Abstract
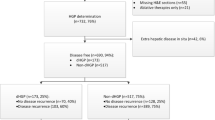
Intrabiliary growth (IG) is an unusual modality for colorectal metastases to spread. Relatively little is known about this condition because large series are lacking. The aim of the study was to compare the surgical and oncological outcomes of patients with or without IG. From 01/2010 to 12/2020, 999 patients underwent hepatectomy for colorectal metastases. Clinicopathological variables were retrospectively analyzed from a prospective-collected database of patients with or without IG. A propensity score matched (PSM) analysis to compare OS and DFS was performed. At first hepatectomy, 29 patients (2.9%) had IG: 7 isolated IG and 22 mixed-type (mass-forming lesion with IG). 4 patients presented IG at repeat hepatectomy for recurrence, of whom 3 had no biliary invasion at initial surgery. IG resulted to be more common in older patients (median age 70 in IG vs 60 years of no-IG, p = 0.004). Mean time from colorectal tumor was longer in IG (20.4 months) than no-IG (12.9 months), p = 0.038. Major hepatectomies (55.2% IG vs 29.7% no-IG, p = 0.003) and anatomic resections (89.7% vs 58.2%, p = 0.001) were more frequently required to treat IG. In 5 (17%) of IG, a resection of main bile duct was performed. Overall postoperative mortality and complications were similar in the two groups, while bile leak was 17.2% IG vs 5.6% no-IG (p = 0.024). Median margin width was comparable in IG (1.4 mm) and no-IG (2 mm). Five-year overall survival (IG 45.9% vs no-IG 44.5%) and Disease-Free Survival (IG 35.9% vs no-IG 36.6%) were similar in the two groups. According to PSM, 145 patients with no-IG were compared to 29 of IG group. After PSM, OS and DFS did not show any statistically significant difference. IG has similar oncological outcomes of resected colorectal metastases without IG, although it affects surgical management.





Similar content being viewed by others
Data availability
Data are available upon request to corresponding author
References
Seshadri RA, Majhi U (2009) Endobiliary metastasis from rectal cancer mimicking intrahepatic cholangiocarcinoma: a case report and review of literature. J Gastrointest Cancer 40(3–4):123–127. https://doi.org/10.1007/s12029-009-9115-6
Estrella JS, Othman ML, Taggart MW, Hamilton SR, Curley SA, Rashid A, Abraham SC (2013) Intrabiliary growth of liver metastases: clinicopathologic features, prevalence, and outcome. Am J Surg Pathol 37(10):1571–1579. https://doi.org/10.1097/PAS.0b013e318293ddf1
Latorre Fragua RA, Manuel Vazquez A, Rodrigues Figueira Y, Ramiro Pérez C, López Marcano AJ, de la Plaza LR, Ramia Ángel JM (2019) Intrabiliary metastases in colorectal cancer: a systematic review. J Hepatobiliary Pancreat Sci 26(7):270–280. https://doi.org/10.1002/jhbp.635
Nagler J, Rochwarger AM (1977) Metastatic colon carcinoma simulating primary bile duct carcinoma via endoscopic cholangiography. Gastrointest Radiol 2(1):75–76. https://doi.org/10.1007/BF02256470
Wenzel DJ, Gaede JT, Wenzel LR (2003) Intrabiliary colonic metastasis mimicking primary biliary neoplasia. AJR Am J Roentgenol 180(4):1029–1032. https://doi.org/10.2214/ajr.180.4.1801029
Zeng H, Xu LB, Wen JM, Zhang R, Zhu MS, Shi XD, Liu C (2015) Hepatocellular carcinoma with bile duct tumor thrombus: a clinicopathological analysis of factors predictive of recurrence and outcome after surgery. Medicine (Baltimore) 94(1):e364. https://doi.org/10.1097/MD.0000000000000364
Chung YE, Kim MJ, Park YN, Choi JY, Pyo JY, Kim YC, Cho HJ, Kim KA, Choi SY (2009) Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 29(3):683–700. https://doi.org/10.1148/rg.293085729
Jinzaki M, Tanimoto A, Suzuki K, Seki T, Satoh Y, Hiramatsu K, Mukai M, Nakanishi I (1997) Liver metastases from colon cancer with intra-bile duct tumor growth: radiologic features. J Comput Assist Tomogr 21(4):656–660. https://doi.org/10.1097/00004728-199707000-00027
Moon SG, Han JK, Kim TK, Kim AY, Kim TJ, Choi BI (2003) Biliary obstruction in metastatic disease: thin-section helical CT findings. Abdom Imaging 28(1):45–52. https://doi.org/10.1007/s00261-001-0191-8
Okano K, Yamamoto J, Moriya Y, Akasu T, Kosuge T, Sakamoto M, Hirohashi S (1999) Macroscopic intrabiliary growth of liver metastases from colorectal cancer. Surgery 126(5):829–834 (PMID: 10568181)
Kubo M, Sakamoto M, Fukushima N, Yachida S, Nakanishi Y, Shimoda T, Yamamoto J, Moriya Y, Hirohashi S (2002) Less aggressive features of colorectal cancer with liver metastases showing macroscopic intrabiliary extension. Pathol Int 52(8):514–518. https://doi.org/10.1046/j.1440-1827.2002.01382.x
