Abstract
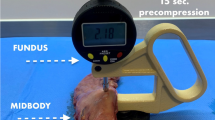
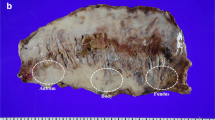
Leakage of the sleeve remains constant after laparoscopic sleeve gastrectomy (LSG). This complication may be due to a mismatch between the staple height and gastric wall thickness (GWT). Our aim was to measure the GWT in Chinese patients with obesity and investigate the relationship between GWT and gender, body mass index (BMI), body weight, and obesity-related comorbidities. The GWT of 210 resected specimens after LSG was measured using a tissue measuring device, at a compression pressure of 8 g/mm2 at three predetermined locations: antrum, midbody, and fundus. Two hundred ten patients (171 female/39 male). The gastric wall was thickest at the antrum followed by the midbody and thinnest at the fundus (3.02 mm, 2.22 mm, and 1.6 mm, respectively). Patients with gastritis and those with reflux esophagitis had thicker GWT at the antrum; male had thicker GWT at the antrum and fundus; patients with body weight > 100 kg, and those with BMI > 40 kg/m2 had thicker GWT at the fundus. Linear regression analysis revealed a significant association between GWT with body weight and BMI at the antrum and fundus; Furthermore, hypertension associated with the GWT at the fundus (P < 0.01, P < 0.01, P < 0.02, P < 0.01; and P < 0.04, respectively). This study showed that the anatomical location of the gastric wall is a major predicting factor of GWT. Furthermore, gastritis, reflux esophagitis, male gender, BMI > 40 kg/m2, body weight > 100 kg, and hypertension may increase the GWT at the antrum and fundus in Chinese patients with obesity.


Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N (2018) IFSO world survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28(12):3783–3794. https://doi.org/10.1007/s11695-018-3450-2
Chinese Obesity and Metabolic Surgery Collaborative, Chinese Society for Metabolic and Bariatric Surgery (2022) Chinese obesity and metabolic surgery database: annual report 2021. CJOM 08(1):15–23. https://doi.org/10.3877/cma.j.issn.2095-9605.2022.01.003
Bruzzi M, Douard R, Voron T, Berger A, Zinzindohoue F, Chevallier JM (2016) Open total gastrectomy with Roux-en-Y reconstruction for a chronic fistula after sleeve gastrectomy. Surg Obes Relat Dis 12(10):1803–1808. https://doi.org/10.1016/j.soard.2016.03.013
van de Vrande S, Himpens J, El Mourad H, Debaerdemaeker R, Leman G (2015) Management of chronic proximal fistulas after sleeve gastrectomy by laparoscopic Roux-limb placement. Surg Obes Relat Dis 9(6):856–861. https://doi.org/10.1016/j.soard.2013.01.003
Silva LB, Moon RC, Teixeira AF, Jaward MA, Ferraz AA, Neto MG, Ramos AC, Campos JM (2015) Gastrobronchial fistula insleeve gastrectomy and Roux-en-Y gastric bypass–a systematic review. Obes Surg 25(10):1959–1965. https://doi.org/10.1007/s11695-015-1822-4
Rebibo L, Fuks D, Blot C, Robert B, Boulet PO, Dhahri A, Verhaeghe P, Regimbeau JM (2015) Gastrointestinal bleeding complication of gastric fistula after sleeve gastrectomy: consider pseudoaneurysms. Surg Endosc 27(8):2849–2855. https://doi.org/10.1007/s00464-013-2833-7
Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc 26(6):1509–1515. https://doi.org/10.1007/s00464-011-2085-3
Gentileschi P, Camperchioli I, D’Ugo S, Benavoli D, Gaspari AL (2012) Staple-line reinforcement during laparoscopic sleeve gastrectomy using three different techniques: a randomized trial. Surg Endosc 26(9):2623–2629. https://doi.org/10.1007/s00464-012-2243-2
Bransen J, Gilissen LP, van Rutte PW, Nienhuijs SW (2015) Costs of leaks and bleeding after sleeve gastrectomies. Obes Surg 25(10):1767–1771. https://doi.org/10.1007/s11695-015-1584-z
Baker RS, Foote J, Kemmeter P, Brady R, Vroegop T, Servelt M (2004) The science of stapling and leaks. Obes Surg 14(10):1290–1298. https://doi.org/10.1381/0960892042583888
Barski K, Binda A, Kudlicka E, Jaworski P, Tarnowski W (2018) Gastric wall thickness and stapling in laparoscopic sleeve gastrectomy—a literature review. Wideochir Inne Tech Maloinwazyjne 13(13):122–127. https://doi.org/10.5114/wiitm.2018.73362
Endo Y, Ohta M, Kwamura M, Fujinaga A, Nakanuma H, Wataneba K, Kawasaki T, Masuda T, Hirashita T, Inomata M (2022) Gastric wall thickness and linear staple height in sleeve gastrectomy in Japanese patients with obesity. Obes Surg 32(2):349–354. https://doi.org/10.1007/s11695-021-05758-3
Gong S, Wang K, Li Y, Zhou Z, Alamia A (2021) Ethnic group differences in obesity in Asian Americans in California, 2013–2014. BCM Public Health 21(1):1589. https://doi.org/10.1186/s12889-021-11612-z
