Abstract
Hospitals in Europe produce approximately 6 million tons of medical waste annually, about one-third of this originating in operating rooms. Most of it is solid waste, which can be recycled if bodily fluids do not contaminate it. Only 2–3% of hospital waste must be disposed of as infectious waste, and this is much lower than the 50–70% of garbage in the biohazard waste stream. In June 2021, at the main operating room of the Department of General Surgery of the University of Turin, we began a separate collection program for materials consisting of plastic, paper, TNT (material not contaminated by bodily fluids), and biohazardous waste. We calculated the number of boxes and the weight of special waste disposed produced every month in one operating room for 18 months. The monthly number of Sanibox and the monthly weight of biohazardous waste decreased during the observation period. The reduction trend was not constant but showed variations during the 18 months. Direct proportionality between number of low-complexity procedures and production of biohazardous waste was found (p = 0.050). We observed an optimization in the collection and filling of plastic, paper and TNT boxes separated and sent for recycling. One of the barriers to recycling hospital waste, and surgical waste in particular, is the failure to separate infectious waste from clean waste. A careful separate collection of waste in the operating room is the first step in reducing environmental pollution and management costs for the disposal of hospital waste.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hospitals in Europe produce approximately 6 million tons of medical waste annually [1] about one-third of this originating in operating rooms. In the United States, hospitals rank second in waste generation, with more than 4 billion tons of waste produced in a year [2]. Infect, the National Health System (NHS) is responsible for 8–10% of total greenhouse gas emissions [3, 4]. All of this affects climate change, which is a major threat to public health in the twenty-first century [5]. Has been estimated that the impact in annual CO2 production in an operating theatre in a university hospital in the UK is equivalent to the production generated by the energy consumption of more than 2000 homes [6]. Surgery is an equipment-intensive and waste-intensive specialty since all equipment must be sterile to various standards. For this reason, the trend has been toward an increase in disposable equipment—though other choices often exist, including reusable and reprocessing equipment. Many types of equipment may be purchased in a disposable or reusable form. Traditionally, the choice focused on cost, patient safety, efficacy and ease of use—however, it has not included environmental considerations. Disposable equipment has become increasingly popular because they easily eliminate the risk of cross-contamination between patients. Hospitals are the largest emitters of carbon dioxide, so greener health care will have a great positive impact on the environment [7].
More recent estimates suggest that operating rooms are responsible for 60–70% [8, 9] of hospital waste. The packaging material used to protect and maintain the sterility of supplies and equipment accounts for a large part of the waste. Also, the increased use of disposable supplies and equipment contributes to the problem. Infectious material, sharps and certain medications, which are hazardous to the environment, must be discarded into special containers and fall under the category of Regulated Medical Waste (RMW).
Most of the material generated in the operating room (OR) is solid waste, which can be recycled if bodily fluids do not contaminate it. One of the barriers to recycling is the failure to separate infectious waste from clean waste. Concern regarding infectious contamination has been one of the most significant barriers to fully capturing recyclable material from the OR. However, with only the recycling of non-contaminated material, the share of biohazardous waste could be reduced. Many pieces of surgical equipment and anaesthesia supplies are made from recyclable materials such as plastic, paper, glass and metal. Most of the general operating room waste can be recycled by educating operating room staff on how to properly separate and dispose of this material.
Interest in the reuse or recycling of medical waste is growing globally [10, 11]. In fact, increasingly medical centres are attempting to establish recycling programs for material product in the operating rooms and medical procedure units. This is not only to have environmental benefits, but also because reducing hospital waste disposal costs saves money, generating potential financial savings for hospitals [12]. The dissemination within surgical eques of knowledge about the carbon footprint resulting from their work and how it can be reduced is necessary [13].
Therefore, by modifying the collection and disposal of room material, generating containers of recoverable materials, we expect to obtain considerable economic savings for the hospital but above all a reduction in the environmental impact. In fact, biohazardous waste is mainly disposed of in incinerators that produce increased CO2 emission. According to the Environmental Protection Agency (EPA), incinerated medical waste is a major source of dioxins and the main polluter of mercury [14, 15]. Reducing this type of waste would notably reduce the carbon footprint.