Imamura H, Sano K, Sugawara Y, Kokudo N, Makuuchi M (2005) Assessment of hepatic reserve for indication of hepatic resection: decision tree incorporating indocyanine green test. J Hepatobiliary Pancreat Surg 12(1):16–22. https://doi.org/10.1007/s00534-004-0965-9
Ferrero A, Viganò L, Polastri R, Muratore A, Eminefendic H, Regge D, Capussotti L (2007) Postoperative liver dysfunction and future remnant liver: where is the limit? Results of a prospective study. World J Surg 31(8):1643–1651. https://doi.org/10.1007/s00268-007-9123-2
Suda K, Ohtsuka M, Ambiru S, Kimura F, Shimizu H, Yoshidome H, Miyazaki M (2009) Risk factors of liver dysfunction after extended hepatic resection in biliary tract malignancies. Am J Surg 197(6):752–758. https://doi.org/10.1016/j.amjsurg.2008.05.007
Langella S, Russolillo N, Forchino F, Lo Tesoriere R, D’Eletto M, Ferrero A (2015) Impact of obesity on postoperative outcome of hepatic resection for colorectal metastases. Surgery 158(6):1521–1529. https://doi.org/10.1016/j.surg.2015.07.024
Ferrero A, Russolillo N, Langella S, Forchino F, Stasi M, Fazio F, Lo TR (2019) Ultrasound liver map technique for laparoscopic liver resections: perioperative outcomes are not impaired by technical complexity. Updates Surg 71(1):49–56. https://doi.org/10.1007/s13304-019-00646-z
Langella S, Menonna F, Casella M, Russolillo N, Lo Tesoriere R, Alessandro F (2020) Vascular resection during hepatectomy for liver malignancies. Results from a tertiary center using autologous peritoneal patch for venous reconstruction. World J Surg 44(9):3100–3107. https://doi.org/10.1007/s00268-020-05564-5
Nakanuma Y, Sato Y, Harada K, Sasaki M, Xu J, Ikeda H (2010) Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol 2(12):419–427. https://doi.org/10.4254/wjh.v2.i12.419
Pang YY (2002) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2000; 2:333–39. HPB (Oxford) 4(2):99. https://doi.org/10.1080/136518202760378489
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258(1):1–7. https://doi.org/10.1097/SLA.0b013e318296c732
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the international study group of liver surgery. Surgery 149(5):680–688. https://doi.org/10.1016/j.surg.2010.12.002
Görgec B, Benedetti Cacciaguerra A, Lanari J, Russolillo N, Cipriani F, Aghayan D, Zimmitti G, Efanov M, Alseidi A, Mocchegiani F, Giuliante F, Ruzzenente A, Rotellar F, Fuks D, D’Hondt M, Vivarelli M, Edwin B, Aldrighetti LA, Ferrero A, Cillo U, Besselink MG, Abu HM (2021) Assessment of textbook outcome in laparoscopic and open liver surgery. JAMA Surg 156(8):e212064. https://doi.org/10.1001/jamasurg.2021.2064
Sugiura T, Nagino M, Oda K, Ebata T, Nishio H, Arai T, Nimura Y (2006) Hepatectomy for colorectal liver metastases with macroscopic intrabiliary tumor growth. World J Surg 30(10):1902–1908. https://doi.org/10.1007/s00268-006-0205-3
Peungjesada S, Aloia TA, Kaur H, Marcal L, Choi H, Vauthey JN, Loyer EM (2013) Intrabiliary growth of colorectal liver metastasis: spectrum of imaging findings and implications for surgical management. AJR Am J Roentgenol 201(4):W582–W589. https://doi.org/10.2214/AJR.12.9508
Postlewait LM, Squires MH, Kooby DA, Weber SM, Scoggins CR, Cardona K, Cho CS, Martin RC, Winslow ER, Maithel SK (2015) A multi-institutional analysis of 429 patients undergoing major hepatectomy for colorectal cancer liver metastases: The impact of concomitant bile duct resection on survival. J Surg Oncol 112(5):524–528. https://doi.org/10.1002/jso.24035
Povoski SP, Klimstra DS, Brown KT, Schwartz LH, Kurtz RC, Jarnagin WR, Fong Y, Blumgart LH (2000) Recognition of intrabiliary hepatic metastases from colorectal adenocarcinoma. HPB Surg 11(6):383–390. https://doi.org/10.1155/2000/17619
Author information
Authors and Affiliations
Contributions
Conceptualization: SL, SA, NR, AF; Data curation: APL, A-PF, SA; Formal analysis and investigation: SL, NR; Writing—original draft preparation: SA, SL; Writing—review and editing: AF, SL, LD; Supervision: AF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Informed consent
Written informed consent was obtained from all participants.
Research involving human participants
The collection and registration of the original database was performed according to regulations and with the approval of the institutional re-view board of our hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Langella, S., Armentano, S., Russolillo, N. et al. Colorectal metastases with intrabiliary growth: incidence, treatment, and outcomes. Updates Surg 76, 459–469 (2024). https://doi.org/10.1007/s13304-024-01752-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-024-01752-3