0466-y