In Italy, the management of hospital waste is regulated by Presidential Decree DPR 254/2003. This represents the implementing regulation of Legislative Decree 22/1997. Hazardous medical waste with an infectious risk must be disposed of by thermal destruction in authorized facilities, as stipulated in Article 10. In April 2006, Legislative Decree D.LGS 152/2006 came into force and states that waste management is revaluated from the perspective of European directives. According to this decree, it is the responsibility of public administrations to promote the life cycle analysis of products based on uniform methodologies.
However, the climate emergency requires the implementation of effective measures to reduce the environmental impact of the health care system, which has become one of the main goals of the 2021 COP26 (XXVI United Nations Climate Change Conference, Glasgow 2021) [16].
This manuscript presents the results of a pilot study conducted in our Department of General Surgery at the University of Turin (Italy) aimed at implementing careful waste collection and separation in the operating room, with the objective of evaluating the extent of biohazard waste reduction achieved by a mere behavioural modification.
Materials and methods
This pilot project was executed in collaboration with the Technical University Delft and OR waste recycling consortium “GreenCycl” in the Netherlands. This collaboration provided practical examples for the creation of our “Green Team” and provided guidelines about recognizing and selecting valuable waste streams and to disseminate knowledge to the OR staff and sterilization department [17].
We formed our “Green Team”, a group of professional figures (two surgeon, one anesthesiologist, one head nurse, two hospital managers) who possessed the knowledge about sustainability. The Green Team's program was based on five pillars, or "5Rs": Reduce, Reuse, Recycle, Rethink and Research [18]. The "Green Team”, through meetings and dissemination of materials explained to the OR staff the various procedures to be performed and implemented for proper waste sorting in the operating room. The “Green Team” also was constantly updating and held meetings to keep all the OR staff updated.
In June 2021, at a single operating room of the Department of General Surgery, we started a separate collection program for materials consisting of plastic, paper, TNT (non-woven fabric), material not contaminated by bodily fluids, and biohazardous material (disposed of in containers called "Sanibox"). All bins had the same capacity (60 L) and have been arranged for the differentiated collection of materials within the entire operating room. Signs have been placed, on each bin, with indications on which material to dispose of in each of them. The separated waste was disposed of not as hospital waste but following the recycling chain.
The number of containers and their weight were counted day by day as well as the surgical activity and the type of procedures performed.
In the 18 months of observation, from June 2021 to November 2022, data were collected regarding the numbers of containers filled with the different waste materials produced in our main operating room, carefully separated: plastic, paper, TNT, non-recyclable material with body fluid contamination disposed of in special containers (Sanibox) as required by law (RMW). The weight of the Sanibox was provided by the company responsible for the disposal of biohazardous medical waste.
An analysis was also conducted on the number and type of surgeries performed. Throughout the observation period, the surgeries procedures performed were 1369. The procedures were divided into high complexity 520 (hemicolectomy, hepatectomy, pancreatectomy, rectum anterior resection, sleeve gastrectomy, gastric bypass, etc.), medium complexity 359 (cholecystectomy, incisional hernia repair, small bowel resection, gastric fundoplication, Heller-Dor procedure, etc.) and low complexity 490 (hernia repair, appendectomy, anal fistulectomy, hemorrhoidectomy, etc.) surgeries. Laparoscopy and laparotomy procedures were included. Robotic procedures were not included. We have divided the surgeries solely according to complexity, because for each degree of complexity the material used in the OR is almost standardized. The intraoperative protocols and materials used were not changed during this period. The health personnel involved has always been the same.
As for descriptive statistics, the categorical variables were reported as absolute/relative frequencies, while the continuous ones as median/IQR (Inter Quartile Range). As for inferential analyses, the bins collection over time have been considered as independent data and, after having recoded as tertiles both the months of collections and the different complexity procedures the Kruskal–Wallis test (a non-parametric analysis of variance) was applied.
All p-values were obtained using the two-sided exact method, at the conventional 5% significance level. Data were analyzed as of November 2023 by R 4.3.2 (R Foundation for Statistical Computing, Vienna-A, http://www.R-project.org).
