Abstract
COVID-19 negatively affected surgical activity, but the potential benefits resulting from adopted measures remain unclear. The aim of this study was to evaluate the change in surgical activity and potential benefit from COVID-19 measures in perspective of Italian surgeons on behalf of SPIGC. A nationwide online survey on surgical practice before, during, and after COVID-19 pandemic was conducted in March–April 2022 (NCT:05323851). Effects of COVID-19 hospital-related measures on surgical patients’ management and personal professional development across surgical specialties were explored. Data on demographics, pre-operative/peri-operative/post-operative management, and professional development were collected. Outcomes were matched with the corresponding volume. Four hundred and seventy-three respondents were included in final analysis across 14 surgical specialties. Since SARS-CoV-2 pandemic, application of telematic consultations (4.1% vs. 21.6%; p < 0.0001) and diagnostic evaluations (16.4% vs. 42.2%; p < 0.0001) increased. Elective surgical activities significantly reduced and surgeons opted more frequently for conservative management with a possible indication for elective (26.3% vs. 35.7%; p < 0.0001) or urgent (20.4% vs. 38.5%; p < 0.0001) surgery. All new COVID-related measures are perceived to be maintained in the future. Surgeons’ personal education online increased from 12.6% (pre-COVID) to 86.6% (post-COVID; p < 0.0001). Online educational activities are considered a beneficial effect from COVID pandemic (56.4%). COVID-19 had a great impact on surgical specialties, with significant reduction of operation volume. However, some forced changes turned out to be benefits. Isolation measures pushed the use of telemedicine and telemetric devices for outpatient practice and favored communication for educational purposes and surgeon–patient/family communication. From the Italian surgeons’ perspective, COVID-related measures will continue to influence future surgical clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The SARS-CoV-2 pandemic has radically changed healthcare systems worldwide. Focusing hospital capacities on the management of a large number of patients with acute respiratory syndrome, a major part of which required intensive care, led to a dramatic decrease of activities among all other clinical services, especially with regard to surgical specialties [1].
Apart from the direct reduction of elective surgical activities during the SARS-CoV-2 pandemic, collateral damage included postponement of disease diagnosis and operation, delays in the oncological pathway, increase in post-operative morbidity, difficulty in outpatient and emergency service access, and also general surgeons’ and patients’ fear of hospital [2,3,4]. Undoubtedly, the rapid need for resource redistribution and isolation measures to face COVID-19 infection rapidly forced major changes in daily clinical practice.
The SARS-CoV-2 pandemic definitely favored a faster digital transition, the use of alternative operating strategies, and the implementation of personal development tools [5]. Thus, the potential benefit derived from the new measurements adopted since the COVID-19 pandemic across surgical disciplines is still unclear. Through a nationwide survey, we aimed to evaluate the changes in surgical practice and the potential benefit derived from SARS-CoV-2-related measures in the future perspective of Italian surgeons on behalf of the Italian Polyspecialistic Society of Young Surgeons (SPIGC).
Materials and methods
Study design
A national online survey on surgical practice before, during, and after the COVID-19 pandemic was conducted in March–April 2022. The survey was designed by a committee of three authors (L.S., M.A., and M.M.), who identified and targeted possible positive evolutions of the SARS-CoV-2 pandemic-driven surgical practice adjustments, and reviewed by four senior authors (A.C., R.A., B.Z., and RM), on behalf of SPIGC. The survey was designed on the SurveyMonkey© web application (SVMK Inc., One Curiosity Way, San Mateo, USA). The purpose of this survey was explained to all participants with a brief introduction. Participants were asked to sign a privacy policy consent form at the start.
The survey was composed of six different sections (S1–S6), including both open and closed questions, as follows: S1 (Q1–Q9), demographic data; S2 (Q10–Q15), pre-operative patient management; S3 (Q16–Q23), peri-operative management; S4 (Q24–Q27), post-operative management; S5 (Q28–Q30), professional development; S6 (Q31–Q32), professional volume. Questions in S2–S5 related to pre-COVID, COVID, and post-COVID periods; and those in S6 (personal activity volume) to pre-COVID and COVID periods. In addition, a final section comprising feedback, with a rating scale of 1–5 (Q33), and a box for comments (Q34) was included. The survey structure is summarized in Table 1.
The pre-COVID period was defined as professional surgical practice until March 2020; the COVID time frame is from March 2020 until the end of the pandemic, a future period in which social distancing and personal protective equipment (PPE) will be no longer be required and restrictions ended; and the post-COVID period starts after the above-mentioned scenario.
Italian surgeons from any surgical specialty were considered eligible for the survey’s analysis. Any type of surgical trainee and junior and senior surgeons were included. All participants were informed that the results of the survey would be used for further statistical evaluation and scientific publication. Anonymity was guaranteed by the study design and authorship in the collaborative group was offered on a voluntary base.
A dedicated account to deliver the survey was created: surveyspigc@gmail.com. This was used to distribute the survey, answer query-related inconsistencies in survey responses, and confirm the final authorship. The survey was promoted through a mailing list of Italian surgeons, instant message services (WhatsApp, Telegram), the official SPIGC site/account, and social media (Facebook, Instagram and Linked-in).
A pilot version of the survey was tested with 17 participants from 7 to 14 March 2022 and, after approval of all committee authors, the revised final version was launched on 15 March 2022 and closed on 30 April 2022.
From 1 to 15 May 2022, the authors of incomplete answers were personally contacted through email to complete the survey. Only those who completed all sections of the survey were considered in the final data analysis. On 15 May 2022, the full dataset was extracted from Survey Monkey, incomplete responses and duplicates were deleted, and the final database was sent to the statistician for result analysis.
Outcome measures
The main outcome of the study was to evaluate, over time, the effect of COVID-19 hospital-related measures on pre-, peri-, and post-operative management of patients and personal surgical development from all surgical specialties, exploring the potential benefits of future surgery. The question outcome was matched with the corresponding activity volume when applicable.
Ethics
Survey participation was voluntary and no incentives were offered. According to the Institutional Review Board of the Policlinico Tor Vergata, no approval was required. This survey was registered at clinicaltrials.gov. NCT05323851.
Reporting of this study follows the American Association for Public Opinion Research reporting guidelines and the CHEcklist for Reporting Results of Internet E-Surveys (CHERRIES) [6].
Statistical analysis
Datasets were collected in Excel (Microsoft, Redmond, WA, USA) and the statistical analysis was performed using SPSS (IBM SPSS Statistics for Windows, Version 27.0; IBM Corp., Armonk, NY, USA). Characteristics were summarized by means of levels for categorical variables or quantiles for continuous variables. All tests were two sided, accepting p < 0.05 as indicating a statistically significant difference, and confidence intervals were calculated at the 95% level.
Results
Study population
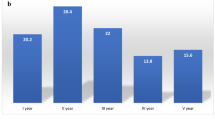
Of 581 surgeons who answered the survey, 108 respondents were excluded (105 incomplete, 3 duplicates) and 473 complete responses were included for analysis (completion rate 82%). Participants had a mean age of 35.3 ± 7.7 years and males accounted for 73.2% of respondents (n = 346). Based on the region of employment in Italy, surgeons were distributed as follows: 42.8% in Central regions (n = 202), 26.6% in Northwest regions (n = 126), 11.4% in Southern regions (n = 54), 10.6% in Northeast regions (n = 50), and 8.6% in Island regions (n = 41).
According to the surgical specialty, respondents included: 66.8% (n = 316) general surgeons, 6.1% (n = 29) orthopedic surgeons, 4.7% (n = 22) thoracic surgeons, 4.7% (n = 22) vascular surgeons, 4.3% (n = 20) oculists, 2.7% (n = 13) gynecologists, 2.7% (n = 13) dental surgeons, 2.1% (n = 10) urologists, 1.7% (n = 8) plastic surgeons, 1.7% (n = 8) pediatric surgeons, 1.1% (n = 5) otorhinolaryngology surgeons, 0.6% (n = 3) maxillary surgeons, 0.4% (n = 2) heart surgeons, and 0.4% (n = 2) neurosurgeons.
Participants were mainly consultants (42.9%, n = 203), followed by surgical trainees (28.8%, n = 136), PhD surgeons (13.5%, n = 64), assistant professors (9.9%, n = 47), and professors (4.9%, n = 23).
Respondents’ institutions included academic hospitals (45.9%, n = 217), public hospitals (30.7%, n = 145), research centers (18%, n = 85), and private hospitals (5.5%, n = 26). During the pandemic the respondents’ institutions changed, with 82.8% (n = 392) in mixed hospitals (COVID and non-COVID services), 10.6% (n = 50) exclusively in COVID centers, and 6.6% (n = 31) in non-COVID centers. Participants’ referral hospitals were secondary centers (53.1%, n = 251), tertiary centers (30.9%, n = 146), and peripheral centers (16%, n = 76).
The demographic data are summarized in Fig. 1 and Table 2.
Pre-operative management
The management of patients’ candidate to surgical operations in the pre-COVID, COVID, and post-COVID periods is reported in Table 3. Before the COVID-19 pandemic, the mean number of patient consultations as outpatients was 90.1 ± 116 per month, which decreased to 29.7 ± 43 during the COVID period (p < 0.0001). Since the pandemic, the use of telematic consultations (4.1% vs. 21.6%; p < 0.0001) and telematic diagnostic evaluations (16.4% vs. 42.2%; p < 0.0001) significantly increased compared to the pre-COVID period. Additionally, surgeons perceived that higher adoption of both the virtual consultation and telematic diagnostic evaluation will be maintained also in the post-COVID period (13.9% and 30.9% of cases, respectively).
