Abstract
The right middle lobe often poorly expands after right upper lobectomy. Postoperative pulmonary function may be inferior after right upper lobectomy than after right lower lobectomy due to poor expansion of the middle lobe. This study examined the difference in the postoperative right middle lobe expansion and pulmonary function between right upper and right lower lobectomy. Patients who underwent right upper or right lower lobectomy through video-assisted thoracic surgery (n = 82) were enrolled in this retrospective study. Pulmonary function tests and computed tomography were performed preoperatively and at 1 year postoperatively. Using three-dimensional computed tomography volumetry, the preoperative and postoperative lung volumes were measured, and the predicted postoperative forced expiratory volume in 1 s was calculated. Middle lobe volume ratio (i.e., ratio of the postoperative to the preoperative middle lobe volume) and the postoperative forced expiratory volume in 1 s ratio (i.e., ratio of the measured to the predicted postoperative forced expiratory volume in 1 s) were compared between right upper and right lower lobectomy. Compared with the patients who underwent right upper lobectomy (n = 50), those who underwent right lower lobectomy (n = 32) had significantly higher middle lobe volume ratio (1.15 ± 0.32 vs. 1.63 ± 0.52, p < 0.001) and postoperative forced expiratory volume in 1 s ratio (1.12 ± 0.12 vs. 1.19 ± 0.13, p = 0.010). The right middle lobe showed more expansion and better recovery of postoperative pulmonary function after right lower lobectomy than after right upper lobectomy.
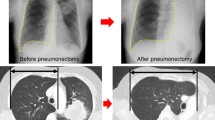
Graphical abstract






Similar content being viewed by others
Data availability
Not applicable.
References
Ueda K, Tanaka T, Hayashi M, Tanaka N, Li TS, Hamano K (2013) Right middle lobe transposition after upper lobectomy: influence on postoperative pulmonary function. Thorac Cardiovasc Surg 61:138–143
Ueda K, Tanaka T, Hayashi M, Li TS, Kaneoka T, Tanaka N et al (2011) Compensation of pulmonary function after upper lobectomy versus lower lobectomy. J Thorac Cardiovasc Surg 142:762–767
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824
Pulmonary Physiology Expert Committee TJRS (2001) The standard value of spirogram and arterial blood gas partial pressure in Japanese people. J Jpn Resp Soc 39:1–37
Ueda K, Hayashi M, Tanaka N, Tanaka T, Hamano K (2014) Long-term pulmonary function after major lung resection. Gen Thorac Cardiovasc Surg 62:24–30
Shibazaki T, Mori S, Harada E, Shigemori R, Kato D, Matsudaira H et al (2021) Measured versus predicted postoperative pulmonary function at repeated times up to 1 year after lobectomy. Interact Cardiovasc Thorac Surg 33:727–733
Yoshimoto K, Nomori H, Mori T, Ohba Y, Shiraishi K, Ikeda K (2011) Combined subsegmentectomy: postoperative pulmonary function compared to multiple segmental resection. J Cardiothorac Surg 6:17
Asakura K, Izumi Y, Kohno M, Ohtsuka T, Okui M, Hashimoto K et al (2011) Effect of cutting technique at the intersegmental plane during segmentectomy on expansion of the preserved segment: comparison between staplers and scissors in ex vivo pig lung. Eur J Cardiothorac Surg 40:34–38
Ueda K, Tanaka T, Hayashi M, Tanaka N, Li TS, Hamano K (2012) Clinical ramifications of bronchial kink after upper lobectomy. Ann Thorac Surg 93:259–265
Seok Y, Cho S, Lee JY, Yang HC, Kim K, Jheon S (2014) The effect of postoperative change in bronchial angle on postoperative pulmonary function after upper lobectomy in lung cancer patients. Interact Cardiovasc Thorac Surg 18:183–188
Kim DH, Moon DH, Kim HR, Lee SM, Chae EJ, Choi CM et al (2019) Effect of inferior pulmonary ligament division on residual lung volume and function after a right upper lobectomy. Interact Cardiovasc Thorac Surg 28:760–766
Sekine Y, Iwata T, Chiyo M, Yasufuku K, Motohashi S, Yoshida S et al (2003) Minimal alteration of pulmonary function after lobectomy in lung cancer patients with chronic obstructive pulmonary disease. Ann Thorac Surg 76:356–361
Kushibe K, Takahama M, Tojo T, Kawaguchi T, Kimura M, Taniguchi S (2006) Assessment of pulmonary function after lobectomy for lung cancer—upper lobectomy might have the same effect as lung volume reduction surgery. Eur J Cardiothorac Surg 29:886–890
Ueda K, Tanaka T, Li TS, Tanaka N, Hamano K (2009) Quantitative computed tomography for the prediction of pulmonary function after lung cancer surgery: a simple method using simulation software. Eur J Cardiothorac Surg 35:414–418
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Clinical registration number
This study was approved by the ethics committee of the Jikei University School of Medicine [approval number: 34-393 (11550)].
Compliance with Ethical Standards, Research involving human participants and/or animals, and Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shibazaki, T., Mori, S., Arakawa, S. et al. Compensatory expansion of the right middle lobe: volumetric and functional analysis of the changes after right upper or lower lobectomy. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01786-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01786-7