Abstract
Despite operative benefit and oncological non-inferiority, videolaparoscopic (VLS) colorectal surgery is still relatively underutilized. This study analyzes the results of a program for the implementation of VLS colorectal surgery started in an Italian comprehensive cancer center shortly before COVID-19 outbreak. A prospective database was reviewed. The study period was divided in four phases: Phase-1 (Open surgery), Phase-2 (Discretional phase), Phase-3 (VLS implementation phase), and Phase-4 (VLS consolidation phase). Formal surgical and perioperative protocols were adopted from Phase-3. Postoperative complications were scored by the Clavien–Dindo classification. 414 surgical procedures were performed during Phase-1, 348 during Phase-2, 360 during Phase-3, and 325 during Phase-4. In the four phases, VLS primary colorectal resections increased from 11/214 (5.1%), to 55/163 (33.7%), 85/151 (57.0%), and 109/147 (74.1%), respectively. The difference was statistically significant (P < 0.001). All-type VLS procedures were 16 (3.5%), 61 (16.2%), 103 (27.0%), and 126 (38.6%) (P < 0.001). Conversions to open surgery of attempted laparoscopic colorectal resections were 17/278 in the overall series (6.1%), and 12/207 during Phase-3 and Phase-4 (4.3%). Severe (grades IIIb-to-V) postoperative complications of VLS colorectal resections were 9.1% in Phase-1, 12.7% in Phase-2, 12.8% in Phase-3, and 5.3% in Phase-4 (P = 0.677), with no significant differences with open resections in each of the four phases: 9.4% (P = 0.976), 11.1% (P = 0.799), 13.8% (P = 1.000), and 8.3% (P = 0.729). Despite the difficulties deriving from the COVID-19 outbreak, our experience suggests that volume of laparoscopic colorectal surgery can be significantly and safely increased in a specialized surgical unit by means of strict operative protocols.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first laparoscopically assisted colectomy was reported by Jacobs [1]. Since then, a number of controlled studies and meta-analyses have shown that videolaparoscopic (VLS) colorectal resections are associated with lesser pain, earlier recovery, and non-inferior oncological outcomes, as compared with open surgery [2,3,4,5,6,7,8,9,10,11,12]. Although in recent years laparoscopic colorectal surgery has become increasingly popular, several Italian and international surveys have shown that it is still relatively underused, with substantial differences among centers [13,14,15,16,17,18,19].
The Fondazione IRCCS Istituto Nazionale dei Tumori of Milan (Italy) is one of the oldest and most important European comprehensive cancer centers. Before November 2018, open surgery was considered as default for colorectal cancer (CRC), except for patients affected by familial adenomatous polyposis (FAP) [20]. After that date, the choice between open and laparoscopic surgery was left at the discretion of surgeons of the Colorectal Surgery Unit (CSU). Finally, a formal program for the implementation of minimally invasive colorectal surgery was started in September 2019.
Shortly after the opening of our program, we had to face the sudden outbreak of Coronavirus disease 19 (COVID-19) [21]. Our institution was designed by Lombardy region health authorities as a COVID-19-free center to manage cancer patients from the surrounding hospitals overloaded by the pandemic. Furthermore, the use of VLS was reduced until data suggesting a negligible risk of COVID-19 transmission during laparoscopic surgery were reported [22].
As monitoring outcomes is a crucial part of health-care innovation, this study was performed to analyze the volume and safety of VLS procedures during the implementation process, and the impact of COVID-19 on our program.
Patients and methods
Data for the current study were retrieved from a prospective electronic database collecting the surgical procedures performed in our institution (http://10.4.0.102:8098/SaleOperatorie/). Accordingly, all the analyses were conducted on a per-procedure basis (one record per procedure). This study was approved by our Institutional Review Board and Ethics Committee (Protocol Number INT149/19), and was conducted in agreement with the principles of Helsinki Declaration. All patients gave informed consent.
Setting
Our CSU is a high volume unit in an oncological tertiary referral center. It includes the Peritoneal Surface Malignancy (PSM) Unit, and Hereditary Tumor Unit. The CSU is run by a team of eleven staff surgeons and two residents. Seven staff members have more than 20 years of experience from their board certification in general surgery. Three surgeons mainly perform cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC), and complex surgery for advanced/metastatic CRC; one surgeon performs both CRS/HIPEC and colorectal surgery; one surgeon treats both CRC and FAP patients; the remaining six mainly treat CRC. Two surgeons have a broad experience in VLS colorectal surgery, one performed regularly VLS as he was working in a general hospital previously, and four received formal VLS training during their residency. Two of them have also visited specialized centers abroad for additional training.
