Abstract
Since its introduction, the minimally invasive treatment of groin hernias has become widely accepted as a viable alternative to open surgery. Still, the rates and reasons for its adoption vary highly among countries and the regions within a country. After almost thirty years since its introduction, its spread is still limited. The present study, conducted under the auspices of AGENAS (Italian National Agency for Regional Services), aims at giving a snapshot of the spreading of minimally invasive and robotic techniques for the treatment of groin hernia in Italy. This study is retrospective, with data covering the period from 1st January 2015 to 31st December 2020. AGENAS provided data using the operation and diagnosis codes used at discharge and reported in the International Classification of Diseases 9th revision (ICD9 2002 version). Admissions performed on an outpatient basis, i.e., without an overnight stay of at least one night in hospital, were excluded. A total of 33,925 laparoscopic hernia repairs were performed during the considered period. Overall, a slight increase in the number of procedures performed was observed from 2015 to 2019, with a mean annual change of 8.60% (CI: 6.46–10.74; p < 0.0001). The number of laparoscopic procedures dropped in 2020, and when considering the whole period, the mean annual change was − 0.98% (CI: − 7.41–5.45; p < 0.0001). Urgent procedures ranged from 335 in 2015 to 508 in 2020 referring to absolute frequencies, and from 0.87% to 9.8% in relative frequencies of overall procedures in 2017 and 2020, respectively (mean = 4.51%; CI = 3.02%–6%; p < 0.001). The most relevant observation that could be made according to our analysis was that the adoption of the laparoscopic approach knew a slow but steady increase from 2015 onward.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical risks and technical difficulties initially hindered the spread of the minimally invasive approach to groin hernia. The possible severe complications and the need for general anesthesia to treat a benign disease that could instead be treated with little risk and under local anesthesia through the open anterior approach contributed to the slowdown in the spread of minimally invasive techniques. After an initial difficulty, several studies and subsequently the EHS (European Hernia Society) and EAES (European Association of Endoscopic Surgery) guidelines have demonstrated the safety and the advantages of the laparoendoscopic approach in the treatment of groin hernia [1, 2]. The high incidence of the disease has made groin hernia repair the most widely performed surgery today, with about 20 million operations per year. About 1.6 million visits are made each year in the United States for problems related to inguinal-crural hernias; the lifetime risk of developing an inguinal hernia is approximately 27–43% in males and 3–6% in females [3, 4]. The initial indications for treating inguinal hernias by laparoendoscopic approach were recurrences after the anterior approach and bilateral inguinal hernias, thus reducing the scope of this approach [5]. However, the Hernia Surge Group has recently shown that the laparoendoscopic approach can be considered safe even for unilateral inguinal hernias when performed by experienced surgeons [1]. The present study, conducted under the auspices of AGENAS (Italian National Agency for Regional Services), aims at giving a snapshot of the spreading of minimally invasive and robotic techniques for the treatment of groin hernia in Italy.
Materials and methods
This study is retrospective, with data covering the period from 1st January 2015 to 31st December 2020. AGENAS provided data using the operation and diagnosis codes used at discharge and reported in the International Classification of Diseases 9th revision (ICD9 2002 version). Admissions performed on an outpatient basis, i.e., without an overnight stay of at least one night in hospital, were excluded. Operations performed by laparoscopic and robotic techniques in patients older than 18 were considered. The coding and diagnosis codes are summarized in Table 1. Operations performed in association with minimally invasive surgery codes are also present in Table 1. Data from admission codes allowed for assessing gender, age, length of hospital stay and associated neurological and cardiovascular comorbidities. In addition, complications, readmission and 30-day mortality were assessed. No data were reported regarding the type of facility (public or private) where the operations were performed.
Statistical analysis
Data were processed using the MedCal statistical package (version 12.5). Qualitative variables were summarized by frequency and percentage, while normally distributed quantitative variables were described by the mean and standard deviation (SD). Statistical analysis was performed using Student's t-test and the Cochran Armitage test for trend as appropriate. A two-tailed p-value < 0.05 was considered statistically significant. The annual intervention rate (AIR) per 100,000 population was calculated, assessing the changes in the considered period. The sample size was the Italian population, reported by region, according to the average yearly population on 31st December from 2015 to 2020, reported by the Italian National Institute of Statistics (ISTAT) (Supplemental Table S1).
