Abstract
Background
Staple line leakage is a well-known complication after laparoscopic sleeve gastrectomy (LSG). Gastric wall thickness and the staple height may be determining factors for the occurrence of insufficiencies. To investigate this problem, an observational cohort study was carried out. Investigation concentrated on the gastroesophageal junction close to the angle of His, since this area is at highest risk for a leakage.
Methods
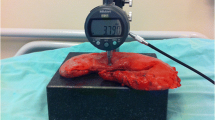
Fundus wall thickness of 141 specimens after LSG was measured by light microscopy at a predetermined location by a blinded pathologist. Furthermore, fundus wall thickness was compared with demographic data, clinical outcome, and the rate of insufficiencies.
Results
One hundred forty-one patients, 38 male and 103 female undergoing LSG, between January 2014 and July 2015 were included in the study. Male gender was associated with thicker gastric fundus wall. Overall leak rate was 2.1% (3/141). Median wall thickness of the 3 patients with detected leaks in the study group was thinner compared to the non-leak group (2810 vs. 3249 μm, respectively).
Discussion/Conclusion
Only male gender correlated with higher wall thickness of the fundus. The fact that all three patients who developed a leak were female, and the fundus of female patients as well as those of the leak group was thinner, indicates that wall thickness may have an impact on the rate of staple line leakage. Further studies with larger patient cohorts are needed.


Similar content being viewed by others
Change history
05 August 2019
There is an error in the published article. One patient���s gender was mistaken; it has been changed from female to male. Thus, the number of male and female patients in Tables��1 and 2, and the median and p value in Table 2 are incorrect.
05 August 2019
There is an error in the published article. One patient���s gender was mistaken; it has been changed from female to male. Thus, the number of male and female patients in Tables��1 and 2, and the median and p value in Table 2 are incorrect.
References
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat dis. 2009;5(4):469–75.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26(6):1509–15.
Al Hajj GN, Haddad J. Preventing staple-line leak in sleeve gastrectomy: reinforcement with bovine pericardium vs oversewing. Obes Surg. 2013;23(11):1915–21.
Knapps J, Ghanem M, Clements J, et al. A systematic review of staple-line reinforcement in laparoscopic sleeve gastrectomy. JSLS. 2013;17(3):390–9.
Kassir R, Blanc P, Amor IB, et al. Division of the stomach and checking on haemostasis for performing sleeve gastrectomy. Points of controversy. Obes Surg. 2015;25(3):537–8.
Benedix F, Benedix D, Knoll C, et al. Are there risk factors that increase the rate of staple line leakage in patients undergoing primary sleeve gastrectomy for morbid obesity? Obes Surg. 2014;24(10):1610–6.
Wölnerhanssen B, Peterli R. State of the art: sleeve gastrectomy. Dig Surg. 2014;31:40–7.
Baker RS, Foote J, Kemmeter P, et al. The science of stapling and leaks. Obes Surg. 2004;14(10):1290–8.
Abou Rached A, Basile M, El Masri H. Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol. 2014;20(38):13904–10.
Basso N, Casella G, Rizzello M, et al. Laparoscopic sleeve gastrectomy as first stage or definitive intent in 300 consecutive cases. Surg Endosc. 2011;25(2):444–9.
Stroh C, Köckerling F, Volker L, et al., Obesity Surgery Working Group; Competence Network Obesity. Results of more than 11,800 sleeve gastrectomies. Data analysis of the German Bariatric Surgery Registry. Ann Surg. 2016;263(5):949–55.
Ferrer-Márquez M, Belda-Lozano R, Ferrer-Ayza M. Technical controversies in laparoscopic sleeve gastrectomy. Obes Surg. 2012;22(1):182–7.
Elariny H, González H, Wang B. Tissue thickness of human stomach measured on excised gastric specimens from obese patients. Surg Technol Int. 2005;14:119–24.
Huang R, Gagner M. A thickness calibration device is needed to determine staple height and avoid leaks in laparoscopic sleeve gastrectomy. Obes Surg. 2015;25(12):2360–7.
Rawlins L, Rawlins MP, Donovan T. Human tissue thickness measurements from excised sleeve gastrectomy specimens. Surg Endosc. 2014;28(3):811–4.
Kunisaki C, Makino H, Takagawa R, et al. Prospective randomized controlled trial comparing the use of 3.5-mm and 4.8-mm staples in gastric surgery. Hepato-Gastroenterology. 2008;55(86–87):1943–7.
Nakayama S, Hasegawa S, Nakayama S, et al. The importance of precompression time for secure stapling with a linear stapler. Surg Endosc. 2011;25(7):2382–6.
Deutsche Adipositas Gesellschaft (DAG). Interdisziplinären Leitlinie der Qualität S3 zur “Prävention und Therapie der Adipositas”. Version 2.0 (April 2014). http://www.adipositas-gesellschaft.de/fileadmin/PDF/Leitlinien/050-001l_S3_Adipositas_Praevention_Therapie_2014-11.pdf
Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie (DGAV). S3-Leitlinie: Chirurgie der Adipositas. 2010. http://www.dgav.de/fileadmin/media/texte_pdf/caadip/leitlinie-chirurgie-deradipositas_2010-06.pdf
Mulisch M, Welsch U, editors. Romeis. Mikroskopische Technik. 18th ed. Heidelberg: Spektrum; 2010.
Acknowledgments
We would like to acknowledge the team of the Department of General, Visceral, Vascular and Bariatric Surgery and the operating room staff at Klinikum Nordstadt and the Department of Pathology of the Klinikum Nordstadt for their assistance and help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics
All procedures and collection of patient data followed the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Boeker, C., Mall, J., Reetz, C. et al. Laparoscopic Sleeve Gastrectomy: Investigation of Fundus Wall Thickness and Staple Height—an Observational Cohort Study. OBES SURG 27, 3209–3214 (2017). https://doi.org/10.1007/s11695-017-2755-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2755-x