Study design
The study period extends from 2017.11.01 to 2021.09.15, and was divided into four equal duration phases:
-
Phase-1 (“Open surgery phase”): from 2017.11.01 to 2018.09.15.
-
Phase-2 (“Discretional phase”): from 2018.11.01 to 2019.09.15.
-
Phase-3 (“VLS implementation”): from 2019.11.01 to 2020.09.15.
-
Phase-4 (“VLS consolidation”): from 2020.11.01 to 2021.09.15.
The duration of Phase-2 (“Discretional phase”) was necessarily defined by the time period between the retirement of the former CSU director, and the taking office of the new director. During Phase-2, the CSU was held ad interim by the Surgical Department Chair, and surgeons were free to choose between open and VLS surgery, mainly based on their own judgment. Consequently, the same time span was chosen for the remaining three phases, to ensure equal length for each phase. During Phase-3 and Phase-4, VLS was considered for all patients, according to surgical and perioperative management protocols. Contraindications included previous extensive abdominal surgery, large tumors directly invading surrounding organs, obesity, severe abnormalities of cardiac output and/or gas exchange.
The surgical procedures were categorized as follows:
-
1.
Colorectal resections for primary CRC; as the present study is focused on surgical procedures, total colectomy/proctocolectomy for FAP, and surgery for anal spinocellular carcinoma relapsing after chemoradiotherapy were included.
-
2.
Transanal resections: transanal minimally invasive surgery (TAMIS), or transanal endoscopic microsurgery (TEM).
-
3.
CRS/HIPEC.
-
4.
Surgery for disease recurrences, such as CRC abdominal/pelvic relapses, peritoneal metastases, and PSM recurrences.
-
5.
Ostomy creation.
-
6.
Ostomy closure.
-
7.
Abdominal explorations, mainly to provide pathological diagnosis, or stage PSM patients before CRS/HIPEC.
-
8.
Emergency procedures, mostly performed to manage postoperative complications, because our center has no emergency department.
-
9.
Other surgical procedures.
Postoperative complications scored as grade IIIb (requiring intervention under general anesthesia), IV (life-threatening complications requiring intermediate/intensive care unit management), or V (death), according to the Clavien–Dindo classification, were considered as severe morbidity [23].
Preoperative procedures
Each patient had an intensive clinical/radiological work-up consisting of clinical history, physical examination, endoscopy, lung and abdominal–pelvic contrast-enhanced computed tomography, carcinoembryonic antigen, and CA-19.9. Patients with rectal tumors underwent pelvic magnetic resonance imaging, and endoscopic ultrasound. Additional studies were performed as needed. All patients were discussed during multidisciplinary meetings involving surgical, medical and radiation oncologists, radiologists, pathologists, and research nurses.
Preoperative radiotherapy was given to patients with cT3, cT4a/b, and/or cN+ primary rectal tumors below the peritoneal reflection, at a dose of 45/50 Gy in 25 days, with concurrent oral capecitabine or 5-fluorouracil-based chemotherapy, or as short-term course (25 Gy in 5 consecutive days).
Patients were admitted the day before surgery. On admission, subcutaneous nadroparin (3800 units once daily) was started. Mechanical bowel preparation was given. Cefazolin 2000 mg and metronidazole 500 mg were administered 30 min before skin incision and repeated every 6 h during surgery. Starting from Phase-3, oral metronidazole 2000 mg, neomycin 25,000 UI, and bacitracin 2500 UI were administered twelve hours before surgery.
Operative treatment
Both open and VLS resections for primary CRC were performed according to the oncologic principles of complete mesocolic excision with central vascular ligation. Total mesorectal excision was performed in rectal tumors, and a distal margin ≥ 2 cm was ensured for upper-third rectal cancer, along with appropriate circumferential resection margins. Any care was taken to preserve the mesorectal fascia. After neoadjuvant chemoradiation, a clear distal resection margin was guaranteed.
