Abstract
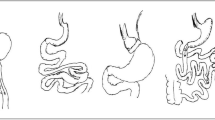
Bariatric surgery (BS) has been as a currently developed treatment of choice for metabolic syndrome (MetS). Which, in turn, is well-known as serious public health concern. Therefore, this study assessed the outcomes of different procedures of BS and possible predictors for improving MetS. This single-center retrospective cohort analysis included bariatric candidates between 2009 and 2017. The operational approach was chosen based on the patient’s condition, as well as the patient’s metabolic profile and the surgeon’s experience. All desired information was evaluated at baseline and 6, 12, and 24 months after the operation. Of the 1111 patients included, 918 (82.6%) were female. There was no considerable trend in the improvement of MetS over the follow-up period of each surgery group. After 6 to 24 months of follow-up, waist circumference reduction was significant in all three types of surgery, and sleeve gastrectomy resulted in the best (but not significant) improvement rates after 24 months (P = 0.079). One anastomosis gastric bypass had highest decrease in percentage of excess weight loss than other procedures (P < 0.001). Each year increase in age was associated with a 4% decrease in MetS remission. In addition, the male gender, was correlated with MetS improvement positively (P = 0.049). Each one-unit increase in hemoglobin A1c (HbA1c) reduced the MetS remission rate by 40%. All three methods of BS were similarly effective in MetS. Consider the predictive value of age, gender, and HbA1c before determining the optimum procedure for each patient is recommended.
Similar content being viewed by others
Data availability
Data of the study will be available based on the request from corresponding author after assessment of the request by all authors.
References
Jammu GS, Sharma R (2016) A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-En-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg 26:926–932
Ji Y, Lee H, Kaura S, Yip J, Sun H, Guan L et al (2021) Effect of bariatric surgery on metabolic diseases and underlying mechanisms. Biomolecules. https://doi.org/10.3390/biom11111582
Quan Y, Huang A, Ye M, Xu M, Zhuang B, Zhang P et al (2015) Efficacy of laparoscopic mini gastric bypass for obesity and type 2 diabetes mellitus: a systematic review and meta-analysis. Gastroenterol Res Pract. https://doi.org/10.1155/2015/152852
Runkel N, Brydniak R (2016) Surgical treatment of metabolic syndrome. Visc Med 32(5):352–356
Fatahi A, Doosti-Irani A, Cheraghi Z (2020) Prevalence and incidence of metabolic syndrome in Iran: a systematic review and meta-analysis. Int J Prev Med. https://doi.org/10.4103/ijpvm.IJPVM_489_18
Wang F-G, Yu Z-P, Yan W-M, Yan M, Song M-M (2017) Comparison of safety and effectiveness between laparoscopic mini-gastric bypass and laparoscopic sleeve gastrectomy: a meta-analysis and systematic review. Medicine. https://doi.org/10.1097/MD.0000000000008924
Roth A, Thornley C, Blackstone R (2020) Outcomes in bariatric and metabolic surgery: an updated 5-year review. Curr Obes Rep 9:380–389
Calvo B, Gracia J, Bielsa M, Martínez M (2020) Metabolic effects and outcomes of sleeve gastrectomy and gastric bypass: a cohort study. Surg Endosc 34:5550–5557
Nassour I, Almandoz JP, Adams-Huet B, Kukreja S, Puzziferri N (2017) Metabolic syndrome remission after Roux-en-Y gastric bypass or sleeve gastrectomy. Diabetes Metab Syndr Obes 10:393–402
Georgiadou D, Sergentanis TN, Nixon A, Diamantis T, Tsigris C, Psaltopoulou T (2014) Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Related Dis 10(5):984–91
Plamper A, Lingohr P, Nadal J, Rheinwalt KP (2017) Comparison of mini-gastric bypass with sleeve gastrectomy in a mainly super-obese patient group: first results. Surg Endosc 31:1156–1162
Kular K, Manchanda N, Rutledge R (2014) Analysis of the five-year outcomes of sleeve gastrectomy and mini gastric bypass: a report from the Indian sub-continent. Obes Surg 24:1724–1728
Kansou G, Lechaux D, Delarue J, Badic B, Le Gall M, Guillerm S et al (2016) Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass: one year outcomes. Int J Surg 33:18–22
Vrakopoulou GZ, Theodoropoulos C, Kalles V, Zografos G, Almpanopoulos K (2021) Type 2 diabetes mellitus status in obese patients following sleeve gastrectomy or one anastomosis gastric bypass. Sci Rep 11(1):4421
Poublon N, Chidi I, Bethlehem M, Kuipers E, Gadiot R, Emous M et al (2020) One anastomosis gastric bypass vs. Roux-en-Y gastric bypass, remedy for insufficient weight loss and weight regain after failed restrictive bariatric surgery. Obes Surg 30:3287–94
Kabir A, Pazouki A, Hajian M (2021) Iran obesity and metabolic surgery (IOMS) cohort study: rationale and design. Indian J Surg. https://doi.org/10.1007/s12262-021-02789-z