Results
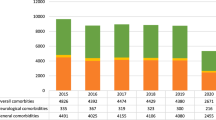
A total of 33,925 laparoscopic hernia repairs were performed during the considered period. Overall, a slight increase in the number of procedures performed was observed from 2015 to 2019, with a mean annual change of 8.60% (CI: 6.46–10.74; p < 0.0001). The number of laparoscopic procedures dropped in 2020, and when considering the whole period, the mean annual change was − 0.98% (CI: − 7.41–5.45; p < 0.0001). The percentage of laparoscopic procedures on the count of total procedures rose from 3.56% in 2015 to 5.98% in 2020. The percentage of laparoscopic procedures performed for bilateral inguinal hernias was almost similar to those performed for monolateral hernias in the whole period (Fig. 1).
The majority of patients were male (> 87% in the whole period), and the mean age was not statistically different (p = 0.972).
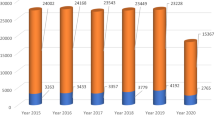
The procedures performed with robotic assistance were 275 in total; however, the use of the robot increased in the considered period with a mean annual change of 10.67% (CI = 2.83%–18.51%) (Fig. 2).
The conversion rate to open surgery decreased from 2015 to 2019 with a mean annual change of − 1.14% (CI: − 10.2%–7.92%; p = 0.429). However, the decrease was not significantly different (p = 0.429) even when including 2020 in the analysis (p = 0.563).
Urgent procedures ranged from 335 in 2015 to 508 in 2020 referring to absolute frequencies, and from 0.87% to 9.8% in relative frequencies of overall procedures in 2017 and 2020 respectively (mean = 4.51%; CI = 3.02% – 6%; p < 0.001) (Fig. 3).
Overall, there was a slight but not significant increase in the complication rate in the whole period (mean annual change = 3.06%; CI = − 1.94%–8%; p = 0.603). Conversely, in 2020, the readmission rate dropped, with a mean annual change of − 38% when considering the whole period (CI:− 77.16%–1.16%; p = 0.740), and an increase limited to the period from 2015 to 2019 (mean annual change = 19.16%; CI = − 10.33%–27.99%; p = 0.080) (Fig. 4).
The overall mortality rate increased significantly when considering the whole period (mean annual change = 13.549%; CI = 4.82%–22.28%; p = 0.018), but this trend was not observed from 2015 to 2019 (mean annual change = 8.04%; CI = − 2.16%–18.24%; p = 0.280) (Fig. 5).
Regional data
The number of elective procedures performed laparoscopically steadily increased all over Italy. However, the difference was insignificant in six regions, considering the whole period and the first five years without analyzing the 2020 data (Valle d'Aosta, Trentino, Veneto, Umbria, Molise, Campania and Sicily). Molise and Campania (AIR = 0) observed the minimum annual intervention rate, while the maximum was registered in Trentino (61 in 2019) Table 2.
Concerning urgent procedures, an increase in the adoption of laparoscopy was observed. However, in 9 regions, this increase was not significant, considering the whole period and the first five years without analyzing the 2020 data (Valle d'Aosta, Trentino, Veneto, Liguria, Umbria, Abruzzo, Molise, Basilicata and Calabria). Furthermore, many regions showed the same annual intervention rate (AIR = 0), while the maximum was registered in Trentino (3).
Table 3 summarizes the distribution of urgent procedures in the index period.
Discussion
The present study provides an epidemiological snapshot of the laparoendoscopic treatment of groin hernias in Italy for the very first. The snapshot was obtained by processing the ICD9 Codes, and therefore the study provides a partial picture of the situation, although it is relatively indicative of the issue in Italy. The introduction in 1996 of the reimbursement system for medical procedures was developed to measure the productivity and intensity of work in hospital systems and was a real revolution in healthcare [6]. The data show a progressive increase in the laparoscopic approach to inguinal hernia over the last six years in all regions, although it is more significant in Northern Italy. The increasing trend was confirmed in 2020, although it was burdened by the COV-2 SARS pandemic afflicting the entire world. Globally, the minimally invasive approach is more widespread in wealthy countries, reaching high percentages in countries such as Australia (55%) and Switzerland (40%), probably determined both by the habits of surgeons and the welfare of the local health system [7, 8].