All VLS resections were performed under the direct supervision of an experienced surgeon, who gave side-by-side intraoperative teaching until the trainees gained proficiency in technical skills. The abdominal cavity was entered through an open access method (Hasson technique). The laparoscopic approach was used to explore the abdomen, mobilize the colon, identify critical structures, and divide vascular pedicles. A medial-to-lateral and from-top-to-bottom approach was followed to preserve mesocolic fascia integrity, and get complete clearance of mesocolic fat together with local–regional lymph nodes. In rectal cancer, inferior mesenteric artery and vein were divided proximally or, in selected cases, just above the emergence of the left colic artery.
The bowel was exteriorized through a small incision for resection and anastomosis. The same incision was used for specimen extraction. Conversion from laparoscopic to open surgery was allowed at the surgeon's discretion because of patient's safety, technical difficulties, advanced disease, or inadequate oncologic margins.
In all patients, a “fast-track” recovery protocol was adopted. The nasogastric tube was removed at the end of the operation. Ambulation and oral fluid intake were started from the day after surgery.
Statistics
Categorical variables were described in terms of frequency and percentages. Continuous variables were described with mean, and standard error. Differences between groups were assessed by 1-way ANOVA test, Chi-square test, or Fisher’s exact test, as appropriate. P values < 0.05 were considered significant. For primary colorectal resections, the learning curve was analyzed by the cumulative sum (CUSUM) methods, using severe complications and conversions to open surgery as indicators [24]. All statistical analyses were conducted by SPSS, version 20.0.0 for Windows (SPSS, Chicago, IL).
Results
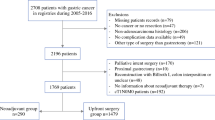
The main characteristics of the surgical procedures performed during each phase of the study are shown in Table 1; 414 procedures were performed during Phase-1, 348 during Phase-2, 360 during Phase-3, and 325 during Phase-4. With respect to the total number of procedures, the proportion of primary colorectal resections decreased over the four phases, although non-significantly (P = 0.053).
Laparoscopic procedures
The number and types of VLS vs. open procedures performed during the four phases of the study are shown in Table 2. The number of VLS colorectal primary resections increased from 11 (5.2%) in Phase-1, to 55 (33.7%) in Phase-2, 86 (57.0%) in Phase-3, and 109 (74.1%) in Phase-4. The difference was highly significant (P < 0.001). In the four phases, the number of all-type laparoscopic procedures was 16 (3.5%), 61 (17.5%), 103 (28.6%), and 126 (38.8%), respectively (P < 0.001). The difference was statistically significant also in the subset of elective procedures potentially eligible to VLS, excluding ostomy closures and transanal resections(P < 0.001).
Concerning the different primary colorectal resections, the percentage of laparoscopic procedures increased over the four study phases for right/transverse colectomies (P < 0.001), left/sigmoid colectomies (P < 0.001), rectal anterior resections (P < 0.001), and abdominal–perineal resections (P = 0.036). Interestingly, the proportion of primary rectal tumors operated by VLS increased more than fourfold from Phase-2 (12/66; 18.2%) to Phase-4 (43/56; 76.8%).
VLS procedures were performed by four surgeons in Phase-1, six surgeons in Phase-2, 11 surgeons in Phase-3 (including one resident), and 14 surgeons in Phase-4 (including three residents). In the four phases, VLS colorectal resections were performed by one, six, nine (including one resident), and 12 surgeons (including three residents), respectively.
The number of VLS vs. open surgical procedures performed each month during Phase-3 is shown in Fig. 1. No significant variation was observed in March 2020, after the COVID outbreak. In April, the total number of procedures and colorectal resections was increased, but only one abdominal exploration was performed laparoscopically. Finally, the number of laparoscopic colorectal resections increased in May, but the proportion of all-type VLS procedures remained low.
Videolaparoscopic (VLS) vs. open colorectal resections for primary tumors a, and VLS vs. open all-type surgical procedures, b performed each month during Phase-3 (2019.11.01 to 2020.09.15). In April 2020, the total number of procedures and colorectal resections was increased, but only one abdominal exploration was performed laparoscopically
In Fig. 2, box-and-whiskers plots show the decreasing operative time across study phases according to type of primary resections. The difference was significant for rectal resections (P = 0.032), but there was only a trend toward a decreased operative time for right/transverse (P = 0.685), and left-sigmoid colectomies (P = 0.158).
