Abstract
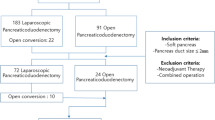
Laparoscopic techniques have been widely used in pancreatic surgery, such as laparoscopic pancreaticoduodenectomy (LPD) and laparoscopic central pancreatectomy (LCP). Laparoscopic pancreaticojejunostomy (LPJ) is a common procedure for LPD and LCP, and is also the most critical. The quality of LPJ is associated with the occurrence of clinically relevant postoperative pancreatic fistula (CR-POPF). Although LPJ technology has been greatly improved, CR-POPF cannot be completely avoided especially to soft pancreas, which is an important reason for the high risk of laparoscopic pancreatic surgery. To date, there is a lack of standard LPJ approaches. Here, we report a U-shaped suture reinforcement for soft pancreatic section combined with penetrating pancreaticojejunostomy (PPJ) technique, called U-PPJ. Twenty-three patients with soft pancreas who underwent laparoscopic pancreatic surgery adopting U-PPJ method between 2017 and 2022 were enrolled (LPD = 19, LCP = 4). Preoperative, intraoperative and postoperative indexes were collected and analyzed. The results showed that all patients treated with U-PPJ were discharged without drainage tube or a small amount of exudate in the drainage tube does not require clinical treatment, but only needs to be removed after 2 days of observation. The average operation time was 417.35 min. The intraoperative blood loss was 171.74 ml. The pancreatic duct diameter was 3.41 mm. The average postoperative hospitalization days were 11.83 days. The average postoperative drainage tube removal time was 13.26 days. The incidence of postoperative B-grade pancreatic fistula was 4.3%, and no C-grade pancreatic fistula occurred. In our experience, U-PPJ can be completed by a skilled surgeon in less than 20 min. U-PPJ is safe, reliable, convenient and has a low incidence of CR-POPF in soft pancreas, which is worthy of clinical application. It also provides more options for laparoscopic pancreatic surgery. Since this is a retrospective study with a small number of cases, more prospective multicenter studies are needed to further verify its safety and efficacy.

Similar content being viewed by others
Data availability
The current research data for statistical analysis has been uploaded to the “Supplementary Information” section.
References
Umemura A, Nitta H, Takahara T, Hasegawa Y, Sasaki A (2018) Current status of laparoscopic pancreaticoduodenectomy and pancreatectomy. Asian J Surg 41(2):106–114. https://doi.org/10.1016/j.asjsur.2016.09.003
Wu J, Zhang G, Yao X, Xiang Y, Lin R, Yang Y, Zhang X (2020) Achilles’ heel of laparoscopic pancreatectomy: reconstruction of the remnant pancreas. Expert Rev Gastroenterol Hepatol 14(7):527–537. https://doi.org/10.1080/17474124.2020.1775582
Olakowski M, Grudzińska E, Mrowiec S (2020) Pancreaticojejunostomy-a review of modern techniques. Langenbecks Arch Surg 405(1):13–22. https://doi.org/10.1007/s00423-020-01855-6
Poves I, Morató O, Burdío F, Grande L (2017) Laparoscopic-adapted Blumgart pancreaticojejunostomy in laparoscopic pancreaticoduodenectomy. Surg Endosc 31(7):2837–2845. https://doi.org/10.1007/s00464-016-5294-y
Cai Y, Luo H, Li Y, Gao P, Peng B (2019) A novel technique of pancreaticojejunostomy for laparoscopic pancreaticoduodenectomy. Surg Endosc 33(5):1572–1577. https://doi.org/10.1007/s00464-018-6446-z
Tang W, Qiu JG, Li GZ, Zhao YF, Du CY (2021) Clinical application of “Double R” anastomosis technique in laparoscopic pancreaticoduodenectomy procedure. Medicine (Baltimore) 100(21):e26204. https://doi.org/10.1097/MD.0000000000026204
Hong D, Li H, Liu X, Jiang P, Yu G, Liu X, Liu J, Liu Y, Liu J, Lau WY (2022) Incidence of postoperative pancreatic fistula after using a defined pancreaticojejunostomy technique for laparoscopic pancreaticoduodenectomy: a prospective multicenter study on 1033 patients. Int J Surg 101:106620. https://doi.org/10.1016/j.ijsu.2022.106620
Lee B, Yoon YS, Kang CM, Choi M, Lee JS, Hwang HK, Cho JY, Lee WJ, Han HS (2021) Fistula risk score-adjusted comparison of postoperative pancreatic fistula following laparoscopic vs open pancreatoduodenectomy. J Hepatobiliary Pancreat Sci 28(12):1089–1097. https://doi.org/10.1002/jhbp.866
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M (2017) International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591. https://doi.org/10.1016/j.surg.2016.11.014
Capretti G, Bonifacio C, De Palma C, Nebbia M, Giannitto C, Cancian P, Laino ME, Balzarini L, Papanikolaou N, Savevski V, Zerbi A (2022) A machine learning risk model based on preoperative computed tomography scan to predict postoperative outcomes after pancreatoduodenectomy. Updates Surg 74(1):235–243. https://doi.org/10.1007/s13304-021-01174-5
Peng X, He Y, Tang Y, Yang X, Huang W, Li J, Zheng L, Huang X (2022) Preliminary experience on laparoscopic pancreaticoduodenal combined with major venous resection and reconstruction anastomosis. Front Surg 9:974214. https://doi.org/10.3389/fsurg.2022.974214
Kawaida H, Kono H, Hosomura N, Amemiya H, Itakura J, Fujii H, Ichikawa D (2019) Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery. World J Gastroenterol 25(28):3722–3737. https://doi.org/10.3748/wjg.v25.i28.3722
Zhang B, Yuan Q, Li S, Xu Z, Chen X, Li L, Shang D (2022) Risk factors of clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy: a systematic review and meta-analysis. Medicine (Baltimore) 101(26):e29757. https://doi.org/10.1097/MD.0000000000029757
Hong SS, Chong JU, Hwang HK, Lee WJ, Kang CM (2021) Laparoscopic pancreaticoduodenectomy reduces incidence of clinically relevant postoperative pancreatic fistula in soft pancreas with a smaller than 2 mm pancreatic duct. Surg Endosc 35(12):7094–7103. https://doi.org/10.1007/s00464-020-08226-8
Edil BH, Cooper MA, Makary MA (2014) Laparoscopic pancreaticojejunostomy using a barbed suture: a novel technique. J Laparoendosc Adv Surg Tech A 24(12):887–891. https://doi.org/10.1089/lap.2014.0053
Acknowledgements
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided and Hui Wang for offering us a hand-drawn surgical map.
Funding
This study was funded by the Anhui province key research and development project (202004j07020051) and Yijishan Hospital talent introduction and peak plans (YR202122, GF2019T03, GF2019G03).
Author information
Authors and Affiliations
Contributions
Daohai Qian and Bin Liu designed and conducted this study, analyzed the result and wrote the paper; Shihang Xi and Xu Wang managed the patients and collected clinical data; Xiaoming Wang revised the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
DHQ: no conflict; BL: no conflict; SHX: no conflict; XW: no conflict; XMW: no conflict.
Research involving human participants and/or animals
The authors declare that no experiments were performed on humans or animals for this study.
Informed consent
This retrospective study was approved and the requirement to obtain informed written consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 275318 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qian, D., Liu, B., Xi, S. et al. Application of a sectional U-shaped reinforcement combined with penetrating pancreaticojejunostomy (U-PPJ) for soft pancreas in laparoscopic pancreatic surgery. Updates Surg 75, 1117–1122 (2023). https://doi.org/10.1007/s13304-023-01468-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01468-w