Due to its explorative nature, no formal sample size determination has been planned for this pilot study. Due to the observational nature of this research, and in accordance with Italian law (Agenzia Italiana del Farmaco-AIFA, Guidelines for observational studies, 20 March 2008), no formal approval from the local Institutional Review Board/Independent Ethics Committee was needed.
Results
The project started in June 2021. The number and percentage of the surgical procedures (Table 1) has been almost constant during these 18 months except for low complexity surgical interventions, which saw their maximum peaks in October 2021, February, March and June 2022 (Fig. 1).
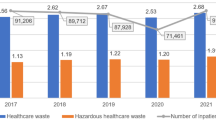
The monthly number of Sanibox and the monthly weight of biohazardous waste decreased during the observation period (Table 2). The reduction trend was not constant but showed variations during the 18 months (Figs. 2, 3). The median number of boxes of special waste disposed passed from 120 in the first tertile (0–6 months) to 95 in the third tertile (13–18 months). Assessing the median in the three tertiles shows a reduction in the third tertile, but not statistically significant (p = 0.481). The median monthly weight of the same waste decreased from 297,06 kg in the first tertile (0–6 months) to 164.30 kg in the third tertile (13–18 months). This decrease is also not constant and not statistically significant (p = 0.238) (Table 3). This was the waste disposed of as regulated medical waste. This reduction is more evident in the last months of the period under examination (August–November 2022) as it became necessary to correctly and meticulously disseminate the guidelines to be followed. Similarly, there was a reduction in the median number of paper bins (p = 0.049). The median number of plastic bins had an interesting reduction trend but without statistical association (p = 0.456). The median number of TNT bins remained constant over time.
Peaks of production of number and weight of Sanibox bins were observed in those months in which more low complexity procedures were completed. This would suggest a direct proportionality between number of low-complexity procedures and production of biohazardous waste.
Very interesting is what emerged from the stratified analysis of the complexity of surgical procedures (Tables 4, 5, 6).
Considering high complexity surgeries, plastic waste decreases as the number of these surgeries decreases (p = 0.012) (Fig. 4). For the other types of waste, no statistical association has been found.
For medium-complexity surgeries, as their number decreases, there is a statistically significant reduction in the number of Saniboxes (p = 0.034) (Fig. 5) and a reduction in the weight of biohazardous waste, even not statistically supported (p = 0.156).
For last category, a direct association was observed between the number of low-complexity surgeries and other the number of Saniboxes (p = 0.046), or the weight of biohazardous waste (p = 0.050) (Fig. 6).
Discussion
Surgical waste is a worldwide growing phenomenon, increasing CO2 emissions. The growing carbon footprint results in climate changes such as global warming that impacts public health primarily through the redistribution of infectious diseases. By 2030, the World Health Organization (WHO) has predicted 250,000 more deaths per year because of climate change [5].
Each surgical operation generates 3.5–8.4 kg [19, 20] of plastic waste with 20% high-quality polypropylene (PP). The increasing number of surgical interventions adds to millions of kilograms of surgical waste yearly [21, 22]. Moreover, surgical waste causes a significant financial burden for hospitals (depending on waste processing contracts). In our hospital, "A.O.U. Città della Salute e della Scienza di Torino (Molinette)", the price per kg for the disposal service of biohazardous waste is equal to 1.24 euro/kg + VAT. Due to lacking knowledge of circular waste management in healthcare, the waste accumulation problem is rarely addressed [10, 12, 23]. Hospitals manage their medical waste in different ways and any coordination program is fading, where there would be a need to adopt shared and "virtuous" measures. Consequently, technical innovation for optimal and shared surgical waste recycling and socio-economic analysis monitoring is necessary to accelerate the circular transition in the healthcare domain. Unfortunately, at present, there are still few projects and actions to achieve this goal.