Pre-operative tests were performed externally to the treating hospital in 15.6% of cases in the pre-COVID period and in 25.9% of cases during the COVID pandemic (p < 0.0001); these figures are predicted to remain unchanged in the future (21.4%). The percentage of patients needing hospital admission for pre-operative tests was 17.8% in the pre-COVID period, 24.6% during COVID, and is predicted to be 17.8% post-COVID (p < 0.0001).
For all surgical specialties, elective surgical activities significantly reduced from the pre-COVID to the COVID period (surgical procedures per month: 27.7 ± 60.2 vs. 9.9 ± 14; p < 0.0001). Moreover, compared to the pre-COVID phase, during the COVID period surgeons opted more frequently for conservative management in patients, with a possible indication for elective surgery (26.3% vs. 35.7%); this approach was predicted to be maintained in 28.4% of cases post-COVID (p < 0.0001).
The mean number of urgent operations per month was 7.1 ± 12 pre-COVID, which decreased to 6.1 ± 10 during the COVID period (p = 0.028). Also, conservative management of patients with a possible indication for urgent surgery increased from 20.4% pre-COVID to 38.5% during COVID, with a prediction of 24.1% post-COVID (p < 0.0001).
Peri-operative management
During the pre-COVID period, surgical procedures listed in public healthcare hospitals were performed in other accredited structures in 11.9% of cases; this modality was adopted in 21.3% of operations during COVID, with a prediction of 17.8% post-COVID (p < 0.0001). Also, the percentage of operations performed in a private setting remained stable in the pre-COVID and COVID periods (15.9% vs. 14.2%). Thus, participants believe that the percentage of patients operated on in the private setting will increase after the COVID period (20%; p < 0.0001).
According to the regimen of admission for surgical procedures, participants stated that operations performed both in outpatient settings (48.7% vs. 27.5%; p < 0.0001) and in a one-day (< 24 h) admission regimen (53.9% vs. 29.2%; p < 0.0001) significantly reduced from pre-COVID to the COVID period. Responders believe that in the post-COVID period, operations that can be performed as an outpatient or on one-day admission will be used in 46.2% and 51.1% of cases, respectively. Moreover, the percentage of operations possible with locoregional anesthesia was 55% during pre-COVID, 46% during COVID and is predicted to be 57% post-COVID (p < 0.0001).
Peri-operative fast-track protocols (i.e., Enhanced Recovery After Surgery [ERAS]) were adopted in 42.9% of operations during pre-COVID and this percentage decreased to 41.9% during COVID; thus, responders predict that they will be used in more than half of cases (51.5%) post-COVID (p < 0.0001).
To avoid in-hospital infections, the use of PPE increased significantly during the COVID pandemic (27.9% vs. 94.3%; p < 0.0001). Interestingly, participants stated that the adoption of PPE would be maintained also in the future (80.7%).
Telematic consultation with patients’ family was more frequently adopted during the COVID pandemic (13.2% vs. 76%) and responders believe that this figure will be maintained in almost 48.7% of cases (p < 0.0001).
The peri-operative management data are summarized in Table 4.
Post-operative management
Results on post-operative management are detailed in Table 5. Although the mean number of patients visited monthly in the post-operative outpatient clinic decreased during the COVID period (36.5 ± 40 vs. 17 ± 2 3 in the pre-COVID and COVID periods, respectively; p < 0.0001), the percentage of post-operative follow-up consultations performed telematically increased from 5.6% to 26% during COVID (p < 0.0001). Moreover, respondents feel that post-operative telematic consultations will be adopted in 15.6% of cases in the post-COVID period (p < 0.0001).
The use of telemetric devices for post-operative home care has increased significantly since the COVID pandemic (3.8% vs. 14%; p < 0.0001) and surgeons believe that they will continue to be used in the future (11.1%).
Post-operatively, communication with patients was performed more frequently through private channels (personal emails, telephone calls and messages) adopted during the COVID phase compared to the pre-COVID period (23.9% vs. 47.5%; p < 0.0001), with a prediction of 38.3% post-COVID (p < 0.0001).
The percentage of online multidisciplinary meetings increased from 7.9% pre-COVID to 79.4% during COVID (p < 0.0001), and surgeons believe that telematic meetings will be maintained in more than half of cases (52.3%) in the future.
Surgeons’ personal development
Pre-COVID, the mean number of educational events participated in was 2.2 ± 3 per month for each participant, which increased to 4.7 ± 6 per month during COVID (p < 0.0001). Online courses (i.e., webinars, seminars, classes) increased from 12.6% to 86.6% during the pre-COVID and COVID periods, respectively, and surgeons perceive that in the post-COVID phase such online educational events will be maintained for more than half (56.4%) of cases.
Surgeons dedicated a mean time of 28.4 ± 46 h per month to their professional development during pre-COVID and this time increased to 34.3 ± 51 h during the COVID period (p < 0.0001).
Also, participants declared that they used a surgical training simulator for about 10.6% of their time before COVID, which increased to 17.1% during COVID (p < 0.0001) and is predicted to be 18.3% in the post-COVID period.
The percentage of time dedicated to online surgery videos used for professional development increased from 10.0% to 29.1% in the pre-COVID and COVID periods, respectively (p < 0.0001), and surgeons believe that they will maintain to consult online surgical videos in the future. The personal development data are summarized in Table 6.
All survey outcomes are summarized in Fig. 2
Discussion
This survey investigated surgical practice in Italy before, during, and “what-is-expected-to-be” after the SARS-CoV-2 pandemic. While clear time frames were established for the pre-COVID and COVID periods, the survey design did not initially include a specific start date for the post-COVID period. However, it is now possible to retrospectively designate May 2023 as the start for the post-COVID period, since declared by the WHO as the end of the pandemic [7]. Substantial differences were identified between the pre-COVID and COVID periods; moreover, while some of the introduced novelties are expected to vanish in the post-pandemic phase, it appears that others might have to stay.
There are numerous previous studies that reported several negative effects of the pandemic (including increased comorbidity, delay in diagnosis, etc.), but very few have addressed the positive transitions that it ushered in [8, 9]. The scope of this study was to identify possible appreciated modifications that could ultimately be adopted and change future practice after the COVID pandemic in the clinical management of surgical patients across different specialties and in the personal education of surgeons.
After the SARS-CoV-2 pandemic, in surgical practice, one major change introduced was in outpatient management. During the COVID period, there was a marked reduction in patient and diagnostic test ambulatory evaluation, which was replaced by online consultation and remote diagnostic test evaluation. Although this practice was already relatively diffuse in some countries (i.e., UK), it was extremely limited in others, such as Italy. Indeed, after the COVID-19 pandemic, the Italian healthcare system’s long-term plan aims to make digital consultation the mainstream source of outpatient management by 2024 [10]. Surgeons involved in the survey are convinced that this practice will remain, probably because it permits optimization of resources and time, patient comfort and attendance rate. Furthermore, remote consulting switches have already been demonstrated to mitigate stress and in-hospital infection risk, especially among frail patients (elderly, immunosuppressed) [11,12,13,14,15].
In a similar way, the patient’s physical presence at the hospital was limited as much as possible, even during necessary steps for elective surgery such as pre-hospitalization. In fact, the percentage of patients who had their pre-operative work-up elsewhere (usually closer to home) increased. This practice is thought to decrease centralization for routine diagnosis, unburdening major hospitals and favoring an improved territorial distribution. Similarly, decentralization occurred for benign and/or uncomplicated diseases, with private practice increasing. The following measures were implemented to cope with increased waiting list times that unfortunately lead, over the pandemic period, to serious delay, also in oncology patients, with a proven negative impact on patients’ health [2, 16,17,18]. All these changes are thought to persist and may help to enhance the overall efficiency of the national health system. Decentralization was reported also in the higher rate of surgical procedures performed in private and private-accredited structures.
In the same direction is the predicted implementation on a greater scale of ERAS protocols and locoregional anesthesia: the pandemic necessities might have helped reluctant surgeons to appreciate the advantages of these approaches, despite there being no great change in these items during the COVID-19 period [19, 20]. This experience may have built trust and confidence in the effectiveness of ERAS, leading to its continued and increased adoption in the future, despite shortage of resources and workforce may hider its systematic use. Surprisingly, other measures such as one-day or ambulatory surgery decreased during the pandemic, as already demonstrated for specific surgery such as laparoscopic cholecystectomy [21]. This may be due to reshaped in-hospital logistics, but the absence of a predicted increase in the future also suggests a possible general weak belief in this surgical practice.
Therapeutic management of surgical disease was significantly different among these time frames. During the pandemic, conservative management increased drastically both in the elective and emergency setting [5, 22,23,24,25]. Surgeons involved in the survey believe that this trend might continue, albeit at a lower level, as the conservative strategy has proved useful in many cases. It is possible that the pandemic has revived conservative management in situations that were considered indications for surgery, with acceptable outcomes. This might also have increased surgeons’ sensitivity to indicate surgery in cases with the greatest expected benefit. The use of PPE, of course, increased dramatically with COVID-19 and surgeons think that this trend will also stay, as PPE may prove helpful in reducing nosocomial infections [4, 26, 27].
Telemetric measures for post-operative follow-up have also been introduced and are now very popular among survey respondents. These measures include online consultation platforms, hospital-provided tablets for questionnaire filling, dedicated chats with hospital personnel and vital sign detection using smart-watches [28, 29]. Online/telephonic measures were used increasingly also for surgeon–patient and especially for surgeon–patient/family contact, with a dramatic 15–80% rise. This may have broken the Italian taboo of physical presence being necessary for correct communication. Again, all these technologies may reduce the workload for surgeons and increase patient satisfaction and outcomes [30].
