Abstract
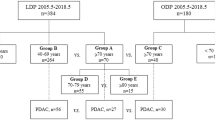
The purpose of the study is to evaluate whether laparoscopic pancreatoduodenectomy (LPD) is safe and feasible for elderly patients. From December 2015 to January 2019, 142 LPD surgeries and 93 OPD surgeries were performed by the same surgeon in the third affiliated hospital of Soochow University. After applying the inclusion and exclusion criteria, we retrospectively collected the date of three defined groups: LPD aged < 70 years (group I, 84 patients), LPD aged ≥ 70 years (group II, 56 patients) and OPD aged ≥ 70 years (group III, 28 patients). Baseline characteristics and short-term surgical outcomes of group I and group II, group II and group III were compared. Totally, 168 patients were included in this study; 100 cases were men; 68 cases were women; mean age was 67.9 ± 9.5 years. LPD does not perform as well in elderly as it does in non-elderly patients in terms of intraoperative blood loss (300.0 (200.0–500.0) ml vs. 200.0 (100.0–300.0) ml, p = 0.003), proportion of intraoperative transfusion (17.9% vs. 6.0%, p = 0.026) and time to oral intake (5.0 (4.0–7.0) day vs. 5.0 (3.0–6.0) day, p = 0.036). Operative time, conversion rate, postoperative stay, and proportion of reoperation, Clavien–Dindo classification, 30-day readmission and 90-day mortality were similar in two groups. In elderly patients, when compared with OPD, LPD had the advantage of shorter time to start oral intake (5.0 (4.0–7.0) day vs. 7.0 (5.0–11.3) day, p = 0.005) but the disadvantage of longer operative time (380.0 (306.3–447.5) min vs. 292.5 (255.0–342.5) min, p < 0.001) and higher hospitalization cost (12447.3 (10,189.7–15,340.0) euros vs. 7251.9 (8994.0–11,717.4) euros, p < 0.001). There was no difference between the two groups in terms of postoperative stay, and proportion of reoperation, Clavien–Dindo classification, 30-day readmission and 90-day mortality. LPD is safe and feasible for elderly people, but we need to consider its high cost and long operative time over OPD.
Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
He X, Song M, Qu J et al (2019) Basic and translational aging research in China: present and future. Protein Cell 10(7):476–484
Sukharamwala P, Thoens J, Szuchmacher M et al (2012) Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB 14(10):649–657
Yuan F, Essaji Y, Belley-Cote EP et al (2018) Postoperative complications in elderly patients following pancreaticoduodenectomy lead to increased postoperative mortality and costs. A retrospective cohort study. Int J Surg 60:204–209
Chen YT, Ma FH, Wang CF et al (2018) Elderly patients had more severe postoperative complications after pancreatic resection: a retrospective analysis of 727 patients. World J Gastroenterol 24(7):844–851
Chen K, Liu XL, Pan Y et al (2018) Expanding laparoscopic pancreaticoduodenectomy to pancreatic-head and periampullary malignancy: major findings based on systematic review and meta-analysis. BMC Gastroenterol 18(1):102
Zhou J, Xin C, Xia T et al (2017) Laparoscopic pancreaticoduodenectomy in A-92-older Chinese patient for cancer of head of the pancreas: a case report. Medicine 96(3):e5962
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591
Lu L, Zhang X, Tang G et al (2018) Pancreaticoduodenectomy is justified in a subset of elderly patients with pancreatic ductal adenocarcinoma: a population-based retrospective cohort study of 4,283 patients. Int J Surg 53:262–268
Shamali A, De’Ath HD, Jaber B et al (2017) Elderly patients have similar short term outcomes and five-year survival compared to younger patients after pancreaticoduodenectomy. Int J Surg 45:138–143
Ito Y, Kenmochi T, Irino T et al (2011) The impact of surgical outcome after pancreaticoduodenectomy in elderly patients. World J Surg Oncol 9:102
Croome KP, Farnell MB, Que FG et al (2014) Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 260(4):633–638 (discussion 638-640)
de Rooij T, Lu MZ, Steen MW et al (2016) Minimally invasive versus open pancreatoduodenectomy: systematic review and meta-analysis of comparative cohort and registry studies. Ann Surg 264(2):257–267