Nevertheless, an interesting observation is that despite the dramatic drop in the surgical caseload for benign disease in 2020, [9, 10] the rate of minimally invasive procedures across the total number of procedures performed raised to 5.98% in 2020, all groin hernia repairs performed.
Additionally, the increase in robotic procedures exceeded 2% of that observed for laparoscopic procedures. We explained the first observation as the surgery results in a few specialized centers with surgeons with the proper expertise in these procedures, whereas other less specialized centers abandoned groin hernia repair during the pandemic or referred the patients to other more qualified hospitals. [10]
As for robotic surgery, we think these data reflect the increasing robotic sprout we are witnessing in every surgical field. Future papers will show if this is connected to actual clinical benefits. [11]
Initially, the minimally invasive approach for treating inguinal hernias was hindered by the technical difficulties and a long learning curve associated with an operation that could be performed anteriorly with excellent results, especially for primary hernias [9, 10]. Moreover, this distrust of the minimally invasive approach was initially fueled by the risk of significant complications: visceral lesions during TAPP and vascular lesions during TEP [1, 3]. However, as of today, the International Guidelines published by the Hernia Surge Group have demonstrated the safety of the laparoendoscopic approach for inguinal hernias, especially concerning complications, and the results in terms of postoperative pain and recurrences are substantially comparable to groin hernia repair performed anteriorly [1]. From the analysis of the data, we are unable to trace the specific types of complications. However, we can see how they have progressively decreased and how mortality after 30 days is in line with the guidelines. The low conversion rate and complications could indicate that the centers performing TAPP or TEP are medium–high volume centers [12, 13]. In our study, we have no breakdown of the types of approach as the evaluation code does not provide differentiation in the kind of approach; however, we are aware that in Europe, transperitoneal operations are less prevalent compared to preperitoneal; while in Germany, according to the data of the German Hernia Surge Register, more TAPPs are performed, and only 20% are TEP; in Sweden and Switzerland, the preperitoneal approach is preferred [14, 15].
In addition to the technical difficulties and a long learning curve, in Italy, a further obstacle to the spread of the laparoscopic technique has been the remuneration of the operation that, regardless of whether the hernia was monolateral, bilateral or recurrent, is remunerated in the same way as a monolateral open hernioplasty. Although some recent studies have reported advantages in healthcare expenditure for laparoendoscopic procedures, this figure is probably distorted by the type of healthcare system adopted in each country [16, 17]. In some countries, the healthcare systems are welfarist, while in others, they are purely insurance-based, and in others still, they are mixed, so the impact of the reimbursement system could affect the push for health insurance in different ways. Moreover, as happened in Italy, the coding system has not been steadily updated, which has led to a lack of alignment with minimally invasive procedures. In Italy, only appendicectomy and cholecystectomy have a specific code when performed laparoscopically. At the same time, the other operations are associated with the laparoscopy code, yet the DRG (Diagnosis Related Group) reimbursement does not change. Reimbursement increases when a second procedure, such as adhesiolysis, is associated with the primary procedure, even if the lysis was performed on a single adhesion that would not have affected the hernioplasty approach. A recent paper by Aydin et al. showed that the cost of an anterior approach is similar to TAPP. However, the costs of hospital stay and anesthesia for each type of procedure are not reported, and bilateral and recurrence are compared [17]. The preperitoneal and transperitoneal approach does not seem to be related to a difference in expenditure. However, suppose the results of TEP and TAPP, as highlighted by the Guidelines, are equivalent, it is unthinkable that the difference in cost is determined only by the cost of the suture to close the peritoneum [1, 16, 17]. Other factors that could affect costs are complications. However, visceral and vascular lesions, in particular, have a very low incidence, so it is difficult to evaluate how much they affect costs [1, 4]. Unlike anterior approaches, high-energy devices (HED) could affect the cost of operations performed with the laparoendoscopic approach. However, as reported by Botteri et al. in a recent survey, the use of HED in abdominal wall surgery is not frequent [18, 19].