Online peer-to-peer contact has also increased, from multidisciplinary meetings to events such as e-congresses and educational surgical videos. This may speed the process of professional development, and probably also reduce costs, and was indeed a welcomed innovation [31,32,33]. E-congresses are easy to sign up for and swift to follow. Surgical videos have democratically given everyone the opportunity to learn from the best surgeons around the world. Similarly, the time spent on simulator training has almost doubled and investment in this form of training may help trainees to speed up their learning curve. In fact, all these measures are predicted to continue to increase in the near future.
This study has several limitations. First, the survey methodology is intrinsically biased in relation to question phrasing and respondents’ subjectivity. Second, the sample, although conspicuous, is mostly composed of general surgeons and, thus, may not represent the real picture of all specialties. Finally, the future predicted values are based on the perspective of the Italian surgeons and may be inaccurate. Thus, this study has highlighted the positive effects of the SARS-CoV-2 crisis on Italian surgical practice. In particular, it appears that the pandemic has boosted the implementation of technology in patient management, both pre- and postoperatively, and in surgical professional development.
The SARS-CoV-2 pandemic had a great impact on surgical specialties, with a significant reduction of patient and operation volume but with some forced changes that turned out to be benefits. The isolation measures pushed the use of telemedicine and telemetric devices for outpatient practice and favored communication for educational purposes and surgeon–patient/family communication. Different clinical and organizational strategies were utilized in patient management to reallocate surgical volume and improve patient outcomes. In the Italian surgeons’ perspective, this change of course driven by COVID-19 will continue and develop further in future clinical practice.
Data availability
Anonymized interview is available on request to the working group and upon reasonable request to the corresponding author.
References
Bellato V, Konishi T, Pellino G, An Y, Piciocchi A, Sensi B, S-COVID Collaborative Group et al (2020) Impact of asymptomatic COVID-19 patients in global surgical practice during the COVID-19 pandemic. Br J Surg 107(10):e364–e365. https://doi.org/10.1002/bjs.11800
Rottoli M, Gori A, Pellino G, Flacco ME, Martellucci C, Spinelli A, Poggioli G, COVID–Colorectal Cancer (CRC) Study Group (2022) Colorectal Cancer Stage at Diagnosis Before vs During the COVID-19 Pandemic in Italy. JAMA Netw Open 5(11):e2243119. https://doi.org/10.1001/jamanetworkopen.2022.43119
COVIDSurg Collaborative (2020) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 396(10243):27–38. https://doi.org/10.1016/S0140-6736(20)31182-X
An Y, Bellato V, Konishi T, Pellino G, Sensi B, Siragusa L, Franceschilli M, Sica GS, S-COVID Collaborative Group (2020) Surgeons’ fear of getting infected by COVID19: a global survey. Br J Surg 107(11):e543–e544. https://doi.org/10.1002/bjs.11833
Tebala GD, Milani MS, Bignell M, Bond-Smith G, Lewis C, Cirocchi R, CovidICE-International Collaborative et al (2022) Emergency surgery admissions and the COVID-19 pandemic: did the first wave really change our practice? Results of an ACOI/WSES international retrospective cohort audit on 6263 patients. World J Emerg Surg 17(1):8. https://doi.org/10.1186/s13017-022-00407-1
Eysenbach G (2004) Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res 6:e34. https://doi.org/10.2196/jmir.6.3.e34
United Nations (2023) WHO chief declares end to COVID-19 as a global health emergency. UN News. https://news.un.org/en/story/2023/05/1136367#:~:text=WHO%20chief%20declares%20end%20to%20COVID%2D19%20as%20a%20global%20health%20emergency,-5%20May%202023&text=The%20head%20of%20the%20UN,no%20longer%20a%20global%20threat. Accessed 12 July 2023
COVIDSurg Collaborative (2020) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 396(10243):27–38. https://doi.org/10.1016/S0140-6736(20)31182-X
Oldani C, Vanni G, Buonomo OC (2020) COVID-19 unintended effects on breast cancer in Italy after the great lockdown. Front Public Health 16(8):601748. https://doi.org/10.3389/fpubh.2020.601748
NHS long term plan. National Health Service. 2019. [2020–02–03]. https://www.longtermplan.nhs.uk
Damery S, Jones J, O’Connell Francischetto E, Jolly K, Lilford R, Ferguson J (2021) Remote consultations versus standard face-to-face appointments for liver transplant patients in routine hospital care: feasibility randomized controlled trial of myVideoClinic. J Med Internet Res 23(9):e19232. https://doi.org/10.2196/19232
Machado PM, Verschueren P, Grainger R, Jones H, Piercy J, van Beneden K, Caporali R, Dejaco C, Fautrel B (2022) Impact of COVID-19 pandemic on the management of patients with RA: a survey of rheumatologists in six European countries. Rheumatol Adv Pract 7(1):rkac108. https://doi.org/10.1093/rap/rkac108
Hamid MA, Kumar A, Gunaseelan L, Arulchelvan A, Sinha A, Razi S et al (2022) Innovative online care: a cross-sectional survey study of potential benefits and challenges of online lactation consultation service with paediatrician consultation. Paediatr Child Health 27(7):414–420. https://doi.org/10.1093/pch/pxac074
Manzia TM, Angelico R, Toti L, Pisani G, Vita G, Romano F et al (2021) The hamletic dilemma of patients waiting for kidney transplantation during the COVID-19 pandemic: to accept or not to accept (an organ offer)? Transpl Infect Dis 23(2):e13560. https://doi.org/10.1111/tid.13560
Angelico R, Blasi F, Manzia TM, Toti L, Tisone G, Cacciola R (2021) The management of immunosuppression in kidney transplant recipients with COVID-19 disease: an update and systematic review of the literature. Medicina (Kaunas) 57(5):435. https://doi.org/10.3390/medicina57050435
Vanni G, Materazzo M, Dauri M, Farinaccio A, Buonomo C, Portarena I et al (2021) Lymphocytes, interleukin 6 and D-dimer cannot predict clinical outcome in coronavirus cancer patients: LyNC1.20 study. Anticancer Res 41(1):307–316. https://doi.org/10.21873/anticanres.14777
COVIDSurg Collaborative (2021) Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol 22(11):1507–1517. https://doi.org/10.1016/S1470-2045(21)00493-9
Vanni G, Pellicciaro M, Materazzo M, Pedini D, Portarena I, Buonomo C et al (2021) Advanced stages and increased need for adjuvant treatments in breast cancer patients: the effect of the one-year COVID-19 pandemic. Anticancer Res 41(5):2689–2696. https://doi.org/10.21873/anticanres.15050
Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G et al (2021) Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surg 156(8):775–784. https://doi.org/10.1001/jamasurg.2021.0586
Sica GS, Campanelli M, Bellato V, Monteleone G (2020) Gastrointestinal cancer surgery and enhanced recovery after surgery (ERAS) during COVID-19 outbreak. Langenbecks Arch Surg 405(3):357–358. https://doi.org/10.1007/s00423-020-01885-0
Manzia TM, Angelico R, Parente A, Muiesan P, Tisone G, MEGAVID (ManagEment of GAllstone disease during coVID-19 pandemic) Clinical Investigator Group (2020) Global management of a common, underrated surgical task during the COVID-19 pandemic: gallstone disease—an international survery. Ann Med Surg (Lond) 57:95–102. https://doi.org/10.1016/j.amsu.2020.07.021
Pata F, Di Martino M, Podda M, Di Saverio S, Ielpo B, Pellino G, ACIE Appy Study Collaborative (2022) Evolving trends in the management of acute appendicitis during COVID-19 waves: the ACIE appy II study. World J Surg 46(9):2021–2035. https://doi.org/10.1007/s00268-022-06649-z
Reichert M, Sartelli M, Weigand MA, Hecker M, Oppelt PU, Noll J, WSES COVID-19 emergency surgery survey collaboration group et al (2022) Two years later: is the SARS-CoV-2 pandemic still having an impact on emergency surgery? An international cross-sectional survey among WSES members. World J Emerg Surg 17(1):34. https://doi.org/10.1186/s13017-022-00424-0
Holleyman RJ, Khan SK, Charlett A, Inman DS, Johansen A, Brown C et al (2022) The impact of COVID-19 on mortality after hip fracture: a population cohort study from England. Bone Jt J 104-B(10):1156–1167. https://doi.org/10.1302/0301-620X.104B10.BJJ-2022-0082.R1
Aldrighetti L, Boggi U, Falconi M, Giuliante F, Cipriani F, Ratti F, Torzilli G, Italian Association of HepatoBilioPancreatic Surgeons-AICEP (2020) Perspectives from Italy during the COVID-19 pandemic: nationwide survey-based focus on minimally invasive HPB surgery. Updates Surg 72(2):241–247. https://doi.org/10.1007/s13304-020-00815-5
Mastri P, Di Petrillo F, Cerone A, Muselli M, Saracco M, Logroscino G, Calvisi V (2022) Reduction in the duration of postoperative fever during the COVID-19 pandemic in orthopedic and traumatic surgery due to PPE and cautions. J Clin Med 11(6):1635. https://doi.org/10.3390/jcm11061635
Monaco A, Manzia TM, Angelico R, Iaria G, Gazia C, Al Alawi Y et al (2020) Awareness and impact of non-pharmaceutical interventions during coronavirus disease 2019 pandemic in renal transplant recipients. Transplant Proc 52(9):2607–2613. https://doi.org/10.1016/j.transproceed.2020.07.010
Coffey JD, Christopherson LA, Williams RD, Gathje SR, Bell SJ, Pahl DF et al (2022) Development and implementation of a nurse-based remote patient monitoring program for ambulatory disease management. Front Digit Health 14(4):1052408. https://doi.org/10.3389/fdgth.2022.1052408
Curfman KR, Poola AS, Blair GE, Kosnik CL, Pille SA, Thilo EL, Hawkins ME, Rashidi L (2022) Ambulatory colectomy: a pilot protocol for same day discharge in minimally invasive colorectal surgery. Am J Surg 224(2):757–760. https://doi.org/10.1016/j.amjsurg.2022.04.039
Vargas-Sánchez HR, Tomás-López JC, Álvarez-Medina V, Gil-Velázquez LE, Vega-Vega H, Alarcón-López A et al (2023) Telephonic follow-up and the risk of death in ambulatory patients with COVID-19. J Am Board Fam Med 36(1):164–169. https://doi.org/10.3122/jabfm.2022.220214R1
Ruiz-Barrera MA, Agudelo-Arrieta M, Aponte-Caballero R, Gutierrez-Gomez S, Ruiz-Cardozo MA, Madrinan-Navia H et al (2021) Developing a web-based congress: the 2020 international web-based neurosurgery congress method. World Neurosurg 148:e415–e424. https://doi.org/10.1016/j.wneu.2020.12.174
Vervoorn MT, Wulfse M, Van Doormaal TPC, Ruurda JP, Van der Kaaij NP, De Heer LM (2023) Mixed reality in modern surgical and interventional practice: narrative review of the literature. JMIR Serious Games 11:e41297. https://doi.org/10.2196/41297
Gallo G, Guaitoli E, Barra F, Picciariello A, Pasculli A, Coppola A, SPIGC Surgical Training Working Group et al (2023) Restructuring surgical training after COVID-19 pandemic: a nationwide survey on the Italian scenario on behalf of the Italian polyspecialistic young surgeons society (SPIGC). Front Surg 9:1115653. https://doi.org/10.3389/fsurg.2022.1115653
Acknowledgements
The authors sincerely acknowledge all the collaborative authors in the SPIGC Survey Collaborative Group, and all the health care professionals involved in COVID-19 pandemic.