Furthermore, medical waste poses a potential threat to employees, patients, and surrounding communities [24]. It is, therefore, important to reduce the volume of medical waste to reduce potentially dangerous effects [19]. To do this, it is necessary to develop a “circular economy” program which reduces biohazardous waste by promoting the recycling of non-contaminated materials. Doing so would not only reduce environmental pollution but also reduce the cost of waste management by hospitals [25, 26]. Within our pilot study, we reduced the processing and incineration costs related to biohazard fees with 3483.41 Euro + VAT. At the same time, we reduced the CO2 emission (CO2e) significantly. 1 kg of biohazardous waste generates approximately 2.8 kg of CO2e when being transported and incinerated [25]. Since in total 2809.2 kg was saved from incineration during the pilot, 1265.04 kg of CO2e was saved. Each kilo of plastic, paper and TNT that is recycled saves approximately 0.5 kg, 0.15 kg, and 0.58 kg of CO2e, respectively. If we now look at the total amount of plastic, paper and TNT saved from incineration with 580.5 kg, 739.2 kg, and 1489.5 kg, respectively, we saved 290.25 kg, 110.88 kg, and 863.91 kg of CO2e in total related to using recycled plastics and paper for new products by hospital mining (Table 7). This emerged from a single operating room. More significant results would be obtained if we applied this protocol to all operating rooms of our hospital.
The support of the hospital health management is essential, which by sharing and supporting the project can provide legislative indications, economic feedback and monitor the complex “assembly chain” (from the collection and sorting of waste in the operating room to its disposal). By virtue of all this, we have initiated a national pilot project on this issue.
As a first step, we undertook a web meeting with Delft University and GreenCycle, pioneers in this field, from which we exported all their experience and organization. Subsequently, we established a “Green Team”, which sensitized the operating room staff on the subject and suggested and followed the implementation of simple measures in waste management without additional costs on their management. We found of primary importance to have regular meetings between "Green Team" members. During these meetings there were updates, exchanges of knowledge and opinions, feedback on the work done. Aiming at the reduction of the production of biohazardous waste favored by a careful and scrupulous differentiated collection in the operating theatre. The “Green Team” is essential for carrying out this activity, as coordination and as a group of professionals who are always up to date and ready to intervene in case of problems [7]. This led to a constant and progressive reduction in the production of biohazardous waste, mainly in the last months of the study, by which time the system had run in, and all the staff knew what to do and how to do it. Separate waste collection in the operating room and minimum effort on the part of all staff have promoted a reduction in environmental pollution and economic savings on the part of the hospital. All of this was done without jeopardizing the safety of patients and staff, without changing treatment strategies and the types of operations performed. The behavioral changes were welcomed by all health care staff with enthusiasm and interest, as the changes were minimal for a major achievement. In addition, the outreach work of the “Green Team” was of paramount importance to achieve this.
Another point to discuss and on which much awareness is needed is the optimization of the filling of the Sanibox. At the beginning of the study, as in previous years, the Sanibox were closed and disposed of even if not full. At the end of the period under review, Sanibox decreased significantly compared to the previous number, although not reaching statistical significance (p = 0.482).
In addition, we looked at the types and numbers of surgeries performed, which did not change during the 18 months of observation. A direct proportionality has emerged between the increase in minor surgery and number of the sanibox and biohazardous waste (p = 0.046; p = 0.050). In fact, minor surgeries are shorter and consequently, the number of those performed in a day is higher. This leads to increased waste, mainly contaminated waste, favouring increased biohazardous waste. Most of the contaminated waste consists of surgical drapes (drapes placed on the patient), gauze and everything needed to monitor the patient's cardio-circulatory activity during surgery. Major surgical interventions, having a longer duration and not requiring continuous changes of the patient's drapes.
Several studies in the literature emphasize how crucial it is to reduce the environmental pollution generated in the operating room [2] and how effective it can be to address the problem "from within." [25]. There are still no studies that show clear and concrete data as reported here.
The carbon footprint generated by the disposal of hospital waste is a very current problem. Throughout the world, efforts are being made to change the attitude of operating room staff and encourage the recycling of materials not contaminated by biological fluids thus reducing CO2e [26]. Providing clear numerical data such as those presented could further raise awareness among this topic all healthcare professionals.