Safety
Seventy severe (Clavien–Dindo grades IIIb–V) complications occurred after 675 primary colorectal resections (10.4%). The most common complications were anastomotic leaks/bowel perforations (n = 42), followed by bleeding (n = 19), abdominal wall dehiscence (n = 6), postoperative ileum (n = 2), and ureter leak (n = 1). In the overall series, 114 severe complications occurred after 1289 all-type elective procedures (8.8%).
No in-hospital mortality occurred in patients undergoing primary colorectal resections during the four study phases. Conversely, one postoperative death occurred after CRS/HIPEC in Phase-4. Two additional patients died during Phase-2, but both patients underwent only emergency procedures to manage complications of elective surgery performed previously. Thus, one in-hospital mortality occurred after 1289 elective procedures included in the present analysis.
Conversion to open surgery occurred in two primary tumor resections (15.4%) during Phase-1, three (5.2%) during Phase-2, three (3.4%) during Phase-3, and nine (7.4%) during Phase-4 (P = 0.299). Concerning all-type surgical procedures, conversions were two (11.1%), three (4.9%), five (4.4%), and eleven (8.0%), respectively (P = 0.281).
Severe postoperative complications occurring during the four phases of the study are shown in Table 3, according to surgical procedure and open vs. laparoscopic approach. Morbidity rates did not change significantly for any surgical procedure over the study period. Complications of both open and VLS primary colorectal resections increased, although non-significantly, in Phase-2 and Phase-3, as compared with Phase-1, and then declined in Phase-4 to lower rates than in Phase-1. Severe morbidity was not significantly different between open and VLS colorectal resections in Phase-1 (P = 0.976), Phase-2 (P = 0.799), Phase-3 (P = 1.000), and Phase-4 (P = 0.729).
Unfortunately, the assessment of our learning curve for primary colorectal resections provided no meaningful result, presumably because splitting our case series into rectal vs. colonic surgery resulted in insufficient sample sizes. Furthermore, severe complication and conversion rates were comparable to reference literature data since the earlier phases of our experience [2,3,4,5,6,7,8,9,10,11,12,13], and did not change significantly during the study, further hampering our analyses (see Table 3).
To better characterize the safety profile of the present series, we assessed ASA score distribution among patients who underwent primary colorectal resections. The proportion of patients with ASA score of III–IV who underwent open surgery increased significantly from 33 (16.3%) in Phase-1 to 26 (23.9%) in Phase-2, 22 (33.8%) in Phase-3, and 18 (47.4%) in Phase-4 (P > 0.001). On the contrary, the proportion of patients with ASA score of III–IV who underwent VLS surgery did not change significantly, being 0, 9 (16.4%), 15 (17.4%), and 19 (17.4%), respectively, over the four phases (P = 0.595).
Discussion
The fundamental purpose of cancer therapy is to eradicate tumors and preserve patients’ quality of life. Laparoscopic colorectal surgery is associated with less postoperative pain, shorter time to recovery, shorter hospital stay, and non-inferior oncological outcomes [2,3,4,5,6,7,8,9,10,11,12]. In a challenging setting, such as the dramatic COVID-19 outbreak during the spring of 2020, our institutional program for the implementation of minimally invasive surgery resulted in a significant increase in the volume of laparoscopic colorectal resections, without clinically and statistically significant changes in postoperative severe complications.
Our CSU was one of the first surgical teams to introduce TME and colo-anal anastomoses in Italy during the 1990s, and it is highly specialized in conservative surgery for low rectal tumors [25]. Open colorectal surgery was considered as default because of lack of training in VLS, perceived oncological limitations of laparoscopic low rectal resections, and logistic issues, such as a large number of patients in the waiting list exceeding the capacity of our operating theaters, and shorter operative times of open surgery. A change of the head of the unit provided the opportunity to start a program for the implementation of VLS.
Recent literature data about the transition to minimally invasive surgery in specialized colorectal units are scarce because many institutions shifted to VLS before the year 2000, or during the first decade of the new millennium. The learning curve of VLS colorectal surgery has been reported to range widely from 30 to 80 cases, depending on colonic vs. rectal primary, and different outcome measures, but these series began in the early 1990s [26, 27]. More recently, the state of the art of laparoscopic surgery has greatly improved [28], and we hypothesized that a “global learning curve” could have resulted in a faster and safer increase in VLS volume. This innovative concept includes continuous technologic advancement, training improvements, and standardization of surgical and perioperative protocols. Our perspective is in agreement with Luglio et al., who report the results of the first 50 laparoscopic cases performed over 18 months in an Italian University Hospital. Operative outcomes were comparable to our series, but, unlike the present study, all the operations were performed by a single surgeon [29].