COLLABORATORS: SPIGC Survey Collaborative Group: Leandro Siragusa (University of Rome “Tor Vergata”, Rome, Italy); Roberta Angelico (University of Rome “Tor Vergata”, Rome, Italy); Biagio Zampogna (Campus Bio-Medico University Rome); Marco Materazzo (University of Rome “Tor Vergata”, Rome, Italy), Roberto Sorge (University of Rome “Tor Vergata”, Rome, Italy), Luca Giordano (Sapienza University of Rome, Rome, Italy), Roberto Meniconi (Department of General Surgery and Liver Transplantation, San Camillo Forlanini Hospital, Rome, Italy), Alessandro Coppola (Department of Surgery, Sapienza University of Rome, Rome, Italy), Annarita Marino (0000-0001-6989-7037 Annunziata di Cosenza Hospital, Cosenza, Italy), Giorgio Giraudo (0000-0002-0273-0096 AO Santa Croce e Carle, Cuneo, Italy), Sofia Esposito (0000-0002-0907-4634 AOU policlinico di Modena, Modena, Italy), Alessia Urbani (0000-0002-4276-6130 AOU Ferrara, Ferrara, Italy), Matteo De Pastena (0000-0001-5244-4357 AOU Verona, Verona, Italy), Rodolfo Mastrapasqua (0000-0002-3558-8081 ASL Turin, Turin, Italy), Mattia Garancini (0000-0001-6091-4574 ASST-Monza San Gerardo Hospital Milano-Bicocca University, Milano, Italy), Alice Frontali (0000-0001-7434-1797 ASST-Vimercate, Vimercate, Italy), Giovanni Pascale (0000-0003-0711-5815 Azienda Ospedaliera Regionale San Carlo, Potenza, Italy), Jacopo Martellucci (0000-0002-7437-9098 Careggi University Hospital, Firenze, Italy), Francesco Falbo (0000-0003-3840-4484 Hospital San Giovanni Addolorata, Roma, Italy), Alessandro Boscarelli (0000-0003-1934-1764 IRCCS Burlo Garofolo, Trieste, Italy), Pietro Bertoglio (0000-0002-6267-0099 IRCCS Azienda Ospedaliero Universitaria di Bologna, Bologna, Italy), Eleonora Trecca (0000-0001-6490-1746 IRCCS Research Hospital Casa Sollievo della Sofferenza; San Giovanni Rotondo Foggia Italy), Luca Galassi (0000-0003-2580-1704 IRCCS San Giovanni dei Tintori Foundation via G.B. Pergolesi 33 20900 Monza (MB), Italy), Vincenzo Vento (0000-0001-5411-2882 lancisi cardiovascular center Ancona Italy), Ambra Chiappini (0000-0002-2792-3548 Local Healthcare Agency Lecce), Alessandro Antonelli (0000-0002-9557-3586 Magna Graecia University of Catanzaro Italy), Francesco Bennardo (0000-0002-6528-2681 Magna Graecia University of Catanzaro Italy), Filippo Familiari (0000-0002-3453-2043 Magna Graecia University of Catanzaro Italy), Giuseppe Giannaccare (0000-0003-2617-0289 Magna Graecia University of Catanzaro Italy), Andrea Sisto Zappia (Magna Graecia University of Catanzaro Italy), Giuseppe Giuliani (0000-0001-9232-398X Misericordia hospital Grosseto), Francesca Falcone (0000-0002-3729-2321 National Institute of Tumours IRCSS "Fondazione G. Pascale" Naples Italy Center for Advanced Endoscopic Gynecologic Surgery Avellino Italy), Stefano Sebastiani (0000-0002-3865-9818 Ospedale Maggiore AUSL Bologna), Mauro Montuori (0000-0002-7968-2109 Policlinico San Pietro—Ponte San Pietro (BG), Italia), Stefano Rossi (0000-0002-9022-4096 San Filippo Neri Hospital ASL Roma 1 Rome Italy), Andrea Sagnotta (0000-0002-0606-0317 San Filippo Neri Hospital ASL Roma 1 Rome Italy), Beatrice Giuliani (0000-0002-3778-166X San Paolo Hospital), Giusy Carmen Imbriani (Sant'Anna e San Sebastiano Agency Caserta), Stefano Restaino (0000-0002-7848-0329 Udine University Hospital DAME Udine Italy), Lorenzo Andreani (0000-0002-8268-6987 Universitary Hospital Agency Pisana), Fabrizio Di Maria (0000-0002-0582-985X Universitary Hospital Policlinico-San Marco di Catania University of Catania Italia), Antonio Simone Laganà (0000-0003-1543-2802 University of Palermo Italy), Livio Vitiello (0000-0001-7867-3342 University of Salerno Italy), Federico Berton (0000-0001-6359-9143 University of Trieste Italy), Edoardo Virgilio (0000-0002-9324-3487 1), Department of Medicine and Surgery University of Parma 2), UOC General Surgery P.O. di Vaio Fidenza), Marco Palisi (0000-0003-4770-2571 A.O. Ordine Mauriziano di Torino), Luca Portigliotti (0000-0002-3390-4298 A.O.U. Ospedale Maggiore della Carità Novara), Marco Calussi (0000-0002-2481-2762 ACOI SICCR), Luigi Conti (0000-0002-1623-5440 Acute care Surgery Unit Department of Surgery G. Da Saliceto Hospital AUSL Piacenza), Claudio Mauriello (0000-0002-3121-5325 ALS Naples 2 nord), Mirko Barone (0000-0002-3578-8657 Annunziata University Hospital of Chieti), Edoardo Saladino (0000-0002-4528-6626 AO Papardo – Messina), Alessia Giaquinta (0000-0003-3227-4340 AOU Policlinico Catania), Domenico Zerbo (0000-0002-6864-7826 AOU Policlinico Catania), Giuseppe Frazzetta (0000-0003-2505-4972 ARNAS Civico Palermo chirurgia oncologica), Giovanni Merola (0000-0002-3237-677X ASL NA 2 Nord—P.O. San Giovanni di Dio—Frattamaggiore), Andrea Chierici (0000-0003-1475-4500 ASST Brianza—Ospedale di Vimercate Chirurgia Generale Roberto Bini (0000-0002-4512-6243 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Leonardo Centonze (0000-0001-9371-7411 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Riccardo De Carlis (0000-0003-3697-1653 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Luca Ferrario (0000-0002-3652-3255 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Alessandro Giani (0000-0003-0718-2321 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Andrea Lauterio (0000-0001-6110-8582 ASST Grande Ospedale Metropolitano Niguarda Milan Italy), Nicolò Tamini (0000-0003-3917-6831 Asst Monza—Ospedale San Gerardo), Stefano Corti (0000-0001-8239-2340 ASST Papa Giovanni XXIII), Emanuele Botteri (0000-0002-6414-915X ASST Spedali Civili Brescia Po Montichiari), Jacopo Andreuccetti (0000-0003-0474-9775 ASST Spedali Civili of Brescia), Rossella D'Alessio (0000-0001-5614-7616 Asst Spedali Civili of Brescia), Giovanni Cestaro (0000-0002-9091-0731 ASST Valle Olona—Ospedale di Gallarate), Guglielmo Clarizia (0000-0003-0592-2904 ASST Valtellina e Alto Lario), Alessandro Spolini (0000-0001-8534-3528 ASST Valtellina-Alto Lario Ospedale di Sondrio), Alberto Salvatore Carboni (ATS Sardegna Enrico Benzoni (0000-0003-4702-3827 aulss 1 Dolomiti Bellluno), Giampaolo Galiffa (0000-0002-9318-398X Aurelia Hospital), Bruno Perotti (0000-0003-0163-3582 AUSL Toscana Nord-Ovest), Massimiliano Veroux (0000-0002-2780-6421 Azienda Osedaliero Universitaria Policlinico San Marco), Valentina Randazzo (Azienda ospedaliera Cannizzaro), Domenico topa ( 0000-0002-0473-8024 Azienda ospedaliera san Giovanni addolorata Roma), Chiara Pranteda (0000- 0002-5186-0612 Azienda ospedaliero-universitaria Sant’Andrea Roma), Massimiliano Veroux (0000-0002-2780-6421 Azienda Policlinico San Marco Università di Catania), Giorgia Contini (0000-0001-6507-4316 Bambino Gesù Children’s Hospital IRCCS Rome Italy), Chiara Iacusso (0000-0003-0934-8735 Bambino Gesù Children’s Hospital IRCCS Rome Italy), Valerio Voglino (0000-0001-7551-7782 Bambino Gesù Children’s Hospital IRCCS Rome Italy), Pietro Vita ( Breast Unit Ospedali Riuniti Foggia Italy), Francesco Maria Carrano (0000-0003-1189-9907 Busto Arsizio Circolo Hospital ASST-Valle Olona Varese Italy), Luca Ambrosio (0000-0003-2424-1274 Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma), Roberto Cammarata (0000-0002-3230-2869 Campus Bio-Medico University Rome), Gabriella Teresa Capolupo (0000-0002-6009-8180 Campus Bio-Medico University Rome), Damiano Caputo (0000-0001-7058-1945 Campus Bio-Medico University Rome), Filippo Carannante (0000-0003-3618-8431 Campus Bio-Medico University Rome), Chiara Cascone (0000-0003-0789-779X Campus Bio-Medico University Rome), Francesco Esperto (0000-0002-0108-1864 Campus Bio-Medico University Rome), Tommaso Farolfi (0000-0003-1932-2846 Campus Bio-Medico University Rome), Luca Frasca (0000-0001-7188-5107 Campus Bio-Medico University Rome), Ida Francesca Gallo (0000-0003-1167-1216 Campus Bio-Medico University Rome), Giulia Gibin (0000-0002-0319-3245 Campus Bio-Medico University Rome), Giancarlo