This study has several intrinsic limitations. It is a retrospective observational analysis based only on data from a single operating room over a short period of time. In addition, it was partly conditioned by the contextual Covid pandemic, which in some months forced a considerable reduction in surgical activity. Nevertheless, it represents aim interesting and encouraging starting point because it demonstrates that with the differentiation of non-contaminated material it is possible to obtain a reduction of biohazardous waste.
Conclusion
Environmental pollution is a global problem that must be tackled seriously and drastically. Hospital waste, especially biohazard waste, largely contributes to carbon footprint by changing the Earth's climate structure and contributing to the cost of its disposal. Within a short pilot demonstrated that minor surgery procedure directly contributes significantly to the biohazardous waste mass and volume. In our experience, it has emerged that behaviour change in the operating room can be established by introducing a recycling program. This drastically reduced the CO2e footprint related to incineration of biohazardous waste, while promoting economic savings for the hospitals.
Data availability
The data in the study are available for consultation.
References
ECHAlliance https://echalliance.com/hospitals-produce-tonnes-of-plastic-waste-annually-how-can-they-reduce-this/
Guetter CR, Williams BJ, Slama E, Arrington A, Henry MC, Möller MG, Tuttle-Newhall JE, Stein S, Crandall M (2018) Greening the operating room. Am J Surg 216(4):683–688. https://doi.org/10.1016/j.amjsurg.2018.07.021. (Epub 2018 PMID: 30055807)
McGain F, Muret J, Lawson C, Sherman JD (2020) Environmental sustainability in anaesthesia and critical care. Br J Anaesth 125(5):680–692. https://doi.org/10.1016/j.bja.2020.06.055
MacNeill AJ, Lillywhite R, Brown CJ (2017) The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 1(9):e381–e388. https://doi.org/10.1016/S2542-5196(17)30162-6
Beloeil H, Albaladejo P (2021) Initiatives to broaden safety concerns in anaesthetic practice: the green operating room. Best Pract Res Clin Anaesthesiol 35(1):83–91. https://doi.org/10.1016/j.bpa.2020.07.010. (Epub 2020 Jul 24 PMID: 33742580)
Gordon D (2020) Sustainability in the operating room: reducing our impact on the planet. Anesthesiol Clin 38(3):679–692. https://doi.org/10.1016/j.anclin.2020.06.006.PMID:32792191;PMCID:PMC7416086
Pietrabissa A, Pugliese L, Filardo M, Marconi S, Muzzi A, Peri A (2022) My OR goes green: surgery and sustainability. Cir Esp (Engl Ed) 100(6):317–319. https://doi.org/10.1016/j.cireng.2022.06.013.PMID:35718371;PMCID:PMC9212941
Kwakye G, Brat GA, Makary MA (2011) Green surgical practices for health care. Arch Surg 146(2):131–136. https://doi.org/10.1001/archsurg.2010.343. (PMID: 21339421)
Albert MG, Rothkopf DM (2015) Operating room waste reduction in plastic and hand surgery. Plast Surg (Oakv) 23(4):235–238. https://doi.org/10.4172/plastic-surgery.1000941
Van Straten B, Dankelman J, Van der Eijk A, Horeman T (2020) A circular healthcare economy; a feasibility study to reduce surgical stainless steel waste. Sustain Product Consump 27:169–175
Pinjing H, Fan L, Hua Z, Liming S (2013) Reference to the circular economy as a guiding principle. Waste Resour 37:144
Voudrias EA (2018) Healthcare waste management from the point of view of circular economy. Waste Manag 75:1–2. https://doi.org/10.1016/j.wasman.2018.04.020. (PMID: 29699811)
Akinocho EM, Ashraf M, Badirou N, Philippe HJ (2023) Knowledge of surgeons and practical stances of healthcare institutions in the Ile-de-France region toward sustainable development: a cross-sectional study. J Visc Surg. https://doi.org/10.1016/j.jviscsurg.2022.12.011
Melamed A (2003) Environmental accountability in perioperative settings. AORN J 77(6):1157–1168. https://doi.org/10.1016/s0001-2092(06)60978-2. (PMID: 12817740)