Another observation could be made regarding materials used for hernia repair. This information was not evaluable from the available dataset. Still, since there is a growing interest in using alternative materials for mesh, it could be interesting to make a further evaluation on the impact of costs on outcomes of their implementation into clinical practice. [20, 21]
Finally, as reported by Bracale et al., one of the major limitations in comparing laparoendoscopic and open surgical techniques is that scientific papers often compare bilateral vs monolateral hernias. [9]
From the data analysis, we can observe that there has been a progressive increase in the laparoendoscopic approach to inguinal hernia repair in Italy, together with an increase in the number of emergency operations performed for incarcerated hernias, showing a boost in confidence in the minimally invasive approach to inguinal hernioplasty even in more complex situations. In the literature, there are currently single experiences of some centers that demonstrate the operation's feasibility in safety, but with limits to the approach, regardless of the type of laparoendoscopic technique [9]; the guidelines of the Hernia Surge Group have not recommended the laparoscopic approach, but the advice is to select the method on a case-by-case basis [1].
It would have been interesting to have a better definition of the associated comorbidities to observe whether complications and mortality increased in correlation with some of them, as reported by some studies and guidelines [1]. However, from the analysis of the discharge codes, it was impossible to obtain reliable data on complications, likely because, due to the retrospective design of the registry, there was a lack of focus by the compilers.
Conclusions
The findings of the present study have shown a first snapshot of the use of minimally invasive techniques for groin hernias in Italy, with substantial compliance with the international guidelines. The most relevant observation that could be made according to our analysis was that the adoption of the laparoscopic approach knew a slow but steady increase from 2015 onward. Undoubtedly, improving the attention paid by medical staff to coding is indispensable, together with a revision of remuneration values, especially in universal-coverage healthcare systems.
References
International guidelines for groin hernia management (2018) HerniaSurge Group. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18(2):151–163. https://doi.org/10.1007/s10029-014-1236-6
Sartori A, De Luca M, Noaro G, Piatto G, Pignata G, Di Leo A, Lauro E, Andreuccetti JJ (2021) Rare Intraoperative and Postoperative Complications After Transabdominal Laparoscopic Hernia Repair: Results from the Multicenter Wall Hernia Group Registry. Laparoendosc Adv Surg Tech A 31(3):290–295. https://doi.org/10.1089/lap.2020.0459
Kingsnoth A, LeBlanc K (2003) Hernias: Inguinal and Incisional. Lancet 362:1561–1571
Pisanu A, Podda M, Saba A, Porceddu G, Uccheddu A (2015) Meta-analysis and review of prospective randomized trials comparing laparoscopic and Lichtenstein techniques in recurrent inguinal hernia repair. Hernia 19(3):355–366. https://doi.org/10.1007/s10029-014-1281-1
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Tran H, Tran K, Turingan I, Zajkowska M, Lam V, Hawthorne W (2015) Single-incision laparoscopic inguinal herniorraphy with telescopic extraperitoneal dissection: technical aspects and potential benefits. Hernia 19:407–416. https://doi.org/10.1007/s10029-015-1349-6
Tschuor C, Metzger J, Clavien PA, Vonlanthen R, Lehmann K (2015) Inguinal hernia repair in Switzerland. Hernia 19(5):741–745. https://doi.org/10.1007/s10029-015-1385-2
Arezzo A, Francis N, Mintz Y, Adamina M, Antoniou SA, Bouvy N, Copaescu C, de Manzini N, Di Lorenzo N, Morales-Conde S, Müller-Stich BP, Nickel F, Popa D, Tait D, Thomas C, Nimmo S, Paraskevis D, Pietrabissa A, EAES Group of Experts for Recovery Amid COVID-19 Pandemic (2021) EAES Recommendations for Recovery Plan in Minimally Invasive Surgery Amid COVID-19 Pandemic. Surg Endosc 35(1):1–17