Giurazza (0000-0003-4385-6813 Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Via Alvaro del Portillo, 00128 Roma, Italy), Luca Improta (0000-0002-8915-1168 Campus Bio-Medico University Rome), Vincenzo La Vaccara (0000-0002-9355-5771 Campus Bio-Medico University Rome), Paolo Luffarelli (0000-0002-2503-8123 Campus Bio-Medico University Rome), Daniela Luvero (0000-0002-3537-7014 Campus Bio-Medico University Rome), Giovanni Marangi (0000-0002-7179-3533 Campus Bio-Medico University Rome), Gianluca Masciana' (Campus Bio-Medico University Rome), Alessandro Mazzola (0000-0002-0179-109X Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Roma, Italy.), Erica Mazzotta ( 0000-0002-9609-9767 Campus Bio-Medico University Rome), Chiara Isabella Miligi (0000-0002-6944-7359 Campus Bio-Medico University Rome), Nunzio Montelione (0000-0003-0983-7045 Campus Bio-Medico University Rome), Antonio Nenna (0000-0002-4069-6781 Campus Bio-Medico University Rome), Paolo Orsaria (Campus Bio-Medico University Rome), Rocco Papalia (0000-0002-6069-4871 Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Roma, Italy), Giuseppe Francesco Papalia (0000-0002-4140-738X Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Roma, Italy.), Francesco Rosario Parisi (0000-0003-2637-3668 Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Via Alvaro del Portillo, 00128 Roma, Italy.), Francesco Prata (0000-0003-3084-6210 Campus Bio-Medico University Rome), Rosa Salzillo (0000-0002-1596-5919 Campus Bio-Medico University Rome), Simone Santini (0000-0001-6580-2010 Operative Research Unit of Orthopaedic and Trauma Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Roma, Italy; Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Roma, Italy), Francesco Sofo ( Campus Bio-Medico University Rome ), Andrea Zampoli (0000-0002-1474-2350 Campus Bio-Medico University Rome), Cinzia Tanda ( 0000-0002-2324-9410 Casa di Cura "Madonna del Rimedio" Oristano), Gaia Altieri (0000-0002-0324-2430 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Francesco Ardito (0000-0003-1596-2862 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Francesco Belia ( 0000-0002-8981-7898 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Valentina Bianchi (0000-0002-8817-3760 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Alberto Biondi (0000-0002-2470-7858 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Giuseppe Brisinda (0000-0001-8820-9471 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Marco Chiappetta (0000-0002-3807-6911 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Gianluca Ciolli (0000-0002-3653-4552 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Alessandro Ciolli (Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Federica Ferracci (0000-0002-8040-2231 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Lorenzo Ferri (0000-0002-4109-9727 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Valeria Fico (0000-0003-1619-4164 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Claudio Fiorillo (Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Pietro Fransvea (0000-0003-4969-3373 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Federica Galiandro (0000-0001-5041-4867 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Francesco Giovinazzo (0000-0002-3392-9292 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Antonio La Greca (0000-0003-2740-143X Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Francesco Litta (0000-0003-1415-621X Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Caterina Mele (0000-0002-2003-9434 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Donato Paolo Pafundi (0000-0002-8981-9949 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy ), Elena Panettieri (0000-0001-7815-8092 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Valerio Papa (0000-0002-3709-8924 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Romeo Patini (0000-0001-7358-8763 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Romeo Patini (0000-0001-7358-8763 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Gerardo Perrotta (0000-0001-6112-6596 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Caterina Puccioni (0000-0001-6092-7957 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Pietro Santocchi (0009-0003-1321-2491 Catholic University of the Sacred Heart—Policlinico Universitario Agostino Gemelli IRCCS Foundation, Roma, Italy), Giulia Armatura (0000-0002-8536-7551 Central Hospital of Bolzano), Stefano Olmi (0000 0002 8307 3402 Chief Director UOC General and Oncological Surgery Policlinico San Marco Zingonia), Gianmaria Casoni Pattacini (0000-0002-1106-4187 Civil Hospital of Baggiovara Modena), Stefano Salgarello (0000-0001-6558-9141 Clinica Odontoiatrica—Università degli Studi di Brescia), Mario Trompetto (0000-0002-1190-4692 Clinica S. Rita—Vercelli), Cristina Bombardini (0000-0002-6585-7932 university hospital of Ferrara, Ferrara, ITaly), Roberto La Rocca (0000-0001-7088-5674 Department of neuroscience Reproductive Sciences and Odontostomatological), Giuseppe Celentano (Department of Neurosciences Reproductive Sciences and Odontostomatological), Andrea Micalef (0000-0003-0026-2580 Department of Surgery General Surgery and Abdominal Transplant Uniti), Antonio Mazzella (0000-0002-5330-5495 European Oncological Institute), Alberto Settembrini (Fondazione IRCCS Policlinico), Cesare Zoia (Fondazione IRCCS Policlinico San Matteo Pavia), Luca Degrate (0000-0003-4176-5555 Fondazione IRCCS San Gerardo dei Tintori Monza Italy), Giovanbattista Musumeci (0000-0003-2503-4760 General Surgery Resident), Carmen Angela Maria Palopoli (0000-0003-0041-8936 General Surgery Resident), Giulia Montori (0000-0002-7649-2174 Vittorio Veneto hospital, Vittorio Veneto, Italy), Elena Bonati (0000-0002-6866-2962 General Surgical Clinic Universitary Hospital Agency of Parma), Vincenza Paola Dinuzzi (0000-0002-8023-5496 Hospital "G.Fornaroli" Magenta), Francesco Velluti (0000-0002-9225-0036 Hospital “Molinette” Città della salute e della Scienza di Torino), Andrea Balla (0000-0002-0182-8761 Hospital “San Paolo” Largo Donatori del Sangue 1 00053 Civitavecchia Rome Italy), Davide Edoardo Bonasia (0000-0002-8286-7243 Hospital Agency ordine mauriziano torino. Università degli studi di Torino), Diego Coletta (0000-0002-9116-0733 Hospital Agency Ospedali Riuniti Marche Nord), Marco Angrisani (0000-0001-6414-7835 Hospital Agency San Camillo-Forlanini), Giammauro Berardi (0000-0001-8827-9189 Hospital Agency San Camillo-Forlanini), Marco Colasanti (Hospital Agency San Camillo-Forlanini), Stefano Ferretti (Hospital Agency San Camillo-Forlanini), Camilla Gasparoli (0000-0000-0000-0000 Hospital Agency San Camillo-Forlanini), Germano Mariano (Hospital Agency San Camillo-Forlanini), Stefano Avenia (0000-0002-5818-6405 Hospital Agency Santa Maria di Terni General Surgery and Surgical Specialties ), Pasquale Cianci (0000-0003-2839-2520 Hospital Lorenzo Bonomo—ASL BAT), Luca Cestino (0000-0003-3119-8606 Maria Vittoria Hospital, Turin), Federico Festa (0000-0001-7685-588X Maria Vittoria Hospital, Turin), Federico Fazio (0000000291129365 Hospital Mauriziano Turin), Francesca Ascari (0000-0002-9959-0922 Hospital of Carpi AUSL Modena), Matteo Desio (0000-0002-4170-101X Hospital of Circolo Varese—ASST Settelaghi), Gabriela Aracelly Arroyo Murillo (0000-0002-3807-908X Hospital of Dolo ULSS3 Serenissima), Marco Cereda (Hospital San Gerardo Monza), raffaele galleano (0000-0001-9787-4908 Hospital san paolo savona asl2 ligure), Giulia David (Hospital sant'anna san fermo della battaglia, Italy), Antonio Pansini (0000-0002-2747-8106 IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy), Carlo Gazia (0000-0002-3543-4170 IRCCS—Regina Elena National Cancer Institute Rome Italy), Giulia Atzori (0000-0001-9206-9432 IRCCS Hospital Policlinico San Martino Genoa), Lorenzo