Wyssusek KH, Keys MT, van Zundert AAJ (2019) Operating room greening initiatives - the old, the new, and the way forward: a narrative review. Waste Manag Res 37(1):3–19. https://doi.org/10.1177/0734242X18793937. (Epub 2018 Aug 22 PMID: 30132405)
Pradere B, Mallet R, de La Taille A, Bladou F, Prunet D, Beurrier S, Bardet F, Game X, Fournier G, Lechevallier E, Meria P, Matillon X, Polguer T, Abid N, De Graeve B, Kassab D, Mejean A, Misrai V, Pinar U, Sustainability Task Force of the French Association of Urology (2023) Climate-smart actions in the operating theatre for improving sustainability practices: a systematic review. Eur Urol 83(4):331–342. https://doi.org/10.1016/j.eururo.2022.01.027
Van Straten B, Alvino L, Horeman T (2023) Creating a circular healthcare economy: circular strategies for sustainable healthcare. Book Delft University of Technology
Hutchins DC, White SM (2009) Coming round to recycling. BMJ 338:b609. https://doi.org/10.1136/bmj.b609. (PMID: 19278971)
McGain F, Story D, Hendel S (2009) An audit of intensive care unit recyclable waste. Anaesthesia 64(12):1299–1302. https://doi.org/10.1111/j.1365-2044.2009.06102.x
Li CS, Jenq FT (1993) Physical and chemical composition of hospital waste. Infect Control Hosp Epidemiol 14(3):145–150. https://doi.org/10.1086/646700. (PMID: 8478527)
Statistiek CBvd. Operaties in het ziekenhuis, 2010. 25-02-2018 [Available from: http://statline.cbs.nl/Statweb/publication/?DM=SLNL&PA=80386NED&D1=0,2-5&D2=0&D3=0&D4=a&D5=10,l&HDR=T&STB=G4,G1,G2,G3&VW=T.
Statline. Medisch Specialistische Zorg; DBC's naar diagnose, zorgkenmerken, 2015. 15-08-2018.
van Straten B, Robertson PD, Oussoren H, Pereira Espindola S, Ghanbari E, Dankelman J, Picken S, Horeman T (2021) Can sterilization of disposable face masks be an alternative for imported face masks? A nationwide field study including 19 sterilization departments and 471 imported brand types during COVID-19 shortages. PLoS ONE 16(9):e0257468. https://doi.org/10.1371/journal.pone.0257468.PMID:34520503;PMCID:PMC8439445
Mesfin D, Assemu D, Tafere T, Gelaw Y, Bantie G (2020) Healthcare waste management practice and associated factors among private and public hospitals of Bahir Dar city administration. J Environ Public Health. https://doi.org/10.1155/2020/7837564
Azouz S, Boyll P, Swanson M, Castel N, Maffi T, Rebecca AM (2019) Managing barriers to recycling in the operating room. Am J Surg 217(4):634–638. https://doi.org/10.1016/j.amjsurg.2018.06.020. (Epub 2018 Jun 23 PMID: 29958657)
Talibi SS, Scott T, Hussain RA (2022) The environmental footprint of neurosurgery operations: an assessment of waste streams and the carbon footprint. Int J Environ Res Public Health 19(10):5995. https://doi.org/10.3390/ijerph19105995.PMID:35627532;PMCID:PMC9141268
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
NL designed the study, acquired data and analyzed data, drafted the article and approved its final version. GS acquired data and analyzed data, drafted the article and approved its final version. FO acquired data, revised the article and approved its final version. TH revised the article and approved its final version. RP, analyzed data, drafted and revised the article and approved its final version. AA analyzed data, drafted and revised the article and approved its final version. MM designed the study, analyzed and interpreted data, revised the article and approved its final version.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare they have nothing to disclose. Authors declare there are no conflicts of interest.
Consent for publication
No source of founding or research and/or publication.
Compliance with Ethical Standards, Research involving human participants and/or animals
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leone, N., Scozzari, G., Olandese, F. et al. “O.R. GOES GREEN”: a first step toward reducing our carbon footprint in the operating room and hospital. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01793-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01793-8