The March 2020 COVID-19 outbreak in Lombardy region had a negative impact on our program. First, the planned attendances of staff members to training courses with animal models and simulators in international centers were canceled. Second, concerns about possible COVID-19 transmission during laparoscopy led to a reduction in the number of VLS procedures until a screening protocol was set to identify asymptomatic COVID-19 patients before admission [30]. Third, since national and international guidelines suggested to postpone all non-strictly urgent surgeries, patients referred from other hospitals were mostly advanced cases or border-line surgical candidates with relevant comorbidities, for whom there was no available intensive care beds for postoperative recovery in the referring hospitals overloaded by COVID-19 [31].
As a result of our implementation program, the percentage of laparoscopic primary resections increased to 74.1% in our center. In 2019, an Italian survey involving 184 surgeons from 57 centers reported a 64.4% rate, but all the participating centers had an experience of ≥ 7 years in laparoscopic colorectal surgery [13]. Data from the UK for the year 2009, and Austria for the year 2013 revealed that only 25% and 26.1%, respectively, of colorectal procedures were performed laparoscopically [17, 18]. According to the National Surgical Quality Improvement Program (NSQIP) database, the use of laparoscopy increased in the USA from 22.7% in 2005 to 49.8% in 2014 [19]. Taken together, these data suggest that adoption rates for laparoscopy are still relatively low, compared to other fields of surgery, presumably due to the complexity of colorectal procedures.
An interesting finding of our study is the low rates of conversion to open surgery, that were required in 17/278 attempted laparoscopic operations in the overall series (6.1%), and 12/207 during Phase-3 and Phase-4 (4.3%). Completion rate is a quality indicator of VLS surgery. Conversions were 6.5% in an Italian survey [13], 17.9% in a systematic meta-analysis collecting 15 studies and 5293 patients [32], and up to 42% in the literature [4,5,6, 8, 32]. Furthermore, although confounding factors such as advanced tumor stage may play a role, unsuccessful laparoscopic surgery has been associated with poor perioperative and long-term outcomes [32].
Another interesting finding is that severe morbidity was not significantly higher in laparoscopic than open surgery. However, morbidity trends across study phases deserve a closer look. Complication rates of laparoscopic colorectal resections were similar between Phase-2 and Phase-3, and declined in Phase-4. This may suggest technical skill improvement, since only easier and less technically demanding cases were treated laparoscopically during Phase-2, and, indeed, there was a fourfold increase in the number of VLS rectal resections from Phase-2 to Phase-4. On the other hand, the steady (albeit non-significant) complication rate increase for open surgery in Phase-2 and Phase-3 appears to be related to the fact that the open approach was increasingly restricted to patients unfit for laparoscopic surgery. Also, the referral of patients with advanced tumors and/or border-line conditions from surrounding hospitals during the COVID-19 pandemic likely resulted in further deterioration of our surgical case-mix.
Our study suffers from the limitations of any retrospective series. However, we took advantage of our prospective clinical database to limit any potential bias. Also, our findings may be specific to our setting, given the broad experience in open colorectal surgery of our unit. Our attempts to analyze our learning curve were unsuccessful. Despite the relatively high volume of all-type VLS resections, the need to analyze separately colonic vs. rectal resections resulted in insufficient sample sizes. Furthermore, the different levels of expertise at baseline among members of our team (from experts who had presumably completed their learning curve, to surgeons trained in standard non-oncologic procedures, and absolute beginners) likely generated additional bias We are planning future studies, as soon as sufficient numbers are accumulated.
Conclusions
Despite the difficulties deriving from COVID-19 outbreak, our program was successful in increasing the volume of laparoscopic colorectal surgery, and keeping complication and conversion rates to acceptable levels. Our findings strongly suggest that other colorectal units still reluctant to embrace laparoscopic surgery should no longer be scared by outdated analyses reporting overly high number of consecutive procedures needed to gain technical proficiency. On the contrary, a rigorous implementation program would result in a faster and safer transition.