Ferro Desideri (0000-0003-0715-6369 IRCCS Hospital Policlinico San Martino Genoa), Simone Famularo (0000-0002-9721-6304 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Jacopo Galvanin (0000-0003-1948-1126 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Veronica Maria Giudici (0000-0002-3550-3471 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Giuseppe Mangiameli (0000-0002-8394-2719 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Simona Mei (0000-0001-7952-0014 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Flavio Milana (0000-0003-3570-9573 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Andrea Pansa (0000-0002-7917-5617 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Matteo Sacchi (0000-0001-8313-4909 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Alberto Testori (0000-0002-3032-9494 IRCCS Humanitas Research Hospital Rozzano, Milan, Italy), Gabriele Di Carlo (0000000288460655 IRCCS-Istituto Ortopedico Rizzoli, Bologna, Italy.), Marco Paratore (0000-0001-8987-9354 IRCCS Ospedale Policlinico San Martino, Genova Italia), Umberto Perrone (0000-0003-0319-2186 IRCCS Ospedale Policlinico San Martino Unit Of Obstetrics And Gynecology Genova Italia ), Aldo Vagge (0000-0002-9346-9267 IRCCS Ospedale Policlinico San Martino Università di Genova DINOGMI), Jacopo Viganò (0000-0002-2319-5475 IRCCS Policlinico San Matteo Foundation Pavia), Beatrice Torre (0000-0002-7388-3241 IRCCS Policlinico Sant'Orsola Bologna), Mauro Alessandro Scotti (0000-0001-8723-4835 IRCCS San Gerardo Monza), Gabriele Carbone (0000-0002-2084-7407 IRCCS San Raffaele Scientific Institute), Raffaele Cerchione (0000-0003-3446-1430 IRCCS San Raffaele Scientific Institute), Paola De Nardi (0000-0002-9337-6765 IRCCS San Raffaele Scientific Institute), Lorenzo Gozzini (0000-0001-6605-4683 IRCCS San Raffaele Scientific Institute), Luca Ottaviani (0000-0002-4846-1354 IRCCS San Raffaele Scientific Institute), Carlotta Senni (0000-0002-0288-9208 IRCCS San Raffaele Scientific Institute), Ottavio Piccin (0000-0002-0184-7460 IRCSS Azienda Ospedaliero Universitaria di Bologna), Luca Pio (0000-0002-3776-9994 Istituto Giannina Gaslini ), Francesco Colombo (0000-0002-6478-7055 L. Sacco University Hospital Milano), Riccardo Avantifiori (La Sapienza University of Rome), Valeria Baldassarri (0000-0002-0677-3894 "La Sapienza" University, Rome, Italy), Roberto Caronna (0000-0002-4683-2756 La Sapienza University of Rome), Pierfranco Maria Cicerchia ( 0000-0003-0324-7810 La Sapienza University of Rome), Diletta Corallino (0000-0002-4937-4332 La Sapienza University of Rome), Daniele Crocetti (0000-0001-9950-3553 La Sapienza University of Rome), Gaetano Gallo (0000-0003-1066-4671 La Sapienza University of Rome), Luca Giordano (La Sapienza University of Rome), Francesco Giovanardi (0000-0002-8395-2722 La Sapienza University of Rome), Francesca Giovannetti (0000-0002-7661-6675 La Sapienza University of Rome), Redan Hassan (0000-0003-2925-8972 La Sapienza University of Rome), Angelo Iossa (0000-0002-6798-8100 La Sapienza University of Rome), Quirino Lai (0000-0003-1487-3235 La Sapienza University of Rome), Francesco Lancellotti (0000-0002-1830-127X La Sapienza University of Rome), Alessio Lucarini (0000-0002-9644-740X La Sapienza University of Rome), Sara Lucchese (0000-0002-1807-4513 La Sapienza University of Rome), Gennaro Mazzarella (0000-0002-1206-9051 La Sapienza University of Rome), Fabio Melandro (0000-0003-4056-9245 La Sapienza University of Rome), Andrea Minervini (La Sapienza University of Rome), Edoardo Maria Muttillo (0000-0003-3562-0392 La Sapienza University of Rome), Livia Palmieri (0000-0003-2499-3580 La Sapienza University of Rome), Rocco Pasqua (0000-0003-3698-7348 La Sapienza University of Rome), Gianmarco Piccolino (0009-0003-9692-6886 La Sapienza University of Rome), Francesco Rosiello (La Sapienza University of Rome), Giacomo Salina (La Sapienza University of Rome), Simone sibio (0000-0002-5694-951X La Sapienza University of Rome), Pasqualino Sirignano (0000-0002-1312-1915 La Sapienza University of Rome), Mariarita Tarallo (0000-0003-3783-4749 La Sapienza University of Rome), Sofia Usai (0000-0002-3789-2108 La Sapienza University of Rome), Camilla Vanni (0000-0001-5218-6757 La Sapienza University of Rome), Edoardo Viglietta (0000-0002-5523-4846 La Sapienza University of Rome), Martina Zambon (0000-0003-2542-9404 La Sapienza University of Rome), Nunzia Ivana Conversano (0000-0003-3817-1430 Lorenzo Bonomo Hospital, Andria, Italy), Angelo Gabriele Epifani (0000-0002-2086-8232 Luigi Sacco University Hospital Study University of Milan Italy), Valentina Milano (0000-0001-6421-8904 Mater Olbia), Luca Sacco (0000-0003-1007-9894 Mazzini Hospital Teramo), Mariachiara Nava (Med chir spec Chirurgia Plastica), Anna Maffioli (0000-0001-7116-4019 Medical Director General Surgery ASST Fatebenefratelli Sacco Milan), Simona Giuratrabocchetta (0000-0002-2611-3674 Medical Director general Surgery San Paolo Milano Hospital), Filippo Baracchi (Medical Director General Surgery and Oncology ASO Santa Croce e Carle Cuneo), Michele Zuolo (0000-0002-3318-6054 Medical Director General Surgery Ospedale "Valli del Noce" Cles APSS Trento), Marco Ceresoli (Milano-Bicocca university School of Medicine and Surgery), Daunia Verdi (0000-0003-2282-2163 Mirano Hospital), Andrea Belli 0000-0002-6252-573X National Institute of Tumours—IRCCS—G. Pascale), Francesco Pata (0000-0003-2634-1199 Nicola Giannettasio Hospital Corigliano-Rossano Italy), Elisa Piovano (0000-0002-5629-703X Obstetrics and Gynecology Unit n 3—AOU Città della Salute e della Scienza di Torino—Presidio Sant'Anna), Giovanlorenzo Pastore (0000-0003-2432-1741 Ophthalmic Unit Department of Neurosciences Biomedicine and Movement Sciences University of Verona Policlinico G.B. Rossi P.Le L.A Scuro 10 37134 Verona VR Italy), Federico Bernabei (0000-0003-0494-6293 Ophthalmology Unit S. Orsola-Malpighi University Hospital University of Bologna Italy), Selene Deiana (0000-0002-7372-0979 Ordine Medici di Genova N°17079), Alberto Arceri (0000-0002-6486-6300 Orthopaedics Institute Rizzoli), Claudio D'Agostino 0000-0003-2616-0662 Orthopaedics Institute Rizzoli), Chiara Marafante (0000-0001-7555-7784 Ospedale degli Infermi di Rivoli), Elisabetta Moggia (0000-0001-8664-5288 Ospedale degli Infermi Asl Torino 3 Rivoli), Sara Parini (0000-0002-6021-6247 Ospedale Maggiore della Carità di Novara Italy), Marco Moretti (Ospedale MG Vannini), Fabio Uggeri (0000-0002-2209-3602 Ospedale San Gerardo di Monza Study University of Milano-Bicocca), Nicholas Pontarolo (ospedale vittorio Veneto ULSS 2), Tommaso Fontana (0000-0002-1511-855X P.O. “Vittorio Emanuele” Gela), Graziano Palmisano (P.O. Valle d'Itria), Mario Giuffrida (0000-0001-8335-3941 Parma University Hospital-General Surgery Unit), Eleonora Guaitoli (0000-0002-2363-874X Po valle d’itria), Carlotta Ferretti ( 0000-0002-1153-4177 Poliambulanza), Giorgia Iacopino (0000-0001-8448-0475 Policlinico di Milano Ospedale Maggiore), Rossella Gioco (0000-0003-3608-6187 Policlinico G.Rodolico Study University of Catania), Giuseppe Roscitano (0000-0001-9529-7561 Policlinico G.Rodolico Study University of Catania), Paolo Montanelli (0000-0001-5400-411X Policlinico San Martino), Maria Francesca Chiappetta (0000 0002 6995 5409 Policlinico San Pietro), Enrico Pinotti (0000-0003-3063-4170 Policlinico San Pietro), Erica Monati (0000-0002-1403-6237 Residency in General Surgery University of Firenze), Giada Fazio (0000-0001-6325-9915 resident at Hospital S. Anna Cona Ferrara), Francesco Di Pietro (0000-0002-9569-0555 Resident in General Surgery), Francesco Damarco (0000-0003-0847-2363 S.C. Thoracic Surgery and of Lung Transplantats Cardiac-Thoracic-Vascular Department—Foundation IRCCS Ca' Granda Hospital Maggiore Policlinico Milano), Andrea Barberis (0000-0003-0472-0120 