Botteri E, Podda M, Sartori A (2020) The COVID-19 pandemic should not take us back to the prelaparoscopic era. J Trauma Acute Care Surg 89(2):273–274
Ayuso SA, Marturano MN, Katzen MM, Aladegbami BG, Augenstein VA (2022) Laparoscopic versus robotic inguinal hernia repair: a single-center case-matched study. Surg Endosc. https://doi.org/10.1007/s00464-022-09368-7
Merola G, Cavallaro G, Iorio O, Frascio M, Pontecorvi E, Corcione F, Andreuccetti J, Pignata G, Stabilini C (2020) Bracale U Learning curve in open inguinal hernia repair: a quality improvement multicentre study about Lichtenstein technique. Hernia 24(3):651–659. https://doi.org/10.1007/s10029-019-02064-x
Bracale U, Merola G, Sciuto A, Cavallaro G, Andreuccetti J, Pignata GJ (2019) Achieving the learning curve in laparoscopic inguinal hernia repair by tapp: a Quality Improvement Study. Invest Surg 32(8):738–745
Köckerling F, Lorenz R, Reinpold W, Zarras K, Conze J, Kuthe A, Lammers B, Stechemesser B, Mayer F, Fortelny R, Hoffmann H, Kukleta J, Weyhe D (2021) What is the reality in outpatient vs inpatient groin hernia repair? An analysis from the Herniamed Registry. Hernia. https://doi.org/10.1007/s10029-021-02494-6
Gass M, Banz VM, Rosella L, Adamina M, Candinas D (2012) Gu¨ller U (2012) TAPP or TEP? Population-based analysis of prospective data on 4,552 patients undergoing endoscopic inguinal hernia repair. World J Surg 36:2782–2786
Mongelli F, Vajana AFT, FitzGerald M, Cafarotti S, Lucchelli M, Proietti F, Di Giuseppe M, La Regina DJ (2019) Open and Laparoscopic Inguinal Hernia Surgery: A Cost Analysis. Laparoendosc Adv Surg Tech A 29(5):608–613. https://doi.org/10.1089/lap.2018.0805
Aydin M, Fikatas P, Denecke C, Pratschke J, Raakow J (2021) Cost analysis of inguinal hernia repair: the influence of clinical and hernia-specific factors. Hernia 25(5):1129–1135
Botteri E, Podda M, Arezzo A, Vettoretto N, Sartori A, Agrusa A, Allaix ME, Anania G, Brachet Contul R, Caracino V, Cassinotti E, Cuccurullo D, D’Ambrosio G, Milone M, Muttillo I, Petz WL, Pisano M, Guerrieri M, Silecchia G (2021) Agresta FCurrent status on the adoption of high energy devices in Italy: An Italian Society for Endoscopic Surgery and New Technologies (SICE) national survey. Surg Endosc 35(11):6201–6211. https://doi.org/10.1007/s00464-020-08117-y
Shimpei O, Yuji K, Atsuyuki M, Yuichi T, Yasuyuki F, Shunsuke O (2017) Ultrasonic energy device versus monopolar energy device in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. Updates Surg 69(1):55–60. https://doi.org/10.1007/s13304-016-0412-x
Pizza F, D’Antonio D, Lucido FS, Del Rio P, Dell’Isola C, Brusciano L, Tolone S, Docimo L, Gambardella C (2022) Is absorbable mesh useful in preventing parastomal hernia after emergency surgery? The Parthenope study. Hernia 26(2):507–516
Pizza F, D’Antonio D, Ronchi A, Lucido FS, Brusciano L, Marvaso A, Dell’Isola C, Gambardella C (2021) Prophylactic sublay non-absorbable mesh positioning following midline laparotomy in a clean-contaminated field: randomized clinical trial (PROMETHEUS). Br J Surg 108(6):638–643
Funding
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
AS, AB and MO conceived the study; AS, AB, MO, MP and EB designed and performed the research; AB and MO analyzed the data; AS, AB, MO and EB, wrote the paper; MG and MP supervised the paper; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflict of interest to disclose.
Research involving human participants and Informed consent
Data were collected anonymously from a national public database; no consent was needed for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ortenzi, M., Botteri, E., Balla, A. et al. Nationwide analysis of laparoscopic groin hernia repair in Italy from 2015 to 2020. Updates Surg 75, 77–84 (2023). https://doi.org/10.1007/s13304-022-01374-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01374-7