Ansar H, Zamaninour N, Pazouki A, Kabir A (2020) Weight loss after one anastomosis gastric bypass-mini gastric bypass (OAGB-MGB): patient-related perioperative predictive factors. Obes Surg 30:1316–1323
Zamaninour N, Pazouki A, Kermansaravi M, Seifollahi A, Kabir A (2021) Changes in body composition and biochemical parameters following laparoscopic one anastomosis gastric bypass: 1-year follow-up. Obes Surg 31:232–238
Zadeh MH, Zamaninour N, Ansar H, Kabir A, Pazouki A, Farsani GM (2021) Changes in serum albumin and liver enzymes following three different types of bariatric surgery: six-month follow-up. A retrospective cohort study. Sao Paulo Med J 139:598–606
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120(16):1640–1645
Singhal R, Cardoso VR, Wiggins T, Super J, Ludwig C, Gkoutos GV et al (2022) 30-day morbidity and mortality of sleeve gastrectomy, Roux-en-Y gastric bypass and one anastomosis gastric bypass: a propensity score-matched analysis of the GENEVA data. Int J Obes 46(4):750–757
Lee W-J, Pok E-H, Almulaifi A, Tsou JJ, Ser K-H, Lee Y-C (2015) Medium-term results of laparoscopic sleeve gastrectomy: a matched comparison with gastric bypass. Obes Surg 25:1431–1438
Kular KS, Manchanda N, Rutledge R (2018) Physiology of the MGB: how it works for long-term weight loss. Essentials of mini-one anastomosis gastric bypass. Springer, pp 31–7
Łukaszewicz A, Gołaszewski P, Nadolny K, Łukaszewicz J, Ładny JR, Hady HR (2022) Effectiveness of laparoscopic sleeve gastrectomy and one anastomosis gastric bypass on the resolution of metabolic syndrome—a review. Med Res J. https://doi.org/10.5603/MRJ.a2022.0055
van Rijswijk A, van Olst N, Meijnikman A, Acherman Y, Bruin S, van de Laar A et al (2022) The effects of laparoscopic Roux-en-Y gastric bypass and one-anastomosis gastric bypass on glycemic control and remission of type 2 diabetes mellitus: study protocol for a multi-center randomized controlled trial (the DIABAR-trial). Trials 23(1):1–12
Kafalı ME, Şahin M, Ece İ, Acar F, Yılmaz H, Alptekin H et al (2017) The effects of bariatric surgical procedures on the improvement of metabolic syndrome in morbidly obese patients: comparison of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass. Turk J Surg 33(3):142
Kim Z, Hur KY (2011) Laparoscopic mini-gastric bypass for type 2 diabetes: the preliminary report. World J Surg 35:631–636
Nora M, Guimarães M, Almeida R, Martins P, Gonçalves G, Santos M et al (2014) Excess body mass index loss predicts metabolic syndrome remission after gastric bypass. Diabetol Metab Syndr 6(1):1–7
Martini F, Anty R, Schneck A-S, Casanova V, Iannelli A, Gugenheim J (2015) Predictors of metabolic syndrome persistence 1 year after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 11(5):1054–1060
Ricci C, Gaeta M, Rausa E, Macchitella Y, Bonavina L (2014) Early impact of bariatric surgery on type II diabetes, hypertension, and hyperlipidemia: a systematic review, meta-analysis and meta-regression on 6,587 patients. Obes Surg 24:522–528
Acknowledgements
The authors extend their sincere thanks to all participants and National Obesity Surgery Database team, who prepared us very useful data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
KA, PA, RS, IS, AH, SK, FF and MF were responsible for the study design process and conception as well as writing, approving the final version of the manuscript, and providing critical revisions, and agreement to be accountable for all aspects of the work. KA and IS helped in data collection. PA and KA as supervisor checked quality control of data and algorithms. KA and IS have made substantial contributions to analysis and interpretation of data for the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in accordance with the Helsinki declaration and approved by the Research Ethics committee (Ethics number: IR.IUMS.REC 1396.32282). Written informed consent form was received from all patients at the time of first registry in our database for any possible anonymous usage from their data.
Informed consent
The written informed consent form was received from all patients at the time of the first registry in our database for any possible anonymous usage of their data.
Research involving human participants and/or animals
The present study complies with the guidelines for human studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kabir, A., Izadi, S., Mashayekhi, F. et al. Effect of different bariatric surgery methods on metabolic syndrome in patients with severe obesity. Updates Surg 76, 547–554 (2024). https://doi.org/10.1007/s13304-023-01699-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01699-x