S.C. General Surgery and Hepatobiliopancreatic surgery E.O. Ospedali Galliera Genoa), Andrea Razzore (0000-0002-7300-725X S.C. HPB and General Surgery E.O. Ospedali Galliera di Genova), Angelo Pascale (0000-0003-3261-0607 S.I.C. Oculistica Azienda Ospedaliera Regionale San Carlo via Potito Petrone 85100 Potenza Italy), Sara Loi (0000-0002-9278-8602 S.O. Obstetrics and Gynecology Nostra Signora della Mercede Hospital ASL Ogliastra-Lanusei), francesco ferrara (0000-0002-8208-1945 San Carlo Borromeo Hospital ASST Santi Paolo e Carlo Milan Italy), Matteo Rossi (0000-0002-3733-8668 Department of General Surgery and Surgical Oncology, San Filippo Neri Hospital, Rome, Italy), Giorgio Lisi (0000-0002-3842-0815 Sant’Eugenio Hospital), Giovanni Viel (0000-0001-9972-7688 Santa Chiara Hospital Trento 38122 Italy), Diego Sasia (0000-0003-3162-4302 Santa Croce and Carle Hospital Cuneo), Dario Bono (0000-0002-7376-447X SC General Surgery PO Borgosesia(VC), ), Emanuele Rampino Cordaro (0000-0001-6024-8647 SOC Plastic Surgery—Ospedale di Udine), Elena Giacomelli (0000-0003-1985-6434 SOD Vascular Surgery-Universitary Hospital Agency Careggi Firenze), Iacopo Giani (0000-0001-6077-6319 SOSD Proctology—USL Toscana Centro), Luca Seriau (SSD Breast Surgery Ospedale di Udine ASUFC), Gianluca Pellino (0000-0002-8322-6421 Study University of Campania Luigi Vanvitelli Naples Italy), Marco Sparavigna (0000-0002-9925-2851 Study University of Genoa), Giuseppe Trigiante (0000-0001-9906-1468 Study University of Bari—General Surgery M. Rubino), Roberto Giuseppe D’Ambrogio (0000-0002-0728-2456 Study University of Brescia), Francesca Cardella (0000-0001-9068-5223 Study University of Campania Luigi Vanvitelli), Sara Guzzetti (0000-0002-7936-4477 Study University of Genoa), Andrea-Pierre Luzzi (0000-0003-4218-3848 Study University of Genoa), Giacomo Carganico (0000-0001-5779-9632 Study University of Genova), Beatrice Drago (0000-0003-3875-6631 Study University of Genova), Giancarlo Micheletto (0000-0003-3687-1126 Study University of Milan), Riccardo Orlandi (Study University of Milano—Statale), Carmen Cutolo (0000-0002-4476-2686 Study University of Salerno), Umberto Gibello (0000-0002-9957-9838 Study University of Turin), Massimiliano Mistrangelo (0000-0001-8506-6794 Study University of Turin), Edoardo Forcignanò (0000-0002-1738-7569 Study University of Turin- Department of Surgical Sciences), Stefano D'Ugo (0000-0002-7073-0565 Surgery Department UOC General Surgery Hospital "V. Fazzi" Lecce), Pasquale Losurdo (0000-0002-7230-2046 Surgical Clinic Unit Department of Medical and Surgical Sciences Hospital of Cattinara University of Trieste Strada di Fiume 447 34149 Trieste Italy), Mattia Manitto (0000-0001-5990-0933 Thoracic Surgeon), Guido Caroli (0000-0002-9470-154X Thoracic Surgery AUSL Romagna), Melania Franco (0000-0003-4840-3901 U.O. Otolaryngology Hospital Sand Donato Arezzo), Pier Luigi Tilocca (0000-0003-1195-1381 U.O. Surgical Pathology Azienda Ospedaliera Universitaria di Sassari), Paolo Mendogni (0000-0002-4303-6244 U.O. Thoracic Surgery and Lung Transplant Foundation ), Giuseppe Sena (0000-0001-9793-3250 U.O. Vascular Surgery A.O. "Pugliese-Ciaccio" Catanzaro), Daniele Sambucci (0000-0002-6177-7046 U.O.C. General Surgery Ospedale di Conegliano (TV), AULSS2 Marca Trevigiana), Claudio Luciani (0000-0002-9819-8582 U.O.C. General Surgery P.O. “A. Cardarelli” ASReM Campobasso), Pietro Atelli (0000-0003-3284-5676 A.Cardarelli Naples), Agostino Guida (0000-0003-0177-1301 A.Cardarelli Naples), Fabio Marino (0000-0002-7535-436X U.O.C. of Surgery IRCCS “Saverio de Bellis”—Castellana Grotte (Ba), ), Andrea Morini (0000-0001-9140-0488 U.O.C. Oncological Surgery—Arcispedale Santa Maria Nuova—AUSL\IRCCS Reggio Emilia), Maria Grazia Sibilla (0000-0002-9166-6275 U.O.C. Surgery 2 Azienda Ospedaliera Universitaria di Ferrara), Filippo Longo (0000-0001-6769-1684 U.O.C. Thoracic Surgery), Sara Giaccari (0000-0002-8356-7525 ULSS2 Marca Trevigiana—U.O.C. General Surgery Hospital of Conegliano), Vincenzo Vigorita (0000-0003-2142-4737 Unit of Coloproctology Complesso Universitario di Vigo), Alberto Balduzzi (0000-0001-6018-8816 Unit of General and Pancreatic Surgery Department of Surgery and Oncology University of Verona Hospital Trust Italy), Fabio Barra (0000-0003-4117-6603 Unit of Obstetrics and Gynecology P.O. "Ospedale del Tigullio"- ASL4 Metropolitan Area of Genoa Genoa Italy), Daniele Delogu (0000-0002-7538-1229 Universitary Hospital Agency of Sassari), Erica Milone (0000-0001-9451-3154 Universitary Hospital Agency "G.Martino"—Messina—Department of Time-Related Emergencies), Lapo Bencini (0000-0001-6331-5542 Universitary Hospital Agency Careggi Firenze), Vittorio Aprile (0000-0001-8538-1719 Universitary Hospital Agency Pisana), Piermarco Papini (0000-0002-4764-2161 Universitary Hospital Agency Pisana—Pisa—Italy), Nicola Montemurro (0000-0002-3686-8907 Universitary Hospital Agency Pisana University of Pisa Pisa Italy) Matteo Cavallo (0000-0002-6093-6033 Universitary Hospital Agency Policlinico “G. Rodolico”- San Marco), Catania Arcangelo Picciariello (0000-0002-6361-1111 University “Aldo Moro” of Bari Department of Emergency and Organ Transplantation), Giovanni Tomasicchio ( 0000-0001-7017-2690 University “Aldo Moro” of Bari Piazza G Cesare 11 70124 Bari Italy), Alessandra Fittipaldi (0009-0002-9163-1248 University Hospital of Catania Italy), Denisa Eskiu (University "Our Lady of Good Council", Tirana, Albania) Michele Maruccia (0000-0002-2122-2732 University of Bari Aldo Moro unit pf plastic and Reconstructive Surgery with Burn Unit), Simone Gerardi (0000-0002-6979-5820 University of Bologna), Nicola Cillara (0000-0001-6877-2267 University of Cagliari, Cagliari, Italy), Simona Deidda (0000-0002-7756-9727 University of Cagliari, Cagliari, Italy), Giuseppe Demarinis (0000-0002-9298-1963 University of Cagliari, Cagliari, Italy), Enrico Peiretti (0000-0003-1088-0163 University of Cagliari, Cagliari, Italy), Filippo Tatti 0000-0002-8630-0367 University of Cagliari, Cagliari, Italy), Claudio Iovino (0000-0003-1984-0555 University of Campania Luigi Vanvitelli Naples Italy), Gaetano Isola (0000-0003-4267-6992 University of Catania Italy), Valerio Calogero Progno (0000-0002-7078-6323, University of Catania, Catania, Italy), Marcello Migliore (0000-0002-6272-8983 University of Catania Italy), Giorgio Badessi (0000-0002-7773-0971 University of Messina Via Consolare Valeria Messina 98125 Italy), Chiara Barillà (0000-0002-1277-1457 University of Messina Via Consolare Valeria Messina 98125 Italy), Gaetano Silvio Calleri (0000-0001-5185-7600 University of Messina Via Consolare Valeria Messina 98125 Italy), Stefano Cianci (0000-0002-0548-9891 University of Messina Via Consolare Valeria Messina 98125 Italy), Fausto Fama' (0000-0002-9017-1991 University of Messina Via Consolare Valeria Messina 98125 Italy), Francesco Fleres (0000-0002-1092-8975 University of Messina Via Consolare Valeria Messina 98125 Italy), Carmelo Mazzeo (0000-0001-9893-7480 University of Messina Via Consolare Valeria Messina 98125 Italy), Mario Gaetano Visaloco (0000-0002-9514-1484 University of Messina Via Consolare Valeria Messina 98125 Italy), Carlo Marchetto (0000-0001-5924-4868 University of Milan Italy), Federico Bolognesi (0000-0002-4143-3692 University of Milan Italy / University of Bologna Bologna Italy), Laura Benuzzi (0000-0003-1542-2807 University of Milan Milan Italy), Greta Bracchetti (0000-0002-6562-8152 University of Milan Milan Italy), Francesco Brucchi (0000-0003-3191-4369 University of Milan Milan Italy), Carlo Alberto Manzo (0000-0002-2401-3434 University of Milan Milan Italy), Luca Scaravilli (0000-0002-1326-1862 University of Milan Milan Italy), Carlo Ferrari (0000-0001-5118-2340 University of Milan Milan Italy), Aldo Rocca (0000-0003-3807-3865 University of Molise Campobasso 