American Diabetes Association (2018) Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care 41(Suppl 1):S13-27. https://doi.org/10.2337/dc18-s002
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, Ballem N, Klidman M, Kothari S, ASMBS Clinical Issues Committee (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis 11(3):489–506. https://doi.org/10.1016/j.soard.2015.02.003
Elariny H, Gonzalez H, Wang B (2005) Tissue thickness of human stomach measured on excised gastric specimens from obese patients. Surg Technol Int 14:119–124
Rawlins L, Rawlins M, Teel D 2nd (2014) Human tissue thickness measurements from excised sleeve gastrectomy specimens. Surg Endosc 28(3):811–814. https://doi.org/10.1007/s00464-013-3264-1
Boeker C, Mall J, Reetz C, Yamac K, Wilkens L, Stroh C, Koehler H (2017) Laparoscopic sleeve gastrectomy: investigation of fundus wall thickness and staple height-an observational cohort study: fundus wall thickness and leaks. Obes Surg 27(12):3209–3214. https://doi.org/10.1007/s11695-017-2755-x
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel, Diaz AA, Arvidsson D et al (2015) International gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis 8:8-19.ectomy. https://doi.org/10.1016/j.soard.2011.10.019. (Obes Surg. 2015;25(12):2360–7)
Ergin A, Ciyiltepe H, Karip ABL et al (2021) The effect of Helicobacter pylori eradication on gastric wall thickness in patients undergoing laparoscopic sleeve gastrectomy. Obes Surg 31(9):4024–4032. https://doi.org/10.1007/s11695-021-05513-8
Yazar FM, Baykara M, Karaağaç M, Bülbüloğlu E (2016) The role of conventional ultrasonography in the evaluation of antrum wall thickness in obese patients. Obes Surg 26(12):2995–3000. https://doi.org/10.1007/s11695-016-2221-1
Abu-Ghanem Y, Meydan C, Segev L, Rubin M, Blumenfeld O, Spivak H (2017) Gastric wall thickness and the choice of linear staples in laparoscopic sleeve gastrectomy: challenging conventional concepts. Obes Surg 27(3):837–843. https://doi.org/10.1007/s11695-016-2516-2
Lee YJ, Kim YN, Park S (2020) Measurement of stomach wall thickness to guide staple selection during sleeve gastrectomy. Obes Surg 30(6):2140–2146. https://doi.org/10.1007/s11695-020-04439-x
Huang R, Gagner M (2015) A thickness calibration device is needed todetermine staple height and avoid leaks in laparoscopic sleeve gastr Rosenthal R, International Sleeve Gastrectomy Expert Panel. Obes Surg 25(12):2360–2367. https://doi.org/10.1007/s11695-015-1705-8
Chekan E, Whelan RL (2014) Surgical stapling device-tissue interactions: what surgeons need to improve patient outcomes. Med Devices (Auckl) 7:305–318. https://doi.org/10.2147/mder.s67338
Barski K, Binda A, Jaworski P et al (2022) Influence of preoperative weight loss on gastric wall thickness—analysis of laparoscopic sleeve gastrectomy histological material. Langenbecks Arch Surg 407:3315–3322. https://doi.org/10.1007/s00423-022-02668-5
Susmallian S, Goitein D, Barnea R, Raziel A (2017) Correct evaluation of gastric wall thickness may support a change in stapler’s size when performing sleeve gastrectomy. IMAJ 19:351–354
Larsen MC, Yan BM, Morton J, Van Gam J (2011) Determination of the relationship between gastric wall thickness and body mass index with endoscopic ultrasound. Obes Surg 21(3):300–304. https://doi.org/10.1007/s11695-009-9839-1
Funding
This work was supported by the Science and Technology Program of Xuzhou (KC22231).
Author information
Authors and Affiliations
Contributions
FKK, CS, and XZ contributed to the conception and design of the study. JW performed the statistical analysis. FKK wrote the first draft of the manuscript. CS and JH wrote sections of the manuscript. LY and XZ contributed to the revision of the manuscript, assistance, and funding. All authors have reviewed and agreed to the submission of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Author 1 declares that he has no conflict of interest. Author 2 declares that he has no conflict of interest. Author 3 declares that he has no conflict of interest. Author 4 declares that he has no conflict of interest. Author 5 declares that he has no conflict of interest. Author 6 declares that he has no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of The Affiliated Hospital of Xuzhou Medical University.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kitaghenda, F.K., Shu, C., Wang, J. et al. Measurement of gastric wall thickness after laparoscopic sleeve gastrectomy: obesity comorbidities and gastric wall in Chinese patients with obesity. Updates Surg 75, 1235–1242 (2023). https://doi.org/10.1007/s13304-023-01538-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01538-z