Palanivelu C, Senthilnathan P, Sabnis SC et al (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104(11):1443–1450
Mesleh MG, Stauffer JA, Bowers SP et al (2013) Cost analysis of open and laparoscopic pancreaticoduodenectomy: a single institution comparison. Surg Endosc 27(12):4518–4523
Gerber MH, Delitto D, Crippen CJ et al (2017) Analysis of the cost effectiveness of laparoscopic pancreatoduodenectomy. J Gastrointest Surg 21(9):1404–1410
Tan CL, Zhang H, Peng B et al (2015) Outcome and costs of laparoscopic pancreaticoduodenectomy during the initial learning curve vs laparotomy. World J Gastroenterol 21(17):5311–5319
Poves I, Burdio F, Morato O et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg 268(5):731–739
Torphy RJ, Friedman C, Halpern A et al (2019) Comparing short-term and oncologic outcomes of minimally invasive versus open pancreaticoduodenectomy across low and high volume centers. Ann Surg 270(6):1147–1155
Liang Y, Zhao L, Jiang C et al (2019) Laparoscopic pancreaticoduodenectomy in elderly patients. Surg Endosc. https://doi.org/10.1007/s00464-019-06982-w
Lee CS, Kim EY, You YK et al (2018) Perioperative outcomes of laparoscopic pancreaticoduodenectomy for benign and borderline malignant periampullary disease compared to open pancreaticoduodenectomy. Langenbecks Arch Surg
Tee MC, Croome KP, Shubert CR et al (2015) Laparoscopic pancreatoduodenectomy does not completely mitigate increased perioperative risks in elderly patients. HPB 17(10):909–918
Chapman BC, Gajdos C, Hosokawa P et al (2018) Comparison of laparoscopic to open pancreaticoduodenectomy in elderly patients with pancreatic adenocarcinoma. Surg Endosc 32(5):2239–2248
Adam MA, Thomas S, Youngwirth L et al (2017) Defining a hospital volume threshold for minimally invasive pancreaticoduodenectomy in the United States. JAMA Surg 152(4):336–342
Kutlu OC, Lee JE, Katz MH et al (2018) Open pancreaticoduodenectomy case volume predicts outcome of laparoscopic approach: a population-based analysis. Ann Surg 267(3):552–560
Evered L, Silbert B, Knopman DS et al (2018) Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth 121(5):1005–1012
Witlox J, Eurelings LS, de Jonghe JF et al (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4):443–451
Steinmetz J, Christensen KB, Lund T et al (2009) Long-term consequences of postoperative cognitive dysfunction. Anesthesiology 110(3):548–555
Hirpara DH, Azin A, Mulcahy V et al (2019) The impact of surgical modality on self-reported body image, quality of life and survivorship after anterior resection for colorectal cancer—a mixed methods study. Can J Surg 62(4):235–242
Gong GL, Liu B, Wu JX et al (2018) Postoperative cognitive dysfunction induced by different surgical methods and its risk factors. Am Surg 84(9):1531–1537
Shin YH, Kim DK, Jeong HJ (2015) Impact of surgical approach on postoperative delirium in elderly patients undergoing gastrectomy: laparoscopic versus open approaches. Korean J Anesthesiol 68(4):379–385
Tan CB, Ng J, Jeganathan R et al (2015) Cognitive changes after surgery in the elderly: does minimally invasive surgery influence the incidence of postoperative cognitive changes compared to open colon surgery? Dement Geriatr Cogn Disord 39(3–4):125–131
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This manuscript has not been published nor submitted for publication elsewhere. All authors have contributed significantly, and agree with the content of the manuscript. The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Ethical approval
This study has been approved by the Institutional Review Board of Changzhou First People’s Hospital ethics committee, and has been performed according to the ethical standards laid down in the 1964 Declaration of Helsinki.
Research involving human participants and/or animals
The study has been performed in accordance with the ethical standard of the instituional and/or national research committe, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tan, Y., Tang, T., Zhang, Y. et al. Laparoscopic vs. open pancreaticoduodenectomy: a comparative study in elderly people. Updates Surg 72, 701–707 (2020). https://doi.org/10.1007/s13304-020-00737-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00737-2