Data availability
Baratti, Dario (2021): Preliminary results of a program for the implementation of laparoscopic colorectal surgery in an Italian comprehensive cancer center during the COVID-19 pandemic.. figshare. Collection. https://doi.org/10.6084/m9.figshare.c.5772248.
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Lacy AM, García-Valdecasas JC, Delgado S et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Hazebroek EJ; Color Study Group (2002) COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc 16:949–953
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Jacob BP, Salky B (2005) Laparoscopic colectomy for colon adenocarcinoma: an 11-year retrospective review with 5-year survival rates. Surg Endosc 19:643–649
Fleshman J, Sargent DJ, Green E et al (2007) Clinical Outcomes of Surgical Therapy Study Group. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246:655–662 (discussion 662-4)
Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WC et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Jeong SY, Park JY, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Fleshman J, Branda ME, Sargent DJ et al (2019) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269:589–595
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 16:CD003432
Elmore U, Vignali A, Rosati R et al (2019) SICE national survey: current state on the adoption of laparoscopic approach to the treatment of colorectal disease in Italy. Updates Surg 71:77–81
Reames BN, Sheetz KH, Waits SA, Dimick JB, Regenbogen SE (2014) Geographic variation in use of laparoscopic colectomy for colon cancer. J Clin Oncol 32:3667–3672
Yeo H, Niland J, Milne D et al (2015) Incidence of minimally invasive colorectal cancer surgery at National Comprehensive Cancer Network centers. J Natl Cancer Inst 107:362
Schwab KE, Dowson HM, Van Dellen J, Marks CG, Rockall TA (2009) The uptake of laparoscopic colorectal surgery in Great Britain and Ireland: a questionnaire survey of consultant members of the ACPGBI. Colorectal Dis 11:318–322
Klugsberger B, Dietmar H, Oppelt P, Neuner L, Shamiyeh A (2015) Current state of laparoscopic colonic surgery in Austria: a national survey. J Laparoendosc Adv Surg Tech 25:976–981
Davis CH, Shirkey BA, Moore LW et al (2018) Trends in laparoscopic colorectal surgery over time from 2005–2014 using the NSQIP database. J Surg Res 223:16–21
Vitellaro M, Bonfanti G, Sala P et al (2011) Laparoscopic colectomy and restorative proctocolectomy for familial adenomatous polyposis. Surg Endosc 25:1866–1875
Rosenbaum L (2020) Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. NEJM 382:1873–1875
Hamid HKM (2020) Surgery during the COVID-19 pandemic. Lancet 396:e73
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Wohl H (1977) The CUSUM plot: its utility in the analysis of clinical data. N Engl J Med 296:1044–1045
Leo E, Belli F, Baldini MT et al (1993) Total rectal resection, colo-endoanal anastomosis and colic reservoir for cancer of the lower third of the rectum. Eur J Surg Oncol 19:283–293
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery. Comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44:217–222
Pascual M, Salvans S, Pera M (2016) Laparoscopic colorectal surgery: current status and implementation of the latest technological innovations. World J Gastroenterol 22:704–717. https://doi.org/10.3748/wjg.v22.i2.704
Luglio G, De Palma GD, Tarquini R et al (2015) Laparoscopic colorectal surgery in learning curve: Role of implementation of a standardized technique and recovery protocol. A cohort study. Ann Med Surg 4:89–94
Zheng MH, Boni L, Fingerhut A (2020) Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg 272:e5-6
Sorrentino L, Guaglio M, Cosimelli M (2020) Elective colorectal cancer surgery at the oncologic hub of Lombardy inside a pandemic COVID-19 area. J Surg Oncol 122:117–119
Clancy C, O’Leary DP, Burke JP et al (2015) A meta-analysis to determine the oncological implications of conversion in laparoscopic colorectal cancer surgery. Colorectal Dis 17:482–490
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All named authors have contributed to this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
This study was approved by the Institutional Review Board and Ethics Committee of the Fondazione IRCCS Istituto Nazionale dei Tumori, Milano (Italy) (Protocol Number INT 149/19).
Research involving human participants and/or animals
All procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version).
Informed consent
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baratti, D., Battaglia, L., Belli, F. et al. Preliminary results of a program for the implementation of laparoscopic colorectal surgery in an Italian comprehensive cancer center during the COVID-19 pandemic. Updates Surg 74, 1271–1279 (2022). https://doi.org/10.1007/s13304-022-01283-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01283-9