86100 Italy), Pasquale Napolitano (0000-0001-6044-7486 University of Molise Via Francesco De Sanctis 1 Campobasso 86100 Italy), Pietro Anoldo (0000-0001-6727-2973 University of Naples Federico II, Naples, Italy), Chiara Caricato (0000-0002-3771-9444 University of Naples Federico II, Naples, Italy), Michele Manigrasso (0000-0001-8204-7942 University of Naples Federico II, Naples, Italy), Marco Milone (0000-0001-5612-1926 University of Naples Federico II, Naples, Italy ), Luigi Napolitano (0000-0003-2036-0356 University of Naples Federico II, Naples, Italy), Giuseppe Palomba (0000-0003-3954-5166 University of Naples Federico II, Naples, Italy), Vincenzo Schiavone (0000-0002-0533-5833 University of Naples Federico II, Naples, Italy), Martino Vetrella (University of Naples Federico II, Naples, Italy), Ugo Grossi (0000-0001-5372-2873 University of Padua), Lucia Moletta (0000-0003-4041-5731 University of Padua, Padova, Italy), Alfredo Annicchiarico (0000-0003-3882-776X University of Parma, Parma, Italt), Ivan Vella (0000-0002-4946-512X University of Pavia, Pavia, Italy), Giuseppe Talesa (0000-0002-8530-4200 Università degli Studi di Perugia, Perugia, Italy), Ugo Boggi (0000-0002-7505-5896 University of Pisa, Pisa, Italy), Francesco Aiello (0000-0001-6479-1807 University of Rome “Tor Vergata”, Rome, Italy), Alessandro Anselmo (0000-0003-1041-8120 University of Rome “Tor Vergata”, Rome, Italy), Amedeo Antonelli (0000-0002-5773-6962 University of Rome “Tor Vergata”, Rome, Italy), Giulia Bacchiocchi (0000-0002-9755-6229 University of Rome “Tor Vergata”, Rome, Italy), Federico Beati (0000-0003-3408-3038 University of Rome “Tor Vergata”, Rome, Italy), vittoria bellato (0000-0003-0123-1700 University of Rome “Tor Vergata”, Rome, Italy), Federica Billeci (0000-0002-4749-5376 University of Rome “Tor Vergata”, Rome, Italy), Francesca Blasi (0000-0002-1058-1174 University of Rome “Tor Vergata”, Rome, Italy), Oreste Claudio Buonomo (0000-0002-9531-8737 University of Rome “Tor Vergata”, Rome, Italy), Michela Campanelli (0000-0002-2134-2275 University of Rome “Tor Vergata”, Rome, Italy), Giulia Coco 0000-0002-2410-6366 University of Rome “Tor Vergata”, Rome, Italy), Alessia Contadini (0000-0002-3458-6674 University of Rome “Tor Vergata”, Rome, Italy), Luigi Eduardo Conte (0000-0002-1280-8029 University of Rome “Tor Vergata”, Rome, Italy), Giulia D'Ippolito (0000-0001-8613-1236 University of Rome “Tor Vergata”, Rome, Italy), Arianna Di Marcantonio (0000-0003-2293-291X University of Rome “Tor Vergata”, Rome, Italy), Claudia Fede Spicchiale (0000-0003-3181-6769 University of Rome “Tor Vergata”, Rome, Italy), Gabriele Gallo Afflitto (0000-0003-0013-6189 University of Rome “Tor Vergata”, Rome, Italy), Alice Gismondi (0000-0002-3484-8814 University of Rome “Tor Vergata”, Rome, Italy), Giulio Gorgolini (0000-0002-0301-9001 University of Rome “Tor Vergata”, Rome, Italy), Alessandra Vittoria Granai (0000-0002-5808-9306 University of Rome “Tor Vergata”, Rome, Italy), Simona Grande (0000-0002-8804-1952 University of Rome “Tor Vergata”, Rome, Italy),Andrea Gravina (0000-0002-5773-4270 University of Rome “Tor Vergata”, Rome, Italy), Andrea Martina Guida (0000-0002-0968-6956 University of Rome “Tor Vergata”, Rome, Italy), Sara Ingallinella (0000-0002-5600-2799 University of Rome “Tor Vergata”, Rome, Italy), Laura Keci (0000-0001-9451-961X University of Rome “Tor Vergata”, Rome, Italy), Eleonora Latini (0000-0003-0032-215X University of Rome “Tor Vergata”, Rome, Italy), Davide Marino (0000-0001-8438-4774 University of Rome “Tor Vergata”, Rome, Italy), Fabio Massimo Oddi (0000-0001-8081-807X University of Rome “Tor Vergata”, Rome, Italy), Luca Orecchia (0000-0001-8376-5380 University of Rome “Tor Vergata”, Rome, Italy), Cristine Brooke Pathirannehalage Don (0000-0003-0522-927X University of Rome “Tor Vergata”, Rome, Italy), Marco Pellicciaro (0000-0001-9557-2850 University of Rome “Tor Vergata”, Rome, Italy), Lorenzo Petagna (0000-0003-0467-550X University of Rome “Tor Vergata”, Rome, Italy), Brunella Maria Pirozzi (0000-0002-0683-0967 University of Rome “Tor Vergata”, Rome, Italy), Claudia Quaranta (0000-0002-6919-729X University of Rome “Tor Vergata”, Rome, Italy), Maurizio Rho (0000-0002-9432-5628 University of Rome “Tor Vergata”, Rome, Italy), Alessandro Rosina (University of Rome "Tor Vergata"), Maria Sara Santicchia (University of Rome "Tor Vergata"), Federica Saraceno (0000-0002-6600-8350 University of Rome “Tor Vergata”, Rome, Italy), Alfonso Schiavone (0000-0001-8439-2950 University of Rome “Tor Vergata”, Rome, Italy), Bruno Sensi (0000-0003-1912-2414 University of Rome “Tor Vergata”, Rome, Italy), Alessandra Spina (0000-0002-6400-6642 University of Rome “Tor Vergata”, Rome, Italy), Luca Sullo (0000-0002-0371-715X University of Rome “Tor Vergata”, Rome, Italy), Federico Tacconi (0000-0001-8850-5027 University of Rome “Tor Vergata”, Rome, Italy), Riccardo Tajè (University of Rome "Tor Vergata"), Gianluca Vanni (0000-0002-3006-5855 University of Rome “Tor Vergata”, Rome, Italy), Danilo Vinci (0000-0002-8215-5756 University of Rome “Tor Vergata”, Rome, Italy), Giulia Vita (University of Rome “Tor Vergata”, Rome, Italy), Giuseppe Alba (0000-0002-5122-988X University of Siena Italy), Simona Badalucco (0000-0001-6382-905X University of Siena Italy), Ludovico Carbone (0000-0003-2862-6788 University of Siena Italy), Osvaldo Carpineto Samorani (0000-0001-8993-7825 University of Siena Italy), Glauco Chisci (0000-0001-6992-324X University of Siena Italy), Roberto Cuomo (0000-0002-8396-095x University of Siena Italy), Alessandro Francia (0000-0001-9834-0414 University of Siena Italy), Daniele Fusario (0000-0002-2804-2814 University of Siena Italy), Bruno Gargiulo (0000-0002-0114-1038 University of Siena Italy), Edoardo Pasqui (0000-0001-6619-0159 University of Siena Italy), Leonardo Pasquetti (0000-0003-2559-3968 University of Siena, Siena, Italy), Pasquale Puoti (0000-0001-5416-7891 University of Siena Italy), Luca Resca (0000-0003-3138-605X University of Siena Italy), Jacopo Cumbo (0009-0000-0055-7341 University of Turin, Turin, Italy), Stefano Ganio (0000-0002-0600-0787 University of Turin, Turin, Italy), Giuseppe Vizzielli (0000-0002-2424-2691 University of Udine, Udine, Italy), Marco Anastasi (0000-0001-8837-053X University of Verona, Verona, Italy), Domenico Guerra (0000-0001-5639-6874 USL Umbria 1, Italy), Andrea Romanzi (0000-0003-3603-1338 Valduce Hospital, Como, Italy), Alberto Vannelli (0000-0002-8894-5361 Valduce Hospital, Como), Marco Baia (0000-0001-8594-6759 Zucchi Clinical Institutes, Italy)
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement. This research did not received grants from any founding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: LS; RA; MM; Methodology: MA; BZ; LG; RM; AC; Software: LS; MM; Formal analysis: RS; RM; Investigation: LS; MM; RA; LG; Data Curation: RS; RM; AC; Writing—Original Draft: LS; AC; MM; RA; BZ; Writing—Review and Editing: MA; BZ; RM Supervision: RA; AC; RM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
According to the IRB of Policlinico Tor Vergata, ethical approval for survey is not required. The study was conducted in accordance with CHERRIES criteria and registered under GovTrial NCT05323851.
Informed consent
Informed consent was obtained during the questionnaire administration.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the SPIGC Survey Collaborative Group are presented in the Acknowledgements section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siragusa, L., Angelico, R., Angrisani, M. et al. How future surgery will benefit from SARS-COV-2-related measures: a SPIGC survey conveying the perspective of Italian surgeons. Updates Surg 75, 1711–1727 (2023). https://doi.org/10.1007/s13304-023-01613-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01613-5